Abstract
According to the MS International Federation, the global prevalence of multiple sclerosis (MS) is increasing, although regional variations have been reported, which could provide valuable insights into MS pathophysiology. As we highlight in this Review, the prevalence of MS in Latin America is comparatively low, possibly owing at least in part to the unique genetic and environmental characteristics of this region. Latin America has experienced centuries of admixture between Native American Indian populations and people from other parts of the world, including Europe and — to a lesser extent — Africa. Moreover, certain environmental factors in the Southern Hemisphere might contribute to this reduced MS prevalence. The McDonald criteria are considered to be a useful tool to diagnose MS in Latin America, although it is important to exclude regional diseases that can mimic MS. MS research is burgeoning in the region, and increasing numbers of Latin American patients are participating in randomized clinical trials. In addition, real-world data from national and regional MS registries are helping us to understand the distinct features of the disease in Latin America.
Key points
-
The prevalence of multiple sclerosis (MS) in Latin America is low-to-medium but is increasing, influenced by the region’s unique genetic admixture and specific environmental factors.
-
The clinical presentation of MS in Latin America is largely similar to that in high-prevalence regions.
-
The adoption of the McDonald criteria has reduced diagnostic delays; however, accurate diagnosis requires careful exclusion of MS mimics.
-
Profound disparities in health-care access, rooted in social determinants of health, substantially affect diagnosis, treatment and outcomes.
-
Collaborative research networks and real-world data from regional registries are crucial to provide insights into the distinct features of MS in Latin America and help address the historical under-representation of this population in clinical trials.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Walton, C. et al. Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS, third edition. Mult. Scler. J. 26, 1816–1821 (2020).
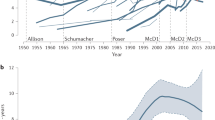
Negrotto, L. & Correale, J. Evolution of multiple sclerosis prevalence and phenotype in Latin America. Mult. Scler. Relat. Disord. 22, 97–102 (2018).
United Sstates Census Bureau. Hispanic Heritage Month: 2023. US Census Bureau https://www.census.gov/newsroom/facts-for-features/2023/hispanic-heritage-month.html#:~:Text=In%201968%2C%20Congress%20set%20aside,%2C%20Guatemala%2C%20Honduras%20and%20Nicaragua (2023).
Miranda-Acuña, J., Casallas-Vanegas, A., McCauley, J., Castro-Castro, P. & Amezcua, L. Multiple sclerosis in Colombia: a review of the literature. Mult. Scler. J. Exp. Transl. Clin. 10, 20552173241293921 (2024).
Gonzales-Gamarra, O. et al. Multiple sclerosis in Peru: national prevalence study using capture-recapture analysis. Mult. Scler. Relat. Disord. 55, 103147 (2021).
Rojas, J. I., Romano, M., Patrucco, L. & Cristiano, E. A systematic review about the epidemiology of primary progressive multiple sclerosis in Latin America and the Caribbean. Mult. Scler. Relat. Disord. 22, 1–7 (2018).
Cristiano, E. & Rojas, J. I. Multiple sclerosis epidemiology in Latin America: an updated survey. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317715050 (2017).
Sánchez, J. L. et al. Prevalence of multiple sclerosis in Colombia [Spanish]. Rev. Neurol. 31, 1101–1103 (2000).
Cristiano, E. et al. Increasing incidence of multiple sclerosis among women in Buenos Aires: a 22 year health maintenance organization based study. Neurol. Sci. 37, 1621–1626 (2016).
Callegaro, D. et al. The prevalence of multiple sclerosis in the city of São Paulo, Brazil, 1997: prevalence of MS in São Paulo, Brazil. Acta Neurol. Scand. 104, 208–213 (2001).
Gracia, F. et al. Prevalence and incidence of multiple sclerosis in Panama (2000–2005). Neuroepidemiology 32, 287–293 (2009).
Correa, E., Paredes, V. & Martínez, B. Prevalence of multiple sclerosis in Latin America and its relationship with European migration. Mult. Scler. J. Exp. Transl. Clin. 2, 2055217316666407 (2016).
Vasconcelos, C. C. F., Thuler, L. C. S., Rodrigues, B. C., Calmon, A. B. & Alvarenga, R. M. P. Multiple sclerosis in Brazil: a systematic review. Clin. Neurol. Neurosurg. 151, 24–30 (2016).
