Abstract
Hip fractures cause major morbidity, mortality and long-term disability among older persons worldwide. The World Health Organization has defined two key indicators within the framework of the UN Decade of Healthy Ageing to measure health system performance in providing care for older adults with hip fractures: the proportion who receive surgery within 48 h of fracture; and the proportion who receive pharmacological treatment for osteoporosis post-fracture. This Perspective article, which describes the clinical importance of these indicators, their amenability for adoption and implications for health equity, is based on findings from audits, guidelines and key literature. Numerous evidence-based solutions — for example, fracture liaison services, orhtogeriatric care models and digital tools support hip-fracture management, yet major barriers remain, such as data gaps, system preparedness and pathway variability. New or modified policies developed by national governments, ministries of health and other relevant authorities and tailored to specific geopolitical contexts are urgently needed to enable the implementation of timely surgical care and secondary fracture prevention strategies aligned with the WHO indicators. Improved health information systems to measure performance and to ensure translation to real-world changes in the lives of older people worldwide are of paramount importance.
Similar content being viewed by others
Introduction
At the 73rd World Health Assembly in 2020, WHO member states endorsed the Decade of Healthy Ageing (2021–2030), marking an important advance in global efforts to promote longer and healthier lives for people aged 60 years and older, the age group defined by the WHO and United Nations (UN) as ‘older people’. The initiative was subsequently declared the United Nations (UN) Decade of Healthy Ageing (2021–2030) at the 75th session of the UN General Assembly in 2021 (ref. 1). This global initiative reflects an unprecedented political and strategic commitment to reorient health systems to meet the needs of an ageing population. The resolution mandates the WHO to monitor progress across three key milestone years, 2023, 2026 and 2029, by assessing how well countries are advancing across four interconnected action areas: changing how we think, feel, and act towards age and ageing; ensuring that communities foster the abilities of older people; delivering person-centred, integrated care and primary health services that are responsive to older people; and providing access to long-term care for those who need it. To support this mandate, in May 2025 the WHO developed a core set of measurable indicators that enable member states to benchmark their performance, identify equity gaps, and track improvements in the responsiveness of health systems to older people. Progress reporting at each of the three milestone years is intended not only to assess accountability but also to catalyse policy reforms and encourage cross-country learning.
This emphasis on measurable progress is especially critical given the rising burden of age-related conditions, chief among them being osteoporotic fractures, a major threat to the health and independence of older adults worldwide. As the global population of older persons continues to grow, the health economic burden of osteoporotic fractures, particularly hip fractures, is rising exponentially2,3,4,5,6. A hip fracture in an older adult is more than just a broken bone; it is often the tipping point that sets off a cascade of decline, from loss of independence to long stays in care facilities, and even early death7. This vulnerability arises in part from the biological relationship between ageing and skeletal fragility: as people age, bone mass and quality deteriorate owing to cumulative imbalances in bone remodelling and hormonal changes, leading to osteoporosis and an increased risk of fragility fractures8. Unfortunately, less than one in three older persons with a hip fracture return to their premorbid level of function. For many, a hip fracture will be the point of permanent loss of independence9. The mortality rate 1 year after hip fracture remains unacceptably high among older persons, with reported rates varying substantially even across high-income settings, ranging from 10.8% in Singapore to 23.8% in New Zealand10. In settings with fewer resources, the chances of surviving a year after a hip fracture are even lower11. Behind these numbers are real people facing delays in surgery, limited access to rehabilitation and little support to avoid future fractures. Standard management of hip fractures in older adults includes prompt surgical repair, post-operative rehabilitation and pharmacological treatment to prevent future fractures12. Yet in many settings, these essential components of care remain fragmented or inconsistently delivered, resulting in missed opportunities to restore function, extend life and prevent avoidable suffering.
Fragility fractures are an interesting litmus test for how well (or poorly) the care needs of older people are being addressed. These disparities underscore the need to examine not only clinical care pathways but also broader systemic responses to ageing and fracture prevention. It is in this context that the WHO has included two important indicators in its framework for measuring the progress and impact of the UN Decade of Healthy Ageing1 : the proportion of older persons receiving surgical treatment for hip fracture within 48 h, and the proportion of older persons receiving pharmacological treatment for osteoporosis after a hip fracture. These indicators effectively capture two important processes in fracture care, namely the acute management phase and the secondary prevention phase, and they provide implementable and measurable metrics for health systems to use as a benchmark for their own performance. The purpose of this Perspective article is to reflect upon the rationale for the selection of these indicators, summarize the evidence that supports the utilization of these measures, assess the operational feasibility of the indicators in an international context, and briefly discuss how implementation at local, national and global levels can be accelerated through coordinated policy, models of care and data systems.
What gets measured gets done
The adage ‘what gets measured gets done’ underpins the WHO’s emphasis on defining clear, meaningful indicators within the UN Decade of Healthy Ageing framework. Selecting the right metrics is critical, not only to track progress but also to drive policy change and accountability. The indicators were formulated through a rigorous consultative process involving global experts, and are grounded in principles of measurability, relevance and equity1. Although the two indicators discussed here, namely timely hip fracture surgery and post-fracture pharmacological treatment, primarily capture process elements, their real-world utility lies in their ability to reflect outcomes such as survival, recovery and long-term independence. Both are classified as ‘Tier II’ indicators in the WHO framework1, meaning that they are considered high-priority measures for which data may not yet be consistently available across all countries but are crucial for benchmarking and system transformation.
It is important to note that although these indicators focus specifically on hip-fracture management and secondary prevention, they do not address the equally important area of primary prevention that includes population-based screening, assessment, and pre-fracture treatment of osteoporosis. This area lies beyond the scope of the current article; however, it is worth emphasizing that primary prevention remains an essential pillar in reducing the global burden of osteoporotic fractures8.
