Abstract
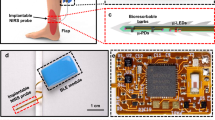
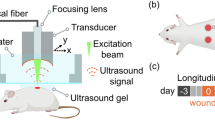
Vascular complications following solid organ transplantation may lead to graft ischemia, dysfunction or loss. Imaging approaches can provide intermittent assessments of graft perfusion, but require highly skilled practitioners and do not directly assess graft oxygenation. Existing systems for monitoring tissue oxygenation are limited by the need for wired connections, the inability to provide real-time data or operation restricted to surface tissues. Here, we present a minimally invasive system to monitor deep-tissue O2 that reports continuous real-time data from centimeter-scale depths in sheep and up to a 10-cm depth in ex vivo porcine tissue. The system is composed of a millimeter-sized, wireless, ultrasound-powered implantable luminescence O2 sensor and an external transceiver for bidirectional data transfer, enabling deep-tissue oxygenation monitoring for surgical or critical care indications.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data supporting the results in this study are available within the article or its Supplementary Information.
Code availability
The custom Labview program and Matlab code used in this study are available on Github at https://github.com/ssonmezoglu/NBT-21.
References
Gibbons, R. D., Meltzer, D. & Duan, N. Waiting for organ transplantation. Science 287, 237–238 (2000).
Piardi, T. Vascular complications following liver transplantation: a literature review of advances in 2015. World J. Hepatol. 8, 36–57 (2016).
Marland, J. R. K. et al. Real-time measurement of tumour hypoxia using an implantable microfabricated oxygen sensor. Sensing and Bio-Sensing Research 30, 100375 (2020).
Peterson, J. I., Fitzgerald, R. V. & Buckhold, D. K. Fiber-optic probe for in vivo measurement of oxygen partial pressure. Anal. Chem. 56, 62–67 (1984).
Liu, S. et al. Quantitative tissue oxygen measurement in multiple organs using 19F MRI in a rat model. Magn. Reson. Med. 66, 1722–1730 (2011).
Elas, M. et al. Electron paramagnetic resonance oxygen images correlate spatially and quantitatively with oxylite oxygen measurements. Clin. Cancer Res. 12, 4209–4217 (2006).
Gómez, H. et al. Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O2 saturation response. Intensive Care Med. 34, 1600–1607 (2008).
Lynch, J. M. et al. Noninvasive optical quantification of cerebral venous oxygen saturation in humans. Acad. Radiol. 21, 162–167 (2014).
Zhang, H. et al. Wireless, battery-free optoelectronic systems as subdermal implants for local tissue oximetry. Sci. Adv. 5, eaaw0873 (2019).
Seo, D. et al. Wireless recording in the peripheral nervous system with ultrasonic neural dust. Neuron 91, 529–539 (2016).
Piech, D. K. et al. A wireless millimetre-scale implantable neural stimulator with ultrasonically powered bidirectional communication. Nat. Biomed. Eng. 4, 207–222 (2020).
Thimot, J. & Shepard, K. L. Bioelectronic devices: wirelessly powered implants. Nat. Biomed. Eng. 1, 0051 (2017).
O’Leary, B. & Vaezy, S. Marketing clearance of diagnostic ultrasound systems and transducers. https://www.fda.gov/media/71100/download (US Food and Drug Administration, 2019).
IEEE standard for safety levels with respect to human exposure to radio frequency electromagnetic fields, 3 kHz to 300 GHz. IEEE Std C95.1-2005 (Revision of IEEE Std C95.1-1991) 1–238 (2006).
Ammi, A. Y. et al. Characterization of ultrasound propagation through ex-vivo human temporal bone. Ultrasound Med. Biol. 34, 1578–1589 (2008).
Maleki, T. et al. An ultrasonically powered implantable micro-oxygen generator (IMOG). IEEE Trans. Biomed. Eng. 58, 3104–3111 (2011).
Kim, A. et al. An implantable ultrasonically-powered micro-light-source (µLight) for photodynamic therapy. Sci. Rep. 9, 1395 (2019).
Sonmezoglu, S. & Maharbiz, M. M. A 4.5mm3 deep-tissue ultrasonic implantable luminescence oxygen sensor. In 2020 IEEE International Solid- State Circuits Conference (ISSCC) 454–456 (2020).
Yao, L., Khan, R., Chodavarapu, V. P., Tripathi, V. S. & Bright, F. V. Sensitivity-enhanced CMOS phase luminometry system using xerogel-based sensors. IEEE Trans. Biomed. Circuits Syst. 3, 304–311 (2009).