Ojeda, E. et al. Prevalence and clinical features of multiple sclerosis in Latin America. Clin. Neurol. Neurosurg. 115, 381–387 (2013).
Aguirre-Cruz, L., Flores-Rivera, J., De La Cruz-Aguilera, D. L., Rangel-López, E. & Corona, T. Multiple sclerosis in Caucasians and Latino Americans. Autoimmunity 44, 571–575 (2011).
Miller, D. H. & Leary, S. M. Primary-progressive multiple sclerosis. Lancet Neurol. 6, 903–912 (2007).
Cristiano, E. et al. The epidemiology of multiple sclerosis in Latin America and the Caribbean: a systematic review. Mult. Scler. J. 19, 844–854 (2013).
Cabre, P. et al. Role of return migration in the emergence of multiple sclerosis in the French West Indies. Brain 128, 2899–2910 (2005).
Rojas, J. I. et al. Gender ratio trends over time in multiple sclerosis patients from Argentina. J. Clin. Neurosci. 38, 84–86 (2017).
Orton, S.-M. et al. Sex ratio of multiple sclerosis in Canada: a longitudinal study. Lancet Neurol. 5, 932–936 (2006).
Ventura, R. E., Antezana, A. O., Bacon, T. & Kister, I. Hispanic Americans and African Americans with multiple sclerosis have more severe disease course than Caucasian Americans. Mult. Scler. J. 23, 1554–1557 (2017).
Aurenção, J. C. K., Vasconcelos, C. C. F., Thuler, L. C. S. & Alvarenga, R. M. P. Disability and progression in Afro-descendant patients with multiple sclerosis. Arq. Neuropsiquiatr. 74, 836–841 (2016).
Amezcua, L. et al. Person-centered social determinants and neighborhood-level deprivation associated with disability in Hispanic people with multiple sclerosis. Neurology 104, e213332 (2025).
Melcon, M. et al. Argentine Patagonia: prevalence and clinical features of multiple sclerosis. Mult. Scler. J. 14, 656–662 (2008).
Díaz, V. et al. Incidence of multiple sclerosis in Chile. A hospital registry study: incidence of multiple sclerosis in Chile. Acta Neurol. Scand. 125, 71–75 (2012).
Risco, J. et al. Latitudinal prevalence gradient of multiple sclerosis in Latin America. Mult. Scler. J. 17, 1055–1059 (2011).
Lett, E., Asabor, E., Beltrán, S., Cannon, A. M. & Arah, O. A. Conceptualizing, contextualizing, and operationalizing race in quantitative health sciences research. Ann. Fam. Med. 20, 157–163 (2022).
Ontaneda, D. & Amezcua, L. Re-thinking race and geography in multiple sclerosis. Mult. Scler. J. 30, 16–18 (2024).
Griffith, D. M., Towfighi, A., Manson, S. M., Littlejohn, E. L. & Skolarus, L. E. Determinants of inequities in neurologic disease, health, and well-being: the NINDS Social Determinants of Health Framework. Neurology 101, S75–S81 (2023).
Papais-Alvarenga, R. M. et al. Central nervous system idiopathic inflammatory demyelinating disorders in South Americans: a descriptive, multicenter, cross-sectional study. PLoS ONE 10, e0127757 (2015).
Vanotti, S. & Caceres, F. J. Cognitive and neuropsychiatric disorders among MS patients from Latin America. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317717508 (2017).
Rodrigues De Moura, R., Coelho, A. V. C., De Queiroz Balbino, V., Crovella, S. & Brandão, L. A. C. Meta-analysis of Brazilian genetic admixture and comparison with other Latin America countries. Am. J. Hum. Biol. 27, 674–680 (2015).
Durand, J. & Massey, D. S. New world orders: continuities and changes in Latin American migration. Ann. Am. Acad. Pol. Soc. Sci. 630, 20–52 (2010).
Krausz, L. S. & Stavans, I. From the “Land of the Future”: how Latin American Jews became global. J. Mod. Jew. Stud. 23, 107–125 (2024).
Sánchez-Alonso, B. The age of mass migration in Latin America. Econ. Hist. Rev 72, 3–31 (2019).
Jacobs, B. M. et al. Towards a global view of multiple sclerosis genetics. Nat. Rev. Neurol. 18, 613–623 (2022).
Comini-Frota, E. R. et al. Frequency of reported European ancestry among multiple sclerosis patients from four cities in the southern and southeastern regions of Brazil. Clin. Neurol. Neurosurg. 115, 1642–1646 (2013).
