Abstract
Although type 1 diabetes mellitus (T1DM) is traditionally viewed as a youth-onset disorder, the number of older adults being diagnosed with this disease is growing. Improvements in the average life expectancy of people with T1DM have also contributed to the growing number of older people living with this disease. We summarize the evidence regarding the epidemiology (incidence, prevalence and excess mortality) of T1DM in older adults (ages ≥60 years) as well as the genetics, immunology and diagnostic challenges. Several studies report an incidence peak of T1DM in older adults of a similar size to or exceeding that in children, and population prevalence generally increases with increasing age. Glutamic acid decarboxylase antibody positivity is frequently observed in adult-onset T1DM. Guidelines for differentiating T1DM from type 2 diabetes mellitus in older adults recommend measuring levels of C-peptide and autoantibodies, including glutamic acid decarboxylase antibodies. However, there is no gold standard for differentiating T1DM from type 2 diabetes mellitus in people aged 60 years and over. As such, the global variation observed in T1DM epidemiology might be in part explained by misclassification, which increases with increasing age of diabetes mellitus onset. With a growing global population of older adults with T1DM, improved genetic and immunological evidence is needed to differentiate diabetes mellitus type at older ages so that a clear epidemiological picture can emerge.
Key points
-
The increasing population of older adults with type 1 diabetes mellitus (T1DM), including those with late-onset T1DM together with those with early-onset T1DM reaching older ages, necessitates a stronger research focus in this age group.
-
Incidence and prevalence of T1DM at older ages vary across the world, partly due to different definitions as well as population characteristics.
-
Given the considerably greater incidence of type 2 diabetes mellitus (T2DM) than of T1DM at older ages, even low levels of misclassification of T2DM as T1DM can lead to major uncertainty in the epidemiology of T1DM.
-
Although survival among older adults with T1DM has improved, older adults with T1DM still have substantially reduced life expectancy compared with those of the same age in the general population.
-
Although glutamic acid decarboxylase positivity and low C-peptide are indicative of T1DM among older adults presenting with new-onset diabetes mellitus, there is no gold standard in differentiating T1DM from T2DM at older ages.
-
A more accurate definition of T1DM in older adults should be developed and applied to epidemiological studies globally to understand the true burden of T1DM among older adults compared with that in other age groups.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Atkinson, M. A., Eisenbarth, G. S. & Michels, A. W. Type 1 diabetes. Lancet 383, 69–82 (2014).
Weisman, A., Bai, J. W., Cardinez, M., Kramer, C. K. & Perkins, B. A. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 5, 501–512 (2017).
Steineck, I. et al. Insulin pump therapy, multiple daily injections, and cardiovascular mortality in 18,168 people with type 1 diabetes: observational study. BMJ 350, h3234 (2015).
Schofield, J., Ho, J. & Soran, H. Cardiovascular risk in type 1 diabetes mellitus. Diabetes Ther. 10, 773–789 (2019).
Arffman, M., Hakkarainen, P., Keskimäki, I., Oksanen, T. & Sund, R. Long-term and recent trends in survival and life expectancy for people with type 1 diabetes in Finland. Diabetes Res. Clin. Pract. 198, 110580 (2023).
Leslie, R. D., Williams, R. & Pozzilli, P. Clinical review: type 1 diabetes and latent autoimmune diabetes in adults: one end of the rainbow. J. Clin. Endocrinol. Metab. 91, 1654–1659 (2006).
Miller, R. G., Secrest, A. M., Sharma, R. K., Songer, T. J. & Orchard, T. J. Improvements in the life expectancy of type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications study cohort. Diabetes 61, 2987–2992 (2012).
Carlson, A. L. et al. Hypoglycemia and glycemic control in older adults with type 1 diabetes: baseline results from the WISDM study. J. Diabetes Sci. Technol. 15, 582–592 (2021).
Musen, G. et al. Cognitive function deficits associated with long-duration type 1 diabetes and vascular complications. Diabetes Care 41, 1749–1756 (2018).
Park, M. & Reynolds, C. F. 3rd Depression among older adults with diabetes mellitus. Clin. Geriatr. Med. 31, 117–137 (2015).
Halper-Stromberg, E. et al. Bone mineral density across the lifespan in patients with type 1 diabetes. J. Clin. Endocrinol. Metab. 105, 746–753 (2020).
Thunander, M. et al. Incidence of type 1 and type 2 diabetes in adults and children in Kronoberg, Sweden. Diabetes Res. Clin. Pract. 82, 247–255 (2008). This was the first study to describe incidence of T1DM in older adults that exceeded that in all age groups, including in children.
Gajewska, K. A., Biesma, R., Sreenan, S. & Bennett, K. Prevalence and incidence of type 1 diabetes in Ireland: a retrospective cross-sectional study using a national pharmacy claims data from 2016. BMJ Open 10, e032916 (2020). This study followed from Thunander et al. (ref. 12) to also report the highest incidence of T1DM in older adults out of all age groups, strengthening the evidence for a possible second incidence peak after age 70 years.
Carstensen, B., Rønn, P. F. & Jørgensen, M. E. Prevalence, incidence and mortality of type 1 and type 2 diabetes in Denmark 1996-2016. BMJ Open Diabetes Res. Care 8, e001071 (2020).
Rogers, M. A. M., Kim, C., Banerjee, T. & Lee, J. M. Fluctuations in the incidence of type 1 diabetes in the United States from 2001 to 2015: a longitudinal study. BMC Med. 15, 199 (2017).
Rodríguez Escobedo, R., Delgado Álvarez, E. & Menéndez Torre, E. L. Incidence of type 1 diabetes mellitus in Asturias (Spain) between 2011 and 2020. Endocrinol. Diabetes Nutr. 70, 189–195 (2023).
Diaz-Valencia, P. A., Bougnères, P. & Valleron, A.-J. Global epidemiology of type 1 diabetes in young adults and adults: a systematic review. BMC Public Health 15, 255 (2015).
Nishioka, Y. et al. Incidence and seasonality of type 1 diabetes: a population-based 3-year cohort study using the National Database in Japan. BMJ Open Diabetes Res. Care 8, e001262 (2020).
Luk, A. O. Y. et al. Secular trends in incidence of type 1 and type 2 diabetes in Hong Kong: a retrospective cohort study. PLoS Med. 17, e1003052 (2020).
Lin, W. H. et al. Incidence of and mortality from Type I diabetes in Taiwan from 1999 through 2010: a nationwide cohort study. PLoS One 9, e86172 (2014).
Jiang, Y. D., Chang, C. H., Tai, T. Y., Chen, J. F. & Chuang, L. M. Incidence and prevalence rates of diabetes mellitus in Taiwan: analysis of the 2000-2009 Nationwide Health Insurance database. J. Formos. Med. Assoc. 111, 599–604 (2012).
Liu, C. et al. Incidence of type 1 diabetes may be underestimated in the Chinese population: evidence from 21.7 million people between 2007 and 2017. Diabetes Care 44, 2503–2509 (2021).
Weng, J. et al. Incidence of type 1 diabetes in China, 2010-13: population based study. BMJ 360, j5295 (2018).
Park, Y. & Eisenbarth, G. S. Genetic susceptibility factors of type 1 diabetes in Asians. Diabetes Metab. Res. Rev. 17, 2–11 (2001).
Schroeder, E. B., Donahoo, W. T., Goodrich, G. K. & Raebel, M. A. Validation of an algorithm for identifying type 1 diabetes in adults based on electronic health record data. Pharmacoepidemiol. Drug Saf. 27, 1053–1059 (2018).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98 (2018).
Australian Bureau of Statistics. Diabetes. Reference Period 2022 https://www.abs.gov.au/statistics/health/health-conditions-and-risks/diabetes/latest-release (2023).
Trief, P. M., Cibula, D., Rodriguez, E., Akel, B. & Weinstock, R. S. Incorrect insulin administration: a problem that warrants attention. Clin. Diabetes 34, 25–33 (2016).
Harding, J. L. et al. Mortality trends among people with type 1 and type 2 diabetes in Australia: 1997-2010. Diabetes Care 37, 2579–2586 (2014).
