Abstract
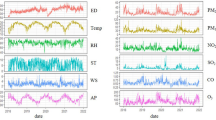
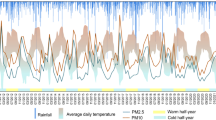
Background: Tropospheric ozone (O₃) is a secondary air pollutant associated with respiratory morbidity. Lleida is an inland Mediterranean city with a continentalized climate, frequent winter thermal inversions and hot, dry summers, where ozone episodes and high humidity often co-occur under stagnant atmospheric conditions. This study explores the association between air pollutants, weather variables, and respiratory emergency admissions in Lleida, Spain. Methods: We conducted a time-series analysis using distributed lag non-linear models (DLNM) on hospital emergency room admissions for acute respiratory conditions in Lleida (2010–2019). Data on weather (temperature, humidity, solar radiation) and air pollution (O₃, NO₂, PM10, SO₂) were obtained from local monitoring stations. The primary outcome was the daily number of admissions for respiratory conditions (ICD-10 codes J09–J18, J20–J22, J44.1, J45.9). Results: A total of 19,428 respiratory admissions were recorded. High O₃ concentrations and elevated relative humidity were significantly associated with increased admissions, even after adjusting for temperature and solar radiation. The strongest effects were observed with delayed lags (up to 21 days). NO₂, PM10, CO and SO₂ levels did not show a significant association. Conclusions: Our findings support a significant and independent association between elevated ozone concentrations, high humidity, and respiratory emergencies. These results highlight the need for public health strategies and policy interventions focused on environmental risk forecasting and air quality management, particularly in vulnerable inland Mediterranean regions.
Similar content being viewed by others
Data Availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at IRBLLEIDA.
References
Romanello, M. et al. The 2024 report of the Lancet Countdown on Health and Climate Change. Lancet 404, 1847–1896 (2024).
Intergovernmental Panel on Climate Change (IPCC). Summary for Policymakers: Land Use, Land-Use Change, and Forestry. 2000.
Ministerio para la Transición Ecológica. Plan Nacional del Aire 2017–2019. Gobierno de España.
Brunekreef, B. & Holgate, S. T. Air pollution and health. Lancet. 360, 1233–1242 (2002).
World Health Organization. Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Global update 2005. WHO; 2006.
Pope, C. A. III & Dockery, D. W. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc. 56, 709–742 (2006).
World Health Organization. 7 million premature deaths annually linked to air pollution. WHO News Release, 25 March (2014). Available from: https://www.who.int/news/item/25-03-2014-7-million-premature-deaths-annually-linked-to-air-pollution.
Impacto de la contaminación atmosférica en la frecuencia de enfermedades cardiovasculares, cerebrovasculares y respiratorias. South Florida J Dev. 2021;2:1897–1914.
Díaz, J. et al. Short-term effects of particulate matter concentration on hospital admissions in the over-75 age group in Madrid, Spain. Public Health 124, 28–36 (2010).
Künzli, N. et al. Public-health impact of outdoor and traffic-related air pollution: a European assessment. Lancet. 356, 795–801 (2000).
Alari, A. et al. Long-term exposure to air pollution and lower respiratory infections in a large adult cohort in Catalonia. Environ Int. 195, 109230 (2025).
Restrepo-Arango, M., Vélez-Pélaez, M., Vallejo-Agudelo, E. & Martínez-Sánchez, L. Impacto clínico de la contaminación aérea. Arch Med (Manizales) 16, 373–384 (2016).
Saygin, H., Mercan, Y. & Yorulmaz, F. The association between air pollution and emergency visits for cardiovascular and respiratory diseases: a time-series analysis. Int Arch Occup Environ Health 95, 599–606 (2022).
Ballester, F. Contaminación atmosférica, cambio climático y salud. Rev Esp Salud Publica. 79, 2 (2005).
Generalitat de Catalunya. Inventari d’emissions atmosfèriques del sector agrari i fonts naturals. 2021.
Generalitat de Catalunya. Inventory of atmospheric emissions from the agricultural sector and natural sources in Catalonia for the years 2019 and 2021. Department of Territory, Housing and Ecological Transition; March 2024. (In Catalan).
Martínez-Solanas, È & Basagaña, X. Temporal changes in the effects of ambient temperatures on hospital admissions in Spain. PLoS One 14, e0218262, https://doi.org/10.1371/journal.pone.0218262 (2019).
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/.
Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw. 2011
Tenías, J. M. et al. Air pollution and ER admissions for COPD in Valencia, Spain. Arch Environ Health 57, 41–47 (2002).
Cirera, L. et al. Daily effects of air pollutants on asthma and COPD ER visits in Cartagena (Spain). Allergol Immunopathol (Madr) 40, 231–237 (2012).
D’Amato, G. et al. Effects of climate change on respiratory allergy and asthma induced by pollen and outdoor molds. Allergy. 70, 1407–1419 (2015).
Ruiz-Páez R. et al. Short-term effects of chemical and noise pollution during heat and cold waves on emergency hospital admissions in Madrid. Int J Biometeorol. https://doi.org/10.1007/s00484-025-02963-y (2025).
Liu, C. et al. Global association between ambient ozone and cause-specific mortality: a systematic review and meta-analysis. Lancet Planet Health 4, e132–e142 (2020).
Linares, C. et al. Heat exposure and cause-specific hospital admissions in Spain: a nationwide cross-sectional study. Environ Health Perspect 131, 047010 (2023).
Baldasano, J. M. et al. Air quality in the Ebro Valley: characterization of ozone episodes. Atmos Res. 145–146, 58–70 (2014).
Stafoggia, M. et al. Short-term associations between ozone and mortality in 25 Italian cities: the EpiAir study. Environ Health Perspect 118, 1239–1245 (2010). Percent refered to admissions at the median value of the exposure variable.
Acknowledgements
No funds were received for that research.
Author information
Authors and Affiliations
Contributions
MM and CL wrote the main manuscript text and MM prepared the figures. EJ and JO collected all the data and created the database. OY reviewed all the project. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
CONSENT FOR PUBLICATION
This manuscript does not contain any individual person’s data in any form (including individual details, images, or videos), and therefore consent for publication is not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Llobet, C., Martinez-Alonso, M., Justribó, E. et al. Environmental Drivers of Respiratory Emergency Admissions: The Role of Tropospheric Ozone and Humidity in Lleida, Spain (2010–2019). npj Prim. Care Respir. Med. (2026). https://doi.org/10.1038/s41533-026-00479-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-026-00479-5