Gracia, F. et al. Multiple sclerosis in central America and Caribbean countries: frequency and clinical characterization of an emergent disease. Front. Epidemiol. 4, 1368675 (2024).
Flores, J. et al. Absence of multiple sclerosis and demyelinating diseases among Lacandonians, a pure Amerindian ethnic group in Mexico. Mult. Scler. Int. 2012, 292631 (2012).
Caballero, A. et al. DQB1*0602 confers genetic susceptibility to multiple sclerosis in Afro-Brazilians. Tissue Antigens 54, 524–526 (1999).
Al Jumah, M. et al. HLA class II polymorphism in Saudi patients with multiple sclerosis. HLA 91, 17–22 (2018).
Fernández, O. et al. DQB1*0602 allele shows a strong association with multiple sclerosis in patients in Malaga, Spain. J. Neurol. 251, 440–444 (2004).
Fernández, O. et al. HLA class II alleles in patients with multiple sclerosis in the Biscay province (Basque Country, Spain). J. Neurol. 256, 1977–1988 (2009).
Michalik, J. et al. The association of HLA-DRB1 and HLA-DQB1 alleles with genetic susceptibility to multiple sclerosis in the Slovak population. Neurol. Res. 37, 1060–1067 (2015).
Ordoñez, G. et al. Genomewide admixture study in Mexican Mestizos with multiple sclerosis. Clin. Neurol. Neurosurg. 130, 55–60 (2015).
Patrucco, L. et al. HLA-DRB1 and multiple sclerosis in Argentina. Eur. J. Neurol. 16, 427–429 (2009).
Toro, J. et al. HLA-DRB1*14 is a protective allele for multiple sclerosis in an admixed Colombian population. Neurol. Neuroimmunol. Neuroinflamm. 3, e192 (2016).
Rojas, O.-L. et al. HLA class II polymorphism in Latin American patients with multiple sclerosis. Autoimmun. Rev. 9, 407–413 (2010).
Montenegro, R. A. & Stephens, C. Indigenous health in Latin America and the Caribbean. Lancet 367, 1859–1869 (2006).
Wallin, M. T. et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology 92, e1029–e1040 (2019).
Correale, J., Farez, M. F. & Gaitán, M. I. Environmental factors influencing multiple sclerosis in Latin America. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317715049 (2017).
Becker, J. et al. Hypovitaminosis D association with disease activity in relapsing remitting multiple sclerosis in Brazil. J. Neurol. Sci. 363, 236–239 (2016).
Correale, J., Ysrraelit, M. C. & Gaitan, M. I. Immunomodulatory effects of vitamin D in multiple sclerosis. Brain 132, 1146–1160 (2009).
Espinosa-Ramírez, G., Ordoñez, G., Flores-Rivera, J. & Sotelo, J. Sunlight exposure and multiple sclerosis in a tropical country. Neurol. Res. 36, 647–650 (2014).
Bach, J.-F. The effect of infections on susceptibility to autoimmune and allergic diseases. N. Engl. J. Med. 347, 911–920 (2002).
Wasko, N. J., Nichols, F. & Clark, R. B. Multiple sclerosis, the microbiome, TLR2, and the hygiene hypothesis. Autoimmun. Rev. 19, 102430 (2020).
Correale, J. & Farez, M. F. The impact of environmental infections (parasites) on MS activity. Mult. Scler. J. 17, 1162–1169 (2011).
Rodríguez-Violante, M., Ordoñez, G., Bermudez, J. R., Sotelo, J. & Corona, T. Association of a history of varicella virus infection with multiple sclerosis. Clin. Neurol. Neurosurg. 111, 54–56 (2009).
Sotelo, J., Ordoñez, G., Pineda, B. & Flores, J. The participation of varicella zoster virus in relapses of multiple sclerosis. Clin. Neurol. Neurosurg. 119, 44–48 (2014).
Correale, J. & Farez, M. Association between parasite infection and immune responses in multiple sclerosis. Ann. Neurol. 61, 97–108 (2007).
Carnero Contentti, E., Giachello, S. & Correale, J. Barriers to access and utilization of multiple sclerosis care services in a large cohort of Latin American patients. Mult. Scler. J. 27, 117–129 (2021).
Carnero Contentti, E. et al. Access and unmet needs to multiple sclerosis care in a cohort of Argentinean patients. Mult. Scler. Relat. Disord. 33, 88–93 (2019).