Indicator 1: timely hip fracture surgery
The WHO Healthy Ageing Framework includes the indicator “Percentage of older people who received surgical treatment for hip fractures within 48 h after admission to the hospital, over the past year”1. This indicator reflects not only timely access to emergency orthopaedic care but also serves as a tracer for health-system responsiveness, coordination and overall quality of acute care for older persons. The WHO does not specify whether “admission” refers to the time of presentation to hospital (including emergency-department arrival) or to formal inpatient admission to an acute-care ward. Internationally, both definitions are in use: for example, the Australian Institute of Health and Welfare13 and the Australian and New Zealand Hip Fracture Registry14 define the 48-h window from presentation to hospital, whereas the Canadian Institute for Health Information15 defines it from inpatient admission. Although the WHO does not specify which definition should be applied, this distinction is noted here to acknowledge differing national conventions in interpreting the indicator.
Rationale for inclusion of this indicator
Large population-based and randomized controlled studies have found no significant difference in outcomes when surgery is performed within 6 h as compared with 24 h after fracture16,17,18, and mortality and complications do not typically emerge until at least 24 h after fracture. However, there is strong and consistent evidence that surgery delayed beyond 48 h is associated with significantly worse outcomes. Surgical fixation of an osteoporotic fracture within 48 h is associated with decreased mortality at 30 days and 1 year, fewer complications and quicker functional recovery19. A 2018 systematic review and meta-analysis found that people who underwent surgery within 48 h of a hip fracture had a 20% lower risk of 12-month mortality (risk ratio (RR) 0.80, 95% CI 0.66–0.97)19. This review incorporated 28 prospective observational studies, encompassing a total of 31,242 people with hip fracture, a robust sample size that enhances confidence in the findings. Although most of the included studies originated from North America and Europe, the review also encompassed data from Asia and Australia, providing broad regional coverage and suggesting that the findings have global relevance across diverse health care systems. A retrospective cohort analysis of data from the American College of Surgery (ACS) National Surgical Quality Improvement Program (NSQIP) database that included 43,071 severely ill people with hip fracture reinforces the evidence that surgery delayed beyond 48 h carries significantly higher complication and mortality rates, particularly among the frailest people20. In this population, hip-fracture surgery performed after 48 h was associated with not only higher complication rates and mortality, but also with higher rates of cerebrovascular accidents (odds ratio (OR) 1.542; CI 1.048–2.269), pneumonia (OR 1.886; CI 1.611–2.209), urinary tract infections (OR 1.546; CI 1.283–1.861), readmission (OR 1.212, CI 1.074–1.366), postoperative length of stay beyond 6 days (OR 1.829, CI 1.670–2.003) and mortality (OR 1.475, CI 1.286–1.693) compared with immediate surgery20. These converging data clearly support the 48-h window as a critical cut-off for timely surgical care, allowing for clinical stabilization while avoiding further avoidable harm.
Delays beyond 48 h have been related to both patient-related characteristics such as the presence of comorbidities as well as to modifiable factors at the health care system level, including limited surgical slots, limited perioperative optimization pathways and inefficient triage to surgery in the emergency department21. It is important to note, however, that in the old-old’ and the ‘oldest-old’, terms often used to describe individuals 85–94 years and ≥95 years old, respectively22, comorbidities might require stabilization before surgery, potentially justifying short, medically warranted delays. It is in this setting that orthogeriatric co-management becomes particularly valuable, offering a coordinated approach to balancing timely surgery with necessary medical stabilization. Orthogeriatric co-management entails the collaborative care of people with hip fracture by orthopaedic surgeons and geriatricians throughout the perioperative and early-recovery phases. This integrated approach facilitates medical optimization, delirium prevention, early mobilization and discharge planning and has been shown to enhance perioperative optimization, shorten time to surgery, and improve both functional recovery and survival23. A 2022 systematic review reported a 28% reduction in-hospital mortality and a 14% reduction in 1-year mortality with early orthogeriatric involvement24. Although several models of orthogeriatric care such as geriatric consultation services, where geriatricians act in an advisory role to the orthopaedic team; geriatric wards, where orthopaedic teams provide input; and integrated care models, where both specialties co-manage patients from admission to discharge exist, and were reviewed in the study, none of them was shown to be superior to the others. However, the consistency of improved outcomes across these models highlights the critical importance of timely, coordinated medical input during the perioperative period24.
Current national standards and benchmarks for time to hip-fracture surgery
Although the importance of timely surgical intervention in hip fracture care is widely acknowledged, the performance indicators used across health systems continue to vary substantially. A 2025 mixed-methods review identified 241 performance indicators for hip-fracture care25. ‘Time to surgery’ was the most frequently reported indicator, appearing in 83% of the studies included in the review. However, definitions of this indicator varied not only with respect to time thresholds, but also in operational parameters, for example, whether time was counted from the moment of injury, hospital presentation or admission, whether medically unfit patients were excluded and whether the clock stopped for delays due to health optimization. This heterogeneity made it impossible to make meaningful comparisons of the quality of care across institutions and countries25. Several countries have made time to surgery an official indicator in their national standards, and existing national indicators align closely with the WHO’s 48-h benchmark. In the UK, the National Institute for Health and Care Excellence guideline26 and National Hip Fracture Database (NHFD; https://www.nhfd.co.uk/) performance indicators define prompt surgery as occurring on the day of or the day after hospital admission (thus prescribing surgery within a time frame of ≤36 h), and Australia’s Hip Fracture Clinical Care Standard27 document states that patients must receive surgery in a timely manner within 36 h. Similar standards exist in Canada15, New Zealand (https://anzhfr.org/registry-reports), Israel28 and Scotland29 and are reported via mandated registries or performance programmes at a national level. These pre-existing benchmarks demonstrate widespread early adoption of timely surgery targets, even before the WHO-endorsed 48-h benchmark was introduced in May 2025. Although these countries are aligned in intent, actual measurement infrastructure and reporting consistency still vary and no country has formally updated its system to explicitly label the indicator as the ‘WHO-endorsed’ measure. Formal integration of the WHO indicator into national monitoring systems across all member states remains a key next step in global harmonization. Alignment efforts are therefore still at a nascent stage, and the WHO Technical Advisory Group encourages member states to consider incorporating these globally standardized indicators to support harmonized tracking, benchmarking, and accountability over the course of the UN Decade of Healthy Ageing1.