McDonagh, C. et al. Phase fluorometric dissolved oxygen sensor. Sens. Actuators B Chem. 74, 124–130 (2001).
Wang, X. & Wolfbeis, O. S. Optical methods for sensing and imaging oxygen: materials, spectroscopies and applications. Chem. Soc. Rev. 43, 3666–3761 (2014).
Holland, R. Resonant properties of piezoelectric ceramic rectangular parallelepipeds. J. Acoust. Soc. Am. 43, 988–997 (1968).
Chan, C.-M., Chan, M.-Y., Zhang, M., Lo, W. & Wong, K.-Y. The performance of oxygen sensing films with ruthenium-adsorbed fumed silica dispersed in silicone rubber. Analyst 124, 691–694 (1999).
Jorge, P. A. S., Caldas, P., Rosa, C. C., Oliva, A. G. & Santos, J. L. Optical fiber probes for fluorescence based oxygen sensing. Sens. Actuators B Chem. 103, 290–299 (2004).
Hartmann, P., Leiner, M. J. P. & Kohlbacher, P. Photobleaching of a ruthenium complex in polymers used for oxygen optodes and its inhibition by singlet oxygen quenchers. Sens. Actuators B Chem. 51, 196–202 (1998).
Guo, J. & Sonkusale, S. A 65 nm CMOS digital phase imager for time-resolved fluorescence imaging. IEEE J. Solid-State Circuits 47, 1731–1742 (2012).
Ghanbari, M. M. et al. A sub-mm3 ultrasonic free-floating implant for multi-mote neural recording. IEEE J. Solid-State Circuits 54, 3017–3030 (2019).
Kino, G. S. Acoustic Waves: Devices, Imaging, and Analog Signal Processing. (Prentice Hall, 1987).
Adkins, J. N. et al. Toward a human blood serum proteome: analysis by multidimensional separation coupled with mass spectrometry. Mol. Cell. Proteomics 1, 947–955 (2002).
Ratner, B. D. Replacing and renewing: synthetic materials, biomimetics, and tissue engineering in implant dentistry. J. Dent. Educ. 65, 1340–1347 (2001).
Blaszykowski, C., Sheikh, S. & Thompson, M. Surface chemistry to minimize fouling from blood-based fluids. Chem. Soc. Rev. 41, 5599–5612 (2012).
Norton, P. T., DeAngelis, G. A., Ogur, T., Saad, W. E. & Hagspiel, K. D. Noninvasive vascular imaging in abdominal solid organ transplantation. Am. J. Roentgenol. 201, W544–W553 (2013).
Boraschi, P., Pina, M. C. D. & Donati, F. Graft complications following orthotopic liver transplantation: role of non-invasive cross-sectional imaging techniques. Eur. J. Radiol. 85, 1271–1283 (2016).
Hickman, P. E., Potter, J. M. & Pesce, A. J. Clinical chemistry and post-liver-transplant monitoring. Clin. Chem. 43, 1546–1554 (1997).
Mitchell, R. N. Graft vascular disease: immune response meets the vessel wall. Annu. Rev. Pathol. 4, 19–47 (2009).
Khaja, M. S., Matsumoto, A. H. & Saad, W. E. Complications of transplantation. Part 1: renal transplants. Cardiovasc. Intervent. Radiol. 37, 1137–1148 (2014).
Wunsch, H., Angus, D. C., Harrison, D. A., Linde-Zwirble, W. T. & Rowan, K. M. Comparison of medical admissions to intensive care units in the United States and United Kingdom. Am. J. Respir. Crit. Care Med. 183, 1666–1673 (2011).
Barrett, M. L., Smith, M. W., Elixhauser, A., Honigman, L. S. & Pines, J. M. Utilization of intensive care services, 2011: statistical brief #185. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs (Agency for Healthcare Research and Quality (US), 2006).
Dyson, A. & Singer, M. Tissue oxygen tension monitoring: will it fill the void? Curr. Opin. Crit. Care 17, 281–289 (2011).
Brandstrup, B. et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: A randomized assessor-blinded multicenter trial. Ann. Surg. 238, 641–648 (2003).
Dünser, M. W. et al. Association of arterial blood pressure and vasopressor load with septic shock mortality: a post hoc analysis of a multicenter trial. Crit. Care 13, R181 (2009).
Ince, C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit. Care 19, S8 (2015).
