Abstract
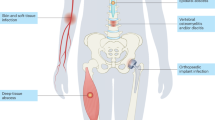
Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most successful modern pathogens. The same organism that lives as a commensal and is transmitted in both health-care and community settings is also a leading cause of bacteraemia, endocarditis, skin and soft tissue infections, bone and joint infections and hospital-acquired infections. Genetically diverse, the epidemiology of MRSA is primarily characterized by the serial emergence of epidemic strains. Although its incidence has recently declined in some regions, MRSA still poses a formidable clinical threat, with persistently high morbidity and mortality. Successful treatment remains challenging and requires the evaluation of both novel antimicrobials and adjunctive aspects of care, such as infectious disease consultation, echocardiography and source control. In this Review, we provide an overview of basic and clinical MRSA research and summarize the expansive body of literature on the epidemiology, transmission, genetic diversity, evolution, surveillance and treatment of MRSA.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Newsom, S. W. Ogston’s coccus. J. Hosp. Infect. 70, 369–372 (2008).
Harkins, C. P. et al. Methicillin-resistant Staphylococcus aureus emerged long before the introduction of methicillin into clinical practice. Genome Biol. 18, 130 (2017).
Katayama, Y., Ito, T. & Hiramatsu, K. A new class of genetic element, staphylococcus cassette chromosome mec, encodes methicillin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 44, 1549–1555 (2000).
Hartman, B. J. & Tomasz, A. Low-affinity penicillin-binding protein associated with beta-lactam resistance in. Staphylococcus aureus. J. Bacteriol. 158, 513–516 (1984).
Tenover, F. C. et al. Characterization of a strain of community-associated methicillin-resistant Staphylococcus aureus widely disseminated in the United States. J. Clin. Microbiol. 44, 108–118 (2006).
Kennedy, A. D. et al. Epidemic community-associated methicillin-resistant Staphylococcus aureus: recent clonal expansion and diversification. Proc. Natl Acad. Sci. USA 105, 1327–1332 (2008). This paper represents one of a series of influential genomic analyses examining the evolution of CA-MRSA in the early 2000s.
McAdam, P. R. et al. Molecular tracing of the emergence, adaptation, and transmission of hospital-associated methicillin-resistant Staphylococcus aureus. Proc. Natl Acad. Sci. USA 109, 9107–9112 (2012). This paper represents another influential genomic analysis, this time focusing on the evolution of HA-MRSA strains.
David, M. Z. et al. Staphylococcus aureus bacteremia at 5 US academic medical centers, 2008-2011: significant geographic variation in community-onset infections. Clin. Infect. Dis. 59, 798–807 (2014).
Casey, J. A., Curriero, F. C., Cosgrove, S. E., Nachman, K. E. & Schwartz, B. S. High-density livestock operations, crop field application of manure, and risk of community-associated methicillin-resistant Staphylococcus aureus infection in Pennsylvania. JAMA Intern. Med. 173, 1980–1990 (2013).
Dantes, R. et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern. Med. 173, 1970–1978 (2013).
Wyllie, D. H. et al. Decline of meticillin-resistant Staphylococcus aureus in Oxfordshire hospitals is strain-specific and preceded infection-control intensification. BMJ Open 1, e000160 (2011). This thought-provoking study demonstrates that MRSA infection rates began to decline prior to implementation of widespread infection control measures. These data suggest strain-specific factors have a substantial role in the epidemiology of MRSA.
Clarridge, J. E. 3rd, Harrington, A. T., Roberts, M. C., Soge, O. O. & Maquelin, K. Impact of strain typing methods on assessment of relationship between paired nares and wound isolates of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 51, 224–231 (2013).
von Eiff, C., Becker, K., Machka, K., Stammer, H. & Peters, G. Nasal carriage as a source of Staphylococcus aureus bacteremia. Study Group. N. Engl. J. Med. 344, 11–16 (2001).
Eells, S. J. et al. Persistent environmental contamination with USA300 methicillin-resistant Staphylococcus aureus and other pathogenic strain types in households with S. aureus skin infections. Infect. Control Hosp. Epidemiol. 35, 1373–1382 (2014).
Azarian, T. et al. Intrahost evolution of methicillin-resistant Staphylococcus aureus USA300 among individuals with reoccurring skin and soft-tissue infections. J. Infect. Dis. 214, 895–905 (2016).
Arshad, S. et al. Ceftaroline fosamil monotherapy for methicillin-resistant Staphylococcus aureus bacteremia: a comparative clinical outcomes study. Int. J. Infect. Dis. 57, 27–31 (2017).
Corey, G. R. et al. Pooled analysis of single-dose oritavancin in the treatment of acute bacterial skin and skin-structure infections caused by Gram-positive pathogens, including a large patient subset with methicillin-resistant. Staphylococcus aureus. Int. J. Antimicrob. Agents 48, 528–534 (2016).
O’Riordan, W. et al. A comparison of the efficacy and safety of intravenous followed by oral delafloxacin with vancomycin plus aztreonam for the treatment of acute bacterial skin and skin structure infections: a phase 3, multinational, double-blind, randomized study. Clin. Infect. Dis. 67, 657–666 (2018).
Huang, D. B. et al. A phase II randomized, double-blind, multicenter study to evaluate efficacy and safety of intravenous iclaprim versus vancomycin for the treatment of nosocomial pneumonia suspected or confirmed to be due to Gram-positive pathogens. Clin. Ther. 39, 1706–1718 (2017).
van Hal, S. J. et al. Predictors of mortality in Staphylococcus aureus bacteremia. Clin. Microbiol. Rev. 25, 362–386 (2012).
Lindsay, J. A. & Holden, M. T. Staphylococcus aureus: superbug, super genome? Trends Microbiol. 12, 378–385 (2004).
Ito, T. et al. Structural comparison of three types of staphylococcal cassette chromosome mec integrated in the chromosome in methicillin-resistant. Staphylococcus aureus. Antimicrob. Agents Chemother. 45, 1323–1336 (2001).
Planet, P. J. et al. Architecture of a species: phylogenomics of Staphylococcus aureus. Trends Microbiol. 25, 153–166 (2017). An overview of the phylogenetics of S. aureus as a species is presented.
Weterings, V. et al. Next-generation sequence analysis reveals transfer of methicillin resistance to a methicillin-susceptible Staphylococcus aureus strain that subsequently caused a methicillin-resistant Staphylococcus aureus outbreak: a descriptive study. J. Clin. Microbiol. 55, 2808–2816 (2017).