Strategies to improve the timeliness of hip-fracture care
Several system-level strategies have been shown to enhance the timeliness and quality of hip-fracture surgery. These strategies include the use of standardized perioperative care pathways, early involvement of orthogeriatric care, the use of clinical checklists and care bundles, and structured documentation and audit systems. Countries such as the UK and Australia have successfully implemented these strategies through national programmes. For instance, the UK NHFD and the Australia and New Zealand Hip Fracture Registry (ANZHFR; https://anzhfr.org/) have supported initiatives such as the Best Practice Tariff30 and the Hip Fracture Clinical Care Standard27, respectively. These efforts have helped to improve time to surgery and reduce variation in care through audit, benchmarking and system-level feedback.
In the USA, although there is no national hip fracture registry equivalent to the NHFD or ANZHFR, individual institutions and health care systems have adopted similar interventions. These interventions include multidisciplinary co-management protocols, enhanced recovery pathways and clinical documentation tools, often tracked through the ACS NSQIP Geriatric Surgery Program31 or institutional quality-improvement dashboards32. However, implementation in the USA remains decentralized and variable, lacking the unified national standards seen in the UK or Australia.
It must be noted that, although the WHO’s recommendation that hip-fracture surgery be performed within 48 h provides a relevant benchmark for the global community, achieving this standard understandably remains a challenge in many low- and middle-income countries (LMICs). In these settings, delays are quite often compounded by systemic issues: direct out-of-pocket costs for implants, limited availability of surgical theatres, delayed admissions and poor perioperative capacity. A 2025 systematic review of evidence from LMICs reflects this reality, with some studies reporting delays of over 2 weeks between injury and surgery33.
Transitioning from such 2-week delays to a 2-day window requires a multipronged strategy. Key enablers of this strategy include the development of fracture-care pathways, the formation of multidisciplinary teams that include trauma surgeons, anaesthesiologists, geriatricians, physiotherapists and other relevant professionals to oversee the pathways, implementing protocols that facilitate immediate admission of all older hip-fracture patients at the time of diagnosis, fast-tracking of patients from the emergency department to orthopaedic wards, dedicated orthopaedic trauma lists, perioperative protocols to expedite medical clearance and securing supply chains for timely implant availability. Certain interventions, such as education of care providers, prioritization of people with hip fractures in triage and standardized preoperative assessment forms and so on can be implemented at a relatively low cost and might yield early gains. Education of patients and caregivers on the need for early surgery and system-level audits to identify avoidable delays also contribute to addressing institutional bottlenecks that contribute to treatment delays, such as delayed surgical clearance, limited access to operating theatres, or a lack of clarity about clinical responsibility. Importantly, such efforts will signal a shift in institutional culture — one that recognizes hip-fracture surgery in older adults as a true time-sensitive emergency rather than an elective orthopaedic event.
Thus, although the 48-h threshold might not yet be feasible in all LMIC settings, it remains a critical aspirational benchmark, and one that is achievable with targeted reforms. Efforts should focus on context-specific strategies that will incrementally reduce surgical delays while maintaining safety and equity in care delivery. For instance, at a tertiary teaching hospital in Punjab, India, the implementation of geriatric hip-fracture care protocols led to positive outcomes: 60.5% of older people with femoral-neck fractures had surgery within 24 h of admission, and 99% underwent surgery within 1 week34.
Indicator 2: pharmacological treatment post-fracture
The WHO Healthy Ageing Framework includes the indicator: “Percentage of older people who have experienced a fragility fracture of the hip or the spine, or more than one fracture, treated with anti-osteoporosis medication over the past year”1. This indicator captures the effectiveness of secondary fracture prevention efforts and reflects the capacity of health systems to deliver continuity of care, evidence-based chronic-disease management, and long-term risk reduction for older adults following a major sentinel event. Although the WHO document does not clarify whether this term encompasses calcium and vitamin D supplementation, it is generally interpreted in the context of currently available pharmacological treatments for osteoporosis.
Rationale for including this indicator
A prior hip fracture is a powerful predictor of subsequent fragility fractures, with patients at an extremely high and imminent risk of a second fracture if pharmacological treatment for osteoporosis is not initiated to address the underlying skeletal fragility35. Conversely, approximately 50% of individuals presenting with a hip fracture have already had a prior fracture, underscoring missed opportunities for earlier intervention36,37. In the USA, health care costs associated with a second fracture have been shown to be up to three times higher than those incurred for the initial fracture38. Therefore, the first fragility fracture is the prototypical ‘low-hanging fruit’ that represents both a clear, early warning sign and an important opportunity for intervention that can prevent both clinical decline and escalating costs39.
Randomized controlled trials and meta-analyses have shown that anti-osteoporosis therapies significantly reduce the risk of subsequent fractures in individuals with a prior fragility fracture40,41. The results of the HORIZON Recurrent Fracture Trial demonstrated that annual infusion of zoledronic acid, initiated within 90 days of a hip fracture, reduced the risk of new clinical fractures by 35% and lowered all-cause mortality by 28% over a median follow-up of 1.9 years42. These results were subsequently supported by a 2017 meta-analysis, which confirmed a 26% reduction in non-vertebral fractures (RR 0.74; 95% CI 0.56–0.98) with zoledronic-acid administration in people with a recent low-trauma fracture41. Oral bisphosphonates, denosumab and anabolic agents such as teriparatide have all demonstrated efficacy in secondary fracture prevention, with RR reductions ranging from 20% to 50% depending on the agent, fracture site and compliance with therapy40,41.
Current standards and benchmarks for post-fracture pharmacological treatment
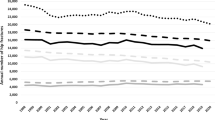
Treatment rates after hip fracture vary widely across countries. A 2023 international study that included health care data at the patient level from 19 countries and regions, and that included people aged 50 years and older hospitalized with a hip fracture from 2005 to 2018, revealed that the proportion who received post-fracture pharmacological treatment ranged from as low as 11.5% (95% CI 11.1–11.9%) in Germany to 50.3% (95% CI 50.0–50.7%) in the UK43. These figures highlight the substantial gap between evidence and real-world practice, even in high-income health systems. Currently, very few countries have formally adopted this WHO indicator into national quality frameworks. Nonetheless, uptake of pharmacological treatment is now tracked in several national registries and audits. In England and Wales, the NHFD reported that 50.8% of people presenting with a hip fracture were discharged on anti-osteoporosis medication between 2016 and 2020 (ref. 44). In Canada, publicly accessible data from the Ontario Osteoporosis Strategy indicate that fewer than 20% of patients with a fracture undergo diagnosis or adequate treatment for osteoporosis45. Similarly, in Japan, 80% of people with a hip fracture initially go untreated, and medication continuation rates after 1 year are just 20%46. These national-level measures underscore both progress and persistent gaps and provide a foundation to benchmark and improve care via secondary-fracture prevention initiatives.
Barriers to post-fracture pharmacological treatment
Despite the strong evidence supporting secondary fracture prevention, multiple barriers continue to impede the initiation of treatment for osteoporosis after hip fracture. Several authoritative international guidelines, including those from the International Osteoporosis Foundation (IOF) and European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis12, the American Association of Clinical Endocrinologists and American College of Endocrinology47, the Endocrine Society48 and national guidance documents such as those from the UK National Osteoporosis Guidance Group49 recommend prompt initiation of pharmacological therapy in people with fragility fractures, particularly hip fractures. These guidelines consistently emphasize the need to treat underlying osteoporosis to reduce the risk of future fractures. However, patients and physicians alike often lack awareness of existing guidelines, and they often underestimate the proven benefits of pharmacological therapy. There may be apprehension regarding adverse effects associated with long-term use of some osteoporosis medicines (such as atypical femur fractures and osteonecrosis of the jaw), cost of medications and confusion about who should initiate treatment, whether it be orthopaedics, rheumatology, endocrinology, geriatrics or primary care50. Poor communication between health care providers, limited patient education and fragmented systems of care only add to the inertia51. Although focused primarily on primary and not secondary prevention of fractures, a systematic review of qualitative studies examining health care providers’ views on osteoporosis, falls and fracture risk revealed deeper issues beneath the surface52. In addition to the barriers mentioned above, clinicians, particularly general practitioners, expressed frustration with the ambiguity and impracticality of current guidelines. Many found the recommendations ill-suited to the complex reality of managing older people with multiple co-morbidities and long lists of medications. In addition, scepticism existed amongst the providers about whether guidelines reflect real-world practice. The health care providers also expressed that there was a growing disconnect between research findings and the realities of everyday patient care52. In LMICs, these issues are compounded by structural limitations to health systems. Barriers such as poor access to specialized care, lack of surgical and rehabilitation services, high out-of-pocket medication costs, and irregular availability of drugs make it even more difficult to deliver consistent, guideline-based osteoporosis management after a fragility fracture.53. These multi-level barriers highlight the urgent need for system-wide reforms, improved education for providers, and structured care coordination to close the evidence–practice gap in post-fracture treatment of osteoporosis.
Strategies to improve rates of post-fracture pharmacological treatment
Transitioning from delayed to timely post-fracture treatment is feasible when health systems prioritize strengthening perioperative and rehabilitation infrastructure, public-insurance coverage for essential medications, training of non-specialist providers in osteoporosis care, institutional dashboard tracking and audit feedback as well as patient and caregiver education initiatives.
One evidence-based solution to overcoming the barriers to medical therapy and follow-up post-fracture is through the implementation of fracture liaison services (FLS), that ensure that all eligible patients are identified, assessed and started on appropriate osteoporosis therapy. FLS reduce ambiguity, improve interdisciplinary communication (for example, between emergency, orthopaedic and endocrinology departments), help to tailor decisions to individual patient contexts, and to embed pharmacological treatment into routine post-fracture workflows, thus reducing the risk that treatment becomes an afterthought (or is simply forgotten). FLS are designed to address specifically the types of organizational and behavioural barriers that have historically impeded the implementation of secondary-fracture prevention. They have repeatedly been shown to improve rates of treatment initiation54,55,56, to reduce rates of refracture57 and refracture costs58,59,60,61. FLS assign responsibility for initiating osteoporosis care to a dedicated coordinator or team; in doing so, the ambiguity about who initiates treatment is removed. Concerns about adverse effects and medication costs can be addressed early through structured counselling and coordinated follow-up. Notably, by automating the identification, assessment and initiation of therapy, FLS can help alleviate the burden on individual clinicians and potentially reduce the risk of patients falling through the cracks. In addition, FLS enable treatment decisions to be made through patient-specific assessments, often with input from multiple disciplines, and to apply guidelines in an individualized manner that considers comorbidities, life expectancy and patient preferences62,63. In doing so, they help to close the evidence-to-practice gap and facilitate the feasibility and scalability of secondary-fracture prevention.
FLS can offer a pragmatic approach to strengthening secondary-fracture prevention in LMICs, too. By streamlining care pathways, identifying cost-effective treatment strategies and prioritizing limited resources (such as surgical access and medications) for people at highest risk, FLS can facilitate more sustainable and targeted service delivery. A qualitative study from Malaysia that examined the perspectives of health care professionals on FLS implementation reported widespread support for the model, while also highlighting critical challenges such as limited staff awareness about FLS and their importance, inconsistent coordination and the absence of dedicated coordinator roles and multidisciplinary training64. Similarly, a commentary from India described a structured, low-cost, multidisciplinary FLS model, but underscored systemic barriers including fragmented follow-up mechanisms and low adherence to medications65. A prospective study in rural Taiwan that evaluated the clinical impact of FLS implementation observed meaningful improvements in length of stay in hospital and in the proportion of people with hip fracture who underwent surgery within 48 h of admission66. Subgroup analysis of the FLS cohort in this study further revealed that those who received anti-osteoporotic treatment had significantly decreased mortality and 30-day readmission rates compared with those who did not66, reinforcing the feasibility and value of FLS implementation even in resource-constrained environments.
Global initiatives to reduce secondary fracture
Capture the Fracture (CtF; https://www.capturethefracture.org/), a global initiative developed by the IOF, the world’s largest non-governmental organization dedicated to musculoskeletal health, seeks to prevent secondary fractures through the integration of FLS into health care systems. As of June 2025, >1,180 FLS from 62 countries have been registered with CtF and evaluated against its internationally endorsed Best Practice Framework for quality of care. The CtF programme is supported by a global network of clinical experts and national societies and thus is uniquely positioned to standardize the identification, investigation and initiation of pharmacological treatment for people with fragility fractures. With its globally endorsed benchmarking framework, practical implementation tools and widespread adoption, the CtF programme is expected to help transform often fragmented responses to osteoporotic fractures into a coordinated, preventive care pathway.
The CtF programme supports providers seeking to establish and scale up the implementation of FLS by offering a suite of practical tools, including the Best Practice Framework for benchmarking, structured implementation toolkits and clinical pathways that are adaptable to local contexts. It facilitates mentorship through a global network of experienced FLS practitioners, enables service improvement via self-assessment audits and feedback mechanisms, and amplifies advocacy efforts by recognizing high-performing sites and promoting national and regional policy engagement. Its benchmarking and quality indicators align closely with the WHO indicator for the percentage of people receiving pharmacological treatment after a hip fracture1. By translating this global target into clear, auditable actions, such as ensuring timely osteoporosis assessment, initiation of therapy and structured follow-up, the CtF framework functions not only as an implementation guide but also as a practical enforcement mechanism. It helps health systems to move from aspirational commitments to concrete, trackable performance, thereby accelerating real-world adoption of the WHO indicator within national and local service-delivery models.
Regional efforts have further supported the scale-up of secondary fracture prevention, particularly in the Asia–Pacific region. The Asia Pacific Consortium on Osteoporosis67 has actively leveraged the CtF framework to harmonize clinical standards and promote the broader uptake of FLS across the region. Although this consortium does not directly implement services, its regional efforts have included the development of tailored educational materials, cross-disciplinary training and an ongoing collaboration with the South Asian Federation of Endocrine Societies to evaluate the cost-effectiveness of FLS models in LMICs in the Asia–Pacific region. In parallel, several providers across the region have adapted the FLS model to local realities, for instance, by embedding FLS coordination into orthopaedic wards, using telehealth to support follow-up and engaging non-physician staff to deliver osteoporosis education and adherence counselling. These adaptations reflect the importance of flexibility in applying the CtF Best Practice Framework within diverse health-system contexts. Complementing these regional efforts, the Fragility Fracture Network, in collaboration with other global and regional organizations such as the IOF, International Geriatric Fracture Society, European Federation of National Associations of Orthopaedics and Traumatology, and European Geriatric Medicine Society, launched a global call in 2018 to action outlining multidisciplinary strategies to improve acute care, rehabilitation and secondary prevention for people presenting with fragility fractures68. Collectively, these initiatives reflect a growing international consensus namely that coordinated, system-wide responses are essential to closing the care gap and reducing the incidence of secondary fractures, even in resource-constrained settings.
Moving towards equitable, integrated care for older persons
Tracking the progress of 194 WHO member countries through clear indicators such as timely hip-fracture surgery and post-fracture treatment of osteoporosis, turns aspiration into accountability, showing where health systems are succeeding, where they are stalling and what must change so that every older person can benefit from the promise of the UN Decade of Healthy Ageing.
