Abstract
Arterial stiffness is an important risk factor for cardiovascular events. Radial augmentation index (AI r ) can be more conveniently measured compared with carotid-femoral pulse wave velocity (cfPWV). However, the performance of AI r in assessing arterial stiffness is limited. This study proposes a novel index AI rd , a combination of AI r and diastolic augmentation index (AI d ) with a weight α, to achieve better performance over AI r in assessing arterial stiffness. 120 subjects (43 ± 21 years old) were enrolled. The best-fit α is determined by the best correlation coefficient between AI rd and cfPWV. The performance of the method was tested using the 12-fold cross validation method. AI rd (r = 0.68, P < 0.001) shows a stronger correlation with cfPWV and a narrower prediction interval than AI r (r = 0.61, P < 0.001), AI d (r = −0.17, P = 0.06), the central augmentation index (AI c ) (r = 0.61, P < 0.001) or AI c normalized for heart rate of 75 bpm (r = 0.65, P < 0.001). Compared with AI r (age, P < 0.001; gender, P < 0.001; heart rate, P < 0.001; diastolic blood pressure, P < 0.001; weight, P = 0.001), AI rd has fewer confounding factors (age, P < 0.001; gender, P < 0.001). In conclusion, AI rd derives performance improvement in assessing arterial stiffness, with a stronger correlation with cfPWV and fewer confounding factors.
Similar content being viewed by others
Introduction
Arterial stiffness is an important risk factor for cardiovascular events1,2,3,4 and other complications5,6,7. Many indicators have been proposed to assess arterial stiffness. Carotid-femoral pulse wave velocity (cfPWV) is considered the ‘gold standard’ in determining arterial stiffness1, 8. However, several limitations still exist. First, it is not convenient to record the carotid and femoral pulse waves simultaneously. Patients should keep in supine position. Second, the distance from the carotid to the femoral artery is difficult to measure accurately especially in patients with abdominal obesity9. Moreover, femoral pulse wave can not be readily and accurately measured in patients with obesity, diabetes, metabolic syndrome, or peripheral artery disease8.
Wave reflection, which is convenient to measure, is of great interest in the estimation of arterial stiffness, and is generally quantified by augmentation index, which is calculated from the pulse wave at a specific artery site10,11,12,13. Central aortic augmentation index (AI c ) has been shown to be an independent predictor of all-cause and cardiovascular mortality in end-stage renal failure patients10. AI c normalized for heart rate of 75 bpm (AI@75) has been proven to be independently associated with severe short- and long-term cardiovascular events in patients undergoing percutaneous coronary interventions11. However, AI c can not be readily obtained non-invasively. Recent studies12,13,14,15,16,17,18 on the estimation of aortic pulse wave using transfer functions provide an alternative method to predict AI c based on peripheral pulse waves. Yet, Millasseau19 concluded that radial augmentation index (AI r ) provides similar information on central arterial stiffness as AI c obtained by a transfer function method. AI r can be directly calculated from a radial pulse wave. It is used to assess arterial stiffness in a widely used device, HEM9000AI (Omron Healthcare, Japan). Kohara20 showed the feasibility of AI r in assessing vascular aging. AI r is also reported to be a predictor of premature coronary artery disease in younger males21. However, the performance of AI r in assessing arterial stiffness is limited, as AI r is influenced by several factors other than cfPWV, like heart rate (HR) and the reflect distance of the pulse wave22. In addition, it has been shown that AI r does not correlate closely with vascular stiffness in those over the age of 5523. Due to the limitations of AI r and the fact that diastolic augmentation index (AI d ) also reflects wave reflection24,25,26, we propose a novel index AI rd in the form of a linear combination of AI r and AI d to derive potentially better performance over AI r in assessing arterial stiffness. Our contribution include the proposed index AI rd and the validation of the linear combination of AI r and AI d , instead of AI r , in assessing arterial stiffness.
The subsequent contents of this paper are organized as follows. The second section describes the methodologies used in this study. The third section presents the results. The discussion and conclusion of our study are presented in the fourth and fifth sections.
