Abstract
Creativity, the capacity and motivation to produce novel and personally meaningful ideas or behaviors, can be influenced by Parkinson’s disease (PD). Non-motor neuropsychological symptoms, such as apathy and negative schizotypy have been linked to reduced creativity, while dopaminergic treatments are associated with increased creative engagement. Building on epidemiological findings investigating changes in creativity, we examined possible drivers of increased and decreased creative activity. In a cross-sectional study, 360 participants with PD completed a questionnaire assessing self-reported creativity changes and associated factors, including personality (Big-Five, Multidimensional-Schizotypy-Scale), lifestyle (e.g., creative lifestyle, free time), and clinical (HY-scores, MoCA, dopaminergic treatments). Using machine learning (gradient-boosted decision-trees), we explained 23% of variance in creativity changes. Dopamine agonists, extraversion, free time, and a creative lifestyle since symptom onset predicted increased creativity, while disorganized schizotypy predicted decreases. The findings provide new insights for future research on creativity as part of PD’s neuropsychological spectrum and for person-centered treatment.
Similar content being viewed by others
Introduction
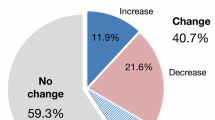
Parkinson’s disease (PD) is traditionally recognized for its motor symptoms1. However, PD also involves a range of cognitive and affective changes, including impaired executive functioning and mood disturbances, which significantly impact behavior in daily life2,3,4. Creativity—broadly defined as the motivation and behavior to engage in novel ideas or activities that offer both artistic expression and personal satisfaction5—has also been suggested to be influenced by PD-related symptoms as well as dopaminergic treatment6,7,8. This has been supported by a recent large-scale epidemiological survey, in which 41% of 793 individuals with PD reported to experience changes in their creativity, with a 2:1 ratio of decreases to increases9.
These changes may, in part, be explained by non-motor deficits, such as apathy, cognitive inflexibility and reduced novelty-seeking, which have been associated with decreases in both the capacity and motivation to engage in creative activities10,11,12. Studies suggest that a reduced engagement in artistic occupations prior to a PD diagnosis may reflect a decline in creative interest during the prodromal phase, with suggested potential recovery upon dopaminergic treatment13,14,15,16,17. Among dopaminergic treatment, dopamine agonists in particular have been associated with increased creativity18,19,20,21,22. Lifestyle adjustments following a PD diagnosis—such as shifts in artistic capacities and changes in creative style—have also been linked to increased inclination towards creative activities15,16,17,23,24.
These findings raise questions about whether changes in creativity, specifically the inclination to engage in and devote time to creative activities, are tied to the neuropsychological spectrum including changes in personality, lifestyle adjustments, and associated with clinical factors. Research on neuropsychological symptoms in PD highlights personality changes20,25,26,27. Such changes include, on the one end, reduced openness to experience (often associated with apathy), increased neuroticism and introversion, which are all linked to decreased creativity28,29,30. On the other end, traits like extraversion, novelty seeking, and positive schizotypy are associated with dopaminergic therapy and increased creativity12,31,32. Similar personality patterns have been observed in artists. Depressive states and negative schizotypy tend to correlate with reduced creativity, while manic states, extraversion, and positive schizotypy are linked to increased creativity8,33,34,35,36,37,38,39.
Lifestyle adjustments may also influence creativity from a neuropsychological perspective. A review on artistic changes in individuals with neurodegenerative disorders suggests that increased free time from early retirement may heighten the propensity to engage in creative activities17,40. Furthermore, the impact of a PD diagnosis on one’s personal life and social environment may encourage creative engagement, either as a personal coping strategy or through caregiver recommendations18,41,42.
We conducted an exploratory, data-driven investigation using machine learning to analyze the effects of personality traits, lifestyle adjustments, and clinical factors on creative engagement in individuals with PD. The analysis is based on data from 360 participants who took part in a follow-up to an epidemiological survey focusing on healthcare impact43 and creativity9. Our aim is to establish a foundation for hypothesis-driven research into the neuropsychological spectrum of PD, with a focus on creativity as a behavioral marker of disease impact, PD treatment, and lifestyle adjustments. By specifically highlighting creative behavior, our study may help inform person-centered care strategies.
Results
Demographics and clinical characteristics are reported in Table 1. Our study involved a final sample of 360 participants (six participants were excluded from analysis due to incomplete questionnaire responses, i.e., not answering for any timepoint). Descriptive statistics and medication are reported in Table S1 in Supplementary Materials. Descriptive statistics of personality trait predictors as well as lifestyle adjustments and drug intake predictors are reported in Table S2 and S3 respectively. The majority of participants (89.25% on average over four items asking about arts training or education, Table S4 in Supplementary Materials) had no formal education in the arts.
Descriptive statistics of reported engagement in creative activities, and changes therein, are reported in Table 2. Each creativity item showed responses across the full range of its respective scale. Participants reported a medium level of creativity before they remembered to notice symptoms (pre-symptomatic). We further observed that the proportion of participants self-reporting changes in creative activity—including both decreases and increases—grew over-time: from 52% at symptom-onset, to 61% post-diagnosis and 71% for current creativity. We further observed decreasing decrease-to-increase ratios (2.42:1 at symptom-onset, 1.91:1 post-diagnosis, 1.54:1 current creativity) suggesting a relative rise in increased creative activity over-time.
Our study cohort showed relatively high levels for agreeableness and conscientiousness, while extraversion and openness were moderate to high44. Neuroticism was lower in comparison to Big Five psychometric norms44, though with more variability among participants. Our cohort exhibits higher levels of negative schizotypy (traits like social withdrawal and anhedonia), while positive schizotypy was less prominent based on the Multidimensional Schizotypy Scale (MSS)-B psychometric norms; disorganized schizotypy was just slightly higher than the reference sample45,46,47.
Results of multivariate regression
The model’s performance was evaluated based on predicting current creativity changes at the time of the survey. The Mean Absolute Error (MAE) for the predictions was 1.48 ± 0.11, with a p-value of less than 0.001 when comparing the obtained MAE to that from shuffled labels, indicating a statistically significant result. The model’s Coefficient of Determination (R²) was 0.23 ± 0.10, with a corresponding p-value also less than 0.001 when compared to shuffled labels, further suggesting the model’s performance was significantly better than chance and indicating that the model explained 23% of the variance considering reported current creativity change.
