Abstract
The sub-study of the INSEMA trial (randomization-2) compares completion axillary lymph node dissection (cALND) with sentinel lymph node biopsy (SLNB) alone in cN0 patients with T1/T2 invasive breast cancer and one to three sentinel node macrometastases undergoing upfront breast-conserving surgery. The key secondary objective is to assess whether the SLNB-alone arm is non-inferior to cALND in terms of invasive disease-free survival (iDFS). Finally, 485 patients were recruited, and 386 patients (cALND: N = 169, SLNB alone: N = 217) were included in the per-protocol set. The median follow-up is 74.2 months. The 5-year iDFS analysis in the per-protocol set demonstrates a non-significant difference between study arms, with a hazard ratio (HR) of 1.69 (95% CI: 0.98-2.94) for SLNB alone compared to cALND. The 5-year iDFS rates are 86.6% (81.0%-90.7%) in the SLNB-alone arm and 93.8% (88.7%-96.6%) in the cALND arm (P = 0.058). The 5-year overall survival rates are 94.9% (90.6%-97.2%) in the SLNB-alone arm and 96.2% (91.7%-98.3%) in the cALND arm (P = 0.663). Locoregional recurrences (LRR) were infrequent, with 5-year incidence rates of 1.1% versus 0.0% (P = 0.405) in the SLNB-alone arm compared to cALND. In summary, no significant differences were observed between SLNB alone versus cALND for iDFS, overall survival, and LRR. Trial registration number: NCT02466737
Similar content being viewed by others
Introduction
The publication of the landmark American College of Surgeons Oncology Group (ACOSOG) Z0011 trial had a significant impact on the axillary management strategy for women with early breast cancer who did not receive neoadjuvant systemic therapy (NAST) and are pathologically sentinel lymph node-positive at diagnosis (after a clinically node-negative [cN0] presentation)1. The first results, after a median follow-up of 6.3 years, showed no difference between sentinel lymph node biopsy (SLNB) alone and completion axillary lymph node dissection (cALND) after breast-conserving surgery (BCS) with one or two metastases in the SLNB2,3. These data were confirmed by long-term analyses after a median follow-up of 9.3 years for overall survival (primary outcome), disease-free survival, and locoregional recurrences4,5.
Various limitations of the ACOSOG Z0011 trial, including the lack of preoperative axillary ultrasound (AUS), the significant enrollment of patients with nodal micrometastases, recruitment numbers lower than expected, and frequent protocol violations involving regional nodal irradiation (RNI)6, have led to the design of numerous validation trials. Four prospective randomized trials (SINODAR-ONE7, SENOMAC8, INSEMA (randomization-2)9, and POSNOC10) investigate the omission of cALND in sentinel lymph node-positive patients with upfront surgery. SINODAR-ONE, SENOMAC, and POSNOC recruited patients with one or two macrometastases in the sentinel nodes after BCS and mastectomy. The INSEMA sub-study enrolled only women with BCS. After protocol amendment #4 (September 2016), the maximum number of sentinel node macrometastases was increased to three.
Recently, 3-year survival and relapse rates after a median follow-up of 2.8 years for SINODAR-ONE patients demonstrated that the SLNB-alone arm was non-inferior to cALND11. The SENOMAC trialists’ group published secondary outcome data (5-year recurrence-free survival, RFS) after a median follow-up of 3.9 years, indicating that the omission of cALND was non-inferior to the more extensive surgery in patients also receiving nodal radiation therapy12. The primary end point of the POSNOC trial is the 5-year axillary recurrence rate; however, outcome data are not yet available.
We are now presenting the key secondary outcome data for the Intergroup-Sentinel-Mamma (INSEMA) trial. The goal of the INSEMA randomization-2 is to demonstrate that omission of cALND (SLNB alone) does not result in inferior invasive disease-free survival (iDFS) compared to the cALND arm in patients with one to three sentinel node macrometastases in early breast cancer treated with BCS and postoperative whole-breast irradiation (WBI).