Iandolo, J. J. et al. Comparative analysis of the genomes of the temperate bacteriophages phi 11, phi 12 and phi 13 of Staphylococcus aureus 8325. Gene 289, 109–118 (2002).
Malachowa, N. & DeLeo, F. R. Mobile genetic elements of Staphylococcus aureus. Cell. Mol. Life Sci. 67, 3057–3071 (2010).
Sidhu, M. S., Heir, E., Leegaard, T., Wiger, K. & Holck, A. Frequency of disinfectant resistance genes and genetic linkage with beta-lactamase transposon Tn552 among clinical staphylococci. Antimicrob. Agents Chemother. 46, 2797–2803 (2002).
Mwangi, M. M. et al. Tracking the in vivo evolution of multidrug resistance in Staphylococcus aureus by whole-genome sequencing. Proc. Natl Acad. Sci. USA 104, 9451–9456 (2007). This paper presents a detailed, truly translational study in which the real-time evolution of drug resistance in a persistent MRSA infection was dissected through repeated whole genome sequencing of isolates from a single individual.
Chen, C. J., Huang, Y. C. & Chiu, C. H. Multiple pathways of cross-resistance to glycopeptides and daptomycin in persistent MRSA bacteraemia. J. Antimicrob. Chemother. 70, 2965–2972 (2015).
Weigel, L. M. et al. Genetic analysis of a high-level vancomycin-resistant isolate of Staphylococcus aureus. Science 302, 1569–1571 (2003).
Rossi, F. et al. Transferable vancomycin resistance in a community-associated MRSA lineage. N. Engl. J. Med. 370, 1524–1531 (2014).
Uhlemann, A. C. et al. Molecular tracing of the emergence, diversification, and transmission of S. aureus sequence type 8 in a New York community. Proc. Natl Acad. Sci. USA 111, 6738–6743 (2014).
Tong, A. et al. Panton-Valentine leukocidin is not the primary determinant of outcome for Staphylococcus aureus skin infections: evaluation from the CANVAS studies. PLOS ONE 7, e37212 (2012).
Li, M. et al. Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. Proc. Natl Acad. Sci. USA 106, 5883–5888 (2009).
Lindsay, J. A. Staphylococcus aureus genomics and the impact of horizontal gene transfer. Int. J. Med. Microbiol. 304, 103–109 (2014).
Jamrozy, D. et al. Evolution of mobile genetic element composition in an epidemic methicillin-resistant Staphylococcus aureus: temporal changes correlated with frequent loss and gain events. BMC Genomics 18, 684 (2017).
Boucher, H. W. & Corey, G. R. Epidemiology of methicillin-resistant. Staphylococcus aureus. Clin. Infect. Dis. 46 (Suppl. 5), 344–349 (2008).
Moran, G. J. et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N. Engl. J. Med. 355, 666–674 (2006).
David, M. Z., Mennella, C., Mansour, M., Boyle-Vavra, S. & Daum, R. S. Predominance of methicillin-resistant Staphylococcus aureus among pathogens causing skin and soft tissue infections in a large urban jail: risk factors and recurrence rates. J. Clin. Microbiol. 46, 3222–3227 (2008).
Hota, B. et al. Community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections at a public hospital: do public housing and incarceration amplify transmission? Arch. Intern. Med. 167, 1026–1033 (2007).
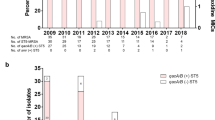
Klein, E. Y. et al. Trends in methicillin-resistant Staphylococcus aureus hospitalizations in the United States, 2010–2014. Clin. Infect. Dis. 65, 1921–1923 (2017). One of the largest and most up-to-date cross-sectional studies on the burden of MRSA infections in US hospitals is presented.
Kallen, A. J. et al. Health care-associated invasive MRSA infections, 2005–2008. JAMA 304, 641–648 (2010).
Landrum, M. L. et al. Epidemiology of Staphylococcus aureus blood and skin and soft tissue infections in the US military health system, 2005–2010. JAMA 308, 50–59 (2012).
de Kraker, M. E. et al. The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin. Microbiol. Infect. 19, 860–868 (2013).
Sutter, D. E. et al. Changing susceptibility of Staphylococcus aureus in a US pediatric population. Pediatrics 137, e20153099 (2016). This up-to-date cross-sectional study confirms a reduction in the MRSA incidence among the US paediatric population, mirroring adult trends.
David, M. Z. & Daum, R. S. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin. Microbiol. Rev. 23, 616–687 (2010).
Popovich, K. J. et al. Genomic and epidemiological evidence for community origins of hospital-onset methicillin-resistant Staphylococcus aureus bloodstream infections. J. Infect. Dis. 215, 1640–1647 (2017).
DeLeo, F. R. et al. Molecular differentiation of historic phage-type 80/81 and contemporary epidemic Staphylococcus aureus. Proc. Natl Acad. Sci. USA 108, 18091–18096 (2011).
Tenover, F. C. & Goering, R. V. Methicillin-resistant Staphylococcus aureus strain USA300: origin and epidemiology. J. Antimicrob. Chemother. 64, 441–446 (2009).
Centers for Disease Control and Prevention. Methicillin-resistant Staphylococcus aureus skin or soft tissue infections in a state prison—Mississippi, 2000. Morb. Mortal. Wkly Rep. 50, 919–922 (2001).
[No authors listed.] Methicillin-resistant Staphylococcus aureus infections among competitive sports participants — Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000–2003. Conn. Med. 67, 549–551 (2003).
Hageman, J. C. et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003–2004 influenza season. Emerg. Infect. Dis. 12, 894–899 (2006).
Toleman, M. S. et al. Systematic surveillance detects multiple silent introductions and household transmission of methicillin-resistant Staphylococcus aureus USA300 in the East of England. J. Infect. Dis. 214, 447–453 (2016).
Glaser, P. et al. Demography and intercontinental spread of the USA300 community-acquired methicillin-resistant Staphylococcus aureus lineage. mBio 7, e02183-15 (2016).
van der Mee-Marquet, N. et al. The incidence of Staphylococcus aureus ST8-USA300 among French pediatric inpatients is rising. Eur. J. Clin. Microbiol. Infect. Dis. 34, 935–942 (2015).
Planet, P. J. et al. Parallel epidemics of community-associated methicillin-resistant Staphylococcus aureus USA300 infection in North and South America. J. Infect. Dis. 212, 1874–1882 (2015).
Murchan, S. et al. Emergence, spread, and characterization of phage variants of epidemic methicillin-resistant Staphylococcus aureus 16 in England and Wales. J. Clin. Microbiol. 42, 5154–5160 (2004).