Foteinopoulou, E. et al. Impact of routine clinic measurement of serum C-peptide in people with a clinician-diagnosis of type 1 diabetes. Diabet. Med. 38, e14449 (2021).
Iqbal, S., Jayyab, A. A., Alrashdi, A. M. & Reverté-Villarroya, S. The predictive ability of C-peptide in distinguishing type 1 diabetes from type 2 diabetes: a systematic review and meta-analysis. Endocr. Pract. 29, 379–387 (2023).
Bullard, K. M. et al. Prevalence of diagnosed diabetes in adults by diabetes type — United States, 2016. MMWR Morb. Mortal. Wkly Rep. 67, 359–361 (2018).
Xu, G. et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ 362, k1497 (2018).
Menke, A. et al. The prevalence of type 1 diabetes in the United States. Epidemiol 24, 773–774 (2013).
Campbell, R. A. S. et al. Socio-economic status and mortality in people with type 1 diabetes in Scotland 2006-2015: a retrospective cohort study. Diabet. Med. 37, 2081–2088 (2020).
Ostrauskas, R. The prevalence of type 1 diabetes mellitus among adolescents and adults in Lithuania during 1991-2004. Medicina 43, 242–250 (2007).
Tomic, D. et al. Lifetime risk, life expectancy, and years of life lost to type 2 diabetes in 23 high-income jurisdictions: a multinational, population-based study. Lancet Diabetes Endocrinol. 10, 795–803 (2022).
National Diabetes Services Scheme. Type 1 Diabetes as at 30 June 2024 https://www.ndss.com.au/wp-content/uploads/Diabetes-Type-1-1.pdf (2024).
Livingstone, S. J. et al. Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008-2010. JAMA 313, 37–44 (2015).
Soedamah-Muthu, S. S. et al. All-cause mortality rates in patients with type 1 diabetes mellitus compared with a non-diabetic population from the UK general practice research database, 1992-1999. Diabetologia 49, 660–666 (2006).
Harding, J. L., Shaw, J. E., Peeters, A., Davidson, S. & Magliano, D. J. Age-specific trends from 2000-2011 in all-cause and cause-specific mortality in type 1 and type 2 diabetes: a cohort study of more than one million people. Diabetes Care 39, 1018–1026 (2016).
Thunander, M., Lindgren, A., Petersson, C., Landin-Olsson, M. & Holmberg, S. Standard mortality rates and years of life lost for serologically defined adult-onset type 1 and type 2 diabetes — a fifteen year follow-up. Diabetes Res. Clin. Pract. 160, 107943 (2020).
Ruiz, P. L. D. et al. Mortality trends in type 1 diabetes: a multicountry analysis of six population-based cohorts. Diabetologia 65, 964–972 (2022). This multi-country analysis highlighted the increased mortality in older adults with T1DM compared with the general population, reporting standardized mortality ratios greater than 1 in all older adult age groups.
Huo, L., Harding, J. L., Peeters, A., Shaw, J. E. & Magliano, D. J. Life expectancy of type 1 diabetic patients during 1997-2010: a national Australian registry-based cohort study. Diabetologia 59, 1177–1185 (2016).
Carstensen, B., Rønn, P. F. & Jørgensen, M. E. Lifetime risk and years lost to type 1 and type 2 diabetes in Denmark, 1996-2016. BMJ Open Diabetes Res. Care 9, e001065 (2021).
Pociot, F. & Lernmark, Å. Genetic risk factors for type 1 diabetes. Lancet 387, 2331–2339 (2016).
Sanjeevi, C. B. et al. Polymorphic amino acid variations in HLA-DQ are associated with systematic physical property changes and occurrence of IDDM. Members of the Swedish Childhood Diabetes Study. Diabetes 44, 125–131 (1995).
Erlich, H. et al. HLA DR-DQ haplotypes and genotypes and type 1 diabetes risk: analysis of the type 1 diabetes genetics consortium families. Diabetes 57, 1084–1092 (2008).
Noble, J. A. & Valdes, A. M. Genetics of the HLA region in the prediction of type 1 diabetes. Curr. Diab. Rep. 11, 533–542 (2011).