Although these indicators were only formally endorsed by WHO in May 2025, as previously mentioned, analogous measures have already been in use across several countries, particularly those with national fracture registries or post-fracture care programmes. This suggests that the infrastructure for implementation exists in many contexts, even if not yet uniformly aligned with the definitions used in the WHO indicators. Beyond their immediate public-health relevance, the two WHO-recommended indicators, namely timely surgery following a hip fracture and initiation of post-fracture pharmacological treatment, offer valuable insights into how health systems are performing in the delivery of equitable, integrated care to older persons. For instance, these indicators can function as proxies for structural equity: evidence from national hip-fracture registries shows that men, individuals living with dementia and those from rural or socio-economically disadvantaged backgrounds are consistently less likely to receive timely surgical intervention or appropriate secondary-fracture prevention therapy69. In this sense, tracking such indicators not only supports clinical benchmarking but also helps to expose the inequalities embedded in many care systems. Moreover, these measures reflect the degree of system integration, that is, the link between emergency triage and surgical scheduling, how effectively multidisciplinary teams coordinate perioperative care and whether discharge planning transitions smoothly into long-term follow-up. They serve as signals of whether a health system is evolving beyond episodic, disease-based responses towards more person-centred, functional, continuous care models. Both indicators provide countries with a way of monitoring how their health systems are adapting to the challenges of population ageing, specifically whether innovations in service delivery promote greater system integration, continuity of care, and person-centred approaches aligned with the ‘healthy ageing’ agenda. Over time, these measures enable jurisdictions to benchmark progress, compare performance across regions and identify outliers or best-practice examples. This capability is especially relevant as many health systems still operate using a disease- or episode-based care model as opposed to a continuity-care- or function-based approach.
Looking ahead, countries can leverage the WHO indicators to transition from aspirational targets to measurable improvements by embedding them into national monitoring systems, aligning care models accordingly and ensuring routine data collection and feedback. Support from global and regional stakeholders including technical assistance, harmonized reporting tools and shared learning platforms will be essential to accelerate progress and close persistent care gaps throughout the UN Decade of Healthy Ageing.
Operationalizing these indicators at scale will probably require national policies that are informed by, and aligned where appropriate, with the WHO-recommended definitions of timely hip-fracture surgery and post-fracture treatment of osteoporosis, alongside coordinated investment in data systems, workforce capacity and service delivery infrastructure. Essential targeted system-level investments include linking hospital performance metrics to national surgical standards, allocating dedicated theatre slots for emergency orthopaedic procedures, strengthening perioperative capacity (for example, anaesthesiology and diagnostics) and improving triage and transfer systems, particularly in facilities where delays are driven by resource constraints and expanding orthogeriatric models of care.
Likewise, national funding is needed to scale up FLS across both tertiary and secondary hospitals. Community-based providers, general practitioners and trained health workers must also be empowered to ensure continuity of treatment after discharge. Addressing affordability through the inclusion of osteoporosis medications that are included on national essential medicines lists would help to ensure equitable access. Robust health information and data systems are essential for turning measurement into meaningful action. Linking inpatient and outpatient records enables tracking of treatment initiation after fractures, whereas tools such as digital FLS dashboards, automated alerts and integrated risk assessments can support timely bone mineral density testing and therapy uptake. Strengthening these systems to support real-time tracking of timing of surgery, treatment initiation and follow-up across care settings is critical to transforming indicators from mere reports into drivers of tangible improvements. National registries such as the ANZHFR in Australia and New Zealand6 and the NHFD in the UK70 provide scalable models for integrating such data streams and enabling continuous quality improvement. Ultimately, however, the value of measurement lies not in the data themselves but in their ability to inform action and improve care delivery. Well-designed systems help clinicians to identify care gaps, support hospitals in refining care pathways, and give policymakers an insight into directing resources where they are most needed. In this way, indicators become not just tools for accountability but catalysts for real and lasting change.
A consolidated overview of key system-level barriers and the corresponding strategies across the hip-fracture care continuum is presented in Table 1.
Conclusions
The world is now halfway through the UN Decade of Healthy Ageing (2021–2030). The WHO indicators for hip-fracture surgery within 48 h and initiation of pharmacological treatment of osteoporosis after fracture are more than clinical metrics; they are sentinel measures of a health system’s readiness for rapidly ageing populations. Systematic tracking of these indicators allows countries to gauge their transition from reactive, fragmented services to proactive, integrated care models. But measurement alone is insufficient. Achieving meaningful change will require sustained political commitment, investment in workforce and digital infrastructure, and a shift in mindset that treats a fracture not as the end of care but as the starting point for lifelong bone-health management.
References
World Health Organization. Measuring the Progress and Impact of the UN Decade of Healthy Ageing (2021–2030): Framework and Indicators Recommended by WHO Technical Advisory Group (2024).
Chandran, M. et al. The health and economic burden of osteoporotic fractures in Singapore and the potential impact of increasing treatment rates through more pharmacological options. Arch. Osteoporos. 14, 114 (2019).
Muschitz, C. et al. Epidemiology and economic burden of fragility fractures in Austria. Osteoporos. Int. 33, 637–647 (2022).
Borgström, F. et al. Fragility fractures in Europe: burden, management and opportunities. Arch. Osteoporos. 15, 59 (2020).
Mohd-Tahir, N.-A. & Li, S.-C. Economic burden of osteoporosis-related hip fracture in Asia: a systematic review. Osteoporos. Int. 28, 2035–2044 (2017).
Australia and New Zealand Hip Fracture Registry. ANZHFR 2022 Annual Report Full e-Report https://anzhfr.org/registry-reports/# (2022).
Dyer, S. M. et al. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 16, 158 (2016).
Compston, J. E., McClung, M. R. & Leslie, W. D. Osteoporosis. Lancet 393, 364–376 (2019).
Moerman, S., Mathijssen, N. M., Tuinebreijer, W. E., Nelissen, R. G. & Vochteloo, A. J. Less than one-third of hip fracture patients return to their prefracture level of instrumental activities of daily living in a prospective cohort study of 480 patients. Geriatr. Gerontol. Int. 18, 1244–1248 (2018).
Harvey, L. A. et al. Variation in mortality following hip fracture across the Asia Pacific region: systematic review and proportional meta-analysis. Arch. Gerontol. Geriatr. 126, 105519 (2024).
