Abstract
Abnormal autonomic function may cause false-positive non-reassuring foetal status (fpNRFS) and may also cause sleeping problems after birth. However, an association between fpNRFS and sleeping problems in infants has not been reported. We previously showed an association of NRFS with temperament, including bad mood and frequent crying for long durations in 1-month-old infants. In the present study, we aimed to assess this association in 1-year-old infants. A total of 62,612 single pregnant women were included in the analysis. fpNRFS was identified from medical records. Sleep problems, such as short sleep duration or crying at night, were investigated in 1-year-old infants using a questionnaire for mothers. We used a log-binominal regression model to explore the association of fpNRFS with each sleep problem and to estimate risk ratios (RRs). The number of fpNRFS cases was 2,071, with a frequency of 3.3%. We observed an association of fpNRFS with shorter sleep duration of less than 8 h a night (RR 1.30, 95% confidence intervals [CI] 1.10–1.54), crying at night (RR 1.19, 95% CI 1.03–1.39), and bedtime after 22:00 (RR 1.09, 95% CI 1.00–1.18). fpNRFS may be associated with sleep problems in 1-year-old infants.
Similar content being viewed by others
Introduction
Children with developmental disorders tend to have sleep problems and abnormal temperaments1,2,3,4. Foetal distress is one of the prenatal risk factors for developmental disorders, such as autism spectrum disorder (ASD)5.
No non-invasive methods have been developed to determine actual foetal distress with foetal acidosis. Obstetricians clinically use non-reassuring foetal status (NRFS) by monitoring foetal heart rate using cardiotocography (CTG) instead of foetal distress. Unfortunately, the false-positive rate of NRFS assessment by CTG is high6,7,8. Many diagnosed NRFS cases do not show actual foetal distress. They demonstrate normal umbilical cord blood pH and normal Apgar scores.
Babies with normal umbilical cord blood and normal Apgar scores may be categorised into two groups. Some babies show abnormal heart rate patterns and are diagnosed with false-positive NRFS (fpNRFS), whereas others do not. Babies showing fpNRFS may inherently have abnormal regulation of heart rate. Autonomic nerves play an important role in heart rate regulation9 and are also closely related to sleep10. Children with ASD tend to have different heart rate variability from that of normal children11, and they frequently have sleep disorders, such as short sleep during the night and frequent night crying12,13. Therefore, children with fpNRFS may have abnormal autonomic functions and could show abnormal sleep patterns after birth.
We previously showed an association of NRFS with temperaments, including bad mood and frequent crying for a long duration in 1-month infants14. These findings suggest that NRFS may be associated with sleep disorders; nevertheless, an association between the two has not been reported. Therefore, this study aimed to investigate the presence of an association between NRFS, especially fpNRFS, and sleep problems in 1-year-old infants.
Methods
Data used in this study were obtained from the Japan Environment and Children’s Study (JECS), an ongoing large-scale cohort study. The JECS was designed to follow-up children from the prenatal period to the age of 13 years. The baseline profile of participants in the JECS was reported previously15.
Ethics of research
The JECS study protocol was approved by the Ministry of the Environment’s Institutional Review Board on Epidemiological Studies (No. 100406001) and the Ethics Committee of all participating institutions: the National Institute for Environmental Studies that leads the JECS, the National Center for Child Health and Development, Hokkaido University, Sapporo Medical University, Asahikawa Medical College, Japanese Red Cross Hokkaido College of Nursing, Tohoku University, Fukushima Medical University, Chiba University, Yokohama City University, University of Yamanashi, Shinshu University, University of Toyama, Nagoya City University, Kyoto University, Doshisha University, Osaka University, Osaka Medical Center and Research Institute for Maternal and Child Health, Hyogo College of Medicine, Tottori University, Kochi University, University of Occupational and Environmental Health, Kyushu University, Kumamoto University, University of Miyazaki, and University of Ryukyu. Written informed consent was obtained from all participants. All methods were performed in accordance with approved guidelines. The detailed protocol has been reported elsewhere16.