Haris, B. et al. Clinical features, epidemiology, autoantibody status, HLA haplotypes and genetic mechanisms of type 1 diabetes mellitus among children in Qatar. Sci. Rep. 11, 18887 (2021).
Haider, M. Z., Shaltout, A., Alsaeid, K., Qabazard, M. & Dorman, J. Prevalence of human leukocyte antigen DQA1 and DQB1 alleles in Kuwaiti Arab children with type 1 diabetes mellitus. Clin. Genet. 56, 450–456 (1999).
El-Amir, M. I. et al. Risk genes and autoantibodies in Egyptian children with type 1 diabetes — low frequency of autoantibodies in carriers of the HLA-DRB1*04:05-DQA1*03-DQB1*02 risk haplotype. Diabetes Metab. Res. Rev. 31, 287–294 (2015).
Noble, J. A. Immunogenetics of type 1 diabetes: a comprehensive review. J. Autoimmun. 64, 101–112 (2015).
Howson, J. M., Rosinger, S., Smyth, D. J., Boehm, B. O. & Todd, J. A. Genetic analysis of adult-onset autoimmune diabetes. Diabetes 60, 2645–2653 (2011).
Redondo, M. J. et al. Heterogeneity of type I diabetes: analysis of monozygotic twins in Great Britain and the United States. Diabetologia 44, 354–362 (2001).
Mishra, R. et al. Genetic discrimination between LADA and childhood-onset type 1 diabetes within the MHC. Diabetes Care 43, 418–425 (2020).
Lynam, A. et al. Development and validation of multivariable clinical diagnostic models to identify type 1 diabetes requiring rapid insulin therapy in adults aged 18-50 years. BMJ Open 9, e031586 (2019).
Jiang, Z. et al. HLA class I genes modulate disease risk and age at onset together with DR-DQ in Chinese patients with insulin-requiring type 1 diabetes. Diabetologia 64, 2026–2036 (2021).
Thomas, N. J. & Jones, A. G. The challenges of identifying and studying type 1 diabetes in adults. Diabetologia 66, 2200–2212 (2023). This 2023 review described the challenges of diagnosing T1DM in older adults.
Zhu, M. et al. Identification of novel T1D risk loci and their association with age and islet function at diagnosis in autoantibody-positive T1D individuals: based on a two-stage genome-wide association study. Diabetes Care 42, 1414–1421 (2019).
Regnell, S. E. & Lernmark, Å. Early prediction of autoimmune (type 1) diabetes. Diabetologia 60, 1370–1381 (2017).
Zampetti, S. et al. GADA titer-related risk for organ-specific autoimmunity in LADA subjects subdivided according to gender (NIRAD study 6). J. Clin. Endocrinol. Metab. 97, 3759–3765 (2012).
Balcha, S. A. et al. Type 1 diabetes in Africa: an immunogenetic study in the Amhara of North-West Ethiopia. Diabetologia 63, 2158–2168 (2020).
Zhou, Z. et al. Frequency, immunogenetics, and clinical characteristics of latent autoimmune diabetes in China (LADA China study): a nationwide, multicenter, clinic-based cross-sectional study. Diabetes 62, 543–550 (2013).
Brooks-Worrell, B. M. & Palmer, J. P. Setting the stage for islet autoimmunity in type 2 diabetes: obesity-associated chronic systemic inflammation and endoplasmic reticulum (ER) stress. Diabetes Care 42, 2338–2346 (2019).
Maddaloni, E. et al. C-peptide determination in the diagnosis of type of diabetes and its management: a clinical perspective. Diabetes Obes. Metab. 24, 1912–1926 (2022).
Wenzlau, J. M. et al. The cation efflux transporter ZnT8 (Slc30A8) is a major autoantigen in human type 1 diabetes. Proc. Natl Acad. Sci. USA 104, 17040–17045 (2007).
Tridgell, D. M., Spiekerman, C., Wang, R. S. & Greenbaum, C. J. Interaction of onset and duration of diabetes on the percent of GAD and IA-2 antibody-positive subjects in the type 1 diabetes genetics consortium database. Diabetes Care 34, 988–993 (2011).
Davis, A. K. et al. Prevalence of detectable C-peptide according to age at diagnosis and duration of type 1 diabetes. Diabetes Care 38, 476–481 (2015).