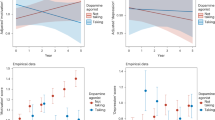
We analyzed the contribution of the individual factors to the model’s performance, i.e., which factors are important to predict changes in creative activity. Figure 1 shows the individual factor importance for predicting creativity change. Figure 2 shows the rank-based predictor importance based on mean SHAP-values for each factor. Plots showing positive or negative association with the experienced creativity change of all significant factors are reported in Figs. S1–S6 in Supplementary Materials. Correlation heatmap is reported in Fig. S7 in Supplementary Materials). Full results, including how each predictor influenced the prediction results are available at our data depository: https://github.com/univiemops/creativity-parkinsons-disease.
Plot displays SHAP values (color code: low = blue, red = high, and showing non-linearity of associations). Note. This SHAP beeswarm plot visually summarizes the influence of predictors on a model’s predictions, illustrating both the magnitude and direction of their contributions. Each dot represents an individual data point, with the x-axis indicating the SHAP value (the predictors contribution to the prediction) and the color denoting the predictor’s value (e.g., blue for low values, red for high values). For the predictor post diagnosis: creativity change, low values (e.g., reduced post-diagnosis: creativity change) correspond to negative SHAP values, indicating a suppressive effect on the prediction of current creativity change. Conversely, high values (e.g., increased post-diagnosis: creativity change) are associated with positive SHAP values, signifying a promotive effect on the prediction.
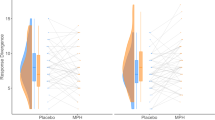
The most important determinant of increased creativity came from the lifestyle adjustment category. Participants who were creatively active after diagnosis showed further increases in current creativity. The second significant factor, from the clinical factor category, was current use of dopamine agonists, which was positively associated with increased creativity. The third and fourth significant determinant, in the lifestyle adjustment category, was increased free time and creativity at symptom onset (where participant likely had not yet taken any medication for PD), again associated with increased creativity. In terms of personality traits, only two factors were significant: higher extraversion was associated with increased creativity, while higher disorganized schizotypy was linked to decreased creativity.
No other personality traits apart from extraversion and disorganized schizotypy contributed significantly to creativity changes. In the lifestyle adjustments category, creatively active before symptoms (pre-symptomatic) showed no significant effect. In the clinical factors, current levodopa, earlier dopaminergic treatments (post-diagnosis), as well as disease stage and cognition showed no significant contributions.
We also analyzed SHAP interaction effects. Some interaction effects were found to be statistically significantly different from interaction effects obtained from models trained with shuffled prediction targets. However, the effect sizes were very small (~0.01) compared to statistically significant main effect sizes (lowest main effect about 10 times bigger than highest interaction effect). Furthermore, after multiple comparison correction no interaction effects remain significant. More details are available online: https://github.com/univiemops/creativity-parkinsons-disease.
Discussion
Our analysis revealed significant contributions to reported current creativity changes in individuals with PD across all three of the selected categories––personality traits, lifestyle adjustments, and clinical factors. We found that engaging in a creative lifestyle after diagnosis, taking dopamine agonists, having increased free time, being creatively active upon noticing symptoms but before receiving a PD diagnosis, and the personality trait extraversion were connected to reported increased creativity. Higher disorganized schizotypy was associated with decreased reported creativity.
Considering our findings in personality traits and current creativity change, we found that extraversion was significantly associated with increased creative activity. The link of extraversion and creativity has been found in prior studies on professional and famous artists, where extreme levels also align with hypomania12,48,49,50. Extraversion’s link to creativity could also be partially attributed to its aspects of novelty seeking, risk-taking, and self-confidence—traits and states that have been connected to heightened dopaminergic activity and specific to hyperdopaminergic behavior within the behavioral spectrum of PD10,19,20,22,51. On the other hand, lower levels of extraversion have been reported in individuals with early PD and prodromal phases, such as those with rapid eye movement sleep behavior disorders27. This variation suggests that decreases and increases in active creative behavior, associated with extraversion levels, could serve as a more person-centered marker for identifying neurological changes linked to both the early stages of PD and response to dopaminergic treatment.
Contrary to established links wherein positive schizotypy correlates with increased creativity and negative schizotypy correlates with decreased creativity31,52, our findings showed that only disorganized schizotypy was associated with decreased creative activity. Even though our findings underscore the need for further research, we want to draw a potential connection between cognitive flexibility and divergent thinking skills necessary for productive creative activity35,53,54. Prior literature suggests that creative cognition is dependent on moderate (but not low or high) levels of striatal and pre-frontal dopamine, which has also been linked to cognitive flexibility, divergent thinking, and problem-solving capabilities21,55. These cognitive attributes appear to be crucial for successful creative behavior (ideation/imagination, production, revision/refinement, and personally useful/socially acceptable products/activities39,55,56,57). In individuals with PD, they have been observed to fluctuate, possibly linked to variations in dopaminergic activity10,21,58,59. The association between disorganized schizotypy and reduced creativity could therefore reflect disruptions in these cognitive processes and neurological balance, which are vital for both generating and executing creative ideas35,54. We acknowledge that more studies remain necessary to explore how disorganized schizotypy affects creative behavior in individuals with PD and its potential links to dopaminergic modulation, before making any further implications.
Our findings in lifestyle adjustments revealed a significant positive association between increased free time and increased creative activity. This finding emphasizes the influence of leisure activities on creativity among individuals with PD, also suggesting that investing in a creative lifestyle might mitigate the disease’s impact on daily life and, potentially increase naturally dopaminergic activity20,21 and consequently well-being18. Regardless, allocating more free time to creative activities post-diagnosis, might well be regarded as another “silver lining” of having received this serious and life-altering diagnosis40.