Results
Patient characteristics
Patient and tumor characteristics for the per-protocol set are presented in Table 1. All baseline parameters were well-balanced between treatment arms except for the Ki-67 index. The percentage of tumors with a high proliferation rate (Ki-67 > 20%) was higher in the cALND arm compared to the SLNB alone arm (23.4 versus 15.4%; P = 0.06). The median age at diagnosis was 59.0 years (range 32.0–89.0; interquartile range [IQR]: 52.0–68.0). The median (IQR) preoperative tumor size, as determined by palpation, was 20 mm (15–20), and by imaging (95% based on sonography), 15 mm (11–19). Consequently, 81.1% of patients were diagnosed with a clinical T1 stage. In contrast to the preoperative evaluation, the rate of the pT2 stage increased to 39.4% after the final pathology report was documented. No difference was observed for medial tumor location between the study arms (cALND: 31.4% versus SLNB alone: 30.9%). Multifocal disease was more frequently diagnosed in the cALND arm (7.1 versus 3.2% in the SLNB alone arm; P = 0.081). The mean number of dissected sentinel lymph nodes was 2.4 (median 2.0; IQR: 1.0–3.0). The mean number of positive sentinel lymph nodes was 1.3 (median 1.0; IQR 1.0–1.0) without difference between study arms (P = 0.346). In the case of cALND, the mean number of dissected axillary lymph nodes was 13.2 (median 13.0; IQR: 10.0–15.0). The mean number of involved axillary lymph nodes in patients with cALND was 2.0 (median 1.0; IQR: 1.0–2.0). In the cALND arm, 19 patients (11.2%) had a pN2a stage.
Postoperative radiotherapy
A total of 386 patients were treated with 3D-conformal radiotherapy (3D-CRT) using standard tangential fields (N = 216, 56.4%). The remaining patients (N = 132, 34.4%) received modern intensity-modulated radiotherapy (IMRT) techniques. The deep inspiration breath-hold technique was applied in 10 patients (2.6%). No differences were observed between randomized groups regarding the radiotherapy technique used.
Conventional fractionation was the preferred schedule for the application of WBI in the randomization-2 cases (N = 304, 80.4%), with significant differences between treatment arms (cALND: 87.0% versus SLNB alone: 75.1%; P = 0.004). Moderate hypofractionation was used for 74 patients (19.6%), with a higher frequency in patients undergoing SLNB alone (24.9%) compared to 13.0% in patients with cALND. Standard WBI values for planned target volume (PTV), dose median, and dose average were not different between study arms with respect to the fractionation schedule. A tumor bed boost was delivered to 325 patients (84.2%) with a higher application rate in the cALND cohort (88.8 versus 80.6% in the SLNB alone arm; P = 0.035). The boost timing was balanced (50.5% simultaneously versus 49.5% sequentially); 23 patients (7.2%) were treated with intraoperative boost irradiation.
Detected values for dose median and dose average for each axillary level are shown in Table 2. All dose parameters are presented as relative doses, expressed as a percentage of the prescribed breast dose, to avoid differences in absolute doses between conventionally fractionated and hypofractionated cases. Approximately 75% of patients included in the analysis of “dose median” in axillary level I (based on the first quartile value; Q1) were unintentionally treated with ≥80% of the prescribed median breast radiation dose (50.9 Gy with conventional fractionation; 40.7 Gy with moderate hypofractionation) without differences between treatment groups. Applied relative doses were lower in axillary levels II and III compared to level I values, with a non-significant trend for higher doses (levels II–III) in the cALND arm.
The RNI was performed in 36.0% of patients with cALND, compared to 20.6% in the SLNB alone arm (P = 0.019). Predominantly, supraclavicular (34.8 versus 20.0%) and infraclavicular nodes (25.8 versus 14.3%) were included in the PTV, and less frequently, the internal mammary nodes (5.7 versus 0.8%). Notably, the RNI documentation started in March 2017 with the implementation of protocol amendment #4 (Table 3).