Jayasekera, P. T. et al. Hip fractures and outcome in elderly patients in a tertiary care hospital of Sri Lanka. Arch. Osteoporos. 18, 113 (2023).
Kanis, J. A., Cooper, C., Rizzoli, R., Reginster, J.-Y. & Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 30, 3–44 (2019).
Australian Institute of Health and Welfare. Hip fracture care clinical care standard indicators: 4a-Proportion of patients with a hip fracture receiving surgery within 48 hours of presentation with the hip fracture. METEOR identifier 628088 https://meteor.aihw.gov.au/content/628088 (2016).
Australian and New Zealand Hip Fracture Registry. ANZHFR User Guide Data Dictionary v17, January 2025 https://go.nature.com/3X9ynYa (2025).
Canadian Institute for Health Information. Hip Fracture Surgery within 48 Hours; https://go.nature.com/3LsaxnY (2025).
Pincus, D. et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA 318, 1994–2003 (2017).
Sobolev, B. et al. Mortality effects of timing alternatives for hip fracture surgery. CMAJ 190, E923–E932 (2018).
HIP ATTACK Investigators Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet 395, 698–708 (2020).
Klestil, T. et al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci. Rep. 8, 13933 (2018).
Darbandi, A. D. et al. Effects of delayed hip fracture surgery on severely ill patients: defining the time to medical optimization. Am. Surg. 89, 1864–1871 (2023).
Ricci, W. M., Brandt, A., McAndrew, C. & Gardner, M. J. Factors affecting delay to surgery and length of stay for patients with hip fracture. J. Orthop. Trauma. 29, e109–e114 (2015).
Cohen-Mansfield, J. et al. The old, old-old, and the oldest old: continuation or distinct categories? An examination of the relationship between age and changes in health, function, and wellbeing. Int. J. Aging Hum. Dev. 77, 37–57 (2013).
Prestmo, A. et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet 385, 1623–1633 (2015).
Van Heghe, A. et al. Effects of orthogeriatric care models on outcomes of hip fracture patients: a systematic review and meta-analysis. Calcif. Tissue Int. 110, 162–184 (2022).
Mazarello Paes, V. et al. Which performance indicators are used globally for evaluating healthcare in patients with a hip fracture? Bone Jt Open. 6, 275–290 (2025).
National Institute for Health and Care Excellence. Hip Fracture: Management https://www.nice.org.uk/guidance/cg124 (22 June 2011).
Australian Commission on Safety and Quality in Health Care. Hip Fracture Clinical Care Standard https://go.nature.com/3JfAuXq (2023).
Weil, Y. A. et al. Hip fracture care and national systems in Israel and South Africa. OTA Int. 3, e065 (2020).
Public Health Scotland. Scottish Hip Fracture Audit: Reporting on 2023; https://go.nature.com/4hJ6eRs (2024).
Eardley, W. & Johansen, A. The national hip fracture database: lessons learned and future horizons. Orthop. Trauma. 38, 108–113 (2024).
Arshi, A., Rezzadeh, K., Stavrakis, A. I., Bukata, S. V. & Zeegen, E. N. Standardized hospital-based care programs improve geriatric hip fracture outcomes: an analysis of the ACS NSQIP Targeted Hip Fracture Series. J. Orthop. Trauma. 33, e223–e228 (2019).
American College of Surgeons. Performance Improvement in a Hip Fracture ERAS Program. https://www.facs.org/quality-programs/qi-resources/case-studies/performance-improvement-in-a-hip-fracture-eras-program/.
Kiani, S. N. et al. Hip fracture surgery in resource-limited environments: a systematic literature review. OTA Int. 8, e373 (2025).
Jain, D. et al. Early results of a geriatric hip fracture program in India for femoral neck fracture. Geriatr. Orthop. Surg. Rehabil. 6, 42–46 (2015).
Kanis, J. A. et al. A systematic review of the worldwide incidence and mortality of hip fracture. Osteoporos. Int. 23, 2239–2256 (2012).
Edwards, B. J., Bunta, A. D., Simonelli, C., Bolander, M. & Fitzpatrick, L. A. Prior fractures are common in patients with subsequent hip fractures. Clin. Orthop. Relat. Res. 461, 226–230 (2007).
Port, L. et al. Osteoporotic fracture: missed opportunity for intervention. Osteoporos. Int. 14, 780–784 (2003).
Song, X. et al. Cost burden of second fracture in the US health system. Bone 48, 828–836 (2011).
Chandran, M. & Akesson, K. Secondary fracture prevention: plucking the low hanging fruit. Ann. Acad. Med. Singap. 42, 541–544 (2013).
Palacios, S. et al. Treatment with denosumab reduces secondary fracture risk in women with postmenopausal osteoporosis. Climacteric 18, 805–812 (2015).
Saito, T. et al. Effectiveness of anti-osteoporotic drugs to prevent secondary fragility fractures: systematic review and meta-analysis. Osteoporos. Int. 28, 3289–3300 (2017).
Lyles, K. W. et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N. Engl. J. Med. 357, 1799–1809 (2007).
Sing, C.-W. et al. Global epidemiology of hip fractures: secular trends in incidence rate, post-fracture treatment, and all-cause mortality. J. Bone Miner. Res. 38, 1064–1075 (2023).
Mohsin, Z., Javaid, M. K. & Johansen, A. Current approaches to secondary prevention after hip fracture in England and Wales — an analysis of trends between 2016 and 2020 using the national hip fracture database (NHFD). Arch. Osteoporos. 18, 93 (2023).