Interestingly, a pre-symptomatic creative lifestyle did not predict either increased or decreased activity, suggesting that early creative habits alone may not influence how creativity evolve throughout life and later during disease course. However, our results did reveal that creativity tended to change around the time of symptom-onset and increased further after diagnosis, with decreasing decrease-to-increase ratios over-time. These findings may complement recent epidemiological studies that have reported a lower prevalence of PD among individuals in artistic professions later in life13,14. Rather than implying a protective effect of artistic work, these patterns may reflect differences in dopaminergic function prior to diagnosis. For example, sustained artistic engagement in later life may indicate a still-functioning mesolimbic dopaminergic system. This is consistent with findings in nicotine research, where individuals with PD often stop smoking years before motor symptoms due to reduced dopaminergic reward sensitivity60. Similarly, early dopaminergic decline may affect personality traits, such as novelty seeking of artistic drive, influencing career choices long before diagnosis.
Nevertheless, engaging in creative activities after diagnosis may still serve as a valuable coping strategy. Such activities can stimulate neurotransmission and help preserve or strengthen synaptic function in meso-cortical circuits, particularly important in individuals with PD, where dopamine-related cognitive and affective circuits are affected. Tailored programs aligned with personal interests and abilities61,62 may support individuals in maintaining or re-engaging with creative pursuits when other occupational or recreational avenues are no longer feasible24,42.
Among the clinical factors, our findings underscore and align with previous research on the significant influence of current medication intake, rather than long-term or past usage, in changing neuropsychological behavior in PD4,11,12,19,20. In our study, this was particularly evident with dopamine agonists (which have a higher affinity to the mesolimbic dopamine D3 receptors compared to endogenous dopamine synthetized from levodopa) in relation to increased creative activity. These results suggest that adjustments to dopaminergic treatment could have a rather immediate effect on creative behavior, offering a potential person-centered indicator of drug efficacy that might guide dosage modifications to optimize therapeutic outcomes. However, our findings offer significant implications only when considering parallel neuropsychological assessments in PD and within-subject comparisons of experienced creativity change. Currently, few neuropsychological scales consider changes in creative behavior as a marker for medication-induced alterations in behavior. Notably, the Ardouin Scale, which assesses both hyper- and hypodopaminergic behaviors in PD, is one of the few tools that includes creativity as an evaluative component51,63. Within this scale creativity is suggested to be part of impulse control and related disorders that share common underlying mechanisms but needs to be separated from hobbyism and punding using comprehensive clinical criteria51,63,64. Our findings, alongside assessment tools, such as the Ardouin Scale, highlight the need for broader integration of creative behavior and changes thereof into clinical assessments as an important aspect of understanding medication effects in PD management.
Increased creativity related to dopaminergic treatment can result not only from disinhibition of previously existing cognitive abilities (such as high intelligence quotient, working memory skills, cognitive flexibility, divergent thinking) and mood (change towards hypomania), but also from modification in personality traits (such as increased novelty seeking, positive schizotypy) in individuals with PD. Creative activity can only occur in a prepared mind, and dopaminergic neurotransmission, although capable of facilitating creative drive, cannot create creative intelligence but rather impact the three basal ganglia-thalamo-cortical loops by enhancing cortico-cortical associations, bottom-up appetitive drive and decreasing prefrontal top-down behavioral control19,31,50,65,66,67.
The distinct impact of dopamine agonists, predominantly D2/D3 receptor selective (notably, nine out of 101 participants took apomorphine that impacts both D1 direct and D2 indirect dopaminergic pathways, hence acting similar to levodopa), contrasts sharply with the lack of prediction importance of levodopa. This discrepancy raises key questions about the specific neurochemical pathways that modulate creative behavior within the dopaminergic system10,21,68. The currently available dopamine agonists—with the notable exception of apomorphine—have a high affinity to the mesolimbic D3 dopamine receptor, which helps explain their dose-dependent potential to induce impulse control disorder and related disorders65,69. In contrast, the effects of apomorphine and levodopa on these behaviors are more closely tied to sensitization of the dopaminergic system. This sensitization is not merely dose-dependent but also significantly influenced by the severity of the presynaptic dopaminergic neurodegeneration underlying pulsatility of the treatment with levodopa60,70. Apomorphine further contributes to pulsatility due to its pharmacokinetic properties—being lipophilic with rapid resorption after injection into subcutaneous fat, easily crossing the blood brain barrier, and having a short half-life. This pharmacodynamic profile may explain why apomorphine more frequently leads to dopamine dysregulation syndrome, which is thought to result from rapidly induced psychotropic effects mediated in the dopaminergic synapse at the level of the nucleus accumbens71.
In our study, levodopa was not significantly associated with reported changes in creativity. This is likely related to the fact that our sample predominantly included individuals with moderate disease stage and not with advanced PD. Indeed, in populations representative of the general PD population, dopamine agonists are a main risk factor to develop impulse control disorder and related behaviors72. In contrast, in advanced PD populations—particularly those undergoing advanced treatments, such as deep brain stimulation—motor complications and impulse control disorder have been observed even in absence of dopamine agonists4,12. This distinction highlights the importance of disease stage, treatment context, and pharmacological specificity in interpreting the behavioral effects of different dopaminergic therapies.
Our findings raise important ethical considerations in clinical practice. While dopamine agonists may facilitate beneficial changes, such as increased creative engagement, they also carry risks of maladaptive behaviors, including impulse control disorders4,73. Clinicians should therefore evaluate both the therapeutic potential and the neuropsychological side effects of dopaminergic medications, ideally within a framework of shared decision-making, regular behavioral monitoring and expert guided creative engagement when given as a treatment and coping strategy40,62.
A limitation of our study is the retrospective self-reported nature of experiencing changes in creative activities, which may be subject to recall bias and potential anchor effects, particularly given the use of similarly scaled items across different time points. While the outcome and key predictor refer to distinct phases—current engagement and post-diagnosis adjustment—their conceptual proximity may have influenced participants’ responses and affect the reliability of our data. Disease severity and cognition were evaluated using questionnaires assessed through an assessor during the initial baseline PRIME survey43. Gender identity was not included as a predictor in the current model, although exploratory findings in another study from the larger PRIME cohort suggest it may be relevant for future analyses9. Additionally, the use of machine learning models on a rather small sample size may limit the generalizability of our findings. It is crucial to interpret our results within the context of the moderate amount of explained variance and we should remain cautious about extrapolating these findings to the broader PD population without further study.