Kara, A., Akin, S. & Ince, C. Monitoring microcirculation in critical illness. Curr. Opin. Crit. Care 22, 444–452 (2016).
Wang, M. L., Chang, T. C. & Arbabian, A. Ultrasonic implant localization for wireless power transfer: active uplink and harmonic backscatter. In 2019 IEEE International Ultrasonics Symposium (IUS) 818–821 (2019).
Koch, T. et al. Ultrasound velocity and attenuation of porcine soft tissues with respect to structure and composition: I. Muscle. Meat Sci. 88, 51–58 (2011).
Wang, M. L. et al. Closed-loop ultrasonic power and communication with multiple miniaturized active implantable medical devices. In 2017 IEEE International Ultrasonics Symposium (IUS) 1–4 (2017).
Shen, K. & Maharbiz, M. M. Ceramic packaging for neural implants. J. Neural Eng. 18, 025002 (2021)
Shen, K. & Maharbiz, M. M. Design of ceramic packages for ultrasonically coupled implantable medical devices. IEEE Trans. Biomed. Eng. 67, 2230–2240 (2020).
Song, E., Li, J., Won, S. M., Bai, W. & Rogers, J. A. Materials for flexible bioelectronic systems as chronic neural interfaces. Nat. Mater. 19, 590–603 (2020).
Pfeiffer, S. A. & Nagl, S. Microfluidic platforms employing integrated fluorescent or luminescent chemical sensors: a review of methods, scope and applications. Methods. Appl. Fluoresc. 3, 034003 (2015).
Lu, X., Manners, I. & Winnik, M. A. Polymer/silica composite films as luminescent oxygen sensors. Macromolecules 34, 1917–1927 (2001).
Hassler, C., Boretius, T. & Stieglitz, T. Polymers for neural implants. J. Polym. Sci. B Polym. Phys. 49, 18–33 (2011).
Chang, T. C. et al. Design of tunable ultrasonic receivers for efficient powering of implantable medical devices with reconfigurable power loads. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 63, 1554–1562 (2016).
El-Sheimy, N., Hou, H. & Niu, X. Analysis and modeling of inertial sensors using allan variance. IEEE Trans. Instrum. Meas. 57, 140–149 (2008).
Acknowledgements
This work was supported by the Chan Zuckerberg Biohub (CZB) (to M.M.M.) and by NIH/NICHD R44HD094414 and R01HD072455 (to J.R.F. and E.M.). We thank C. Losser, R. Hutchings and C. Vento for expert assistance with animal handling and surgery as well as members of the Laboratory Animal Resource Center (LARC) at the University of California, San Francisco. We also thank the Berkeley Wireless Research Center and R. Muller (University of California, Berkeley) for access to IC design software.
Author information
Authors and Affiliations
Contributions
S.S. supervised the project, designed and built the wireless system, designed and performed the in vitro and ex vivo experiments and analyzed and interpreted the associated data. S.S., J.R.F. and E.M. designed and performed the in vivo experiments and interpreted biological data. M.M.M. contributed to the design of the experiments. S.S., E.M. and M.M.M. participated in writing the paper. All authors contributed to the discussion of the paper.
Corresponding authors
Ethics declarations
Competing interests
M.M.M. is an employee of iota Biosciences, Inc., a fully owned subsidiary of Astellas Pharma. All of the other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Notes and Figs. 1–14.
Rights and permissions
About this article
Cite this article
Sonmezoglu, S., Fineman, J.R., Maltepe, E. et al. Monitoring deep-tissue oxygenation with a millimeter-scale ultrasonic implant. Nat Biotechnol 39, 855–864 (2021). https://doi.org/10.1038/s41587-021-00866-y
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41587-021-00866-y
This article is cited by
-
Barriers to translating continuous monitoring technologies for preventative medicine
Nature Biomedical Engineering (2025)
-
Wirelessly controlled drug delivery systems for translational medicine
Nature Reviews Electrical Engineering (2025)
-
Improving the Cardiovascular Outcomes of Obstructive Sleep Apnea: Towards More Precise Hypoxia-Based Models of Disease Severity
Current Sleep Medicine Reports (2025)
-
A subnanolitre tetherless optoelectronic microsystem for chronic neural recording in awake mice
Nature Electronics (2025)
-
Standardized Pre-clinical Surgical Animal Model Protocol to Investigate the Cellular and Molecular Mechanisms of Ischemic Flap Healing
Biological Procedures Online (2024)