Rojas, J. I. et al. Multiple sclerosis and neuromyelitis optica spectrum disorder testing and treatment availability in Latin America. Neurol. Res. 43, 1081–1086 (2021).
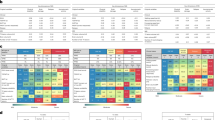
Patrucco, L., Rojas, J., Miguez, J. & Cristiano, E. Application of the McDonald 2010 criteria for the diagnosis of multiple sclerosis in an Argentinean cohort of patients with clinically isolated syndromes. Mult. Scler. J. 19, 1297–1301 (2013).
Pagani Cassará, F. et al. Application of the 2017 McDonald criteria for the diagnosis of multiple sclerosis after a first demyelinating event in patients from Argentina. Mult. Scler. Relat. Disord. 41, 102043 (2020).
Ferreira Vasconcelos, C. C., Miranda Santos, C. M., Papais Alvarenga, M., Camargo, S. M. G. & Papais Alvarenga, R. M. The reliability of specific primary progressive MS criteria in an ethnically diverse population. J. Neurol. Sci. 270, 159–164 (2008).
Filippi, M. et al. Performance of the 2017 and 2010 revised McDonald criteria in predicting MS diagnosis after a clinically isolated syndrome: a MAGNIMS study. Neurology 98, e1–e14 (2022).
Hyun, J.-W. et al. Application of the 2017 McDonald diagnostic criteria for multiple sclerosis in Korean patients with clinically isolated syndrome. Mult. Scler. J. 25, 1488–1495 (2019).
Souissi, A. et al. Multiple sclerosis 2017 McDonald criteria are also relevant for Tunisians. Mult. Scler. Relat. Disord. 43, 102161 (2020).
Zheng, Y. et al. Application of the 2017 McDonald criteria in a Chinese population with clinically isolated syndrome. Ther. Adv. Neurol. Disord. 13, 1756286419898083 (2020).
Lee, D.-H., Peschke, M., Utz, K. S. & Linker, R. A. Diagnostic value of the 2017 McDonald criteria in patients with a first demyelinating event suggestive of relapsing–remitting multiple sclerosis. Eur. J. Neurol. 26, 540–545 (2019).
Habek, M. et al. Establishing the diagnosis of multiple sclerosis in Croatian patients with clinically isolated syndrome: 2010 versus 2017 McDonald criteria. Mult. Scler. Relat. Disord. 25, 99–103 (2018).
Marrodan, M. et al. Performance of McDonald 2017 multiple sclerosis diagnostic criteria and evaluation of genetic ancestry in patients with a first demyelinating event in Argentina. Mult. Scler. J. 29, 559–567 (2023).
Wong, Y. Y. M. et al. Real-world validation of the 2017 McDonald criteria for pediatric MS. Neurol. Neuroimmunol. Neuroinflamm. 6, e528 (2019).
Van Der Vuurst, et al. Application of the 2017 revised McDonald criteria for multiple sclerosis to patients with a typical clinically isolated syndrome. JAMA Neurol. 75, 1392–1398 (2018).
Montalban, X. et al. Diagnosis of multiple sclerosis: 2024 revisions of the McDonald criteria. Lancet Neurol. 24, 850–865 (2025).
Correale, J. et al. Differential diagnosis of suspected multiple sclerosis: global health considerations. Lancet Neurol. 23, 1035–1049 (2024).
Solomon, A. J., Naismith, R. T. & Cross, A. H. Misdiagnosis of multiple sclerosis: Impact of the 2017 McDonald criteria on clinical practice. Neurology 92, 26–33 (2019).
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17, 162–173 (2018).
Lennon, V. A., Kryzer, T. J., Pittock, S. J., Verkman, A. S. & Hinson, S. R. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J. Exp. Med. 202, 473–477 (2005).
Rivera, V. M. et al. Status of the neuromyelitis optica spectrum disorder in Latin America. Mult. Scler. Relat. Disord. 53, 103083 (2021).
Carnero Contentti, E. et al. The real-world applicability of the 2023 international myelin oligodendrocyte glycoprotein antibody-associated disease criteria in a Latin American cohort. Eur. J. Neurol. 31, e16445 (2024).
Fragoso, Y., Elso, F. & Carrá, A. Differential diagnosis of multiple sclerosis in Latin America. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317714279 (2017).