Despite these limitations, our exploratory and data-driven approach provides a valuable new perspective on neuropsychological phenomena associated with PD. Future research should aim to validate these findings in larger, prospective studies looking at individual changes in creative activities and creative cognition skills from prodromal to early onset and later drug efficacy. Further hypothesis-driven studies could provide new insights to our findings, especially those on personality traits, dopaminergic treatment effects, lifestyle, and creative activity as part of changed neuropsychological behavior. This could further inform the development of diagnostic tools and patient care strategies that incorporate the neuropsychological and creative engagement characteristics of individuals with PD, ultimately contributing to the advancement of person-centered medicine.
Methods
We conducted an exploratory cross-sectional study using self-reported questionnaires to collect data once per participant from March 2021 to March 2022.
Participants
Inclusion criteria comprised a clinical diagnosis of parkinsonism, excluding drug-induced parkinsonism, in patients who had visited a Neurology outpatient clinic at one of the four community hospitals associated with the previously described ‘Proactive and Integrated Management and Empowerment in PD (PRIME Parkinson) healthcare innovation project in the South-East region of the Netherlands43,74. In short, the PRIME Parkinson project consists of the implementation and evaluation of a new care model for people with PD entitled ‘PRIME Parkinson’ care.
Procedure
We invited participants who are enrolled in the PRIME-NL study, which evaluates the new PRIME Parkinson care model43. The PRIME-NL study is coordinated through the Radboudumc (Center of Expertise for Parkinson and Movement Disorders).
Our initial survey study included 793 respondents from 913 participants within the PRIME-NL cohort9,43. Out of these, we invited participants to complete an additional one-time questionnaire on experienced changes in their creativity and associated factors as described in study endpoints between March 2021 to March 2022. Of those who attended the current study, 45.9% reported experiencing a change (increase/decrease), while 54.1% had reported not to have experienced a change in creativity in the initial survey9. Comparisons of invitees and attendees along demographic, lifestyle factors, and healthcare region provided by PRIME Parkinson are provided in Table S5-S7 in Supplementary Materials. Eligible participants received an information letter outlining the study’s background, objectives, and methods. Following this, they had the opportunity to discuss any questions with the researcher to fully understand the implications of their involvement. Those who agreed to participate provided written informed consent. Participants received, based on individual preference, either a digital survey version (SoSci-Survey75) or a paper-pencil version; people were asked to complete the survey within two weeks with two weeks extension in case of request.
Our study was approved by the ethical board METC Oost-Nederland, Radboudumc (CMO file numbers 2021-12985). Participants had to be willing and able to provide written informed consent.
Study endpoints
We developed a predictive model for our dependent variable, termed ‘current creativity change,’’ which reflected self-experienced changes in engaging into creative activities. Participants were asked to consider their momentary (at timepoint of survey) experience, including their creative engagement over the past three months. The possible range of creative activities was explained by providing examples across diverse creative domains, including visual arts, performing arts, literature, and music76. Additionally, we included complementary arts, such as creative cooking, science and technology, handicrafts, interior and garden design, and other practical crafts77 (see for full detail of wording description D1 in Supplementary Materials). This variable was assessed using an 11-point Likert scale, with responses ranging from -5 (strong decrease) to +5 (strong increase), with 0 indicated no change.
We aimed to explore a comprehensive list of potential factors; however, constraints of the data-driven model and the number of eligible participants limited us to including a maximum of twenty independent variables. Therefore, we focused on three key factor categories:
Personality-related factors were represented by eight determinants using two instruments measuring traits. This included the 10-item version of the BIG5 dimensions44 (5-point Likert scale; strongly disagree to strongly agree): (1) openness to experience, (2) conscientiousness, (3) extraversion, (4) agreeableness and (5) neuroticism. We used the Multidimensional Schizotypy Scale (MSS-B)45,46,47 with a binary scale (true, not true) to determine schizotypy along three sub-scales: (6) positive schizotypy (or psychotic-like symptom) dimension is characterized by disruptions in the content of thought, ranging from magical ideation to full-blown delusions, perceptual oddities (including illusions and hallucinations), and suspiciousness/paranoia; (7) negative schizotypy (or deficit) dimension involves a diminution in experiences, encompassing symptoms, such as alogia, anergia, avolition, anhedonia, flattened affect, and disinterest in others and the world; (8) disorganized schizotypy (or cognitive-behavioral disorganization) dimension is characterized by disturbances in the ability to organize and express thoughts and behavior, ranging from mild disruptions in thinking and behavior to formal thought disorder and markedly disorganized actions. Due to the absence of a validated Dutch version, the MSS-B items were translated and back-translated from the original version following the cross-cultural adaptation guidelines78,79.
Lifestyle adjustments was represented by six determinants. Creative lifestyle was assessed for three time points (self-reported, retrospectively, see also Description D1 in Supplementary Materials): (1) pre-symptomatic baseline (assessed whether the participant was creatively active before noticing any symptoms, 11-point Likert scale from 0 = ‘not at all creatively active’’ to 10 = ‘very much creatively active’’), (2) creativity change at symptom onset (examined whether the participant was creatively active upon noticing symptoms but before receiving a PD diagnosis), and (3) creativity change post-diagnosis (evaluated whether the participant to engaged in creative activities after receiving a diagnosis). The last two factors were evaluated on a 11-point Likert scale ranging from -5 (strong decrease) to +5 (strong increase), with 0 indicated no change. Participants were also asked why they believe their creativity had or had not changed, using a binary scale (yes/no). Included factors were that participants experienced a change due to (4) increased free time, (5) personal reactions to living with PD, and (6) caregiver suggested; latter meant that either family/friends or healthcare professional had recommended the person with PD to engage in creative activities.