O’Neill, G. L., Murchan, S., Gil-Setas, A. & Aucken, H. M. Identification and characterization of phage variants of a strain of epidemic methicillin-resistant Staphylococcus aureus (EMRSA-15). J. Clin. Microbiol. 39, 1540–1548 (2001).
Knight, G. M. et al. Shift in dominant hospital-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) clones over time. J. Antimicrob. Chemother. 67, 2514–2522 (2012). The tendency of dominant MRSA strains to shift over time is well documented in this paper.
Johnson, A. P. Methicillin-resistant Staphylococcus aureus: the European landscape. J. Antimicrob. Chemother. 66, iv43–iv48 (2011).
Song, J. H. et al. Spread of methicillin-resistant Staphylococcus aureus between the community and the hospitals in Asian countries: an ANSORP study. J. Antimicrob. Chemother. 66, 1061–1069 (2011).
Arias, C. A. et al. A prospective cohort multicenter study of molecular epidemiology and phylogenomics of Staphylococcus aureus bacteremia in nine Latin American countries. Antimicrob. Agents Chemother. 61, e00816-17 (2017).
Blomfeldt, A., Eskesen, A. N., Aamot, H. V., Leegaard, T. M. & Bjornholt, J. V. Population-based epidemiology of Staphylococcus aureus bloodstream infection: clonal complex 30 genotype is associated with mortality. Eur. J. Clin. Microbiol. Infect. Dis. 35, 803–813 (2016).
Rolo, J. et al. High genetic diversity among community-associated Staphylococcus aureus in Europe: results from a multicenter study. PLOS ONE 7, e34768 (2012).
Xie, X. et al. Molecular epidemiology and characteristic of virulence gene of community-acquired and hospital-acquired methicillin-resistant Staphylococcus aureus isolates in Sun Yat-sen Memorial hospital, Guangzhou, Southern China. BMC Infect. Dis. 16, 339 (2016).
Otter, J. A. & French, G. L. Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Europe. Lancet Infect. Dis. 10, 227–239 (2010).
Chuang, Y. Y. & Huang, Y. C. Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Asia. Lancet Infect. Dis. 13, 698–708 (2013). This paper presents one of a series of molecular epidemiologic studies that has markedly expanded our understanding of MRSA genetic diversity in Asia, collectively demonstrating generally greater genetic diversity than is seen in the United States.
Liu, Y. et al. Molecular evidence for spread of two major methicillin-resistant Staphylococcus aureus clones with a unique geographic distribution in Chinese hospitals. Antimicrob. Agents Chemother. 53, 512–518 (2009).
Zhao, C. et al. Characterization of community acquired Staphylococcus aureus associated with skin and soft tissue infection in Beijing: high prevalence of PVL+ST398. PLOS ONE 7, e38577 (2012).
Harch, S. A. J. et al. High burden of complicated skin and soft tissue infections in the Indigenous population of Central Australia due to dominant Panton Valentine leucocidin clones ST93-MRSA and CC121-MSSA. BMC Infect. Dis. 17, 405 (2017).
Blomfeldt, A. et al. Bengal Bay clone ST772-MRSA-V outbreak: conserved clone causes investigation challenges. J. Hosp. Infect. 95, 253–258 (2017).
Casey, J. A. et al. High-density livestock production and molecularly characterized MRSA infections in Pennsylvania. Environ. Health Perspect. 122, 464–470 (2014). A strong example of the One Health approach probing the risk of MRSA infection acquired from livestock is presented.
Witte, W., Strommenger, B., Stanek, C. & Cuny, C. Methicillin-resistant Staphylococcus aureus ST398 in humans and animals, Central Europe. Emerg. Infect. Dis. 13, 255–258 (2007).
Smith, T. C. et al. Methicillin-resistant Staphylococcus aureus (MRSA) strain ST398 is present in midwestern U. S. swine and swine workers. PLOS ONE 4, e4258 (2009).
Sung, J. M., Lloyd, D. H. & Lindsay, J. A. Staphylococcus aureus host specificity: comparative genomics of human versus animal isolates by multi-strain microarray. Microbiology 154, 1949–1959 (2008).
Alam, M. T. et al. Transmission and microevolution of USA300 MRSA in U. S. households: evidence from whole-genome sequencing. mBio 6, e00054 (2015).
Diep, B. A. et al. Complete genome sequence of USA300, an epidemic clone of community-acquired meticillin-resistant Staphylococcus aureus. Lancet 367, 731–739 (2006).
Li, M. et al. Comparative analysis of virulence and toxin expression of global community-associated methicillin-resistant Staphylococcus aureus strains. J. Infect. Dis. 202, 1866–1876 (2010).
Holden, M. T. et al. A genomic portrait of the emergence, evolution, and global spread of a methicillin-resistant Staphylococcus aureus pandemic. Genome Res. 23, 653–664 (2013).
Gorwitz, R. J. et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001–2004. J. Infect. Dis. 197, 1226–1234 (2008).
Lekkerkerk, W. S. N. et al. Newly identified risk factors for MRSA carriage in The Netherlands. PLOS ONE 12, e0188502 (2017).
Lucet, J. C., Chevret, S., Durand-Zaleski, I., Chastang, C. & Regnier, B. Prevalence and risk factors for carriage of methicillin-resistant Staphylococcus aureus at admission to the intensive care unit: results of a multicenter study. Arch. Intern. Med. 163, 181–188 (2003).
Shet, A. et al. Colonization and subsequent skin and soft tissue infection due to methicillin-resistant Staphylococcus aureus in a cohort of otherwise healthy adults infected with HIV type 1. J. Infect. Dis. 200, 88–93 (2009).
Schechter-Perkins, E. M. et al. Prevalence and predictors of nasal and extranasal staphylococcal colonization in patients presenting to the emergency department. Ann. Emerg. Med. 57, 492–499 (2011).
Karanika, S., Kinamon, T., Grigoras, C. & Mylonakis, E. Colonization with methicillin-resistant Staphylococcus aureus and risk for infection among asymptomatic athletes: a systematic review and metaanalysis. Clin. Infect. Dis. 63, 195–204 (2016).
Cluzet, V. C. et al. Duration of colonization and determinants of earlier clearance of colonization with methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 60, 1489–1496 (2015).
Mollema, F. P. et al. Transmission of methicillin-resistant Staphylococcus aureus to household contacts. J. Clin. Microbiol. 48, 202–207 (2010).