Hope, S. V. et al. Random non-fasting C-peptide: bringing robust assessment of endogenous insulin secretion to the clinic. Diabet. Med. 33, 1554–1558 (2016).
Wentworth, J. M. et al. Beta cell function in type 1 diabetes determined from clinical and fasting biochemical variables. Diabetologia 62, 33–40 (2019).
Sajjadi, S. F. et al. Algorithms to define diabetes type using data from administrative databases: a systematic review of the evidence. Diabetes Res. Clin. Pract. 203, 110859 (2023).
Tuomi, T. et al. Antibodies to glutamic acid decarboxylase reveal latent autoimmune diabetes mellitus in adults with a non-insulin-dependent onset of disease. Diabetes 42, 359–362 (1993).
Jones, A. G., McDonald, T. J., Shields, B. M., Hagopian, W. & Hattersley, A. T. Latent autoimmune diabetes of adults (LADA) is likely to represent a mixed population of autoimmune (type 1) and nonautoimmune (type 2) diabetes. Diabetes Care 44, 1243–1251 (2021).
Fourlanos, S. et al. Latent autoimmune diabetes in adults (LADA) should be less latent. Diabetologia 48, 2206–2212 (2005).
Brophy, S. et al. Time to insulin initiation cannot be used in defining latent autoimmune diabetes in adults. Diabetes Care 31, 439–441 (2008).
Hawa, M. I. et al. Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: action LADA 7. Diabetes Care 36, 908–913 (2013).
Maddaloni, E. et al. Latent autoimmune diabetes in adults in the United Arab Emirates: clinical features and factors related to insulin-requirement. PLoS One 10, e0131837 (2015).
Xiang, Y. et al. Glutamic acid decarboxylase autoantibodies are dominant but insufficient to identify most Chinese with adult-onset non-insulin requiring autoimmune diabetes: LADA China study 5. Acta Diabetol. 52, 1121–1127 (2015).
Buzzetti, R. et al. High titer of autoantibodies to GAD identifies a specific phenotype of adult-onset autoimmune diabetes. Diabetes Care 30, 932–938 (2007).
Murao, S. et al. Anti-thyroid peroxidase antibody, IA-2 antibody, and fasting C-peptide levels predict beta cell failure in patients with latent autoimmune diabetes in adults (LADA) — a 5-year follow-up of the Ehime study. Diabetes Res. Clin. Pract. 80, 114–121 (2008).
Brahmkshatriya, P. P., Mehta, A. A., Saboo, B. D. & Goyal, R. K. Characteristics and prevalence of latent autoimmune diabetes in adults (LADA). ISRN Pharmacol. 2012, 580202 (2012).
Carlsson, S., Midthjell, K. & Grill, V. Influence of family history of diabetes on incidence and prevalence of latent autoimmune diabetes of the adult: results from the Nord-Trøndelag Health Study. Diabetes Care 30, 3040–3045 (2007).
Li, X., Yang, L., Zhou, Z., Huang, G. & Yan, X. Glutamic acid decarboxylase 65 autoantibody levels discriminate two subtypes of latent autoimmune diabetes in adults. Chin. Med. J. 116, 1728–1732 (2003).
Zimmet, P. Z. et al. Latent autoimmune diabetes mellitus in adults (LADA): the role of antibodies to glutamic acid decarboxylase in diagnosis and prediction of insulin dependency. Diabet. Med. 11, 299–303 (1994).
Turner, R. et al. UKPDS 25: autoantibodies to islet-cell cytoplasm and glutamic acid decarboxylase for prediction of insulin requirement in type 2 diabetes. UK Prospective Diabetes Study Group. Lancet 350, 1288–1293 (1997).
Naik, R. G., Brooks-Worrell, B. M. & Palmer, J. P. Latent autoimmune diabetes in adults. J. Clin. Endocrinol. Metab. 94, 4635–4644 (2009).
Palmer, J. P., Hampe, C. S., Chiu, H., Goel, A. & Brooks-Worrell, B. M. Is latent autoimmune diabetes in adults distinct from type 1 diabetes or just type 1 diabetes at an older age? Diabetes 54, S62–S67 (2005).