Clinical factors included six determinants: (1) the disease stage as defined by the Hoehn-Yahr (HY) score and based on six questions from the Movement Disorder Society Unified PD Rating Scale (MDS-UPDRS80) and two self-structured items (see Table S8 for HY-score categorization parameters); (2) cognition was assessed using the short version of the Montreal Cognitive Assessment (MoCA) (MoCA43,81, scale maximum 22 points). Data on disease stage and cognition were assessed by the initial PRIME baseline survey through an assessor43. Finally, dopaminergic treatment was assessed focusing on two self-reported timepoints: (3) post-diagnosis medication (immediately after diagnosis) and (4) current medication (over the past three months at the timepoint of answering the questionnaire). We split the medications further into two categories, (5) levodopa only, and (6) dopamine agonists, with or without levodopa intake (see for drug lists, medication classes, and descriptive statistics Table S1 in Supplementary Materials).
Data analysis: multivariate regression
We adopted an interpretable machine learning-based approach for multivariable statistical analysis82,83. The multivariable statistical regression analyses were conducted using Python v3.11 and the scikit-learn library v1.484. The process involved three main steps: (1) training prediction models, (2) testing generalizability, and (3) analyzing the models.
Prediction Model Training: Gradient Boosted Decision Tree (GBTD) models were chosen for the regression task due to their computational efficiency and high accuracy85,86. GBDT models inherently capture non-linear associations and variable interactions. They are robust against multicollinearity and outliers in the data. The 20 predictors for these models included clinical factors, personality-related factors, and lifestyle adjustments with ‘current creativity change’ serving as the prediction target.
Generalizability Testing: To evaluate the model’s ability to generalize to unknown (out-of-sample) data, a nested cross-validation (CV) procedure was implemented, as recommended by prior research87,88. This procedure involves repeated splits of the data into training and testing sets. In the outer CV loop a 5-folds split scheme grouped by participants was applied repeatedly until a minimum number of 10,000 predictions was reached. Model complexity tuning utilizes a random search scheme to identify well performing complexity parameters (column sample per tree 0.1–1; using extra trees True/False; path smoothing 1–100 log-scale). The performance of each parameter set was assessed in a nested (inner) CV procedure, using training data only. A 5-folds split scheme grouped by participants was applied again and repeated until a minimum number of 1000 predictions was met. The parameter set achieving the highest score was selected and subsequently employed in the model of the main CV loop along with constant parameters (learning rate 0.01; number of leaves 100; number of boosting rounds 1000). Regression performance was measured using prediction coefficient of determination score (prediction R²) and MAE score, while classification performance was evaluated using balanced classification accuracy score89.
Model Analysis: The importance of individual predictors, i.e., the effect on the prediction, was determined using SHapley Additive exPlainations (SHAP), an interpretable machine learning method based on cooperative game theory90,91. SHAP assesses each predictor’s contribution to the model’s performance, providing a detailed analysis of their significance in the regression task.
Data analysis: statistical tests
The assessment of statistical significance for differences between the means of prediction R² metric, prediction accuracy, and the importance of predictors was carried out using a modified paired t-test. It compares the observed values with their counterparts generated under a simulated null-hypothesis, where data labels are subjected to shuffling. To address sample dependence introduced by CV, the t-test was adapted, aligning with the recommendations of prior research92,93. A Bonferroni correction was applied to the t-test results in instances where multiple comparisons were conducted. We provide full access to the data and results: https://github.com/univiemops/creativity-parkinsons-disease.
Sample size considerations
Our study was exploratory, and without a preceding study to guide a power analysis, we opted for a convenience sample. Drawing on prior experience with PRIME-NL participants, we estimated that at least 250 individuals from the available recruitment cohort would participate (comparisons of invitees and attendees along demographic, lifestyle factors, and healthcare region provided by PRIME Parkinson are provided in Table S5–S7 in Supplementary Materials).
Determining an adequate sample size for non-linear machine learning models is challenging, as no established standards exist for high-dimensional, multivariable analyses94. General guidelines suggest requiring 10–20 samples per predictor or a minimum of 50 samples to initiate meaningful machine learning analysis84. Another contentious viewpoint advocates for a minimum of 10–20 samples per degree of freedom (predictor), potentially resulting in a range of 200–400 samples for the current study95,96. Our final dataset included 360 participants, after excluding six cases due to recording issues. This sample size reflects a pragmatic balance between methodological recommendations and resource constraints. Based on a post hoc power analysis, the study achieved a statistical power of 76.4% to detect small effects (Cohen’s d = 0.2) at a significance level of 0.05, which approaches the conventional threshold of 80%.
Data availability
The datasets generated and/or analyzed during the current study are available in the github repository: https://github.com/univiemops/creativity-parkinsons-disease.
References
Steinmetz, J. D. et al. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 23, 344–381 (2024).
Bloem, B. R., Okun, M. S. & Klein, C. Parkinson’s disease. Lancet 397, 2284–2303 (2021).
Kehagia, A. A., Barker, R. A. & Robbins, T. W. Neuropsychological and clinical heterogeneity of cognitive impairment and dementia in patients with Parkinson’s disease. Lancet Neurol. 9, 1200–1213 (2010).
Lamberti, V. M. J. et al. Profile of neuropsychiatric symptoms in Parkinson’s disease: surgical candidates compared to controls. J. Parkinson’s Dis. 6, 133–142 (2016).
Abraham, A. Why the standard definition of creativity fails to capture the creative act. Theory Psychol. 35, 40–60 (2025).
Dietrich, A. Types of creativity. Psychonom. Bull. Rev. 26, 1–12 (2019).
Jung, R. E. & Vartanian, O. The Cambridge Handbook of the Neuroscience of Creativity (Cambridge University Press, 2018).
Sternberg, R. J. Handbook of Creativity (Cambridge University Press, 1999).
Spee, B. T. M. et al. Prevalence of experienced changes in artistic and everyday creativity in people with Parkinson’s disease. npj Parkinsons Dis. 11, 97 (2025).
Spee, B. T. M. et al. Repeating patterns: Predictive processing suggests an aesthetic learning role of the basal ganglia in repetitive stereotyped behaviors. Front. Psychol. 13, 930293 (2022).
Fleury, V. et al. Dopaminergic modulation of emotional conflict in Parkinson’s disease. Front. Aging Neurosci. 6, 164 (2014).
Lhommée, E. et al. Personality, dopamine, and Parkinson’s disease: insights from subthalamic stimulation. Mov. Disord. 32, 1191–1200 (2017).