Adjuvant systemic therapy
No differences in the application of postoperative systemic treatment were observed between randomization groups in the per-protocol set (Table 3). Slightly more patients received adjuvant chemotherapy in the cALND arm (39.8 versus 33.6% in the SLNB alone arm; P = 0.239). Identical chemotherapy application rates were observed among the intention-to-treat (ITT) population: 35.7% in the cALND arm versus 36.3% in the SLNB-alone arm (P = 0.924).
End point analyses
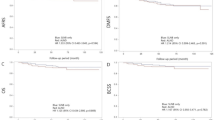
The median follow-up is 74.2 months (6.2 years), with an overall follow-up completeness of 89.3%13. The iDFS analysis in the per-protocol set demonstrates a non-significant difference between study arms, with an HR of 1.69 (95% confidence interval [CI]: 0.98–2.94) for SLNB alone compared to cALND (Fig. 1a), indicating that non-inferiority could not be demonstrated. The estimated 5-year iDFS rates are 86.6% (81.0–90.7%) in the SLNB-alone arm and 93.8% (88.7–96.6%) in the cALND arm (log-rank P = 0.058).
The first iDFS events for SLNB alone versus cALND are listed in Table 4. Differences were observed when comparing distant relapse (SLNB alone: 6.9% versus cALND: 4.1%) and secondary malignancy rates (SLNB alone: 4.1% versus cALND: 2.4%). The estimated 5-year overall survival rates are 94.9% (90.6–97.2%) in the SLNB-alone arm and 96.2% (91.7–98.3%) in the cALND arm (Fig. 1b; log-rank P = 0.663).
Analyses among the sensitivity set (including patients without radiotherapy; N = 404) confirmed the results in the per-protocol set with estimated 5-year iDFS rates of 86.1% (80.5–90.2%) for the SLNB alone versus 93.3% (88.2–96.2%) for the cALND arm (log-rank P = 0.061). Among the ITT set, the iDFS analysis (Fig. 1c) shows no difference between study arms, with an HR of 1.26 (95% CI: 0.80–1.99) for SLNB alone compared to cALND. The distribution (SLNB alone versus cALND) of first iDFS events (N = 75) was slightly different from the per-protocol set: invasive locoregional recurrences (2.5 versus 1.6%), including axillary recurrences (0.8 versus 0.4%), invasive contralateral breast cancer (0.8 versus 0.0%), distant metastases (6.6 versus 4.5%), secondary malignancies (3.7 versus 2.9%), and deaths (3.7 versus 4.5%). The estimated 5-year iDFS rates (ITT set) are 86.0% (80.6–90.0%) in the SLNB-alone arm and 89.3% (84.3–92.8%) in the cALND arm (log-rank P = 0.314).
Multivariate Cox regression analysis for iDFS, adjusted by stratification factors, showed that age ≥65 years and preoperative tumor size >2 cm, but not tumor grading G3, were related to worse iDFS (Table S1). The univariate Cox regression for iDFS in subgroups for age, tumor size, and number of macrometastases showed no substantial heterogeneity in HR (SLNB alone versus cALND) between subgroups (Fig. 2). Patients with highly proliferative tumors (Ki-67 > 20%) significantly benefited from the cALND regarding 5-year iDFS (HR = 4.36 [1.20–15.86] versus HR = 1.39 [0.75–2.58] for patients with a Ki-67 ≤ 20%). Patients potentially candidates for SLNB omission according to the published INSEMA randomization-1 results14 and updated ASCO guideline criteria15 had less benefit from the cALND in terms of 5-year iDFS compared to patients who are still candidates for the SLNB procedure (HR = 1.47 [0.70–3.08] versus HR = 1.97 [0.86–4.49]).
ASCO guideline criteria for SLNB omission during breast-conserving therapy are: postmenopausal status (age ≥50 years), preoperative tumor size ≤2 cm, tumor grading G1-G2, and hormone receptor-positive/HER2-negative subtype. pT pathological tumor stage, N numbers, TS preoperative tumor size, based on sonography results. If those were missing, results from other assessments were used in the following order: mammography and magnetic resonance imaging.
Surgical complications
The rate of updated short-term surgery-related complications (Table S2) confirmed previously published data16. The long-term safety analysis demonstrates that patients in the SLNB alone arm benefited in terms of reduced lymphedema rate (6.6 versus 14.9%), arm/shoulder mobility restriction (2.5 versus 8.0%), and arm/shoulder movement pain (3.1 versus 5.8%), all parameters not resolved at the last follow-up visit (Table S3).
Discussion
INSEMA randomization-2 provides additional data on the oncological safety of patients with cALND omission following a positive SLNB during BCS, with a strict indication for RNI and radiotherapy quality assurance. For the first time, these results suggest a potential impact of omission of the cALND on the 5-year iDFS. However, fair conclusion cannot be given due to the fact that the targeted number of patients (initially 1968) was not met. The objective of the randomization-2 was downgraded to a secondary outcome during recruitment period so that previous statistical assumptions for non-inferiority of the SLNB-only arm as co-primary end point are not appropriate for the current analysis.
The INSEMA randomization-2 is a validation trial with an identical follow-up (6.2 versus 6.3 years) to the first publication of the ACOSOG Z0011 data2,3. The number of recruited patients with macrometastases in the SLNB is comparable between the two studies; all patients underwent BCS in both trials. In contrast to Z0011 and other validation trials, women with three sentinel nodes macrometastases (3.4%) could be enrolled in the INSEMA sub-study.
Regarding overall survival, the primary end point of the Z0011 trial, our secondary outcome analyses confirm the previous data. No difference was observed between the treatment arms, with slightly higher estimated 5-year overall survival rates in the INSEMA randomization-2, indicating a different risk profile for the recruited patients. Rates for clinical T2 stage, hormone receptor negativity, and high tumor grading (G3) were higher among the Z0011 population3. Overall survival rates as a primary end point in other validation trials (SINODAR-ONE, SENOMAC) are only available for SINODAR-ONE (per-protocol set: N = 822). After a median follow-up of 34.0 months, the 5-year overall survival rates were 99.2% and 98.7% in the cALND and SLNB-alone arms, respectively11.
Similarly, the 5-year iDFS did not differ significantly between the two groups of axillary treatment among INSEMA randomization-2. However, the iDFS curves separate after a follow-up of 36 months, with numerically higher iDFS rates in the cALND arm. This iDFS curve splitting was more pronounced in the per-protocol and sensitivity cohorts compared to the ITT set. The reported absolute difference of 7.2% for the estimated 5-year iDFS rates (per-protocol set) is primarily attributed to higher rates of distant relapses, unrelated secondary malignancies, and deaths. However, based on the fact that there was only 1 axillary recurrence in the entire per-protocol population over 6 years, the benefit of cALND to prevent axillary recurrences is negligible, and it seems unlikely that omission of cALND in the setting of appropriate systemic therapy and unintentionally radiation coverage to the lower axilla in most cases translates to significantly worse distant events. In contrast, Z0011 and recently published validation trials reported no differences in secondary survival parameters comparing SLNB alone versus cALND; the 5-year disease-free survival rates were 83.9% and 82.2%, respectively, among the Z0011 population3. In the SINODAR-ONE per-protocol cohort, the 5-year RFS rates were 95.6% and 96.4%, respectively11. The per-protocol SENOMAC population comprised 2540 patients, with estimated 5-year RFS rates of 89.7% and 88.7%, respectively12.
The INSEMA cALND cohort is characterized by higher rates of postoperative chemotherapy, conventionally fractionated WBI, tumor bed boost application, and RNI. The imbalance in chemotherapy and RNI frequencies between the randomization-2 groups was expected, given the knowledge of the pN2a stage in the cALND arm (11.2%). However, this cannot fully explain the described effect on the 5-year iDFS among the INSEMA population. Higher rates of postoperative chemotherapy in the cALND arm were also reported for the SINODAR-ONE and SENOMAC patients with no impact on RFS11,17.