Methods
Subjects and study protocol
128 subjects participated in the study. 8 of them were excluded for lack of accuracy in the measurement of cfPWV, resulting in a sample of 120 subjects (54 females, 66 males) aged 18 to 92 years old (mean ± SD, 43 ± 21 years old). 4 subjects had arrhythmias, 2 had premature ventricular contractions, and 5 had hypertension and arrhythmia, hypertension, hypothyroidism, arteriosclerosis, and mitral regurgitation, respectively. Information on the subjects is shown in Table 1 and is also detailed in Supplementary Table S1. All subjects gave informed consents before the study. The datasets generated during the current study are available from the corresponding author on reasonable request. This study was approved by School of Sino-Dutch Biomedical and Information Engineering, Northeastern University, China. The experiment was carried out in accordance with the Interim Measures for Guidelines on Ethical Review of Biomedical Research Involving Human Subjects.
Measurements were performed in a quiet room at a constant temperature of 22 to 23 °C. Subjects stayed in supine position throughout the experiment and were advised to keep still without talking, laughing or sleeping. Subjects had a 15 min rest before the test. Measurements of augmentation indexes and cfPWV were performed sequentially. There was no significant difference (paired t-test: mean ± SD, −0.6 ± 3.6 bpm; P = 0.07) in pulse rate between the two measurements.
Measurement of cfPWV
cfPWV is defined as pulse traveled distance divided by pulse transit time (PTT) from carotid to femoral artery. The pulse travelled distance was calculated as 0.8 times the direct distance from the right common carotid artery to the right common femoral artery22. The distance was measured using a non-elastic tape. PTT was calculated as time difference between the feet of pulse waves at two different artery sites. In each trial, right carotid and right femoral pulse waves were measured using two pressure pulse sensors (MP100, Xinhangxingye Co. Ltd., Beijing, China). The signals were recorded simultaneously for 30 seconds in each trial and were sampled at a rate of 1000 Hz.
The pulse wave signals were then pre-processed to eliminate baseline drift and noise, which influence the accuracy of subsequent calculations. Baseline drift is mainly due to body motion artifact and respiration. The baseline drift was removed by applying ‘sym7’ wavelet decomposition27, 28 at level 10 to the data and eliminating the approximation coefficients in the wavelet decomposition. Similarly, the noise was removed by applying ‘db7’ wavelet decomposition27, 28 at level 4 to the data and eliminating the detail coefficients in the wavelet decomposition.
The foot of a pulse wave was extracted using an intersecting tangents technique29,30,31, which determines the foot by the intersection of the horizontal line through the minimum and the tangent line through the maximum first derivative with respect to time.
PTT was obtained from every cardiac cycle in a series of data, and those exceeding 90% of the SD distribution curve of the PTTs were discarded. The remaining PTTs were averaged. Two measurements of cfPWV were applied in each subject. If the difference between two successive measurements in one subject was less than 0.5 m/s22, the mean of the two measurements was taken. Otherwise, the data of this subject was discarded. According to this criterion, 8 subjects were excluded as mentioned earlier.
Pulse wave analysis
The radial pulse wave was recorded using a SphygmoCor device (AtCor, Australia) with a sampling rate of 128 Hz. The quality of the measurement was controlled by an operator index assessed by the device. A measurement that yields an operator index of lower than 85% was discarded and another measurement was performed. Two trials with an operator index higher than 85% were required on each subject, and two to five measurements were applied to achieve this goal. Augmentation indexes were calculated as the mean of the two measurements. For each measurement, an average radial pulse wave was derived using an ensemble average method. AI r and AI d were both calculated from the average pulse wave.
As shown in Fig. 1, AI r is defined as the amplitude difference (P 2) between the second peak and the foot divided by the amplitude difference (P 1) between the first peak and the foot. AI d is the amplitude difference (P d ) between the diastolic peak and the foot divided by P 1. The locations of the second peak and diastolic peak of all subjects were determined through a second-derivative method.
Features of the radial pulse wave. Amplitude of the peak and foot are the systolic (SBP) and diastolic (DBP) blood pressures, respectively. P 1 indicates the difference between the first peak and the foot in amplitude; P 2 is the amplitude of the second peak minus DBP; P d is the amplitude of the diastolic peak minus DBP.
In this paper, a linear combination of AI r and AI d is defined as:
where α determines the weights of AI r and AI d in the combination. AI rd equals −AI d and AI r when α is 0 and 1, respectively. AI c and AI@75 were also included in the study for comparison with AI rd in assessing arterial stiffness. AI c is defined as the ratio of the late systolic boost in the aortic pressure wave and pulse pressure32. Both AI c and AI@75 were calculated using the SphygmoCor device based on the central aortic pulse wave, which was estimated by applying a transfer function to the radial pulse wave.