Darweesh, S. K. L. et al. Professional occupation and the risk of Parkinson’s disease. Eur. J. Neurol. 25, 1470–1476 (2018).
Haaxma, C. A., Borm, G. F., van der Linden, D., Kappelle, A. C. & Bloem, B. R. Artistic occupations are associated with a reduced risk of Parkinson’s disease. J. Neurol. 262, 2171–2176 (2015).
Lauring, J. O. et al. Why would Parkinson’s disease lead to sudden changes in creativity, motivation, or style with visual art?: a review of case evidence and new neurobiological, contextual, and genetic hypotheses, Neuroscience and Biobehavioral Reviews, pp. 129-165 (Elsevier, 2019).
Lauring, J. O. et al. Parkinson’s disease and changes in the appreciation of art: A comparison of aesthetic and formal evaluations of paintings between PD patients and healthy controls. Brain Cogn. 136, 103597 (2019).
Pelowski, M. et al. Can we really ‘read’ art to see the changing brain? A review and empirical assessment of clinical case reports and published artworks for systematic evidence of quality and style changes linked to damage or neurodegenerative disease. Phys. Life Rev. 43, 32–95 (2022).
Bloem, B. R., Pfeijffer, I. L. & Krack, P. Art for better health and wellbeing. BMJ Brit. Med. J. 363, 5353 (2018).
Lhommée, E. et al. Dopamine and the biology of creativity: lessons from Parkinson’s disease. Front. Neurol. 5, 55 (2014).
Maradan-Gachet, M. E., Debove, I., Lhommée, E. & Krack, P. Creativity and Parkinson’s Disease, in: A. Richard, M. Pelowski, B. T. M. Spee (Eds.), Art and Neurological Disorders: Illuminating the Intersection of Creativity and the Changing Brain, pp. 65-89 (Springer International Publishing, 2023).
Boot, N., Baas, M., van Gaal, S., Cools, R. & De Dreu, C. K. W. Creative cognition and dopaminergic modulation of fronto-striatal networks: integrative review and research agenda. Neurosci. Biobehav. Rev. 78, 13–23 (2017).
Béreau, M. et al. Hyperdopaminergic behavioral spectrum in Parkinson’s disease: a review. Rev. Neurologique 174, 653–663 (2018).
Pelowski, M., Spee, B. T. M., Richard, A., Krack, P. & Bloem, B. R. What Parkinson’s reveals about the artistic spark. Am. Sci. 108, 240–244 (2020).
Bloem, B. R. & Volpe, D. What art can tell us about the human brain, in health and disease: comment on “Can we really ‘read’ art to see the changing brain”. Phys. Life Rev. 45, 52–55 (2023).
Menza, M. A., Forman, N. E., Goldstein, H. S. & Golbe, L. I. Parkinson’s disease, personality, and dopamine. J. Neuropsychiatry Clin. Neurosci. 2, 282–287 (1990).
Kaasinen, V. et al. Personality traits and brain dopaminergic function in Parkinson’s disease. Proc. Natl Acad. Sci. 98, 13272–13277 (2001).
Baig, F. et al. Personality and addictive behaviours in early Parkinson’s disease and REM sleep behaviour disorder. Parkinsonism Relat. Disord. 37, 72–78 (2017).
Terracciano, A. et al. Neuroticism and risk of Parkinson’s disease: a meta-analysis. Mov. Disord. 36, 1863–1870 (2021).
Sieurin, J., Zhan, Y., Pedersen, N. L. & Wirdefeldt, K. Neuroticism, smoking, and the risk of Parkinson’s disease. J. Parkinson’s Dis. 11, 1325–1334 (2021).
Thobois, S., Ardouin, C., Lhommée, E. & Krack, P. Non-motor dopamine withdrawal syndrome after surgery for Parkinson’s disease: predictors and underlying mesolimbic denervation. Brain 133, 1111–1127 (2010).
Oehrn, C. R. et al. Schizotypy in Parkinson’s disease predicts dopamine-associated psychosis. Sci. Rep. 11, 1–10 (2021).
Faust-Socher, A., Kenett, Y. N., Cohen, O. S., Hassin-Baer, S. & Inzelberg, R. Enhanced creative thinking under dopaminergic therapy in Parkinson disease. Ann. Neurol. 75, 935–942 (2014).
Bogousslavsky, J. Artistic creativity, style and brain disorders. Eur. Neurol. 54, 103–111 (2005).
Bogousslavsky, J. & Paciaroni, M. Parkinsonism in Poets and Writers. Prog. Brain Res. 206, 59–71 (2013).
Stamatis, C. A. & Weisman de Mamani, A. A latent profile analysis of creativity: associations of convergent and divergent thinking with subclinical schizotypal, obsessive-compulsive, and affective symptoms. Psychol. Aesthet. Creativity, Arts 16, 651–664 (2022).
Jamison, K. R. Mood disorders and patterns of creativity in British writers and artists. Psychiatry 52, 125–134 (1989).
Mohammadi, D. Nancy C Andreasen: creativity and mental illness. Lancet Psychiatry 4, 192 (2017).
Jamison, K. R. Touched with fire: Manic-depressive illness and the artistic temperament (Simon and Schuster, 1996).
Eysenck, H. J. Creativity as a product of intelligence and personality, International handbook of personality and intelligence pp. 231-247 (Springer, 1995).
Alonso-Canovas, A. et al. The silver linings of Parkinson’s disease. npj Parkinson’s Dis. 8, 21–21 (2022).
Stap, T. B. et al. Holding Still, Together: Person-Centered Parkinson’s Care Portrayed, in: A. Richard, M. Pelowski, B. T. M. Spee (Eds.), art and neurological disorders: illuminating the intersection of creativity and the changing brain pp. 197-214 (Springer International Publishing, 2023).
Gros, P., Spee, B. T. M., Bloem, B. R. & Kalia, L. V. If art were a drug: implications for Parkinson’s disease. J. Parkinson’s Dis. 24, 159–172 (2024).
Ypinga, J. H. L. et al. Rationale and design to evaluate the PRIME Parkinson care model: a prospective observational evaluation of proactive, integrated and patient-centred Parkinson care in The Netherlands (PRIME-NL). BMC Neurol. 21, 286–286 (2021).
Rammstedt, B. & John, O. P. Measuring personality in one minute or less: a 10-item short version of the big five inventory in english and german. J. Res. Personal. 41, 203–212 (2007).
Gross, G. M., Kwapil, T. R., Raulin, M. L., Silvia, P. J. & Barrantes-Vidal, N. The multidimensional schizotypy scale-brief: Scale development and psychometric properties. Psychiatry Res. 261, 7–13 (2018).
Kemp, K. C., Bathery, A. J., Barrantes-Vidal, N. & Kwapil, T. R. A brief questionnaire measure of multidimensional schizotypy predicts interview-rated symptoms and impairment. PLOS ONE 15, e0237614–e0237614 (2020).
Kwapil, T. R., Gross, G. M., Silvia, P. J., Raulin, M. L. & Barrantes-Vidal, N. Development and psychometric properties of the Multidimensional Schizotypy Scale: A new measure for assessing positive, negative, and disorganized schizotypy. Schizophrenia Res. 193, 209–217 (2018).
Eysenck, H. J. Genius: A Natural History of Creativity (Cambridge University Press, 1995).
Furnham, A. Personality and Creativity, O Perceptual and Motor Skills, pp. 407-408 (Sage, 1999).
Greenwood, T. A., Chow, L. J., Gur, R. C. & Kelsoe, J. R. Bipolar spectrum traits and the space between madness and genius: the muse is in the dose. J. Psychiatr. Res. 153, 149–158 (2022).
Ardouin, C. et al. Évaluation des troubles comportementaux hyper- et hypodopaminergiques dans la maladie de Parkinson. Rev. Neurologique 165, 845–856 (2009).
Nettle, D. Schizotypy and mental health amongst poets, visual artists, and mathematicians. J. Res. Personal. 40, 876–890 (2006).
Beaty, R. E. & Kenett, Y. N. Associative thinking at the core of creativity. Trends Cogn. Sci. 27, 671–683 (2023).
Polner, B., Nagy, H., Takáts, A. & Kéri, S. Kiss of the muse for the chosen ones: de novo schizotypal traits and lifetime creative achievement are related to changes in divergent thinking during dopaminergic therapy in Parkinson’s disease. Psychol. Aesthet., Creativity, Arts 9, 328–339 (2015).
Beaty, R. E., Benedek, M., Silvia, P. J. & Schacter, D. L. Creative Cognition and Brain Network Dynamics, Trends in Cognitive Sciences, pp. 87-95 (Elsevier, 2016).
Baer, J. Creativity and Divergent Thinking (Psychology Press, 2014).
Spee, B. T. M. et al. Machine learning revealed symbolism, emotionality, and imaginativeness as primary predictors of creativity evaluations of western art paintings. Sci. Rep. 13, 12966 (2023).
Cools, R. et al. Smulders, M.H.M. Timmer, Role of dopamine and clinical heterogeneity in cognitive dysfunction in Parkinson’s disease. Prog. Brain Res. 269, 309–343 (2022).
Tichelaar, J. G., Sayalı, C., Helmich, R. C. & Cools, R. Impulse control disorder in Parkinson’s disease is associated with abnormal frontal value signalling. Brain 146, 3676–3689 (2023).
Amstutz, D. et al. Psychiatric and cognitive symptoms of Parkinson’s disease: A life’s tale. Rev. Neurologique 181, 265–283 (2024).
Spee, B. T. M. et al. Unleashing creativity in people with Parkinson’s disease: a pilot study of a co-designed creative arts therapy. J. Neurol. 272, 161 (2025).
Spee, B. T. M. et al. Co-creating a person-centered creative engagement intervention for Parkinson’s care. Front. Psychol. 15, 1469120 (2025).
Rieu, I. et al. International validation of a behavioral scale in Parkinson’s disease without dementia. Mov. Disord. 30, 705–713 (2015).
Evans, A. H. et al. Scales to assess impulsive and compulsive behaviors in Parkinson’s disease: critique and recommendations. Mov. Disord. 34, 791–798 (2019).
Sierra, M. et al. Apathy and impulse control disorders: yin & yang of dopamine dependent behaviors. J. Parkinson’s Dis. 5, 625–636 (2015).
Carson, S. H. Creativity and psychopathology: a shared vulnerability model. Can. J. Psychiatry 56, 144–153 (2011).
Bódi, N. et al. Reward-learning and the novelty-seeking personality: a between-and within-subjects study of the effects of dopamine agonists on young Parkinson’s patients. Brain 132, 2385–2395 (2009).
Cools, R. Dopaminergic modulation of cognitive function-implications for l-DOPA treatment in Parkinson’s disease. Neurosci. Biobehav. Rev. 30, 1–23 (2006).
Debove, I. et al. Management of impulse control and related disorders in Parkinson’s disease: an expert consensus. Mov. Disord. 39, 235–248 (2024).
Weiss, D. et al. Changing gears - DBS for dopaminergic desensitization in Parkinson’s disease? Ann. Neurol. 90, 699–710 (2021).
Delpont, B. et al. Psychostimulant effect of dopaminergic treatment and addictions in Parkinson’s disease. Mov. Disord. 32, 1566–1573 (2017).
Weintraub, D. & Claassen, D. O. Impulse control and related disorders in Parkinson’s disease. Int. Rev. Neurobiol. 133, 679–717 (2017).
Claassen, D. O. et al. The risky business of dopamine agonists in Parkinson disease and impulse control disorders. Behav. Neurosci. 125, 492 (2011).
Bloem, B. R. et al. Integrated and patient-centred management of Parkinson’s disease: a network model for reshaping chronic neurological care. Lancet Neurol. 19, 623–634 (2020).
Leiner, D. J. SoSci Survey (Version 3.2.43) [Computer Software], http://www.soscisurvey.com, 2018.
Benedek, M., Bruckdorfer, R. & Jauk, E. Motives for creativity: exploring the what and why of everyday creativity. J. Creative Behav. 54, 610–625 (2020).