The de-escalation of axillary surgery during BCS must be discussed in the context of radiotherapy. According to the INSEMA protocol, the randomization-2 cohort is characterized by a representative proportion of patients treated with moderate hypofractionation (19.6%). The high rate of 84.2% for tumor bed boost application after BCS is comparable to the SINODAR-ONE trial data (68.8% with boost). Despite a higher use of RNI in the cALND arm, no differences between the arms of the INSEMA randomization-2 were observed regarding incidental doses to the axilla. Recently, the EBCTCG meta-analysis demonstrates that RNI reduces the rate of breast cancer recurrence and improves breast cancer-specific and overall survival after long-term follow-up18. The current ESTRO ACROP guideline recommends consideration of moderate hypofractionation for RNI19. The HypoG-01 and the DBCG Skagen-1 trials have established non-inferiority of moderate hypofractionation for lymphedema. However, conflicting results have been reported regarding oncological outcomes. The HypoG-01 trialists demonstrated significant improvements in locoregional recurrence-free survival, disease-free survival, and overall survival with moderate hypofractionation20. In contrast, the DBCG Skagen trial-1 found that breast cancer-specific mortality was higher with moderate hypofractionation21. Again, while differences in RNI use and fractionation regimens may have affected the outcome in INSEMA randomization-2, the minor differences in treatment patterns do not fully explain the observed differences in the 5-year iDFS.
The consequences of omitting cALND after one to three macrometastases in the SLNB (including the questionable trend for impaired 5-year iDFS and lack of information for postoperative treatment indications, such as RNI and chemotherapy) must be weighted against the benefits of improved quality-of-life (QoL) and reduced risk of long-term complications. The large number of patients excluded from the per-protocol analysis (N = 66) due to not accepting randomization to the cALND arm suggests that both patients and providers are choosing to avoid cALND over the timeframe of the INSEMA study.
This INSEMA Rando2 analysis has numerous strengths. First, data are based on the longest median follow-up and the highest axillary tumor burden of all Z0011 validation trials. Second, patient-reported outcomes and prospective assessment regarding incidental axillary irradiation dose values during WBI are secondary outcomes for the study population. Third, target volumes for postoperative radiotherapy were predefined, thereby avoiding potential overtreatment.
In addition, our study has several limitations. First, the target recruitment number for the second randomization was not achieved, leading to an underpowered sub-study with only 20–25% of the planned enrollment. Second, major crossover between per-protocol and ITT cohorts lead to incongruent results comparing 5-year iDFS rates. Finally, the median follow-up of 6.2 years is appropriate for reporting 5-year survival data, but it may miss late recurrences in hormone receptor-positive diseases22. The analysis of 10-year survival data is planned for September 2029.
In conclusion, INSEMA randomization-2 demonstrated no significant differences between cALND versus SLNB alone in sentinel node-positive patients with early breast cancer and primary breast-conserving therapy. From a statistical point of view, our results regarding observed 5-year iDFS differences may be inconclusive and do not necessarily represent a failure to demonstrate non-inferiority of the SLNB-only arm. In the setting of increased use of RNI for any macrometastatic node-positive disease in the radiation oncology world, our results do not support the indication for cALND in patients with one to three sentinel node macrometastases.
Methods
A comprehensive review of the INSEMA trial design was published in December 2024, together with the report of primary outcome data of the INSEMA randomization-1. Patients were first randomized to either no axillary surgery or SLNB in a 1:4 allocation. The complete omission of surgical axillary staging was non-inferior to SLNB, analyzing the 5-year iDFS after a median follow-up of 6.1 years14. The Clinical Trial Number is NCT02466737. The date on which the study record was first available on ClinicalTrials.gov was 2015-JUN-09.
Patients
Women with breast cancer up to 5 cm (cT1/T2 stages), cN0 status (clinically and per imaging [iN0]), and upfront BCS were eligible. Patients with SLNB and pN+(sn) status (1–3 macrometastases) were randomized (1:1 ratio) to either SLNB alone or cALND. During follow-up, patients were assessed according to standard clinical practice.