Statistical analysis
The reliability of all measurements were evaluated by two-way random average-measure intra-class correlation coefficients (ICC). An ICC higher than 0.9 was deemed appropriate33.
A 12-fold cross validation was used in the determination of α. The raw data was randomly grouped into 12 subsets (with 10 subjects in each). The 12 subsets were divided in all possible ways (12 in total) into a training group with 11 subsets and a test group with 1 subset. In each trial, the best-fit α was calculated based on the training data, and was then used to calculate AI rd of the test group. The best-fit α was determined by finding the strongest correlation between AI rd and cfPWV. The stability of the best-fit α was assessed by analysis of variance in 12 trials.
The correlation of cfPWV with each augmentation index (AI r , AI d , AI rd , AI c or AI@75) was calculated. Prediction interval34, 35 was calculated to evaluate the estimate of cfPWV by each augmentation index. The dependence of AI r and AI rd were studied by performing stepwise multi-regression analysis (enter if P < 0.01, remove if P > 0.01) with the following parameters: gender, age, height, weight, HR, brachial systolic (SBP) and diastolic (DBP) blood pressure. In this study, all statistical significance tests are two-tailed. A probability value of P < 0.01 is considered statistically significant.
Results
Reliability test
The two-way random average-measure ICC of cfPWV (n = 120) is 0.99 (P < 0.001). The ICCs of AI r , AI d , AI c and AI@75 (n = 120) are 0.99 (P < 0.001), 0.95 (P < 0.001), 0.98 (P < 0.001) and 0.98 (P < 0.001), respectively. All the measurements in this study derive an ICC higher than 0.9.
Regression analysis
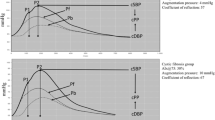
Figure 2 shows the determination and stability analysis of α in 12 trials. The correlation coefficient between AI rd and cfPWV is stable and so is the best-fit α, which is determined with respect to the peak of each correlation coefficient curve. The mean ± SD of all best-fit α in the 12 trials is 0.44 ± 0.02. Thus, α was determined as 0.44. When α equals 0.44, the correlation coefficient of AI rd with cfPWV improves by 0.07 ± 0.01, compared with that of AI r with cfPWV.
Determination of α. The solid line and the dashed area indicate the correlation coefficients between AI rd and cfPWV with the change of α. The solid line is the mean in all 12 trials and the dashed area the confidence band. The best-fit α was determined by the peak of the correlation coefficient curve in each trial. The vertical dash line indicates the mean of the best-fit α in 12 trials, and the bar indicates the standard deviation.
Regression analysis (n = 120) between cfPWV and each augmentation index is shown in Fig. 3. cfPWV shows a stronger correlation with AI rd (r = 0.68; P < 0.001) than with AI r (r = 0.61; P < 0.001), AI c (r = 0.61; P < 0.001), or AI@75 (r = 0.65; P < 0.001). No significant correlation between cfPWV and AI d (r = −0.17; P = 0.06) was found. In addition, compared with other augmentation indexes, AI rd derives a narrower prediction interval in the estimation of cfPWV.
Multi-regression analysis (n = 120) shown in Table 2 reveals that AI r is significantly associated with age (P < 0.001), gender (P < 0.001), HR (P < 0.001), DBP (P < 0.001), and weight (P = 0.001). AI d is significantly dependent on HR (P < 0.001), DBP (P < 0.001), and age (P = 0.001). AI rd is only associated with age (P < 0.001) and gender (P < 0.001).
Discussion
The significance of AI r has been presented in multiple studies20, 21. However, the performance of AI r in assessing arterial stiffness is unsatisfactory22, 23. The present study proposed a novel index, AI rd , by combining AI r and AI d with a weight coefficient α. The weight α is stable in 12 trials. AI rd correlates better with cfPWV compared with AI r , AI d , AI c and AI@75, and is dependent on fewer confounding factors than AI r .
The best-fit α is stable in 12 trials (mean ± SD, 0.44 ± 0.02). The mean best-fit α derives stable improvement of AI rd over AI r in assessing arterial stiffness (with the improvement in correlation coefficient of AI rd over AI r with cfPWV being 0.07 ± 0.01 when α = 0.44 in the training data of 12 trials). In addition, in Fig. 2, a wide range of α (from 0.25 to 1.0) allows AI rd better performance over AI r . The stability and this wide range of α demonstrates the reliability and feasibility of the proposed method.