Huang, S. S. et al. Strain-relatedness of methicillin-resistant Staphylococcus aureus isolates recovered from patients with repeated infection. Clin. Infect. Dis. 46, 1241–1247 (2008). This study shows that MRSA infection following either initial colonization or prior infection is most often caused by the same strain.
Calderwood, M. S. et al. Staphylococcal enterotoxin P predicts bacteremia in hospitalized patients colonized with methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 209, 571–577 (2014).
Patel, A. B., Hill, E., Simpson, E. L. & Hanifin, J. M. Reversion of methicillin-resistant Staphylococcus aureus skin infections to methicillin-susceptible isolates. JAMA Dermatol. 149, 1167–1171 (2013).
Iwase, T. et al. Staphylococcus epidermidis Esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Nature 465, 346–349 (2010).
Matheson, A. et al. Nasal swab screening for methicillin-resistant Staphylococcus aureus — how well does it perform? A cross-sectional study. Infect. Control Hosp. Epidemiol. 33, 803–808 (2012).
Kelley, P. G., Grabsch, E. A., Howden, B. P., Gao, W. & Grayson, M. L. Comparison of the Xpert methicillin-resistant Staphylococcus aureus (MRSA) assay, BD GeneOhm MRSA assay, and culture for detection of nasal and cutaneous groin colonization by MRSA. J. Clin. Microbiol. 47, 3769–3772 (2009).
Blanc, D. S. et al. High proportion of wrongly identified methicillin-resistant Staphylococcus aureus carriers by use of a rapid commercial PCR assay due to presence of staphylococcal cassette chromosome element lacking the mecA gene. J. Clin. Microbiol. 49, 722–724 (2011).
Warnke, P., Frickmann, H., Ottl, P. & Podbielski, A. Nasal screening for MRSA: different swabs—different results! PLOS ONE 9, e111627 (2014).
Shaw, A. G. et al. Detection of methicillin-resistant and methicillin-susceptible Staphylococcus aureus colonization of healthy military personnel by traditional culture, PCR, and mass spectrometry. Scand. J. Infect. Dis. 45, 752–759 (2013).
Currie, A. et al. Sensitivities of nasal and rectal swabs for detection of methicillin-resistant Staphylococcus aureus colonization in an active surveillance program. J. Clin. Microbiol. 46, 3101–3103 (2008).
Batra, R., Eziefula, A. C., Wyncoll, D. & Edgeworth, J. Throat and rectal swabs may have an important role in MRSA screening of critically ill patients. Intensive Care Med. 34, 1703–1706 (2008).
Gagnaire, J. et al. Epidemiology and clinical relevance of Staphylococcus aureus intestinal carriage: a systematic review and meta-analysis. Expert Rev. Anti Infect. Ther. 15, 767–785 (2017).
Mermel, L. A., Cartony, J. M., Covington, P., Maxey, G. & Morse, D. Methicillin-resistant Staphylococcus aureus colonization at different body sites: a prospective, quantitative analysis. J. Clin. Microbiol. 49, 1119–1121 (2011).
Lauderdale, T. L. et al. Carriage rates of methicillin-resistant Staphylococcus aureus (MRSA) depend on anatomic location, the number of sites cultured, culture methods, and the distribution of clonotypes. Eur. J. Clin. Microbiol. Infect. Dis. 29, 1553–1559 (2010).
McKinnell, J. A., Huang, S. S., Eells, S. J., Cui, E. & Miller, L. G. Quantifying the impact of extranasal testing of body sites for methicillin-resistant Staphylococcus aureus colonization at the time of hospital or intensive care unit admission. Infect. Control Hosp. Epidemiol. 34, 161–170 (2013).
Popovich, K. J. et al. Anatomic sites of colonization with community-associated methicillin-resistant Staphylococcus aureus. Infect. Control Hosp. Epidemiol. 35, 1192–1194 (2014).
Vos, M. C. et al. 5 years of experience implementing a methicillin-resistant Staphylococcus aureus search and destroy policy at the largest university medical center in the Netherlands. Infect. Control Hosp. Epidemiol. 30, 977–984 (2009).
Bartels, M. D., Kristoffersen, K., Boye, K. & Westh, H. Rise and subsequent decline of community-associated methicillin resistant Staphylococcus aureus ST30-IVc in Copenhagen, Denmark through an effective search and destroy policy. Clin. Microbiol. Infect. 16, 78–83 (2010).
Jain, R. et al. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N. Engl. J. Med. 364, 1419–1430 (2011). This study demonstrates that the implementation of a MRSA bundle that couples active surveillance with contact precautions and hand hygiene results in decreased rates of health-care-associated MRSA infections.
Robicsek, A. et al. Topical therapy for methicillin-resistant Staphylococcus aureus colonization: impact on infection risk. Infect. Control Hosp. Epidemiol. 30, 623–632 (2009).
Harbarth, S. et al. Universal screening for methicillin-resistant Staphylococcus aureus at hospital admission and nosocomial infection in surgical patients. JAMA 299, 1149–1157 (2008). This study shows no added benefit for universal, rapid MRSA admission screening strategy on nosocomial MRSA infection rates in a surgical department.
Saraswat, M. K. et al. Preoperative Staphylococcus aureus screening and targeted decolonization in cardiac surgery. Ann. Thorac. Surg. 104, 1349–1356 (2017).
Jog, S. et al. Impact of preoperative screening for meticillin-resistant Staphylococcus aureus by real-time polymerase chain reaction in patients undergoing cardiac surgery. J. Hosp. Infect. 69, 124–130 (2008).
Huang, S. S. et al. Targeted versus universal decolonization to prevent ICU infection. N. Engl. J. Med. 368, 2255–2265 (2013). This large multicentre study shows that universal decolonization is more effective than targeted decolonization or screening and isolation in reducing rates of MRSA clinical isolates and bloodstream infection in patients in the ICU.
Climo, M. W. et al. Effect of daily chlorhexidine bathing on hospital-acquired infection. N. Engl. J. Med. 368, 533–542 (2013). This study shows that daily bathing with chlorhexidine reduces the risks of acquisition of multidrug-resistant organisms and hospital-acquired bloodstream infections.
Lindgren, A. K., Nilsson, A. C., Akesson, P., Gustafsson, E. & Melander, E. Eradication of methicillin-resistant Staphylococcus aureus (MRSA) throat carriage: a randomised trial comparing topical treatment with rifampicin-based systemic therapy. Int. J. Antimicrob. Agents 51, 642–645 (2017).