Artal, F. J. C. & Araujo, A. Q.-C. Neurological complications in adults with Zika and chikungunya virus infection. Lancet Neurol. 19, 799–801 (2020).
Brito Ferreira, M. L. et al. Neurological disease in adults with Zika and chikungunya virus infection in Northeast Brazil: a prospective observational study. Lancet Neurol. 19, 826–839 (2020).
Da Costa, V. G., Saivish, M. V., Sinhorini, P. F., Nogueira, M. L. & Rahal, P. A meta-analysis of Chikungunya virus in neurological disorders. Infect. Dis. Now. 54, 104938 (2024).
De Armas Fernández, J. R. et al. Report of an unusual association of Oropouche fever with Guillain–Barré syndrome in Cuba, 2024. Eur. J. Clin. Microbiol. Infect. Dis. 43, 2233–2237 (2024).
França, L. C. et al. Molecular mimicry between Zika virus and central nervous system inflammatory demyelinating disorders: the role of NS5 Zika virus epitope and PLP autoantigens. Arq. Neuropsiquiatr. 81, 357–368 (2023).
López De Romaña, D., Olivares, M. & Brito, A. Introduction: prevalence of micronutrient deficiencies in Latin America and the Caribbean. Food Nutr. Bull. 36, S95–S97 (2015).
Barnabé, A. et al. Folate, vitamin B12 and homocysteine status in the post-folic acid fortification era in different subgroups of the Brazilian population attended to at a public health care center. Nutr. J. 14, 19 (2015).
Kumar, N., Gross, J. B. & Ahlskog, J. E. Copper deficiency myelopathy produces a clinical picture like subacute combined degeneration. Neurology 63, 33–39 (2004).
Román, G. C. An epidemic in Cuba of optic neuropathy, sensorineural deafness, peripheral sensory neuropathy and dorsolateral myeloneuropathy. J. Neurol. Sci. 127, 11–28 (1994).
Hedges, T. R., Hirano, M., Tucker, K. & Caballero, B. Epidemic optic and peripheral neuropathy in Cuba: a unique geopolitical public health problem. Surv. Ophthalmol. 41, 341–353 (1997).
Galicia, L., Grajeda, R. & de Romaña, D. L. Nutrition situation in Latin America and the Caribbean: current scenario, past trends, and data gaps. Rev. Panam. Salud Publica 40, 104–113 (2016).
Patrucco, L. Application of the McDonald criteria in Latin America. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317721943 (2017).
Dujmović, I., Mesaroš, Š, Pekmezović, T., Lević, Z. & Drulović, J. Primary progressive multiple sclerosis: clinical and paraclinical characteristics with application of the new diagnostic criteria. Eur. J. Neurol. 11, 439–444 (2004).
da Gama, P. D. et al. Oligoclonal bands in cerebrospinal fluid of black patients with multiple sclerosis. Biomed. Res. Int. 2015, 217961 (2015).
da Gama, P. D. et al. Study of oligoclonal bands restricted to the cerebrospinal fluid in multiple sclerosis patients in the city of São Paulo. Arq. Neuropsiquiatr. 67, 1017–1022 (2009).
Filippi, M. et al. Present and future of the diagnostic work-up of multiple sclerosis: the imaging perspective. J. Neurol. 270, 1286–1299 (2023).
Gaitán, M. I. et al. The frequency and characteristics of multiple sclerosis misdiagnosis in Latin America: a referral center study in Buenos Aires, Argentina. Mult. Scler. J. 28, 1373–1381 (2022).
Matthews, L. et al. Distinction of seropositive NMO spectrum disorder and MS brain lesion distribution. Neurology 80, 1330–1337 (2013).
Bensi, C. et al. Brain and spinal cord lesion criteria distinguishes AQP4-positive neuromyelitis optica and MOG-positive disease from multiple sclerosis. Mult. Scler. Relat. Disord. 25, 246–250 (2018).
Tseriotis, V.-S. et al. MRI lesion distribution criteria for MS, NMOSD and MOGAD differentiation: a systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry https://doi.org/10.1136/jnnp-2025-336694 (2025).
Carnero Contentti, E. et al. Brain and spinal MRI features distinguishing MS from different AQP4 antibody serostatus NMOSD at disease onset in a cohort of Latin American patients. Mult. Scler. J. 26, 945–954 (2020).