As central arteries become stiffer, cfPWV increases and the reflected wave from lower body returns to the ascending aorta earlier and also arrives at the radial artery earlier, which causes increases in both AI c and AI r 36, 37. Thus, both AI c and AI r reflect central arterial stiffness, which is demonstrated in the present study (with the correlation coefficient between AI r and cfPWV, r = 0.61; P < 0.001; and the correlation coefficient between predicted AI c and cfPWV, r = 0.61; P < 0.001), and also in multiple previous studies20, 37, 38. Millasseau et al.19 further concluded that AI r provides similar information on central arterial stiffness as AI c obtained by applying a transfer function to the radial pulse wave (AI r versus AI c , r = 0.94, P < 0.001). Similar results were derived in Kohara’s study20, and also in the present study with a significant correlation between AI r and AI c (r = 0.95, P < 0.001). AI c directly measured in the aorta might derive a stronger correlation with cfPWV. However, the aortic pulse wave cannot be readily acquired directly using noninvasive techniques. The most commonly used noninvasive technique is to apply a generalized transfer function12, 13 to the radial pulse wave, which derives satisfactory performance in the estimation of central aortic blood pressures. Specialized transfer function techniques14,15,16,17,18 proposed in recent years further improve the accuracy. However, these techniques are unable to derive satisfactory performance in predicting AI c . The reason is that the accuracy of the inflection point, based on which AI c is calculated, depends on higher frequency components of the aortic pulse wave, which are difficult to obtain accurately from the transfer function, either generalized or specialized. AI c predicted by individualized transfer functions is a promising approach to assess arterial stiffness, however, its accuracy requires further improvements.
AI rd (r = 0.68; P < 0.001) correlates better with cfPWV than AI r (r = 0.61; P < 0.001) does, with a narrower prediction interval. AI r is not only determined by cfPWV, but is also influenced by HR39, 40 (inversely) and the changes in reflection sites at the lower body8. The reflecting site distance from the aorta is related to reflected wave amplitude41, which is equal to or largely contributes to the amplitude of diastolic peak. HR inversely influences DBP42. DBP affects reflecting site distance8 and peripheral resistance41, both of which are determinants of reflected wave amplitude and also the amplitude of diastolic peak. The weighted subtraction of AI d from AI r could reduce the influence of changes in reflection sites on AI r . This can be demonstrated through our result that AI r and AI d both significantly correlate with DBP(P < 0.001 for both) and HR (P < 0.001 for both), while AI rd shows no significant correlation with DBP or HR.
The multi-regression analysis (Table 2) demonstrated that AI r is dependent on factors including age (P < 0.001), gender (P < 0.001), HR (P < 0.001), DBP (P < 0.001), and weight (P = 0.001). This is consistent with previous studies by Sugawara et al.43 and Kohara et al.20. AI d is significantly correlated with HR (P < 0.001), DBP (P < 0.001), and age (P = 0.001). AI rd is only associated with age (P < 0.001) and gender (P < 0.001). This means that by linearly combining AI r with AI d , the influence of DBP and HR is reduced, which allows AI rd a higher reliability and better applicability than AI r in assessing arterial stiffness.
Our study has a few limitations. During the experiment, all subjects were required to be in supine position. The stability of α and the performance of AI rd in assessing arterial stiffness in other postures (for instance, sitting) is not evaluated. Besides, differences in AI r could exist when measuring radial pulse wave using different devices44. The best-fit α might also be different when AI r and AI d were measured using different devices.
Conclusion
In conclusion, AI rd derives performance improvement over AI r in assessing arterial stiffness, with stronger correlation with cfPWV and fewer confounding factors. AI rd is a potential surrogate for both central and radial augmentation indexes in assessing arterial stiffness, with the same measurement procedure but achieving improved performance. Comparing to the ‘gold standard’, cfPWV, methods based on pulse wave analysis (AI r and AI rd ) are much more convenient in the assessment of central arterial stiffness. However, in order to evaluate the physiological and pathological significance of AI rd , longitudinal studies are needed on the relationship between AI rd and cardiovascular events.
References
Mancia, G. et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 22, 193–278 (2013).
Ben-Shlomo, Y. et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J. Am. Coll. Cardiol. 63, 636–646 (2014).
O’Rourke, M. F., O’Brien, C. & Edelman, E. R. Arterial stiffening in perspective: advances in physical and physiological science over centuries. Am. J. Hypertens. hpw019 (2016).