Kaasch, A. J. et al. Use of a simple criteria set for guiding echocardiography in nosocomial Staphylococcus aureus bacteremia. Clin. Infect. Dis. 53, 1–9 (2011).
Mermel, L. A. et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 49, 1–45 (2009).
Neely, M. N. et al. Are vancomycin trough concentrations adequate for optimal dosing? Antimicrob. Agents Chemother. 58, 309–316 (2014).
van Hal, S. J., Lodise, T. P. & Paterson, D. L. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin. Infect. Dis. 54, 755–771 (2012).
Fowler, V. G. Jr. et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N. Engl. J. Med. 355, 653–665 (2006). This is one of very few RCTs addressing the treatment of MRSA bacteraemia or endocarditis, proving daptomycin is non-inferior to vancomycin.
Silverman, J. A., Mortin, L. I., Vanpraagh, A. D., Li, T. & Alder, J. Inhibition of daptomycin by pulmonary surfactant: in vitro modeling and clinical impact. J. Infect. Dis. 191, 2149–2152 (2005).
Sharma, M., Riederer, K., Chase, P. & Khatib, R. High rate of decreasing daptomycin susceptibility during the treatment of persistent Staphylococcus aureus bacteremia. Eur. J. Clin. Microbiol. Infect. Dis. 27, 433–437 (2008).
Gasch, O. et al. Emergence of resistance to daptomycin in a cohort of patients with methicillin-resistant Staphylococcus aureus persistent bacteraemia treated with daptomycin. J. Antimicrob. Chemother. 69, 568–571 (2014).
Stryjewski, M. E. et al. A randomized Phase 2 trial of telavancin versus standard therapy in patients with uncomplicated Staphylococcus aureus bacteremia: the ASSURE study. BMC Infect. Dis. 14, 289 (2014).
Raad, I. et al. Efficacy and safety of weekly dalbavancin therapy for catheter-related bloodstream infection caused by gram-positive pathogens. Clin. Infect. Dis. 40, 374–380 (2005).
Wilcox, M. H. et al. Complicated skin and skin-structure infections and catheter-related bloodstream infections: noninferiority of linezolid in a phase 3 study. Clin. Infect. Dis. 48, 203–212 (2009).
Casapao, A. M. et al. Large retrospective evaluation of the effectiveness and safety of ceftaroline fosamil therapy. Antimicrob. Agents Chemother. 58, 2541–2546 (2014).
Davis, J. S. et al. Combination of vancomycin and beta-lactam therapy for methicillin-resistant Staphylococcus aureus bacteremia: a pilot multicenter randomized controlled trial. Clin. Infect. Dis. 62, 173–180 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02365493 (2018).
Thwaites, G. E. et al. Adjunctive rifampicin for Staphylococcus aureus bacteraemia (ARREST): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 391, 668–678 (2017). One of the few existing RCTs assessing the treatment of MRSA bacteraemia, ARREST finds no decrease in mortality with combination therapy including rifampin.
Cosgrove, S. E. et al. Initial Low-dose Gentamicin for Staphylococcus aureus Bacteremia and Endocarditis Is Nephrotoxic. Clinical Infectious Diseases 2009; 199: 201-8.
Rehm, S. J. et al. Daptomycin versus vancomycin plus gentamicin for treatment of bacteraemia and endocarditis due to Staphylococcus aureus: subset analysis of patients infected with methicillin-resistant isolates. J. Antimicrob. Chemother. 62, 1413–1421 (2008).
Liu, C. et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 52, e18–e55 (2011).
Holland, T. L. et al. Effect of algorithm-based therapy versus usual care on clinical success and serious adverse events in patients with staphylococcal bacteremia: a randomized clinical trial. JAMA 320, 1249–1258 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01792804 (2018).
Tissot, F. et al. Mandatory infectious diseases consultation for MRSA bacteremia is associated with reduced mortality. J. Infect. 69, 226–234 (2014).
Jenkins, T. C., Price, C. S., Sabel, A. L., Mehler, P. S. & Burman, W. J. Impact of routine infectious diseases service consultation on the evaluation, management, and outcomes of Staphylococcus aureus bacteremia. Clin. Infect. Dis. 46, 1000–1008 (2008).
Baddour, L. M. et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 132, 1435–1486 (2015).
Kang, D. H. et. al. Early surgery versus conventional treatment for infective endocarditis. N. Engl. J. Med. 366, 2466–2473 (2012).
Martinez-Aguilar, G., Hammerman, W. A., Mason, E. O. Jr & Kaplan, S. L. Clindamycin treatment of invasive infections caused by community-acquired, methicillin-resistant and methicillin-susceptible Staphylococcus aureus in children. Pediatr. Infect. Dis. J. 22, 593–598 (2003).
Wunderink, R. G. et al. Linezolid in methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a randomized, controlled study. Clin. Infect. Dis. 54, 621–629 (2012).
Conte, J. E. Jr., Golden, J. A., Kipps, J. & Zurlinden, E. Intrapulmonary pharmacokinetics of linezolid. Antimicrob. Agents Chemother. 46, 1475–1480 (2002).
Kalil, A. C. et al. Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: a systematic review and meta-analysis. Crit. Care Med. 38, 1802–1808 (2010).
Dombrowski, J. C. & Winston, L. G. Clinical failures of appropriately-treated methicillin-resistant Staphylococcus aureus infections. J. Infect. 57, 110–115 (2008).
Moenster, R. P., Linneman, T. W., Finnegan, P. M. & McDonald, J. R. Daptomycin compared to vancomycin for the treatment of osteomyelitis: a single-center, retrospective cohort study. Clin. Ther. 34, 1521–1527 (2012).
Gallagher, J. C. et al. Daptomycin therapy for osteomyelitis: a retrospective study. BMC Infect. Dis. 12, 133 (2012).
Seaton, R. A. et al. Daptomycin use in patients with osteomyelitis: a preliminary report from the EU-CORE(SM) database. J. Antimicrob. Chemother. 68, 1642–1649 (2013).
Senneville, E. et al. Effectiveness and tolerability of prolonged linezolid treatment for chronic osteomyelitis: a retrospective study. Clin. Ther. 28, 1155–1163 (2006).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03009045 (2018).
Feigin, R. D., Pickering, L. K., Anderson, D., Keeney, R. E. & Shackleford, P. G. Clindamycin treatment of osteomyelitis and septic arthritis in children. Pediatrics 55, 213–223 (1975).
Daver, N. G. et al. Oral step-down therapy is comparable to intravenous therapy for Staphylococcus aureus osteomyelitis. J. Infect. 54, 539–544 (2007).
