Abstract
Proximity barcoding assay, a high-throughput method for single-exosome analysis, was employed to profile surface proteins on individual exosomes of SCZ patients. This analysis identified five differentially expressed proteins (DEPs) between SCZ patients and healthy controls (HC) and six DEPs between antipsychotic responders and non-responders. Furthermore, two exosome clusters were found to be associated with SCZ, and certain DEPs were correlated with cognitive functions.
Similar content being viewed by others
Introduction
Schizophrenia (SCZ) is a severe psychiatric disorder affecting approximately 1% of the global population, leading to an average potential life loss of about 14.5 years1. Early diagnosis and intervention can improve patient outcomes2. However, the diagnosis of SCZ currently relies on the subjective assessment and judgment of psychiatrists and lacks objective biomarkers. Additionally, the efficacy of antipsychotic medications varies among individuals, with approximately 40% of patients exhibiting poor response and being classified as having refractory schizophrenia3. Exosomes have garnered considerable attention due to their distinctive physiological functions4. Furthermore, exosomes participate in several physiological mechanisms closely associated with SCZ, including cell communication5, regulation of synaptic plasticity, and nerve regeneration processes6. Previous studies investigating exosomes in SCZ have primarily examined bulk exosomes rather than individual exosomes. In this study, we employed the proximity barcoding assay (PBA)7, an innovative high-throughput method for single-exosome analysis, to simultaneously profile 256 surface proteins, encompassing markers of exosomes and proteins associated with nervous system, immunity, tumors, cardiovascular diseases, and other conditions8,9, on individual exosomes of antipsychotic responders (RES) and non-responders (NRES).
Methods
The study was approved by the Medical Ethics Committee of the second Xiangya Hospital and written informed consent was obtained from all participants. Patients (n = 50) with first-episode SCZ underwent cognitive function assessments and provided plasma samples at baseline and then received risperidone for a duration of 3 months. Following this treatment period, participants were classified as either RES (reduction rate > 50%) or NRES based on the PANSS. Plasma exosomes from bottom 10 NRES and top 10 RES, as well as 10 matched healthy controls (HCs), were used for PBA. Details of PBA was provided in Supplement methods. To prioritize reliable proteins relevant to SCZ, we filtered the differential expressed proteins (DEPs) using two criteria: first, the protein expression was 1.5 folds or higher in the SCZ (NRES) compared to the HC (RES) group, and second, the protein or gene had been previously associated with schizophrenia in the published literature.
Results
The participants in our study included RES (n = 10), NRES (n = 10), and healthy controls (HC, n = 10). There was no difference in total PANSS scores or PANSS positive symptom scores between the RES and NRES at baseline (Table S2).
We first compared exosomes protein expression among SCZ patients, including both RES and NRES, and HC. Total protein expression and the average expression of proteins on extracellular vesicles (EVs) showed no difference (Fig. S1C–E). In differential protein analysis, 52 surface proteins exhibited significant differences (Table S3). After further filtering with criteria in methods, five DEPs remained: FN1, ITGB3, PECAM1, ITGA6, and CD5 (Fig. S1I). These proteins demonstrated an area under the curve (AUC) of up to 0.805 in ROC analysis for distinguishing SCZ from HC (Fig S2A–E).
Furthermore, we examined protein expression between RES and NRES groups. Both total protein expression and average EV protein expression showed no difference between RES and NRES (Fig. S1F–H). When it comes to individual proteins, 18 exhibited significant differences (Table S4). After further filtering, six DEPs—ITGB3, CD33, CD40, CD36, TENM2, and EGFR—met our criteria (Fig. S1J) with an AUC of up to 0.87 in discriminating between RES and NRES(Fig. S2F–L).