Wakabayashi, I. Homocysteine levels and arterial stiffness in the general population. J. Atheroscler. Thromb. 23, 668–670 (2016).
van Varik, B. J. et al. Arterial stiffness and decline of renal function in a primary care population. Hypertens. Res. 40, 73–78 (2017).
García-Espinosa, V. et al. Children and adolescent obesity associates with pressure-dependent and age-related increase in carotid and femoral arteries’ stiffness and not in brachial artery, indicative of nonintrinsic arterial wall alteration. Int. J. Vasc. Med. 2016 (2016).
Wang, G. et al. Using brachial-ankle pulse wave velocity to screen for metabolic syndrome in community populations. Sci. Rep. 5 (2015).
Laurent, S. et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur. Heart J. 27, 2588–2605 (2006).
Van Bortel, L. M. et al. Clinical applications of arterial stiffness, Task Force III: recommendations for user procedures. Am. J. Hypertens. 15, 445–452 (2002).
London, G. M. et al. Arterial wave reflections and survival in end-stage renal failure. Hypertension 38, 434–438 (2001).
Weber, T. et al. Increased arterial wave reflections predict severe cardiovascular events in patients undergoing percutaneous coronary interventions. Eur. Heart J. 26, 2657–2663 (2005).
Chen, C. H. et al. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure validation of generalized transfer function. Circulation 95, 1827–1836 (1997).
Pauca, A. L., O’Rourke, M. F. & Kon, N. D. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension 38, 932–937 (2001).
Gao, M. et al. A simple adaptive transfer function for deriving the central blood pressure waveform from a radial blood pressure waveform. Sci. Rep. 6 (2016).
Hahn, J. O. Individualized estimation of the central aortic blood pressure waveform: a comparative study. IEEE J. Biomed. Health Inform. 18, 215–221 (2014).
Hahn, J. O., Reisner, A. T., Jaffer, F. A. & Asada, H. H. Subject-specific estimation of central aortic blood pressure using an individualized transfer function: a preliminary feasibility study. IEEE Trans. Inf. Technol. Biomed. 16, 212–220 (2012).
Hahn, J. O., McCombie, D. B., Reisner, A. T., Hojman, H. M. & Asada, H. H. Identification of multichannel cardiovascular dynamics using dual laguerre basis functions for noninvasive cardiovascular monitoring. IEEE Trans. Automatic Control Technology 18, 170–176 (2010).
Swamy, G., Xu, D., Olivier, N. B. & Mukkamala, R. An adaptive transfer function for deriving the aortic pressure waveform from a peripheral artery pressure waveform. Am. J. Physiol. Heart Circ. Physiol. 297, H1956–H1963 (2009).
Millasseau, S. C., Patel, S. J., Redwood, S. R., Ritter, J. M. & Chowienczyk, P. J. Pressure wave reflection assessed from the peripheral pulse is a transfer function necessary? Hypertension 41, 1016–1020 (2003).
Kohara, K. et al. Radial augmentation index: a useful and easily obtainable parameter for vascular aging. Am. J. Hypertens. 18, 11S–14S (2005).
Fischer-Rasokat, U., Brenck, F., Zeiher, A. M. & Spyridopoulos, I. Radial augmentation index unmasks premature coronary artery disease in younger males. Blood Press Monit. 14, 59–67 (2009).
Van Bortel, L. M. et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J. Hypertens. 30, 445–448 (2012).
Fantin, F., Mattocks, A., Bulpitt, C. J., Banya, W. & Rajkumar, C. Is augmentation index a good measure of vascular stiffness in the elderly? Age Ageing 36, 43–48 (2007).
Heffernan, K. S., Kasprowicz, A. G., Tarzia, B. J., Davies, J. E. & Casey, D. P. Sex differences in peripheral augmentation index and arterial reservoir pressure during upper limb postural shifts. Physiology Journal 2014 (2014).
Jaccoud, L. et al. Major impact of body position on arterial stiffness indices derived from radial applanation tonometry in pregnant and nonpregnant women. J. Hypertens. 30, 1161–1168 (2012).
Heim, A., Liaudet, L., Waeber, B. & Feihl, F. Pulse wave analysis of aortic pressure: diastole should also be considered. J. Hypertens. 31, 94–102 (2013).
Mallat, S. G. A theory for multiresolution signal decomposition: the wavelet representation. IEEE Trans. Pattern Anal. Mach. Intell. 11, 674–693 (1989).