Gaitán, M. I. et al. SWAN-venule: an optimized MRI technique to detect the central vein sign in MS plaques. AJNR Am. J. Neuroradiol. 41, 456–460 (2020).
Gaitán, M. I. et al. The central vein sign is present in most infratentorial multiple sclerosis plaques. Mult. Scler. Relat. Disord. 58, 103484 (2022).
Micheletti, L. et al. Utility of paramagnetic rim lesions on 1.5-T susceptibility phase imaging for the diagnosis of pediatric multiple sclerosis. Pediatr. Radiol. 52, 97–103 (2022).
Vieira, G. D. D., Antônio, F. F. & Damasceno, A. Association between paramagnetic rim lesions with cognitive impairment in pediatric multiple sclerosis. Mult. Scler. Relat. Disord. 91, 105867 (2024).
Pitombeira, M. S. et al. Innate immune cells and myelin profile in multiple sclerosis: a multi-tracer PET/MR study. Eur. J. Nucl. Med. Mol. Imaging 49, 4551–4566 (2022).
Rojas, J. I., Carnero Contentti, E., Henestroza, P., Giachello, S. & Correale, J. Time interval between disease onset and MS diagnosis during the last decades in Latin America. Mult. Scler. Relat. Disord. 48, 102672 (2021).
De Melo, J. R. V., Marzano, L. A. S., Kleinpaul, R. & Santiago-Amaral, J. Time between the first symptom, diagnosis and treatment of multiple sclerosis in a Brazilian cohort. The impact of early diagnosis. Mult. Scler. Relat. Disord. 93, 106178 (2025).
Rojas, J. I., Patrucco, L., Pappolla, A. & Cristiano, E. Improvement over previous decades in time of diagnosis but not in time of initiating DMD in MS patients in Argentina. Mult. Scler. Relat. Disord. 52, 103007 (2021).
Correale, J. et al. Management of relapsing–remitting multiple sclerosis in Latin America: practical recommendations for treatment optimization. J. Neurol. Sci. 339, 196–206 (2014).
Cristiano, E. et al. Argentinean recommendations on the identification of treatment failure in relapsing remitting multiple sclerosis patients. J. Neurol. Sci. 385, 217–224 (2018).
Marques, V. D. et al. Brazilian consensus for the treatment of multiple sclerosis: Brazilian Academy of Neurology and Brazilian Committee on Treatment and Research in Multiple Sclerosis. Arq. Neuropsiquiatr. 76, 539–554 (2018).
Cristiano, E. et al. Consensus recommendations for the diagnosis and treatment of primary progressive multiple sclerosis in Latin America. J. Neurol. Sci. 393, 4–13 (2018).
Skromne-Eisenberg, E. et al. Clinical practice patterns in multiple sclerosis management: Mexican consensus recommendations. Mult. Scler. Relat. Disord. 53, 103053 (2021).
Caparó-Zamalloa, C. et al. Clinical pathway for the diagnosis and management of patients with relapsing–remitting multiple sclerosis: a first proposal for the Peruvian population. Front. Neurol. 12, 667398 (2021).
Silva, B. A. et al. Latin American consensus recommendations on the risk of infections in people with multiple sclerosis treated with disease modifying drugs. Mult. Scler. Relat. Disord. 77, 104840 (2023).
Becker, J. et al. Recommendations by the Scientific Department of Neuroimmunology of the Brazilian Academy of Neurology (DCNI/ABN) and the Brazilian Committee for Treatment and Research in Multiple Sclerosis and Neuroimmunological Diseases (BCTRIMS) on vaccination in general and specifically against SARS-CoV-2 for patients with demyelinating diseases of the central nervous system. Arq. Neuropsiquiatr. 79, 1049–1061 (2021).
Navas, C. et al. Diagnosis and treatment of latent tuberculosis in patients with multiple sclerosis, expert consensus. On behalf of the Colombian Association of Neurology, committee of multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 4, 2055217317752202 (2018).
Cristiano, E. et al. Multiple sclerosis care units in Latin America: consensus recommendations about its objectives and functioning implementation. J. Neurol. Sci. 429, 118072 (2021).
Cristiano, E. et al. Consenso sobre la identificación y seguimiento de la esclerosis múltiple secundaria progresiva en Argentina [Spanish]. Rev. Neurol. 72, 23–32 (2021).
Atun, R. et al. Health-system reform and universal health coverage in Latin America. Lancet 385, 1230–1247 (2015).
Dahham, J., Rizk, R., Kremer, I., Evers, S. M. A. A. & Hiligsmann, M. Economic burden of multiple sclerosis in low- and middle-income countries: a systematic review. Pharmacoeconomics 39, 789–807 (2021).
Frenk, J. & Gómez-Dantés, O. Health systems in Latin America: the search for universal health coverage. Arch. Med. Res. 49, 79–83 (2018).
Organisation for Economic Co-operation and Development & World Bank. Health at a Glance: Latin America and the Caribbean 2023 (OECD, 2023).
Organisation for Economic Co-operation and Development. Health at a Glance 2021: OECD Indicators (OECD, 2021).
Gilardino, R. E., Valanzasca, P. & Rifkin, S. B. Has Latin America achieved universal health coverage yet? Lessons from four countries. Arch. Public. Health 80, 38 (2022).
De Andrade, L. O. M. et al. Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries. Lancet 385, 1343–1351 (2015).
Gracia, F. et al. Costs of multiple sclerosis in Panama from societal, patient perspectives and health-related quality of life. PLoS ONE 13, e0204681 (2018).
Villar Uribe, M., Escobar, M.-L., Ruano, A. L. & Iunes, R. F. Realizing the right to health in Latin America, equitably. Int. J. Equity Health 20, 34 (2021).
Rivera, V. M., Medina, M. T., Duron, R. M. & Macias, M. A. Multiple sclerosis care in Latin America. Neurology 82, 1660–1661 (2014).
MS International Federation. Atlas of MS. MSIF https://atlasofms.org/chart/united-kingdom/disease-modifying-treatments/availability-of-on-label-dmts (2022).
Alonso, R. et al. Barriers against a successful MS treatment: the importance of effectiveness beyond efficacy. Mult. Scler. Relat. Disord. 30, 129–135 (2019).
Almusalam, N. et al. Comparison of physician therapeutic inertia for management of patients with multiple sclerosis in Canada, Argentina, Chile, and Spain. JAMA Netw. Open 2, e197093 (2019).
Skromne-Eisenberg, E., Ordoñez-Boschetti, L. & Treviño-Frenk, I. Disease-modifying therapies in multiple sclerosis in Latin America. Mult. Scler. J. Exp. Transl. Clin. 3, 2055217317723369 (2017).
Rocha, V. & Navas, C. Multiple sclerosis care in Latin America. Int. J. MS Care 27, T7–T12 (2024).
Steinberg, J. et al. Practical issues concerning the approval and use of biosimilar drugs for the treatment of multiple sclerosis in Latin America. Neurol. Ther. 8, 207–214 (2019).
Azevedo, V. F., Sandorff, E., Siemak, B. & Halbert, R. J. Potential regulatory and commercial environment for biosimilars in Latin America. Value Health Reg. Issues 1, 228–234 (2012).
Amato, M. P. et al. Disease-modifying drugs can reduce disability progression in relapsing multiple sclerosis. Brain 143, 3013–3024 (2020).
Lotti, C. B. D. C., Oliveira, A. S. B., Bichuetti, D. B., Castro, I. D. & Oliveira, E. M. L. Late onset multiple sclerosis: concerns in aging patients. Arq. Neuropsiquiatr. 75, 451–456 (2017).
Andersen, M. A., Buron, M. D. & Magyari, M. Late-onset MS is associated with an increased rate of reaching disability milestones. J. Neurol. 268, 3352–3360 (2021).
Zanghì, A. et al. First-line therapies in late-onset multiple sclerosis: an Italian registry study. Eur. J. Neurol. 28, 4117–4123 (2021).
Ziemssen, T., Medin, J., Couto, C. A.-M. & Mitchell, C. R. Multiple sclerosis in the real world: a systematic review of fingolimod as a case study. Autoimmun. Rev. 16, 355–376 (2017).
Mahendraratnam, N., Mercon, K., Gill, M., Benzing, L. & McClellan, M. B. Understanding use of real-world data and real-world evidence to support regulatory decisions on medical product effectiveness. Clin. Pharmacol. Ther. 111, 150–154 (2022).
Gligorijević, V., Malod-Dognin, N. & Pržulj, N. Integrative methods for analyzing big data in precision medicine. Proteomics 16, 741–758 (2016).
Flachenecker, P. et al. Multiple sclerosis registries in Europe — results of a systematic survey. Mult. Scler. J. 20, 1523–1532 (2014).