Park, K. H. et al. Optimal duration of antibiotic therapy in patients with hematogenous vertebral osteomyelitis at low risk and high risk of recurrence. Clin. Infect. Dis. 62, 1262–1269 (2016).
Bejon, P. et al. Two-stage revision for prosthetic joint infection: predictors of outcome and the role of reimplantation microbiology. J. Antimicrob. Chemother. 65, 569–575 (2010).
Zimmerli, W., Trampuz, A. & Ochsner, P. E. Prosthetic-joint infections. N. Engl. J. Med. 351, 1645–1654 (2004).
Lora-Tamayo, J. et al. A large multicenter study of methicillin-susceptible and methicillin-resistant Staphylococcus aureus prosthetic joint infections managed with implant retention. Clin. Infect. Dis. 56, 182–194 (2013).
Westberg, M., Grogaard, B. & Snorrason, F. Early prosthetic joint infections treated with debridement and implant retention: 38 primary hip arthroplasties prospectively recorded and followed for median 4 years. Acta Orthop. 83, 227–232 (2012).
Daum, R. S. et al. A placebo-controlled trial of antibiotics for smaller skin abscesses. N. Engl. J. Med. 376, 2545–2555 (2017). This is one of the most recent studies to address the need for antibiotics following incision and drainage of a cutaneous abscess. This study finds a reduced risk of recurrence for those receiving oral antibiotics following abscess drainage.
Holland, T. L. et al. A phase 3, randomized, double-blind, multicenter study to evaluate the safety and efficacy of intravenous iclaprim versus vancomycin for treatment of acute bacterial skin and skin structure infections suspected or confirmed to be due to Gram-positive pathogens (REVIVE-2 study). Antimicrob. Agents Chemother. 62, e02580-17 (2018).
Huang, D. B. et al. A phase 3, randomized, double-blind, multicenter study to evaluate the safety and efficacy of intravenous iclaprim vs vancomycin for the treatment of acute bacterial skin and skin structure infections suspected or confirmed to be due to Gram-positive pathogens: REVIVE-1. Clin. Infect. Dis. 66, 1222–1229 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02877927 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02426918 (2018).
Corey, G. R. et al. Single-dose oritavancin in the treatment of acute bacterial skin infections. N. Engl. J. Med. 370, 2180–2190 (2014).
Boucher, H. W. et al. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N. Engl. J. Med. 370, 2169–2179 (2014).
Dunne, M. W. et al. A randomized clinical trial of single-dose versus weekly dalbavancin for treatment of acute bacterial skin and skin structure infection. Clin. Infect. Dis. 62, 545–551 (2016).
Shinefield, H. et al. Use of a conjugate vaccine in patients receiving hemodialysis. N. Engl. J. Med. 346, 491–496 (2002).
Giersing, B. K., Dastgheyb, S. S., Modjarrad, K. & Moorthy, V. Status of vaccine research and development of vaccines for Staphylococcus aureus. Vaccine 34, 2962–2966 (2016).
Rutherford, K. et al. Artemis: sequence visualization and annotation. Bioinformatics 16, 944–945 (2000).
Omuse, G. et al. Molecular characterization of Staphylococcus aureus isolates from various healthcare institutions in Nairobi, Kenya: a cross sectional study. Ann. Clin. Microbiol. Antimicrob. 15, (51 (2016).
Xiao, M. et al. National surveillance of methicillin-resistant Staphylococcus aureus in China highlights a still-evolving epidemiology with 15 novel emerging multilocus sequence types. J. Clin. Microbiol. 51, 3638–3644 (2013).
Kang, G. S. et al. Prevalence of major methicillin-resistant Staphylococcus aureus clones in Korea between 2001 and 2008. Ann. Lab. Med. 36, 536–541 (2016).
Gostev, V. et al. Molecular epidemiology and antibiotic resistance of methicillin-resistant Staphylococcus aureus circulating in the Russian Federation. Infect. Genet. Evol. 53, 189–194 (2017).
Drougka, E. et al. A 12-year survey of methicillin-resistant Staphylococcus aureus infections in Greece: ST80-IV epidemic? Clin. Microbiol. Infect. 20, 796–803 (2014).
Udo, E. E. & Sarkhoo, E. The dissemination of ST80-SCCmec-IV community-associated methicillin resistant Staphylococcus aureus clone in Kuwait hospitals. Ann. Clin. Microbiol. Antimicrob. 9, 31 (2010).
David, M. Z. et al. Comparing pulsed-field gel electrophoresis with multilocus sequence typing, spa typing, staphylococcal cassette chromosome mec (SCCmec) typing, and PCR for Panton-Valentine leukocidin, arcA, and opp3 in methicillin-resistant Staphylococcus aureus isolates at a US Medical Center. J. Clin. Microbiol. 51, 814–819 (2013).
Diekema, D. J. et al. Continued emergence of USA300 methicillin-reistant Staphylococcus aureus in the United States: results from a nationwide surveillance study. Infect. Control Hosp. Epidemiol. 35, 285–292 (2014).
Nichol, K. A. et al. Changing epidemiology of methicillin-resistant Staphylococcus aureus in Canada. J. Antimicrob. Chemother. 68, 47–55 (2013).
Sharma-Kuinkel, B. K. et al. Potential influence of Staphylococcus aureus clonal complex 30 genotype and transcriptome on hematogenous infections. Open Forum Infect. Dis. 2, ofv093 (2015).
Kuroda, M. et al. Whole genome sequencing of meticillin-resistant Staphylococcus aureus. Lancet 357, 1225–1240 (2001).
Holden, M. T. et al. Complete genomes of two clinical Staphylococcus aureus strains: evidence for the rapid evolution of virulence and drug resistance. Proc. Natl Acad. Sci. USA 101, 9786–9791 (2004).
Sharma-Kuinkel, B. K., Rude, T. H. & Fowler, V. G. Jr. Pulse field gel electrophoresis. Methods Mol. Biol. 1373, 117–130 (2016).
Blanc, D. S., Francioli, P. & Hauser, P. M. Poor value of pulsed-field gel electrophoresis to investigate long-term scale epidemiology of methicillin-resistant Staphylococcus aureus. Infect. Genet. Evol. 2, 145–148 (2002).
Enright, M. C., Day, N. P., Davies, C. E., Peacock, S. J. & Spratt, B. G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 38, 1008–1015 (2000).
O’Hara, F. P. et al. spa typing and multilocus sequence typing show comparable performance in a macroepidemiologic study of Staphylococcus aureus in the United States. Microb. Drug Resist. 22, 88–96 (2016).