Cousins, E.,Tischler, V., Garabedian, C. & Dening, T. A Taxonomy of arts interventions for people with dementia. Gerontologist 60, 124–134 (2019).
Sousa, V. D. & Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J. Evaluation Clin. Pract. 17, 268–274 (2011).
Beaton, D. E., Bombardier, C., Guillemin, F. & Ferraz, M. B. Guidelines for the process of cross-cultural adaptation of self-report measure. Spine 25, 3186–3191 (2000).
Goetz, C. G. et al. Movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov. Disord. 23, 2129–2170 (2008).
Nasreddine, Z. S. et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatrics Soc. 53, 695–699 (2005).
Qiu, W. et al. Interpretable machine learning prediction of all-cause mortality. Commun. Med. 2, 125 (2022).
Dwyer, D. B., Falkai, P. & Koutsouleris, N. Machine learning approaches for clinical psychology and psychiatry. Annu. Rev. Clin. Psychol. 14, 91–118 (2018).
Pedregosa, F. et al. Duchesnay, scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Ke, G. et al. Lightgbm: A highly efficient gradient boosting decision tree. Adv. neural Inf. Process. Syst., Adv. neural Inf. Process. Syst. 30, 3146–3154 (2017).
Grinsztajn, L., Oyallon, E. & Varoquaux, G. Adv. Neural Inf. Process. Syst. 35, 507–520 (2022).
Cawley, G. C. & Talbot, N. L. C. On over-fitting in model selection and subsequent selection bias in performance evaluation. J. Mach. Learn. Res. 11, 2079–2107 (2010).
Rosenberg, M. D. & Finn, E. S. How to establish robust brain–behavior relationships without thousands of individuals. Nat. Neurosci. 25, 835–837 (2022).
Hastie, T. Tibshirani, R. & Friedman, J. The Elements of Statistical Learning Data Mining, Inference, and Prediction, 2nd ed. (Springer, 2016).
Lundberg, S. M. & Lee, S.-I. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst., Adv. Neural Inf. Process. Syst. 30, 4765–4774 (2017).
Molnar, C. Interpretable machine learning. A Guide for Making Black Box Models Explainable, https://christophm.github.io/interpretable-ml-book/, (2019).
Bouckaert, R. R. & Frank, E. Evaluating the Replicability of Significance Tests for Comparing Learning Algorithms, pp. 3-12 (Springer, 2004).
Nadeau, C. Inference for the generalization error. Mach. Learn., Mach. Learn. 52, 239–281 (2003).
Rosenbusch, H., Soldner, F., Evans, A. M. & Zeelenberg, M. Supervised machine learning methods in psychology: a practical introduction with annotated R code. Soc. Pers. Psychol. Compass 15, e12579 (2021).
Riley, R. D. et al. Minimum sample size for developing a multivariable prediction model: PART II - binary and time-to-event outcomes. Stat. Med. 38, 1276–1296 (2019).
Vittinghoff, E. & McCulloch, C. E. Relaxing the rule of ten events per variable in logistic and cox regression. Am. J. Epidemiol. 165, 710–718 (2007).
Acknowledgements
The study was conducted during a scholarship to BTM.S., supported by the Österreichischer Austauschdienst (OeAD), Mariette Blau Scholarship. This research was funded in part by the Austrian Science Fund (FWF) #ConnectingMinds under grant agreement number CM 1100-B with the short title: Unlocking the Muse, available via https://www.fwf.ac.at/en/discover/research-radar. The study funders and sponsors were not involved in the study design, the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.This research is supported by the Proactive and Integrated Management and Empowerment in PD (PRIME) project, which was funded by the Gatsby Foundation [GAT3676] as well as by the Ministry of Economic Affairs by means of the PPP Allowance made available by the Top Sector Life Sciences & Health to stimulate public-private partnerships. The Center of Expertise for Parkinson and Movement Disorders was supported by a center of excellence grant by the Parkinson Foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed to writing the manuscript. S.Z. and B.T.M.S. wrote first manuscript draft. B.T.M.S., S.D., M.J.M., and M.P. designed the study. B.T.M.S., M.P., S.D., J.S.C., and B.R.B. supervised the study. P.K. provided expertise in personality and neuropsychology. B.T.M.S. and M.J.M. developed questionnaire. S.Z. and B.T.M.S. conducted the data collection and pre-processed the dataset. D.S. conducted the analysis. B.T.M.S. and D.S. prepared all figures and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Prof. Bloem serves as the co-Editor in Chief for the Journal of PD, serves on the editorial board of Practical Neurology and Digital Biomarkers, has received fees from serving on the scientific advisory board for the Critical Path Institute, Gyenno Science, MedRhythms, UCB, Kyowa Kirin and Zambon (paid to the Institute), has received fees for speaking at conferences from AbbVie, Bial, Biogen, GE Healthcare, Oruen, Roche, UCB and Zambon (paid to the Institute), and has received research support from Biogen, Cure Parkinson’s, Davis Phinney Foundation, Edmond J. Safra Foundation, Fred Foundation, Gatsby Foundation, Hersenstichting Nederland, Horizon 2020, IRLAB Therapeutics, Maag Lever Darm Stichting, Michael J Fox Foundation, Ministry of Agriculture, Ministry of Economic Affairs & Climate Policy, Ministry of Health, Welfare and Sport, Netherlands Organization for Scientific Research (ZonMw), Not Impossible, Parkinson Vereniging, Parkinson’s Foundation, Parkinson’s UK, Stichting Alkemade-Keuls, Stichting Parkinson NL, Stichting Woelse Waard, Topsector Life Sciences and Health, UCB, Verily Life Sciences, Roche and Zambon. Prof. Bloem does not hold any stocks or stock options with any companies that are connected to PD or to any of his clinical or research activities. BTM.S. is funded as postdoc by the Austrian Science Fund (FWF – Der Wissenschaftsfonds), #ConnectingMinds under grant agreement number CM 1100-B with the short title: Unlocking the Muse. All other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zeggio, S., Steyrl, D., Pelowski, M. et al. Neuropsychological insights into creativity in people with Parkinson’s disease. npj Parkinsons Dis. 11, 324 (2025). https://doi.org/10.1038/s41531-025-01165-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01165-y