Study participants
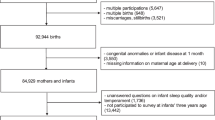
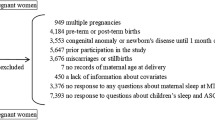
Between 2011 and 2014, 103,062 pregnancies were registered from 15 regions throughout Japan (Fig. 1). Of those, we excluded 40,450 pregnancies due to the following reasons: prior participation in the study (n = 5,647), multiple pregnancies (n = 949), miscarriage or stillbirth (n = 3,676), pre-term or post-term birth (n = 4,586), no records of umbilical cord blood pH or Apgar score at 5 min (n = 16,346), congenital anomaly or newborn disease at 1 month old (n = 2,635), missing information on maternal age at delivery (n = 6), and no response to the questions about infant sleep at the age of 1 year (n = 6,605). Finally, 62,612 single pregnant women were included in our analysis.
Population flow chart. NRFS: non-reassuring foetal status; true-positive NRFS (tpNRFS): cases with umbilical cord pH < 7.2 and Apgar score of < 7 at 5 min after birth of all NRFS cases; false-positive NRFS (fpNRFS): cases with umbilical cord pH ≥ 7.2 and Apgar score of ≥ 7 at 5 min after birth of all NRFS cases.
Exposure (NRFS)
In Japan, abnormal patterns in foetal heart rate are categorised into five levels based on baseline heart rate, variability, kinds, severity of deceleration, and so on17. Level 1 is considered normal, while levels 3 or higher are usually diagnosed as NRFS, and require preparation and execution of forced delivery.
In the present study, the NRFS cases were selected in two ways, based on the medical record transcription at birth. First, we selected cases diagnosed as NRFS by obstetricians. In the cohort data, only information on the presence or absence of NRFS was available. Second, we selected cases that were not diagnosed as NRFS but showed umbilical cord blood pH < 7.2 and Apgar scores < 7 at 5 min after birth.
Of all the NRFS cases, those showing umbilical cord blood pH < 7.2 and Apgar scores of < 7 at 5 min were categorised as true-positive NRFS (tpNRFS) cases, and those showing umbilical cord blood pH ≥ 7.2 and Apgar scores ≥ 7 at 5 min were categorised as false-positive NRFS (fpNRFS) cases. Only cases that met either umbilical cord blood pH or Apgar scores at 5 min were excluded from the stratified analysis with tpNRFS and fpNRFS.
Outcome (infant sleep and crying at night)
At 1 year after delivery, information on infant sleep and crying at night was collected via a parent-reported questionnaire. In this analysis, we focused on five points. First, from the responses regarding infant’s sleeping period the previous day, we determined the number of nocturnal awakenings. We defined ≥ 3 awakenings as too many because a previous study reported that the upper limit of number of awakenings during the night is 2.5 for 1-year-old infants.18 Second, we analysed whether the infants awoke more than once and kept awake for more than 1 h during the night. Third, we analysed the duration of sleep during the night (20:00–7:59). We regarded less than 8 h as unusual. Fourth, we determined bedtime of infants. We defined bedtime after 22:00 as too late. Fifth, we analysed crying at night in the past month. If the mother answered that her infant awoke and cried during the night and that the frequency of crying at night was more than 5 times in a week, we defined the case as crying at night.
Covariates
Information about maternal age at delivery, smoking habits, alcohol consumption, pre-pregnancy body mass index (BMI), parity, gestational age at birth, infertility treatment, type of delivery, small for gestational age, infant sex, maternal psychological distress at 1 year after delivery, physician diagnosis of asthma and atopic dermatitis at 1 year old, and feeding status were collected via self-administered questionnaires and/or medical records. Maternal psychological distress was assessed using the Kessler 619,20, including the questionnaire at 1 year after delivery. According to previous studies, participants with scores of 5 or more were categorised as having distress21.