Mathema, B., Mediavilla, J. & Kreiswirth, B. N. Sequence analysis of the variable number tandem repeat in Staphylococcus aureus protein A gene: spa typing. Methods Mol. Biol. 431, 285–305 (2008).
Brandt, K. M. et al. Evaluation of multiple-locus variable number of tandem repeats analysis for typing livestock-associated methicillin-resistant Staphylococcus aureus. PLOS ONE 8, e54425 (2013).
Garcia-Alvarez, L. et al. Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: a descriptive study. Lancet Infect. Dis. 11, 595–603 (2011).
Ross, T. L., Merz, W. G., Farkosh, M. & Carroll, K. C. Comparison of an automated repetitive sequence-based PCR microbial typing system to pulsed-field gel electrophoresis for analysis of outbreaks of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 43, 5642–5647 (2005).
Salipante, S. J. et al. Application of whole-genome sequencing for bacterial strain typing in molecular epidemiology. J. Clin. Microbiol. 53, 1072–1079 (2015).
Cramton, S. E., Schnell, N. F., Gotz, F. & Bruckner, R. Identification of a new repetitive element in Staphylococcus aureus. Infect. Immun. 68, 2344–2348 (2000).
Quelle, L. S., Corso, A., Galas, M. & Sordelli, D. O. STAR gene restriction profile analysis in epidemiological typing of methicillin-resistant Staphylococcus aureus: description of the new method and comparison with other polymerase chain reaction (PCR)-based methods. Diagn. Microbiol. Infect. Dis. 47, 455–464 (2003).
Climo, M. W. et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit. Care Med. 37, 1858–1865 (2009).
Robicsek, A. et al. Universal surveillance for methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Ann. Intern. Med. 148, 409–418 (2008).
Dillon, H. C. & Derrick, C. W. Clinical experience with clindamycin hydrochloride: I. Treatment of streptococcal and mixed streptococcal-staphylococcal skin infections. Pediatrics 55, 205–212 (1975).
Frank, A. L., Marcinak, J. F., Mangat, P. D. & Schreckenberger, P. C. Community-acquired and clindamycin-susceptible methicillin-resistant Staphylococcus aureus in children. Pediatr. Infect. Dis. J. 18, 993–1000 (1999).
Arbeit, R. D., Maki, D., Tally, F. P., Campanaro, E. & Eisenstein, B. I. The safety and efficacy of daptomycin for the treatment of complicated skin and skin-structure infections. Clin. Infect. Dis. 38, 1673–1681 (2004).
Byren, I. et al. Randomized controlled trial of the safety and efficacy of Daptomycin versus standard-of-care therapy for management of patients with osteomyelitis associated with prosthetic devices undergoing two-stage revision arthroplasty. Antimicrob. Agents Chemother. 56, 5626–5632 (2012).
Weigelt, J. et al. Linezolid versus vancomycin in treatment of complicated skin and soft tissue infections. Antimicrob. Agents Chemother. 49, 2260–2266 (2005).
Shorr, A. F. et al. Analysis of the phase 3 ESTABLISH trials of tedizolid versus linezolid in acute bacterial skin and skin structure infections. Antimicrob. Agents Chemother. 59, 864–871 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02019420 (2018).
Ramani, A. et al. Contemporary use of ceftaroline fosamil for the treatment of community-acquired bacterial pneumonia: CAPTURE study experience. J. Chemother. 26, 229–234 (2014).
Corey, G. R. et al. Integrated analysis of CANVAS 1 and 2: phase 3, multicenter, randomized, double-blind studies to evaluate the safety and efficacy of ceftaroline versus vancomycin plus aztreonam in complicated skin and skin-structure infection. Clin. Infect. Dis. 51, 641–650 (2010).
Burnett, Y. J., Echevarria, K. & Traugott, K. A. Ceftaroline as salvage monotherapy for persistent MRSA bacteremia. Ann. Pharmacother. 50, 1051–1059 (2016).
Polenakovik, H. M. & Pleiman, C. M. Ceftaroline for meticillin-resistant Staphylococcus aureus bacteraemia: case series and review of the literature. Int. J. Antimicrob. Agents 42, 450–455 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02335905 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01645735 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01701219 (2014).
Awad, S. S. et al. A phase 3 randomized double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia. Clin. Infect. Dis. 59, 51–61 (2014).
Noel, G. J., Bush, K., Bagchi, P., Ianus, J. & Strauss, R. S. A randomized, double-blind trial comparing ceftobiprole medocaril with vancomycin plus ceftazidime for the treatment of patients with complicated skin and skin-structure infections. Clin. Infect. Dis. 46, 647–655 (2008).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03138733 (2018).
Rubinstein, E. et al. Telavancin versus vancomycin for hospital-acquired pneumonia due to gram-positive pathogens. Clin. Infect. Dis. 52, 31–40 (2011).
Stryjewski, M. E. et al. Telavancin versus vancomycin for the treatment of complicated skin and skin-structure infections caused by gram-positive organisms. Clin. Infect. Dis. 46, 1683–1693 (2008).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02208063 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03426761 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02679573 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03148756 (2018).
Nichols, R. L. et al. Treatment of hospitalized patients with complicated gram-positive skin and skin structure infections: two randomized, multicentre studies of quinupristin/dalfopristin versus cefazolin, oxacillin or vancomycin. Synercid Skin and Skin Structure Infection Group. J. Antimicrob. Chemother. 44, 263–273 (1999).
Fagon, J. et al. Treatment of gram-positive nosocomial pneumonia. Prospective randomized comparison of quinupristin/dalfopristin versus vancomycin. Nosocomial Pneumonia Group. Am. J. Respir. Crit. Care Med. 161, 753–762 (2000).
Tanaseanu, C. et al. Integrated results of 2 phase 3 studies comparing tigecycline and levofloxacin in community-acquired pneumonia. Diagn. Microbiol. Infect. Dis. 61, 329–338 (2008).
Ellis-Grosse, E. J., Babinchak, T., Dartois, N., Rose, G. & Loh, E. The efficacy and safety of tigecycline in the treatment of skin and skin-structure infections: results of 2 double-blind phase 3 comparison studies with vancomycin-aztreonam. Clin. Infect. Dis. 41 (Suppl. 5), 341–353 (2005).
Gardiner, D., Dukart, G., Cooper, A. & Babinchak, T. Safety and efficacy of intravenous tigecycline in subjects with secondary bacteremia: pooled results from 8 phase III clinical trials. Clin. Infect. Dis. 50, 229–238 (2010).