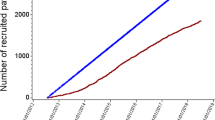
Four hundred eighty-five patients were recruited for the second randomization (ITT set: N = 243 with cALND versus N = 242 with SLNB alone). After excluding 99 patients, 386 patients (cALND: N = 169, SLNB alone: N = 217) were included in the per-protocol set (Fig. 3). The main reasons for excluding patients (20.4%) were axillary surgery not according to the randomized arm (cALND: N = 66 versus SLNB alone: N = 14) and no application of postoperative radiotherapy (cALND: N = 7 versus SLNB alone: N = 11). The safety set was used to analyze both short-term and long-term surgical complications.
Local treatment
The preoperative diagnostic workup included a routine AUS performed before biopsy. All patients underwent ipsilateral BCS with postoperative WBI regardless of the intrinsic subtype. Conventional fractionation or moderate hypofractionation was an option using 3D-CRT or IMRT techniques for WBI. The axilla was not explicitly targeted. RNI was only recommended for patients with four or more positive axillary lymph node metastases as reported in the final pathology. Boost irradiation of the tumor bed was generally recommended but could be omitted in selected patients (those aged >60 years, with small tumor sizes, and favorable prognostic factors). The use of partial breast irradiation alone was not allowed. The first three radiotherapy plans treated at each center underwent central quality assurance23. Dosimetric data for axillary lymph node levels I-III were prospectively collected for the entire study population.
Trial end points
The iDFS, as the primary outcome for the first randomization, is defined as the period between randomization and the first event (locoregional or distant invasive recurrence, death from any cause, contralateral invasive breast cancer, or second primary invasive cancer [non-breast])24. Due to the number of SLNB-positive patients being fewer than expected, the iDFS analysis for the second randomization was downgraded from a co-primary to a key secondary outcome following protocol amendment #5 (December 2018). Other secondary end points were overall survival, locoregional disease-free survival, ipsilateral axillary recurrence rate, distant disease-free survival, QoL analyses, and dose distribution in ipsilateral axilla levels I-III during radiotherapy.
Statistical analysis
The following assumptions were made for the second randomization: the 5-year iDFS for optimally treated patients with one to three sentinel node macrometastases was considered 81%, and the non-inferiority margin was defined as the SLNB-alone group having a 5-year iDFS of not less than 76.5% (upper 95% CI end for HR < 1.271). The overall error rate of a false-positive outcome (α) is 5%, and the adjusted α for the second randomization was 3.61%. The error rate for a false-negative result (β) was set to 20%, i.e., the power of the trial was set to 80% for the difference in clinical interest. The calculated number of patients included in the per-protocol set for the second randomization was initially 1968. An event-driven final efficacy analysis was planned when 484 events occurred.
However, this target number of randomization-2 was not achieved for various reasons. First, the observed sentinel node-positivity rate for one to three macrometastases was lower than expected, at only 11.3% among the first INSEMA randomization cohort. Second, the recruitment rate directly for randomization-2 was below the planned numbers. Third, the ACOSOG Z0011 publication of long-term follow-up data in 2016/2017 led to modifications in the German guidelines and a decrease in the acceptance of the INSEMA randomization-2 design among physicians and patients. The INSEMA protocol amendment #5, which includes downgrading the iDFS analysis of randomization-2 to a secondary outcome without statistical assumptions, was released following a recommendation from the Independent Data Monitoring Committee.
Due to the non-inferiority study design, the key secondary end point analysis was performed on the per-protocol set25,26. All outcome results will be reported for both the per-protocol and ITT sets, as well as in a sensitivity analysis that includes patients who did not receive radiotherapy.