Mallat, S. A wavelet tour of signal processing (Academic press, 1999).
Gaddum, N., Alastruey, J., Beerbaum, P., Chowienczyk, P. & Schaeffter, T. A technical assessment of pulse wave velocity algorithms applied to non-invasive arterial waveforms. Ann. Biomed. Eng. 41, 2617–2629 (2013).
Zhang, G., Gao, M., Xu, D., Olivier, N. B. & Mukkamala, R. Pulse arrival time is not an adequate surrogate for pulse transit time as a marker of blood pressure. J. Appl. Physiol. 111, 1681–1686 (2011).
Mukkamala, R. et al. Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans. Biomed. Eng. 62, 1879–1901 (2015).
Nichols, W. W., O’Rourke, M. F. & Vlachopoulos, C. Mcdownald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles, 6th ed., 77–109 (Arnold, 2011).
Portney, L. G. & Watkins, M. P. Foundations of clinical research: applications to practice (FA Davis, 2015).
Nelson, W. B. Two-sample prediction. General Electric Company TIS Report 9 (1968).
Hahn, G. J. & Meeker, W. Q. Statistical intervals: a guide for practitioners, vol. 328 (John Wiley & Sons, 2011).
Gkaliagkousi, E. & Douma, S. The pathogenesis of arterial stiffness and its prognostic value in essential hypertension and cardiovascular diseases. Hippokratia 13, 70–75 (2009).
Nichols, W. W. Clinical measurement of arterial stiffness obtained from noninvasive pressure waveforms. Am. J. Hypertens. 18, 3S–10S (2005).
O’Rourke, M. F., Staessen, J. A., Vlachopoulos, C. & Duprez, D. Clinical applications of arterial stiffness; definitions and reference values. Am. J. Hypertens. 15, 426–444 (2002).
Wilkinson, I. B., Christison, D. J. W. & Cockcroft, J. R. Isolated systolic hypertension: a radical rethink. BMJ. 320, 1685 (2000).
Wilkinson, I. et al. Increased augmentation index and systolic stress in type 1 diabetes mellitus. QJM. 93, 441–448 (2000).
Nichols, W. W. & Edwards, D. G. Arterial elastance and wave reflection augmentation of systolic blood pressure: deleterious effects and implications for therapy. J. Cardiovasc. Pharmacol. Ther. 6, 5–21 (2001).
Wilkinson, I. B. et al. The influence of heart rate on augmentation index and central arterial pressure in humans. J. Physiol. 525, 263–270 (2000).
Sugawara, J., Komine, H., Hayashi, K., Maeda, S. & Matsuda, M. Relationship between augmentation index obtained from carotid and radial artery pressure waveforms. J. Hypertens. 25, 375–381 (2007).
Nürnberger, J. et al. Can arterial stiffness parameters be measured in the sitting position? Hypertens. Res. 34, 202–208 (2011).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Nos 61374015 and 61202258), and the Fundamental Research Funds for the Central Universities (Nos N161904002 and N130404016).
Author information
Authors and Affiliations
Contributions
Y.Y. conceived the experiments, L.H., L.X. and L.Q. fixed the experiment program, Y.S. and B.Y. did efforts in the experiment on clinical issues. Y.Y. and Y.Z. conducted the experiments. Y.Y. wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yao, Y., Hao, L., Xu, L. et al. Diastolic Augmentation Index Improves Radial Augmentation Index in Assessing Arterial Stiffness. Sci Rep 7, 5864 (2017). https://doi.org/10.1038/s41598-017-06094-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-06094-2
This article is cited by
-
Quantitative comparison of the performance of acoustic, optical and pressure sensors for pulse wave analysis
Scientific Reports (2025)
-
A recyclable PANI/PAAMPSA nanocomposite with repeatable, rapid, autonomous self-healing, and unprecedented electro-mechanical properties
Advanced Composites and Hybrid Materials (2025)
-
Changes in plant biodiversity facets of rocky outcrops and their surrounding rangelands across precipitation and soil gradients
Scientific Reports (2022)
-
Plant–plant interactions influence phylogenetic diversity at multiple spatial scales in a semi-arid mountain rangeland
Oecologia (2019)
-
Multiple processes at different spatial scales determine beta diversity patterns in a mountainous semi-arid rangeland of Khorassan-Kopet Dagh floristic province, NE Iran
Plant Ecology (2019)