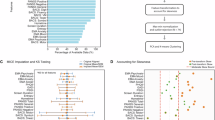
To classify exosomes based on proteomic characteristics, an unsupervised machine learning algorithm, FlowSOM10, was applied to generate exosome clusters. The t-SNE plot in Fig. 1A displays the clustering of exosomes from all samples, revealing 13 identified clusters through FlowSOM. Fig, 1B depicts the biomarkers of each cluster. Next, we analyzed the similarities and differences among the RES, NRES, and HC groups (Fig. 1C, D). Among all clusters, cluster 12 exhibited an increasing trend in proportion in SCZ, from 8.48% in the HC to 13.27% in NRES and 20.16% in RES (P = 0.037 for SCZ and HC, P = 0.003 for NRES and RES, Fig. 1F). DEPs ITGB3, PECAM1, and ITGA6 are predominantly expressed in cluster 12, suggesting an association of cluster 12 with SCZ and antipsychotic effectiveness. The proportion of cluster 11 also showed an increasing trend in SCZ, rising from 3.57% in the HC group to 7.05% in the SCZ group (P = 0.031), with no significant difference between RES and NRES (Fig. 1E). Since DEPs PECAM1, and ITGA6 are also predominantly expressed in cluster 11, cluster 11 may also be associated with SCZ.
A Exosome subpopulations from plasma samples of both SCZ patients and healthy donors were determined via the FlowSOM algorithm, an unsupervised machine learning process. Thirteen subpopulations were shown in t-distributed stochastic neighbor embedding (t-SNE) plot. B Proteomic biomarkers of each subpopulation were shown in heatmap. C The distribution of exosomes among each subpopulation was displayed for each sample group, including HC, RES and NRES groups. D t-SNE plot for each sample with group information. E, F Cluster 11 and 12 featured expressing PECAM1, ITGA6 and ITGB3 increased significantly in SCZ group, furthermore, cluster 12 increased in NRES group compared to RES. Data represent the mean ± SD, Statistical analyses were performed using the t test, n = 10 for HC, RES and NRES, n = 20 for SCZ. *P < 0.05; **P < 0.01.
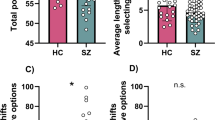
To investigate whether exosomes-expressed these surface proteins were correlated with cognitive functions, we assessed the cognitive functions of individuals with SCZ and HC (Table S5) and performed correlation analysis DEPs and cognitive functions (Fig. 2). For DEPs between SCZ and HC, FN1 was positively correlated with completion time of TMTB (r = −0.67 P = 0.004514) and SCWT-A (r = −0.669 P = 0.004514) after FDR correction. For DEPs between NRES and RES, correlations were not significant after FDR correction.
For DEPs between SCZ and HC, PECAM1, ITGB3, ITGA6 and FN1 were negatively correlated with scores on BACS-SC, BVMT-R, and CF; Additionally, PECAM1 was negatively correlated with scores on HVLT-R and positively correlated with the time taken for TMTB and SCWT-A; ITGA6 was negatively correlated with accuracy of CPT-Hearing; FN1 was positively correlated with completion time of CPT-Version, TMTA, TMTB and SCWT; CD5 was positively correlated with completion time of TMTB and SCWT-B. For DEPs between NRES and RES, CD33 was negatively correlated with score of HVLT-R, maze task and BVMT-R; CD40 was negatively correlated with score of HVLT-R, BASC-SC and BVMT-R; TENM2 was negatively correlated with WMS-III parallel and total score; *P < 0.05; **P < 0.01; ***P < 0.001.
Discussion
Our results reveal differences in the expression of proteins, including FN1, ITGB3, PECAM1, ITGA6, and CD5, on single exosomes between SCZ patients and healthy controls. Similarly, differences were observed in the expression of proteins ITGB3, CD33, CD40, CD36, TENM2, and EGFR between RES and NRES patients. ROC analysis demonstrated their potential as biomarkers for distinguishing SCZ from healthy controls or NRES from RES. Moreover, the proportion of exosome subpopulations expressing PECAM1, ITGA6, ITGB3, and ITGB1 increased in the total plasma exosomes of SCZ patients, particularly in those who were responsive to treatment (RES). Additionally, DEPs including PECAM1, ITGA6, ITGB3 and FN1 were found to be correlated with cognitive function.