Sørgjerd, E. P. et al. Presence of anti-GAD in a non-diabetic population of adults; time dynamics and clinical influence: results from the HUNT study. BMJ Open Diabetes Res. Care 3, e000076 (2015).
Steck, A. K. et al. Predictors of progression from the appearance of islet autoantibodies to early childhood diabetes: the environmental determinants of diabetes in the young (TEDDY). Diabetes Care 38, 808–813 (2015).
Williams, A. J. et al. Detection of antibodies directed to the N-terminal region of GAD is dependent on assay format and contributes to differences in the specificity of gad autoantibody assays for type 1 diabetes. Diabetes 64, 3239–3246 (2015).
Kuhtreiber, W. M. et al. Low levels of C-peptide have clinical significance for established type 1 diabetes. Diabet. Med. 32, 1346–1353 (2015).
Fawwad, A. et al. Relationship of C-peptide levels to duration of Type 1 diabetes — a study from Sindh, Pakistan. Pak. J. Med. Sci. 36, 765–769 (2020).
Ibrahim, T. A. M. et al. Clinical features, biochemistry, and HLA-DRB1 status in youth-onset type 1 diabetes in Sudan. Pediatr. Diabetes 22, 749–757 (2021).
Besançon, S. et al. Clinical features, biochemistry, and HLA-DRB1 status in youth-onset type 1 diabetes in Mali. Pediatr. Diabetes 23, 1552–1559 (2022).
Fawwad, A. et al. Clinical features, biochemistry and HLA-DRB1 status in youth-onset type 1 diabetes in Pakistan. Diabetes Res. Clin. Pract. 149, 9–17 (2019).
Zabeen, B. et al. Clinical features, biochemistry and HLA-DRB1 status in children and adolescents with diabetes in Dhaka, Bangladesh. Diabetes Res. Clin. Pract. 158, 107894 (2019).
Ahmadov, G. A. et al. Epidemiology of childhood-onset type 1 diabetes in Azerbaijan: incidence, clinical features, biochemistry, and HLA-DRB1 status. Diabetes Res. Clin. Pract. 144, 252–259 (2018).
Ahlqvist, E. et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 6, 361–369 (2018).
Petrie, D. et al. Recent trends in life expectancy for people with type 1 diabetes in Sweden. Diabetologia 59, 1167–1176 (2016).
Author information
Authors and Affiliations
Contributions
D.T. and D.J.M. researched data for the article and wrote the article. J.L.H., A.J.J. and J.E.S. contributed substantially to discussion of the content. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Mikael Knip, Xia Li and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Review criteria
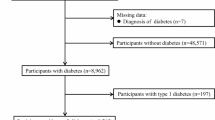
We conducted a Medline search to find articles published in English between 2000 and 2023 using the terms “type 1 diabetes mellitus” AND “incidence” OR “prevalence” OR “mortality”, which were mapped to subject headings. We included all articles that contained age-specific data on any of incidence, prevalence or mortality of type 1 diabetes among adults aged ≥60 years. The 25 identified studies were summarized in a narrative manner. Regarding genetics, immunology and diagnostic challenges of those with type 1 diabetes mellitus, we sourced information from the most recent reviews of the evidence in these areas.
Related links
Human Mortality Database: https://www.mortality.org/
International Diabetes Federation Diabetes Atlas: https://diabetesatlas.org/
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tomic, D., Harding, J.L., Jenkins, A.J. et al. The epidemiology of type 1 diabetes mellitus in older adults. Nat Rev Endocrinol 21, 92–104 (2025). https://doi.org/10.1038/s41574-024-01046-z
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41574-024-01046-z
This article is cited by
-
Global burden of diabetes in women from 1990 to 2021, with projections to 2050: population-based study
BMC Medicine (2025)
-
Older people with type 1 diabetes mellitus: a call for a new management approach
Nature Reviews Endocrinology (2025)
-
Typ 1 Diabetes mellitus
Die Diabetologie (2025)
-
Preparing to Meet the Needs of a Growing Older Adult Population with Type 1 Diabetes: A Narrative Review
Journal of General Internal Medicine (2025)