The analyses were performed using data available as of August 30, 2024, following 5.3 years of follow-up since the last patient was enrolled. The Kaplan–Meier product-limit method estimated 5-year iDFS rates (reported with the two-sided 95% CI). The non-inferiority was tested based on the 95% CI of the HR from the Cox proportional hazard model to exclude the HR of 1.271, but with no conclusive value for the key secondary objective. A multivariate Cox proportional hazards model adjusted HRs for stratification factors (age, tumor size, and tumor grading). The homogeneity of findings was explored in subgroups defined by age, tumor size, the number of macrometastases, and Ki-67 index using univariate Cox regression analyses. The Pocock minimization method27 was used for treatment allocation, stratified according to defined stratification criteria.
Analyses were performed using SAS® (Statistical Analysis Software; Cary, NC, USA) version 9.4 with SAS Enterprise Guide 8.3. There was no prespecified plan to adjust for multiple comparisons. All CIs and tests were two-sided; the widths of the CIs are not adjusted for multiple comparisons and should not be used in place of hypothesis testing of secondary outcomes.
Ethics approval declaration
All patients provided informed written consent. The trial was conducted and monitored according to Good Clinical Practice guidelines based on the Declaration of Helsinki. After approval by the local independent review board at the University of Rostock (Germany, registration number HV-2011-0010), INSEMA randomization-2 enrolled women aged 18 years or older between September 2015 and April 2019 at 114 German and six Austrian study sites.
Data availability
All available data are presented in the current manuscript.
References
Brackstone, M. et al. Management of the axilla in early-stage breast cancer: Ontario Health (Cancer Care Ontario) and ASCO Guideline. J. Clin. Oncol. 39, 3056–3082 (2021).
Giuliano, A. E. et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann. Surg. 252, 426–432 (2010).
Giuliano, A. E. et al. Axillary dissection vs. no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA 305, 569–575 (2011).
Giuliano, A. E. et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: Long-term follow-up from the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 randomized trial. Ann. Surg. 264, 413–420 (2016).
Giuliano, A. E. et al. Effect of axillary dissection vs. no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318, 918–926 (2017).
Jagsi, R. et al. Radiation field design in the ACOSOG Z0011 (Alliance) Trial. J. Clin. Oncol. 32, 3600–3606 (2014).
Tinterri, C., Canavese, G., Bruzzi, P. & Dozin, B. SINODAR-ONE, an ongoing randomized clinical trial to assess the role of axillary surgery in breast cancer patients with one or two macrometastatic sentinel nodes. Breast 30, 197–200 (2016).
de Boniface, J. et al. Survival and axillary recurrence following sentinel node-positive breast cancer without completion axillary lymph node dissection: the randomized controlled SENOMAC trial. BMC Cancer 17, 379 (2017).
Reimer, T., Hartmann, S., Stachs, A. & Gerber, B. Local treatment of the axilla in early breast cancer: concepts from the NSABP B-04 to the planned INSEMA trial. Breast Care 9, 87–95 (2014).
Goyal, A. et al. POSNOC – POsitive Sentinel NOde: adjuvant therapy alone versus adjuvant therapy plus Clearance or axillary radiotherapy: a randomised controlled trial of axillary treatment in women with early-stage breast cancer who have metastases in one or two sentinel nodes. BMJ Open 11, e054365 (2021).
Tinterri, C. et al. Preservation of axillary lymph nodes compared with complete dissection in T1-2 breast cancer patients presenting one or two metastatic sentinel lymph nodes: the SINODAR-ONE multicenter randomized clinical trial. Ann. Surg. Oncol. 29, 5732–5744 (2022).
de Boniface, J. et al. Omitting axillary dissection in breast cancer with sentinel-node metastases. N. Engl. J. Med. 390, 1163–1175 (2024).
Clark, T. G., Altman, D. G. & De Stavola, B. L. Quantification of the completeness of follow-up. Lancet 359, 1309–1310 (2002).
Reimer, T. et al. Axillary surgery in breast cancer—primary results of the INSEMA trial. N. Engl. J. Med. 392, 1051–1064 (2025).
Park, K. U. et al. Sentinel lymph node biopsy in early-stage breast cancer: ASCO guideline update. J. Clin. Oncol. 41, 1720–1741 (2025).