Shen, F. et al. Efficacy and safety of tigecycline for the treatment of severe infectious diseases: an updated meta-analysis of RCTs. Int. J. Infect. Dis. 39, 25–33 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02253342 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02244827 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01875939 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02217930 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02052388 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01211470 (2012).
Acknowledgements
N.A.T. and T.L.H. were supported, in part, by an Antibacterial Resistance Leadership Group fellowship (National Institute of Allergy and Infectious Diseases, UM1AI104681, from the National Institutes of Health). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. S.A.M. was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (1KL2TR002554). V.G.F. was supported by U01 AI-124319-01, 2R01-AI068804 and K24-AI093969, from the National Institutes of Health.
Reviewer information
Nature Reviews Microbiology thanks M. Otto and other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
T.L.H. has been a consultant for Basilea Pharmaceutica, Genentech, The Medicines Company, Motif Biosciences and Theravance Biopharma and has received grant support from Basilea Pharmaceutica and Achaogen. V.G.F. served as Chair of the V710 Scientific Advisory Committee (Merck); has received grant support from Cerexa/Actavis/Allergan, Pfizer, Advanced Liquid Logics, National Institutes of Health (NIH), MedImmune, Basilea Pharmaceutica, Karius, ContraFect, Regeneron Pharmaceuticals and Genentech; has NIH STTR/SBIR grants pending with Affinergy, Locus and Medical Surface; has been a consultant for Achaogen, AmpliPhi Biosciences, Astellas Pharma, Arsanis, Affinergy, Basilea Pharmaceutica, Bayer, Cerexa, ContraFect, Cubist, Debiopharm, Destiny Pharmaceuticals, Durata Therapeutics, Grifols, Genentech, MedImmune, Merck, The Medicines Company, Pfizer, Novartis, NovaDigm Therapeutics, Theravance Biopharma, XBiotech and Integrated BioTherapeutics; has received honoraria from Theravance Biopharma and Green Cross; and has a patent pending in sepsis diagnostics.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinicalTrials.gov database: https://clinicaltrials.gov/
Glossary
- Endocarditis
-
An infection of the interior heart structures or valves.
- Osteomyelitis
-
An infection involving bone.
- Methicillin
-
An anti-staphylococcal penicillin.
- Fomite
-
An object or material capable of carrying or transmitting infection.
- Echocardiography
-
A diagnostic imaging technique in which ultrasound is used to construct images of heart chambers, valves and associated structures.
- Mobile genetic elements
-
Segments of DNA-encoding enzymes that mediate transfer of DNA within and between bacterial genomes.
- Clindamycin
-
An antibiotic in the lincosamide family.
- Methicillin-susceptible Staphylococcus aureus
-
(MSSA). Staphylococcus aureus strains that are susceptible to methicillin, oxacillin and cefoxitin.
- Minimum inhibitory concentrations
-
(MICs). The lowest concentration of a chemical at which bacterial growth is prevented.
- Competent
-
Refers to bacteria capable of taking up DNA from their environment for recombination.
- Hyaluronidase
-
An enzyme that catalyses the degradation of hyaluronic acid; it may play a role in pathogenesis by facilitating the breakdown of host intercellular matrix.
- Arginine-catabolic mobile element
-
(ACME). A mobile genetic element that accompanies staphylococcal cassette chromosome mec (SCCmec) and is believed to have a role in the regulation of growth and survival in Staphylococcus aureus and strain fitness.
- Panton–Valentine leukocidin
-
(PVL). A cytotoxin produced by some strains of Staphylococcus aureus that induces pore formation in the membranes of white blood cells, resulting in cell lysis.
- att s sites
-
Sites targeted by the staphylococcal cassette recombinases.
- Gene nurseries
-
Regions of the genome from which other genes are believed to have originated.
- Phenol-soluble modulin
-
(PSM). A peptide toxin that attracts and lyses white blood cells.
- One Health approach
-
An integrative approach to medicine that recognizes connections between animal, environmental and human health.
- Mupirocin
-
A topical antibiotic with activity against S. aureus.
- Transoesophageal
-
A technique for echocardiography in which the echo probe is positioned within the oesophagus, providing much higher resolution imaging of select heart structures.
- Transthoracic
-
The standard, non-invasive method for echocardiographic imaging of the heart by applying the echo probe to the external chest wall.
- Non-inferior
-
In the specific context of clinical trials, a statistical definition by which an intervention is determined to be no worse than its comparator within a pre-specified range.
- Pulmonary surfactant
-
A lipoprotein substance secreted by the lungs that reduces surface tension and thus prevents collapse of alveoli.
- Modified intention-to-treat analysis
-
A variation on the traditional analysis of clinical trial results in which some subset of patients are excluded after randomization; there is no single definition for how this exclusion occurs, and there is some risk of introduction of bias.
- Embolization
-
The occlusion of a blood vessel by a material travelling within the bloodstream; this may be caused by clot (that is, thrombus) or infectious material.
- Pharmacokinetics
-
The study of the movement and distribution of medications within the body.
- Myelosuppression
-
The inhibition of bone marrow activity resulting in decreased red blood cells, white blood cells and platelets.
- Neuropathy
-
The dysfunction or disease of the peripheral nerves.
- Two-stage exchange arthroplasty
-
A method of joint replacement in which the original infected artificial joint is removed in one operation, antibiotic treatment is given and re-implantation of a new artificial joint is performed at a later date.
- Parenteral
-
Administered by a route other than the gastrointestinal tract; in general, refers to intravenous or injection therapies.
- Haematogenous
-
Blood-borne or carried within the bloodstream.
Rights and permissions
About this article
Cite this article
Turner, N.A., Sharma-Kuinkel, B.K., Maskarinec, S.A. et al. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol 17, 203–218 (2019). https://doi.org/10.1038/s41579-018-0147-4
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41579-018-0147-4
This article is cited by
-
Genomic and epidemiological insights into the emergence and dominance of MRSA clones in Riyadh’s healthcare facilities
Scientific Reports (2026)
-
Iterative discovery of potent polymeric antibiotics via multi-stage and multi-task learning against antimicrobial resistance
Nature Communications (2026)
-
Genomics reveal Staphylococcus aureus persists during long-term urinary catheterization despite antimicrobial therapy and catheter exchanges
Nature Communications (2026)
-
Injectable hydrogels for osteomyelitis treatment induce metabolic reprogramming for protection against reinfection
Nature Communications (2026)
-
Molecular Framework of Multidrug Resistance in Pseudomonas aeruginosa
Current Microbiology (2026)