Rojas, J. I. et al. Real-world experience of ocrelizumab in multiple sclerosis patients in Latin America. Arq. Neuropsiquiatr. 79, 305–309 (2021).
Rojas, J. I. et al. Research priorities in multiple sclerosis in Latin America: a multi-stakeholder call to action to improve patients care. Mult. Scler. Relat. Disord. 53, 103038 (2021).
Ordoñez-Boschetti, L. et al. Safety and tolerability of fingolimod in Latin American patients with relapsing–remitting multiple sclerosis: the open-label FIRST LATAM study. Adv. Ther. 32, 626–635 (2015).
Negrotto, L. et al. High persistence and low adverse events burden in cladribine treated MS patients from Argentina. Mult. Scler. Relat. Disord. 68, 104403 (2022).
Carrá, A. et al. Optimizing outcomes in multiple sclerosis: consensus guidelines for the diagnosis and treatment of multiple sclerosis in Latin America. Ther. Adv. Neurol. Disord. 4, 349–360 (2011).
Soelberg Sorensen, P. et al. The multiple sclerosis care unit. Mult. Scler. J. 25, 627–636 (2019).
Fragoso, Y. D. & Peres, M. Prevalence of multiple sclerosis in the city of Santos. Sp. Rev. Bras. Epidemiol. 10, 479–482 (2007).
Toro, J. et al. Prevalence of multiple sclerosis in Bogotá, Colombia. Neuroepidemiology 28, 33–38 (2007).
Cristiano, E. et al. Prevalence of multiple sclerosis in Buenos Aires, Argentina using the capture-recapture method. Eur. J. Neurol. 16, 183–187 (2009).
Vizcarra Escobar, D. et al. Prevalencia de esclerosis múltiple en Lima – Perú [Spanish]. Rev. Med. Hered. 20, 146–150 (2009).
Abad, P. et al. Prevalence of multiple sclerosis in Ecuador [Spanish]. Neurologia 25, 309–313 (2010).
Ribeiro, S. B. F., Maia, D. F., Ribeiro, J. B., Cardoso, F. A. G. & Silva, C. Clinical and epidemiological profile of patients with multiple sclerosis in Uberaba, Minas Gerais, Brazil. Arq. Neuropsiquiatr. 69, 184–187 (2011).
Lana-Peixoto, M. A., Frota, E. R. C., Campos, G. B. & Monteiro, L. P. The prevalence of multiple sclerosis in Belo Horizonte, Brazil. Arq. Neuropsiquiatr. 70, 102–107 (2012).
Cristiano, E. et al. Increasing prevalence of multiple sclerosis in Buenos Aires, Argentina. Mult. Scler. Relat. Disord. 9, 91–94 (2016).
Mellinger, S. et al. Multiple sclerosis prevalence in Salta City, Argentina. Mult. Scler. Relat. Disord. 25, 212–215 (2018).
Correa-Díaz, E. P. et al. Prevalence of multiple sclerosis in Cuenca, Ecuador. Mult. Scler. J. Exp. Transl. Clin. 5, 2055217319884952 (2019).
Luetic, G. G. & Menichini, M. L. Prevalence of multiple sclerosis in Rosario, Argentina. Mult. Scler. Relat. Disord. 55, 103212 (2021).
Cristiano, E. et al. Incidence of multiple sclerosis in Buenos Aires: a 16-year health maintenance organization-based study. Eur. J. Neurol. 17, 479–482 (2010).
Rocha, V. et al. Incidence of multiple sclerosis in Uruguay: a prospective population-based study. Neuroepidemiology 58, 317–325 (2024).
Organisation for Economic Co-operation and Development (OECD). Health Care Resources: MRI Units (OECD.Stat, accessed 5 November 2025); https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_REAC.
Vargas-Pelaez, C. M. et al. Judicialization of access to medicines in four Latin American countries: a comparative qualitative analysis. Int. J. Equity Health 18, 68 (2019).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks Lilyana Amezcua, who co-reviewed with Christopher Orlando; Teresa Corona; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
BRANDO: www.medbase.com.br/brando
RelevarEM: www.latambase.com.ar
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Becker, J., Pitombeira, M.S. & Rojas, J.I. Epidemiology and characteristics of multiple sclerosis in Latin America. Nat Rev Neurol 22, 22–36 (2026). https://doi.org/10.1038/s41582-025-01160-0
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41582-025-01160-0