Osteoporosis Canada. Facts and Stats; https://osteoporosis.ca/facts-and-stats/ (2019).
International Osteoporosis Foundation. Major Milestone for Secondary Fracture Prevention Announced in Japan; https://go.nature.com/4hLhZ9Z (2022).
Camacho, P. M. et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis — 2020 update. Endocr. Pract. 26, 1–46 (2020).
Eastell, R. et al. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 104, 1595–1622 (2019).
Gregson, C. L. et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch. Osteoporos. 17, 58 (2022).
Chandran, M., Cheen, M., Ying, H., Lau, T. C. & Tan, M. Dropping the ball and falling off the care wagon. Factors correlating with nonadherence to secondary fracture prevention programs. J. Clin. Densitom. 19, 117–124 (2016).
Bennett, M. J., Center, J. R. & Perry, L. Exploring barriers and opportunities to improve osteoporosis care across the acute-to-primary care interface: a qualitative study. Osteoporos. Int. 34, 1249–1262 (2023).
Cho, C., Bak, G., Sumpton, D., Richards, B. & Sherrington, C. Perspectives of healthcare providers on osteoporosis, falls and fracture risk: a systematic review and thematic synthesis of qualitative studies. Arch. Osteoporos. 19, 90 (2024).
Muzzammil, M., Owais Minhas, M. & Jamil, A. Closing the gap: addressing health disparities in the management of fragility fractures in low and middle-income countries’ geriatric population. J. Orthop. Rep. 4, 100468 (2025).
Ruggiero, C. et al. The interdisciplinary fracture liaison service improves health-related outcomes and survival of older adults after hip fracture surgical repair. Arch. Osteoporos. 17, 135 (2022).
Chandran, M. et al. Secondary prevention of osteoporotic fractures — an “OPTIMAL” model of care from Singapore. Osteoporos. Int. 24, 2809–2817 (2013).
Kim, M. S. et al. The impact of a fracture liaison service for patients with femoral fractures on subsequent fractures and mortality: focusing on systematic literature review and metaanalysis. Arch. Osteoporos. 20, 24 (2025).
Javaid, M. K. Efficacy and efficiency of fracture liaison services to reduce the risk of recurrent osteoporotic fractures. Aging Clin. Exp. Res. 33, 2061–2067 (2021).
Xu, L. et al. Return on investment of fracture liaison services: a systematic review and analysis. Osteoporos. Int. 35, 951–969 (2024).
Pinedo-Villanueva, R., Burn, E., Maronga, C., Cooper, C. & Javaid, M. K. Expected benefits and budget impact from a microsimulation model support the prioritization and implementation of fracture liaison services. J. Bone Miner. Res. 38, 499–511 (2023).
Cooper, M. S., Palmer, A. J. & Seibel, M. J. Cost-effectiveness of the concord minimal trauma fracture liaison service, a prospective, controlled fracture prevention study. Osteoporos. Int. 23, 97–107 (2012).
Moriwaki, K. & Noto, S. Economic evaluation of osteoporosis liaison service for secondary fracture prevention in postmenopausal osteoporosis patients with previous hip fracture in Japan. Osteoporos. Int. 28, 621–632 (2017).
Mitchell, P. et al. Implementation of Models of Care for secondary osteoporotic fracture prevention and orthogeriatric models of care for osteoporotic hip fracture. Best. Pract. Res. Clin. Rheumatol. 30, 536–558 (2016).
Curtis, J. & Silverman, S. L. Commentary: the five Ws of a Fracture Liaison Service: Why, Who, What, Where and How? In osteoporosis, we reap what we sow. Curr. Osteoporos. Rep. 11, 365–368 (2013).
Cheah, M. H., Lai, P. S. M. & Ong, T. Views of healthcare professionals regarding barriers and facilitators for a Fracture Liaison Service in Malaysia. PLoS ONE 19, e0307919 (2024).
Maldar, A. & Chadha, M. Fracture liaison services in India: challenges and opportunities. J. Assoc. Physicians India 71, 11–13 (2023).
Wang, C.-C., Liu, H.-C., Lee, M.-T. & Huang, W.-T. Effects of fracture liaison service on outcomes of patients with hip fracture in rural area of an Asian country. Geriatr. Orthop. Surg. Rehabil. 14, 21514593231204783 (2023).
Chandran, M. et al. Development of the Asia Pacific Consortium on Osteoporosis (APCO) framework: clinical standards of care for the screening, diagnosis, and management of osteoporosis in the Asia-Pacific region. Osteoporos. Int. 32, 1249–1275 (2021).
Dreinhöfer, K. E. et al. A global call to action to improve the care of people with fragility fractures. Injury 49, 1393–1397 (2018).
Fujii, T., Mori, T., Komiyama, J., Kuroda, N. & Tamiya, N. Factors associated with non-initiation of osteoporosis pharmacotherapy after hip fracture: analysis of claims data in Japan. Arch. Osteoporos. 18, 103 (2023).
Royal College of Physicians. 15 Years of Quality Improvement: the 2023 National Hip Fracture Database Annual Report on 2022; https://www.nhfd.co.uk/2023report (2023).
Author information
Authors and Affiliations
Contributions
M.C. researched data for the article. M.C., J.A.T., O.B., N.H., R.R. and J.-Y.R. substantially contributed to discussion of the content. M.C. wrote the article. All authors edited/reviewed the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Rheumatology thanks Cristina Ojeda-Thies and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chandran, M., Thiyagarajan, J.A., Alokail, M. et al. WHO benchmarks for equitable hip-fracture care and osteoporosis treatment in older people. Nat Rev Rheumatol 22, 62–70 (2026). https://doi.org/10.1038/s41584-025-01319-5
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41584-025-01319-5