Statistical analyses
We used a log-binominal regression model to explore the association of NRFS with each outcome and to estimate the risk ratio (RRs) of each outcome and 95% confidence intervals (CIs). We initially adjusted for maternal age at delivery and then further adjusted for smoking habits (never smokers, ex-smokers who quit before pregnancy, smokers during early pregnancy), alcohol consumption (never drinkers, ex-drinkers who quit before pregnancy, drinkers during early pregnancy), pre-pregnancy BMI (< 18.5, 18.5–24.9, ≥ 25.0 kg/m2), parity (0, ≥ 1), infertility treatment (no, ovulation stimulation/artificial insemination by sperm from husband, assisted reproductive technology), type of delivery (vaginal, caesarean section), gestational age at birth (37–38, 39–41 weeks), small for gestational age (yes, no), psychological distress at 1 year after delivery (yes, no), doctor diagnosis of asthma and atopic dermatitis at 1 year old, and feeding (breast milk, synthetic milk, both).
We used a fixed dataset “jecs-an-20180131,” which was released in March 2018. Stata version 15 (StataCorp LP, College Station, Texas, USA) was used for all the analyses.
Results
The baseline characteristics of the present study population with or without NRFS are shown in Table 1. The number of all NRFS cases was 2,475, with a frequency of 4.0%. Among the NRFS cases, 67 cases (2.7%) were tpNRFS, 2,071 cases (83.7%) were fpNRFS. The other 337 cases (13.7%) did not belong to any groups because these cases met only either umbilical cord pH or Apgar scores at 5 min.
Table 2 shows the RRs for NRFS and infant sleep and crying at night. In the multivariable model, we observed the association of all NRFS with shorter sleep time less than 8 h during the night (RR 1.28, 95% CI 1.10–1.49), crying at night (RR 1.17, 95% CI 1.02–1.34) and bedtime after 22:00 (RR 1.10, 95% CI 1.01–1.18). The same associations were also observed only in the fpNRFS cases (RR for short sleep 1.30, 95% CI 1.10–1.54, RR for crying at night = 1.19, 95% CI 1.03–1.39, RR for bedtime after 22:00 = 1.09, 95% CI 1.00–1.18). tpNRFS was not associated with any outcomes.
Discussion
This study showed that children with NRFS before birth tended to have sleep problems at 1 year old. The association of fpNRFS with sleep problems was similar to that of all NRFS with sleep problems. This finding was attributed to children with fpNRFS comprising most of the group with all NRFS. tpNRFS was not associated with any outcomes; however, the number of tpNRFS cases was few, limiting the ability to make conclusions.
The present study had two major limitations. First, there could be unmeasured confounding factors, such as parental life rhythm and other siblings. Second, child sleep was evaluated using a questionnaire for mothers, which might introduce some bias. On the other hand, a strong point of the present study was the large sample size collected nationwide.
We previously reported an association between NRFS and temperament at 1 month after birth14. The present study showed that NRFS before birth appeared to influence sleep at 1 year. The possible reason for this is that temperament and sleep are formed prenatally22,23, and foetal temperament affects heart rate reaction to stress.
It is conceivable that children with sleep problems in early infancy are more likely to have developmental disorders than those without sleep problems. Thus, careful follow up of neonates showing NRFS may lead to early detection of developmental disorders.
On the other hand, the RRs for sleeping problems in the NRFS group for sleep problems were not very large. Further investigations are needed to confirm an association between NRFS and sleeping problems in infants.
In conclusion, fpNRFS may be associated with sleep problems in 1-year-old infants.
Ethical approval
The study protocol was approved by the Ministry of the Environment’s Institutional Review Board on Epidemiological Studies (No. 100406001) and the Ethics Committee of all participating institutions. Written informed consent was obtained from all participants.
References
Paterson, S. J. et al. The importance of temperament for understanding early manifestations of autism spectrum disorder in high-risk infants. J. Autism Dev. Disord. https://doi.org/10.1007/s10803-019-04003-2 (2019).
Sacrey, L.-A.R. et al. Temperament and its association with autism symptoms in a high-risk population. J. Abnorm. Child Psychol. 44, 757–769 (2015).
Humphreys, J. S. et al. Sleep patterns in children with autistic spectrum disorders: A prospective cohort study. Arch. