Abstract
Acute heart failure (AHF) is a syndrome defined as the new onset (de novo heart failure (HF)) or worsening (acutely decompensated heart failure (ADHF)) of symptoms and signs of HF, mostly related to systemic congestion. In the presence of an underlying structural or functional cardiac dysfunction (whether chronic in ADHF or undiagnosed in de novo HF), one or more precipitating factors can induce AHF, although sometimes de novo HF can result directly from the onset of a new cardiac dysfunction, most frequently an acute coronary syndrome. Despite leading to similar clinical presentations, the underlying cardiac disease and precipitating factors may vary greatly and, therefore, the pathophysiology of AHF is highly heterogeneous. Left ventricular diastolic or systolic dysfunction results in increased preload and afterload, which in turn lead to pulmonary congestion. Fluid retention and redistribution result in systemic congestion, eventually causing organ dysfunction due to hypoperfusion. Current treatment of AHF is mostly symptomatic, centred on decongestive drugs, at best tailored according to the initial haemodynamic status with little regard to the underlying pathophysiological particularities. As a consequence, AHF is still associated with high mortality and hospital readmission rates. There is an unmet need for increased individualization of in-hospital management, including treatments targeting the causative factors, and continuation of treatment after hospital discharge to improve long-term outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ponikowski, P. et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 37, 2129–2200 (2016). The guidelines of the European Society of Cardiology provide evidence-based recommendations on diagnosis and treatment of chronic HF and AHF.
Braunwald, E. Heart failure. JACC Heart Fail. 1, 1–20 (2013).
Mebazaa, A. et al. Recommendations on pre-hospital and early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine–short version. Eur. Heart J. 36, 1958–1966 (2015). This consensus document contains contemporary recommendations endorsed by different professional societies on the management of AHF.
Ambrosy, A. P. et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J. Am. Coll. Cardiol. 63, 1123–1133 (2014).
Crespo-Leiro, M. G. et al. European Society of Cardiology Heart Failure long-term registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur. J. Heart Fail. 18, 613–625 (2016).
Mentz, R. J. & O’Connor, C. M. Pathophysiology and clinical evaluation of acute heart failure. Nat. Rev. Cardiol. 13, 28–35 (2015).
Ishihara, S. et al. Similar hemodynamic decongestion with vasodilators and inotropes: systematic review, meta-analysis, and meta-regression of 35 studies on acute heart failure. Clin. Res. Cardiol. 105, 971–980 (2016).
Mebazaa, A. et al. Short-term survival by treatment among patients hospitalized with acute heart failure: the global ALARM-HF registry using propensity scoring methods. Intensive Care Med. 37, 290–301 (2010).
Mebazaa, A. et al. Acute heart failure and cardiogenic shock: a multidisciplinary practical guidance. Intensive Care Med. 42, 147–163 (2015).
Mebazaa, A. et al. Management of cardiogenic shock complicating myocardial infarction. Intensive Care Med. 44, 760–773 (2018).
Follath, F. et al. Clinical presentation, management and outcomes in the acute heart failure global survey of standard treatment (ALARM-HF). Intensive Care Med. 37, 619–626 (2011).
Greene, S. J. et al. The vulnerable phase after hospitalization for heart failure. Nat. Rev. Cardiol. 12, 220–229 (2015). This paper reviews the topic of the vulnerable phase after an AHF episode, which is characterized by high mortality and readmission rates.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1736–1788 (2018).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196 (2012).
Setoguchi, S., Stevenson, L. W. & Schneeweiss, S. Repeated hospitalizations predict mortality in the community population with heart failure. Am. Heart J. 154, 260–266 (2007).
Gheorghiade, M. et al. Acute heart failure syndromes: current state and framework for future research. Circulation 112, 3958–3968 (2005).
Hamo, C. E. et al. A critical appraisal of short-term endpoints in acute heart failure clinical trials. J. Card. Fail. 24, 783–792 (2018).
Cleland, J. et al. The EuroHeart Failure survey programme—a survey on the quality of care among patients with heart failure in Europe: Part 1: patient characteristics and diagnosis. Eur. Heart J. 24, 442–463 (2003).
Cuffe, M. S. et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA 287, 1541–1547 (2002).
Dharmarajan, K. et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 309, 355–363 (2013).
Fudim, M. et al. Aetiology, timing and clinical predictors of early vs. late readmission following index hospitalization for acute heart failure: insights from ASCEND–HF. Eur. J. Heart Fail. 20, 304–314 (2018).
Giamouzis, G. et al. Hospitalization epidemic in patients with heart failure: risk factors, risk prediction, knowledge gaps, and future directions. J. Card. Fail. 17, 54–75 (2011).
Sokoreli, I. et al. Prognostic value of psychosocial factors for first and recurrent hospitalizations and mortality in heart failure patients: insights from the OPERA–HF study. Eur. J. Heart Fail. 20, 689–696 (2018).
Ferreira, J. P. et al. World Heart Federation Roadmap for heart failure. Glob. Heart 14, 197–214 (2019).
Dokainish, H. et al. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet Glob. Health 5, e665–e672 (2017). This study provides epidemiological data on mortality associated with HF across different continents.
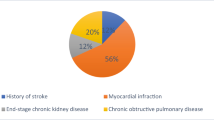
Khatibzadeh, S., Farzadfar, F., Oliver, J., Ezzati, M. & Moran, A. Worldwide risk factors for heart failure: a systematic review and pooled analysis. Int. J. Cardiol. 168, 1186–1194 (2013).
Damasceno, A. et al. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries. Arch. Intern. Med. 172, 1386–1394 (2012).
Parada, H., Carrasco, H. A., Añez, N., Fuenmayor, C. & Inglessis, I. Cardiac involvement is a constant finding in acute Chagas’ disease: a clinical, parasitological and histopathological study. Int. J. Cardiol. 60, 49–54 (1997).
Bocchi, E. A. et al. Long-term prospective, randomized, controlled study using repetitive education at six-month intervals and monitoring for adherence in heart failure outpatients: the REMADHE trial. Circ. Heart Fail. 1, 115–124 (2008).
Doval, H. C. et al. Randomised trial of low-dose amiodarone in severe congestive heart failure. Grupo de Estudio de la Sobrevida en la Insuficiencia Cardiaca en Argentina (GESICA). Lancet 344, 493–498 (1994).
Zühlke, L. et al. Clinical outcomes in 3343 children and adults with rheumatic heart disease from 14 low- and middle-income countries: two-year follow-up of the global rheumatic heart disease registry (the REMEDY Study). Circulation 134, 1456–1466 (2016).
Sliwa, K. et al. Incidence and characteristics of newly diagnosed rheumatic heart disease in urban African adults: insights from the Heart of Soweto study. Eur. Heart J. 31, 719–727 (2010).
Bauersachs, J. et al. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur. J. Heart Fail. 21, 827–843 (2019).
Abraham, W. T. et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J. Am. Coll. Cardiol. 52, 347–356 (2008).
Sliwa, K. et al. Readmission and death after an acute heart failure event: predictors and outcomes in sub-Saharan Africa: results from the THESUS-HF registry. Eur. Heart J. 34, 3151–3159 (2013).
Arrigo, M., Parissis, J. T., Akiyama, E. & Mebazaa, A. Understanding acute heart failure: pathophysiology and diagnosis. Eur. Heart J. Suppl. 18, G11–G18 (2016). This review summarizes the pathophysiology and the diagnostic process in AHF with special attention to treatment-relevant aspects.
Shah, A. M. Ventricular remodeling in heart failure with preserved ejection fraction. Curr. Heart Fail. Rep. 10, 341–349 (2013).
Wang, M. & Shah, A. M. Age-associated pro-inflammatory remodeling and functional phenotype in the heart and large arteries. J. Mol. Cell. Cardiol. 83, 101–111 (2015).
Zile, M. R. et al. Transition from chronic compensated to acute decompensated heart failure: pathophysiological insights obtained from continuous monitoring of intracardiac pressures. Circulation 118, 1433–1441 (2008). This study provides unique insights into the pathophysiology of AHF using data obtained from continuous monitoring of intracardiac pressures.
Miller, W. L. & Mullan, B. P. Understanding the heterogeneity in volume overload and fluid distribution in decompensated heart failure is key to optimal volume management: role for blood volume quantitation. JACC Heart Fail. 2, 298–305 (2014).
Kaye, D. M. et al. Neurochemical evidence of cardiac sympathetic activation and increased central nervous system norepinephrine turnover in severe congestive heart failure. J. Am. Coll. Cardiol. 23, 570–578 (1994).
Fallick, C., Sobotka, P. A. & Dunlap, M. E. Sympathetically mediated changes in capacitance: redistribution of the venous reservoir as a cause of decompensation. Circ. Heart Fail. 4, 669–675 (2011).
Chaudhry, S. I., Wang, Y., Concato, J., Gill, T. M. & Krumholz, H. M. Patterns of weight change preceding hospitalization for heart failure. Circulation 116, 1549–1554 (2007).
Nijst, P. et al. The pathophysiological role of interstitial sodium in heart failure. J. Am. Coll. Cardiol. 65, 378–388 (2015).
Titze, J. et al. Glycosaminoglycan polymerization may enable osmotically inactive Na+ storage in the skin. Am. J. Physiol. Heart Circ. Physiol. 287, H203–H208 (2004).
Guyton, A. C. Interstitial fluid presure. II. Pressure-volume curves of interstitial space. Circ. Res. 16, 452–460 (1965).
Hartupee, J. & Mann, D. L. Neurohormonal activation in heart failure with reduced ejection fraction. Nat. Rev. Cardiol. 14, 30–38 (2017).
Mullens, W., Verbrugge, F. H., Nijst, P. & Tang, W. H. W. Renal sodium avidity in heart failure: from pathophysiology to treatment strategies. Eur. Heart J. 38, 1872–1882 (2017).
McKie, P. M. et al. Impaired natriuretic and renal endocrine response to acute volume expansion in pre-clinical systolic and diastolic dysfunction. J. Am. Coll. Cardiol. 58, 2095–2103 (2011).
Mullens, W. & Tang, W. H. W. The early intertwining of the heart and the kidney through an impaired natriuretic response to acute volume expansion. J. Am. Coll. Cardiol. 58, 2104–2105 (2011).
Mullens, W. et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J. Am. Coll. Cardiol. 53, 589–596 (2009). This study highlights the impact of congestion (instead of reduced cardiac output) on renal function in patients with AHF.
Damman, K. et al. Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J. Am. Coll. Cardiol. 53, 582–588 (2009).
Nijst, P., Martens, P., Dupont, M., Tang, W. H. W. & Mullens, W. Intrarenal flow alterations during transition from euvolemia to intravascular volume expansion in heart failure patients. JACC Heart Fail. 5, 672–681 (2017).
Cotter, G., Metra, M., Milo-Cotter, O., Dittrich, H. C. & Gheorghiade, M. Fluid overload in acute heart failure – re-distribution and other mechanisms beyond fluid accumulation. Eur. J. Heart Fail. 10, 165–169 (2014).
Greenway, C. V. & Lister, G. E. Capacitance effects and blood reservoir function in the splanchnic vascular bed during non-hypotensive haemorrhage and blood volume expansion in anaesthetized cats. J. Physiol. 237, 279–294 (1974).
Verbrugge, F. H. et al. Abdominal contributions to cardiorenal dysfunction in congestive heart failure. J. Am. Coll. Cardiol. 62, 485–495 (2013).
Fonarow, G. C. et al. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Arch. Intern. Med. 168, 847–854 (2008).
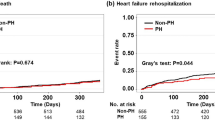
Arrigo, M. et al. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur. J. Heart Fail. 19, 201–208 (2017). This study shows the impact of precipitating factors on prognosis of patients with AHF in a large intercontinental registry.
Arrigo, M. et al. Effect of precipitating factors of acute heart failure on readmission and long-term mortality. ESC. Heart Fail. 3, 115–121 (2016).
Platz, E. et al. Prevalence and prognostic importance of precipitating factors leading to heart failure hospitalization: recurrent hospitalizations and mortality. Eur. J. Heart Fail. 20, 295–303 (2018).
Miró, Ò. et al. Time-pattern of adverse outcomes after an infection-triggered acute heart failure decompensation and the influence of early antibiotic administration and hospitalisation: results of the PAPRICA-3 study. Clin. Res. Cardiol. 109, 34–45 (2020).
Parrinello, G. et al. Water and sodium in heart failure: a spotlight on congestion. Heart Fail. Rev. 20, 13–24 (2015).
Volpe, M., Carnovali, M. & Mastromarino, V. The natriuretic peptides system in the pathophysiology of heart failure: from molecular basis to treatment. Clin. Sci. 130, 57–77 (2016).
MacIver, D. H., Adeniran, I., MacIver, I. R., Revell, A. & Zhang, H. Physiological mechanisms of pulmonary hypertension. Am. Heart J. 180, 1–11 (2016).
Borné, Y. et al. Vascular endothelial growth factor D, pulmonary congestion, and incidence of heart failure. J. Am. Coll. Cardiol. 71, 580–582 (2018).
Houston, B. A. et al. Relation of lymphangiogenic factor vascular endothelial growth factor-D to elevated pulmonary artery wedge pressure. Am. J. Cardiol. 124, 756–762 (2019).
von Moos, S. et al. Vascular endothelial growth factor D is a biomarker of fluid overload in haemodialysis patients. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfz281 (2020).
Ware, L. B. & Matthay, M. A. Clinical practice. Acute pulmonary edema. N. Engl. J. Med. 353, 2788–2796 (2005).
Harjola, V.-P. et al. Organ dysfunction, injury and failure in acute heart failure: from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. J. Heart Fail. 19, 821–836 (2017). This review summarizes pathophysiology, diagnosis and management of organ dysfunction occurring in patients with AHF.
Braam, B., Cupples, W. A., Joles, J. A. & Gaillard, C. Systemic arterial and venous determinants of renal hemodynamics in congestive heart failure. Heart Fail. Rev. 17, 161–175 (2012).
Legrand, M., Mebazaa, A., Ronco, C. & Januzzi, J. L. When cardiac failure, kidney dysfunction, and kidney injury intersect in acute conditions: the case of cardiorenal syndrome. Crit. Care Med. 42, 2109–2117 (2014).
Mullens, W. et al. Elevated intra-abdominal pressure in acute decompensated heart failure. J. Am. Coll. Cardiol. 51, 300–306 (2008).
Ahmad, T. et al. Worsening renal function in patients with acute heart failure undergoing aggressive diuresis is not associated with tubular injury. Circulation 137, 2016–2028 (2018).
Maisel, A. S. et al. Neutrophil gelatinase-associated lipocalin for acute kidney injury during acute heart failure hospitalizations: the AKINESIS study. J. Am. Coll. Cardiol. 68, 1420–1431 (2016).
Mullens, W. et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21, 137–155 (2019). This position statement from the Heart Failure Association of the European Society of Cardiology provides practical guidance on the use of diuretics to relieve congestion in patients with AHF.
Metra, M. et al. Is worsening renal function an ominous prognostic sign in patients with acute heart failure? The role of congestion and its interaction with renal function. Circ. Heart Fail. 5, 54–62 (2012).
Auer, J. What does the liver tell us about the failing heart? Eur. Heart J. 34, 711–714 (2013).
Møller, S. & Bernardi, M. Interactions of the heart and the liver. Eur. Heart J. 34, 2804–2811 (2013).
Samsky, M. D. et al. Cardiohepatic interactions in heart failure: an overview and clinical implications. J. Am. Coll. Cardiol. 61, 2397–2405 (2013).
Rogler, G. & Rosano, G. The heart and the gut. Eur. Heart J. 35, 426–430 (2014).
Sandek, A. et al. Altered intestinal function in patients with chronic heart failure. J. Am. Coll. Cardiol. 50, 1561–1569 (2007).
Valentova, M. et al. Intestinal congestion and right ventricular dysfunction: a link with appetite loss, inflammation, and cachexia in chronic heart failure. Eur. Heart J. 37, 1684–1691 (2016).
Colombo, P. C. et al. Peripheral venous congestion causes inflammation, neurohormonal, and endothelial cell activation. Eur. Heart J. 35, 448–454 (2014).
Colombo, P. C. et al. Venous congestion, endothelial and neurohormonal activation in acute decompensated heart failure: cause or effect? Curr. Heart Fail. Rep. 12, 215–222 (2015).
McMurray, J. J. V. et al. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 371, 993–1004 (2014).
McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381, 1995–2008 (2019).
Van Aelst, L. N. L. et al. Acutely decompensated heart failure with preserved and reduced ejection fraction present with comparable haemodynamic congestion. Eur. J. Heart Fail. 20, 738–747 (2018).
Van de Werf, F. et al. Diastolic properties of the left ventricle in normal adults and in patients with third heart sounds. Circulation 69, 1070–1078 (1984).
Mebazaa, A. et al. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur. J. Heart Fail. 17, 544–558 (2015).
Ponikowski, P. et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. J. Heart Fail. 18, 891–975 (2016).
Fonarow, G. C. et al. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA 293, 572–580 (2005). This study provides one easy-to-use risk score (among many others available) to stratify patients admitted with AHF.
Peterson, P. N. et al. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association Get With the Guidelines program. Circ. Cardiovasc. Qual. Outcomes 3, 25–32 (2010).
Miró, Ò. et al. Predicting 30-day mortality for patients with acute heart failure in the emergency department: a cohort study. Ann. Intern. Med. 167, 698–705 (2017).
Gheorghiade, M. et al. Assessing and grading congestion in acute heart failure: a scientific statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur. J. Heart Fail. 12, 423–433 (2010). This position statement from the Heart Failure Association of the European Society of Cardiology provides a statement on the assessment and quantification of congestion in AHF.
Maisel, A. S. et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N. Engl. J. Med. 347, 161–167 (2002).
Januzzi, J. L. Jr et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am. J. Cardiol. 95, 948–954 (2005).
Maisel, A. et al. Mid-region pro-hormone markers for diagnosis and prognosis in acute dyspnea. J. Am. Coll. Cardiol. 55, 2062–2076 (2010).
McCullough, P. A. et al. B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) multinational study. Circulation 106, 416–422 (2002).
Arrigo, M., Nijst, P. & Rudiger, A. Optimising heart failure therapies in the acute setting. Card. Fail. Rev. 4, 38–42 (2018).
Platz, E. et al. Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur. Heart J. 37, 1244–1251 (2016).
Aras, M. A. & Teerlink, J. R. Lung ultrasound: a ‘B-line’ to the prediction of decompensated heart failure. Eur. Heart J. 37, 1252–1254 (2016).
Matsue, Y. et al. Time-to-furosemide treatment and mortality in patients hospitalized with acute heart failure. J. Am. Coll. Cardiol. 69, 3042–3051 (2017). This study shows a beneficial association between early administration of decongestive treatment (loop diuretics) and mortality in AHF.
Ledwidge, M. et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 310, 66–74 (2013).
Rubio-Gracia, J. et al. Prevalence, predictors and clinical outcome of residual congestion in acute decompensated heart failure. Int. J. Cardiol. 258, 185–191 (2018).
Gayat, E. et al. Heart failure oral therapies at discharge are associated with better outcome in acute heart failure: a propensity-score matched study. Eur. J. Heart Fail. 20, 345–354 (2018). This study shows in a propensity-matched cohort a positive association between pre-discharge implementation of neuro-humoral blockers (β-adrenergic receptor blockers and renin–angiotensin inhibitors) and survival in patients with AHF.
Plaisance, P., Pirracchio, R., Berton, C., Vicaut, E. & Payen, D. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur. Heart J. 28, 2895–2901 (2007).
Arrigo, M. & Mebazaa, A. Understanding the differences among inotropes. Intensive Care Med. 41, 912–915 (2015).
Butler, J., Gheorghiade, M. & Metra, M. Moving away from symptoms-based heart failure treatment: misperceptions and real risks for patients with heart failure. Eur. J. Heart Fail. 18, 350–352 (2016).
Kula, A. J. et al. Influence of titration of neurohormonal antagonists and blood pressure reduction on renal function and decongestion in decompensated heart failure. Circ. Heart Fail. 9, e002333 (2016).
Brinkley, D. M. et al. Spot urine sodium as triage for effective diuretic infusion in an ambulatory heart failure unit. J. Card. Fail. 24, 349–354 (2018).
Costanzo, M. R. et al. Extracorporeal ultrafiltration for fluid overload in heart failure. J. Am. Coll. Cardiol. 69, 2428–2445 (2017).
Costanzo, M. R. et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J. Am. Coll. Cardiol. 49, 675–683 (2007).
Bart, B. A. et al. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N. Engl. J. Med. 367, 2296–2304 (2012).
ter Maaten, J. M. et al. Diuretic response in acute heart failure–pathophysiology, evaluation and therapy. Nat. Rev. Cardiol. 12, 184–192 (2015). This article reviews the mechanisms and the treatment of diuretic resistance occurring in AHF.
Martens, P., Nijst, P. & Mullens, W. Current approach to decongestive therapy in acute heart failure. Curr. Heart Fail. Rep. 12, 367–378 (2015).
Yancy, C. W. et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 136, e137–e161 (2017).
Peacock, W. F. et al. Cardiac troponin and outcome in acute heart failure. N. Engl. J. Med. 358, 2117–2126 (2008).
Logeart, D. et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J. Am. Coll. Cardiol. 43, 635–641 (2004).
Rehman, S. U., Mueller, T. & Januzzi, J. L. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J. Am. Coll. Cardiol. 52, 1458–1465 (2008).
Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J. Am. Coll. Cardiol. 62, 1495–1539 (2013).
Passantino, A., Monitillo, F., Iacoviello, M. & Scrutinio, D. Predicting mortality in patients with acute heart failure: role of risk scores. World J. Cardiol. 7, 902–911 (2015).
Wadhera, R. K. et al. Association of the Hospital Readmissions Reduction Program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA 320, 2542–2552 (2018).
Gheorghiade, M. et al. A comprehensive, longitudinal description of the in-hospital and post-discharge clinical, laboratory, and neurohormonal course of patients with heart failure who die or are re-hospitalized within 90 days: analysis from the EVEREST trial. Heart Fail. Rev. 17, 485–509 (2012).
Grodin, J. L. et al. Prognostic implications of changes in amino-terminal Pro-B-type natriuretic peptide in acute decompensated heart failure: insights from ASCEND-HF. J. Card. Fail. 25, 703–711 (2019).
Mueller, C. et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur. J. Heart Fail. 21, 715–731 (2019).
Simon, M. A., Schnatz, R. G., Romeo, J. D. & Pacella, J. J. Bedside ultrasound assessment of jugular venous compliance as a potential point-of-care method to predict acute decompensated heart failure 30-day readmission. J. Am. Heart Assoc. 7, e008184 (2018).
Platz, E. et al. Lung ultrasound in acute heart failure: prevalence of pulmonary congestion and short- and long-term outcomes. JACC Heart Fail. 7, 849–858 (2019).
Palazzuoli, A. et al. Early readmission for heart failure: an avoidable or ineluctable debacle? Int. J. Cardiol. 277, 186–195 (2019).
Abraham, W. T. et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet 377, 658–666 (2011).
Adamson, P. B. et al. Wireless pulmonary artery pressure monitoring guides management to reduce decompensation in heart failure with preserved ejection fraction. Circ. Heart Fail. 7, 935–944 (2014).
Givertz, M. M. et al. Pulmonary artery pressure-guided management of patients with heart failure and reduced ejection fraction. J. Am. Coll. Cardiol. 70, 1875–1886 (2017).
Krahnke, J. S. et al. Heart failure and respiratory hospitalizations are reduced in patients with heart failure and chronic obstructive pulmonary disease with the use of an implantable pulmonary artery pressure monitoring device. J. Card. Fail. 21, 240–249 (2015).
Loh, J. P., Barbash, I. M. & Waksman, R. Overview of the 2011 Food and Drug Administration Circulatory System Devices Panel of the Medical Devices Advisory Committee Meeting on the CardioMEMS Champion Heart Failure Monitoring System. J. Am. Coll. Cardiol. 61, 1571–1576 (2013).
Van Veldhuisen, D. J. et al. Intrathoracic impedance monitoring, audible patient alerts, and outcome in patients with heart failure. Circulation 124, 1719–1726 (2011).
Chaudhry, S. I. et al. Telemonitoring in patients with heart failure. N. Engl. J. Med. 363, 2301–2309 (2010).
Jayaram, N. M. et al. Impact of telemonitoring on health status. Circ. Cardiovasc. Qual. Outcomes 10, e004148 (2017).
Koehler, F. et al. Telemedical Interventional Monitoring in Heart Failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: study design. Eur. J. Heart Fail. 12, 1354–1362 (2010).
Cleland, J. G. F. et al. Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) study. J. Am. Coll. Cardiol. 45, 1654–1664 (2005).
Van Spall, H. G. C. et al. Effect of patient-centered transitional care services on clinical outcomes in patients hospitalized for heart failure: the PACT-HF randomized clinical trial. JAMA 321, 753–761 (2019).
Zambroski, C. H., Moser, D. K., Bhat, G. & Ziegler, C. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur. J. Cardiovasc. Nurs. 4, 198–206 (2005).
Rutledge, T., Reis, V. A., Linke, S. E., Greenberg, B. H. & Mills, P. J. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J. Am. Coll. Cardiol. 48, 1527–1537 (2006).
Freedland, K. E. et al. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom. Med. 65, 119–128 (2003).
Adelborg, K. et al. Mortality risk among heart failure patients with depression: a nationwide population-based cohort study. J. Am. Heart Assoc. 5, e004137 (2016).
Sullivan, M., Simon, G., Spertus, J. & Russo, J. Depression-related costs in heart failure care. Arch. Intern. Med. 162, 1860–1866 (2002).
O’Connor, C. M. & Joynt, K. E. Depression: are we ignoring an important comorbidity in heart failure? J. Am. Coll. Cardiol. 43, 1550–1552 (2004).
Reeves, G. R. et al. Comparison of frequency of frailty and severely impaired physical function in patients ≥60 years hospitalized with acute decompensated heart failure versus chronic stable heart failure with reduced and preserved left ventricular ejection fraction. Am. J. Cardiol. 117, 1953–1958 (2016).
Warraich, H. J. et al. Physical function, frailty, cognition, depression, and quality of life in hospitalized adults ≥60 years with acute decompensated heart failure with preserved versus reduced ejection fraction: insights from the REHAB-HF trial. Circ. Heart Fail. 11, e005254 (2018).
Dewan, P. et al. Differential impact of heart failure with reduced ejection fraction on men and women. J. Am. Coll. Cardiol. 73, 29–40 (2019).
Allen, L. A. et al. Identifying patients hospitalized with heart failure at risk for unfavorable future quality of life. Circ. Cardiovasc. Qual. Outcomes 4, 389–398 (2011).
Sidebottom, A. C., Jorgenson, A., Richards, H., Kirven, J. & Sillah, A. Inpatient palliative care for patients with acute heart failure: outcomes from a randomized trial. J. Palliat. Med. 18, 134–142 (2015).
Mebazaa, A. et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE randomized trial. JAMA 297, 1883–1891 (2007).
Teerlink, J. R. et al. Acute treatment with omecamtiv mecarbil to increase contractility in acute heart failure. J. Am. Coll. Cardiol. 67, 1444–1455 (2016).
Packer, M. et al. Effect of ularitide on cardiovascular mortality in acute heart failure. N. Engl. J. Med. 376, 1956–1964 (2017).
Konstam, M. A. et al. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial. JAMA 297, 1319–1331 (2007).
Voors, A. A. et al. Adrenomedullin in heart failure: pathophysiology and therapeutic application. Eur. J. Heart Fail. 21, 163–171 (2019).
Deniau, B. et al. Circulating dipeptidyl peptidase 3 is a myocardial depressant factor: dipeptidyl peptidase 3 inhibition rapidly and sustainably improves haemodynamics. Eur. J. Heart Fail. 14, e0220866 (2019).
Takagi, K. et al. Circulating dipeptidyl peptidase 3 and alteration in haemodynamics in cardiogenic shock: results from the OptimaCC trial. Eur. J. Heart Fail. https://doi.org/10.1002/ejhf.1600 (2019).
Troughton, R., Michael Felker, G. & Januzzi, J. L. Natriuretic peptide-guided heart failure management. Eur. Heart J. 35, 16–24 (2014).
Demissei, B. G. et al. A multimarker multi-time point-based risk stratification strategy in acute heart failure: results from the RELAX-AHF trial. Eur. J. Heart Fail. 19, 1001–1010 (2017).
Acknowledgements
N.R. is supported by the National Institutes of Health, National Human Genome Research Institute, Ruth L. Kirschstein Institutional National Research Service T32 Award in Genomic Medicine (T32 HG009495).
Author information
Authors and Affiliations
Contributions
Introduction (A.M. and M.A.); Epidemiology (K.S.); Mechanisms/pathophysiology (M.A., W.M. and A.M.S.); Diagnosis, screening and prevention (A.M. and M.A.); Management (M.J., W.M. and N.R.); Quality of life (M.J. and N.R.); Outlook (A.M.); Overview of Primer (A.M.).
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks A. Palazzuoli and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arrigo, M., Jessup, M., Mullens, W. et al. Acute heart failure. Nat Rev Dis Primers 6, 16 (2020). https://doi.org/10.1038/s41572-020-0151-7
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-020-0151-7
This article is cited by
-
PRRs-related genes and immune landscape in heart failure and COPD
Scientific Reports (2026)
-
Dynamic changes in mortality risk factors for acute leukemia patients in the ICU and Post-ICU periods
Annals of Hematology (2026)
-
USP8 protects rat-derived H9C2 cardiomyocytes from doxorubicin-triggered ferroptosis and cell death through deubiquitination-mediated stabilization of MDM4
Hereditas (2025)
-
The comparative study of the efficacy of recombinant human brain natriuretic peptide combined with vasoactive medications for elderly patients with heart failure and hypotension receiving injections
BMC Cardiovascular Disorders (2025)
-
Integrated bioinformatics analysis identifies RPS27A and PPP2R1A as shared hub genes in heart failure and COVID-19
Journal of Cardiothoracic Surgery (2025)