Exosomal surface proteins reflect the characteristics of their respective cells and tissues11, indicating that increased expression of these proteins reflects heightened cellular and tissue activities and communication. The increased expression of FN1 may contribute to the transformation of vascular smooth muscle cells in intimal thickening of atherosclerotic lesions12, while PECAM1 is associated with endothelial cell function13. Morris et al.13 have shown that endothelial dysfunction is caused by inflammation, oxidative stress, and mitochondrial dysfunction, all of which play significant roles in the pathology of SCZ. Previous studies indicate that patients with SCZ face a substantially higher risk of cardiovascular disease (CVD) compared to the general population14. FN1 and PECAM1 may contribute to the heightened risk of CVD in SCZ patients. Both ITGA6 and ITGB3 are integrin components involved in mediating cell-matrix and cell-cell adhesion processes15. Integrin β has been found to play a crucial role in synapses, with β3 influencing synaptic strength by regulating the magnitude size and content of excitatory synaptic transmission15. Additionally, β3 integrins are necessary for homeostatic plasticity, a type of synaptic plasticity16. Simultaneously, ITGA6 may be associated with neuronal migration17. Besides, ITGB1, which has not been directly reported to be associated with SCZ but is found to be highly expressed in SCZ group in the present study, is essential for synapse formation18. This suggests that ITGB3, ITGA6, and ITGB1 could play roles in the neurodevelopmental processes and synapses function of SCZ. CD5 is an immune-associated protein expressed on both T cells and B cells. Printz et al.19 demonstrated the elevation of CD5 + B lymphocytes in SCZ patients, which may be the origin of the highly expressed CD5+ exosomes observed in this study.
We also identified 6 DEPs ITGB3, CD33, CD40, CD36, TENM2, and EGFR between RES and NRES. ITGB3, which was also differentially expressed between SCZ patients and HC, was found to be expressed at lower levels in NRES. As mentioned earlier, ITGB3 influences synaptic function. Synaptic dysfunction mediated by low ITGB3 may result in a weak response to drugs. CD33, CD40, and CD36 are immune-related proteins. Both CD3320 and CD4021 were found to be elevated in SCZ patient, induced by pro-inflammation factors and microglia activation22. Lower levels of CD33 and CD40 found in NRES may indicate suppressed microglial activation, suggesting that microglial may play a role in the prognosis of SCZ. Tomasik et al.23 found that monocyte CD36 levels could serve as a reliable indicator of response to olanzapine treatment. They demonstrated that patients with high CD36 expression on monocytes were less likely to respond to olanzapine, consistent with our finding that NRES patients had higher CD36 levels. TENM2, an adhesion molecule highly expressed in neurons, plays a critical role in neural migration24 and intracellular calcium signaling25 and has been proposed as a SCZ-related gene26. EGFR, the receptor of epidermal growth factor, is distributed across cell populations involved in SCZ neuropathology, including GABAergic and dopaminergic neurons27. Postmortem studies have revealed up-regulation of EGFR protein in the forebrain regions of patients with SCZ28. Animal studies have demonstrated that EGFR activation in the brain leads to dopamine release in the striatum or globus pallidus, resulting in behavioral impairments relevant to SCZ29,30,31. Moreover, epidermal growth factor negatively regulates GABAergic development in the neocortex32.
Our findings suggested that DEPs on exosomes are correlated with cognitive functions, particularly those distinguishing SCZ from HC. Exosomes originating from the brain can traverse the blood–brain barrier and be identified in plasma4. On the other hand, elevated levels of cell adhesion proteins are linked with increased cerebrovascular resistance33, potentially leading to reduced blood flow in watershed areas of the brain, resulting in ischemic damage to regions controlling motor function and attention34.
There were several limitations in our study. Firstly, we analyzed plasma samples from a limited pool of 30 individuals, which may have excluded certain biomarkers and obscured correlations between proteins and cognitive functions after FDR correction. Secondly, we did not validate the identified surface proteins using an independent cohort. This was due to the limited number of NRES in our cohort, making it insufficient to establish an independent cohort for validation. Lastly, Lastly, the pathophysiological function of these exosome-expressed DEPs in schizophrenia remains unclear. Therefore, future studies are needed to validate the results in a larger cohort and explore the specific roles these proteins play in schizophrenia.
In conclusion, we utilized a novel single-exosome analysis method, PBA, to profile the expression features of exosome surface proteins in the plasma of SCZ patients. We identified differentially expressed surface proteins in single exosomes and evaluated their diagnostic and prognostic capacities using ROC analysis. Additionally, we observed alterations in exosome subpopulations among RES patients, NRES patients, and the HC group, identifying two subpopulations characterized by the expression of PECAM1, ITGB3, ITGA6, and ITGB1 associated with SCZ. Further research is warranted to validate these potential biomarkers and elucidate their roles in schizophrenia.
Data availability
All data associated with this study are shown in the manuscript, Supplementary materials, and Source Data file. Source data are provided with this paper.
References
Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
Chang, Q. et al. Suicide ideation, suicide attempts, their sociodemographic and clinical associates among the elderly Chinese patients with schizophrenia spectrum disorders. J. Affect. Disord. 256, 611–617 (2019).
Orsolini, L. et al. An update of safety of clinically used atypical antipsychotics. Expert. Opin. Drug Saf. 15, 1329–1347 (2016).
Wang, Y., Amdanee, N. & Zhang, X. Exosomes in schizophrenia: pathophysiological mechanisms, biomarkers, and therapeutic targets. Eur. Psychiatry 65, e61 (2022).
Vella, L. J. et al. Packaging of prions into exosomes is associated with a novel pathway of PrP processing. J. Pathol. 211, 582–590 (2007).
György, B. et al. Membrane vesicles, current state-of-the-art: emerging role of extracellular vesicles. Cell Mol. Life Sci. 68, 2667–2688 (2011).
Wu, D. et al. Profiling surface proteins on individual exosomes using a proximity barcoding assay. Nat. Commun. 10, 3854 (2019).
Guo, W. et al. Single-Exosome Profiling Identifies ITGB3+ and ITGAM+ exosome subpopulations as promising early diagnostic biomarkers and therapeutic targets for colorectal cancer. Research 6, 0041 (2023).
Sun, R. et al. Proteomic profiling of single extracellular vesicles reveals colocalization of SARS-CoV-2 with a CD81/integrin-rich EV subpopulation in sputum from COVID-19 severe patients. Front. Immunol. 14, 1052141 (2023).
Van Gassen, S. et al. FlowSOM: using self-organizing maps for visualization and interpretation of cytometry data. Cytometry A 87, 636–645 (2015).
Larssen, P. et al. Tracing cellular origin of human exosomes using multiplex proximity extension assays. Mol. Cell Proteom. 16, 502–511 (2017).
Magnusson, M. K. & Mosher, D. F. Fibronectin: structure, assembly, and cardiovascular implications. Arterioscler Thromb. Vasc. Biol. 18, 1363–1370 (1998).
Morris, G. et al. Endothelial dysfunction in neuroprogressive disorders-causes and suggested treatments. BMC Med. 18, 305 (2020).
Correll, C. U. et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 16, 163–180 (2017).
Pozo, K. et al. β3 integrin interacts directly with GluA2 AMPA receptor subunit and regulates AMPA receptor expression in hippocampal neurons. Proc. Natl Acad. Sci. USA 109, 1323–1328 (2012).
Cingolani, L. A. & Goda, Y. Differential involvement of beta3 integrin in pre- and postsynaptic forms of adaptation to chronic activity deprivation. Neuron Glia Biol. 4, 179–187 (2008).
Anton, E. S., Kreidberg, J. A. & Rakic, P. Distinct functions of alpha3 and alpha(v) integrin receptors in neuronal migration and laminar organization of the cerebral cortex. Neuron 22, 277–289 (1999).
He, B., Wang, Y., Li, H. & Huang, Y. The role of integrin beta in schizophrenia: a preliminary exploration. CNS Spectr. 28, 561–570 (2023).
Printz, D. J. et al. Elevation of CD5+ B lymphocytes in schizophrenia. Biol. Psychiatry 46, 110–118 (1999).
Scheiber, C., Schulz, T., Schneider, J. M., Bechter, K. & Schneider, E. M. Old and new biomarkers for infection, inflammation, and autoimmunity in treatment-resistant affective and schizophrenic spectrum disorders. Pharmaceuticals 15. https://doi.org/10.3390/ph15030299 (2022).
Murphy, C. E. et al. Nuclear factor kappa B activation appears weaker in schizophrenia patients with high brain cytokines than in non-schizophrenic controls with high brain cytokines. J. Neuroinflamm. 17, 215 (2020).
Crocker, P. R., Paulson, J. C. & Varki, A. Siglecs and their roles in the immune system. Nat. Rev. Immunol. 7, 255–266 (2007).
Tomasik, J. et al. Pretreatment levels of the fatty acid handling proteins H-FABP and CD36 predict response to olanzapine in recent-onset schizophrenia patients. Brain Behav. Immun. 52, 178–186 (2016).
Del Toro, D. et al. Structural basis of Teneurin-Latrophilin interaction in repulsive guidance of migrating neurons. Cell 180, 323–339.e319 (2020).
Kamran, M. et al. Independent associated SNPs at SORCS3 and its protein interactors for multiple brain-related disorders and traits. Genes 14. https://doi.org/10.3390/genes14020482 (2023).
Li, S., DeLisi, L. E. & McDonough, S. I. Rare germline variants in individuals diagnosed with schizophrenia within multiplex families. Psychiatry Res. 303, 114038 (2021).
Iwakura, Y. & Nawa, H. ErbB1-4-dependent EGF/neuregulin signals and their cross talk in the central nervous system: pathological implications in schizophrenia and Parkinson’s disease. Front. Cell Neurosci. 7, 4 (2013).
Futamura, T. et al. Abnormal expression of epidermal growth factor and its receptor in the forebrain and serum of schizophrenic patients. Mol. Psychiatry 7, 673–682 (2002).
Futamura, T. et al. Neonatal perturbation of neurotrophic signaling results in abnormal sensorimotor gating and social interaction in adults: implication for epidermal growth factor in cognitive development. Mol. Psychiatry 8, 19–29 (2003).
Tohmi, M. et al. Distinct influences of neonatal epidermal growth factor challenge on adult neurobehavioral traits in four mouse strains. Behav. Genet. 35, 615–629 (2005).
Sotoyama, H. et al. Pallidal hyperdopaminergic innervation underlying D2 receptor-dependent behavioral deficits in the schizophrenia animal model established by EGF. PLoS ONE 6, e25831 (2011).
Namba, H. et al. Transforming growth factor alpha attenuates the functional expression of AMPA receptors in cortical GABAergic neurons. Mol. Cell Neurosci. 31, 628–641 (2006).
Tchalla, A. E. et al. Elevated soluble vascular cell adhesion Molecule-1 is associated with cerebrovascular resistance and cognitive function. J. Gerontol. A Biol. Sci. Med. Sci. 72, 560–566 (2017).
Schneider, A. L. et al. Hemoglobin, Anemia, and cognitive function: the atherosclerosis risk in communities study. J. Gerontol. A Biol. Sci. Med. Sci. 71, 772–779 (2016).
Acknowledgements
We would like to express our sincere thanks to all participants in this work. This research was supported by the National Key Research and Development Program of China (Grant No. 2021YFE0191400 (X.C.)), National Natural Science Foundation of China (Grant No. 82101576 (Z.L.)), Science and Technology Innovation Program of Hunan Province (Grant No. 2022RC1040 (Z.L.)), Natural Science Foundation of Hunan Province of China (Grant No.2022JJ40695 (Z.L.)), the Scientific Research Launch Project for new employees of the Second Xiangya Hospital of Central South University (Z.L. and Y.H.), and the Fundamental Research Funds for the Central Universities of Central South University (Grant No. 2024ZZTS0932 (S.Z.))
Author information
Authors and Affiliations
Contributions
The study was designed and supervised by Zongchang Li, Ying He and Xiaogang Chen. Data were collected by Aijun Liao, Yujue Wang, Qian Liu, Lijun Ouyang, Huiqing Peng, Xinbo Yang, Liu Yuan, and Linlin Zhao. The analyses and interpretation of data were performed by Sijie Zhang and Zongchang Li. The manuscript was first drafted by Sijie Zhang, and revised critically by Xiaogang Chen, Zongchang Li, and Ying He for important intellectual content. All co-authors revised and approved the final version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41537_2024_510_MOESM1_ESM.docx
Supplement Material for Profiling Expressing Features of Surface Proteins on Single-Exosome in First-episode Schizophrenia Patients: A Preliminary Study
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, S., Liao, A., Wang, Y. et al. Profiling expressing features of surface proteins on single-exosome in first-episode Schizophrenia patients: a preliminary study. Schizophr 10, 84 (2024). https://doi.org/10.1038/s41537-024-00510-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41537-024-00510-z