Reimer, T. et al. Patient-reported outcomes for the Intergroup Sentinel Mamma study (INSEMA): a randomised trial with persistent impact of axillary surgery on arm and breast symptoms in patients with early breast cancer. EClinicalMedicine 55, 101756 (2022).
Tvedskov, T. F. et al. Axillary clearance and chemotherapy rates in ER+/HER2- breast cancer: secondary analysis of the SENOMAC trial. Lancet Reg. Health Eur. 47, 101083 (2024).
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Radiotherapy to regional nodes in early breast cancer: an individual patient data meta-analysis of 14324 women in 16 trials. Lancet 402, 1991–2003 (2023).
Meattini, I. et al. European Society for Radiotherapy and Oncology Advisory Committee in Radiation Oncology Practice consensus recommendations on patient selection and dose and fractionation for external beam radiotherapy in early breast cancer. Lancet Oncol. 23, e21–e31 (2022).
Rivera, S. et al. Locoregional hypo vs normofractionated RT in early breast cancer: 5 years results of the HypoG-01 phase III UNICANCER trial. In Proc. ESMO Congress 2024. Abstract 231O Ann Oncol 35, (2024)..
Offersen, B. V. et al. DBCG Skagen trial 1:Phase III randomised trial of hypo- vs standard fractionated loco-regional radiotherapy in node-positive breast cancer patients. Late-breaking abstract #5027. Radiother. Oncol. 206, S4430–S4432 (2025).
Pan, H. et al. 20-year risks of breast cancer recurrence after stopping endocrine therapy at 5 years. N. Engl. J. Med. 377, 1836–1846 (2017).
Hildebrandt, G. et al. Central review of radiation therapy planning among patients with breast-conserving surgery: results from a quality assurance process integrated into the INSEMA trial. Int J. Radiat. Oncol. Biol. Phys. 107, 683–693 (2020).
Hudis, C. A. et al. Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J. Clin. Oncol. 25, 2127–2132 (2007).
European Medicines Agency: ICH Topic E9 statistical principles for clinical trials. https://www.ema.europa.eu/en/ich-e9-statistical-principles-clinical-trials-scientific-guideline. Accessed 25 December (2025).
Hernán, M. A. & Robins, J. M. Per-protocol analyses of pragmatic trials. N. Engl. J. Med. 377, 1391–1398 (2017).
Pocock, S. J. & Simon, R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 31, 103–115 (1975).
Acknowledgements
The INSEMA trial was sponsored by the University Medicine Rostock (Germany) and financed by the Deutsche Krebshilfe under grant numbers #110580 and #70110580 (German Cancer Aid, Bonn, Germany). The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript. The locoregional subboard of GBG (Neu-Isenburg, Germany) overlooked the trial; the ABCSG (Vienna, Austria) coordinated the Austrian study sites. Oral presentation at the San Antonio Breast Cancer Symposium 2025.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
T.R., A.S., K.V., T.K., J.H., S.P., F.M., E.T., G.H., D.K., B.A., R.R., S.R., C.D., I.B., N.S., M.T., H.S., T.M., M.G., D.Z., J.H., M.K., V.N., S.L., and B.G. contributed to the study design, collection, and documentation of data. T.R., A.S., T.K., D.K., J.H., V.N., S.L., and B.G. wrote the main manuscript text, and V.N. prepared Figs. 1–3. V.N. was responsible for statistical analysis. T.R., A.S., K.V., T.K., J.H., S.P., F.M., E.T., G.H., D.K., B.A., R.R., S.R., C.D., I.B., N.S., M.T., H.S., T.M., M.G., D.Z., J.H., M.K., V.N., S.L., and B.G. reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reimer, T., Stachs, A., Veselinovic, K. et al. Axillary surgery in patients with sentinel node macrometastases: secondary results of the randomized INSEMA trial. npj Breast Cancer 12, 19 (2026). https://doi.org/10.1038/s41523-026-00902-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-026-00902-7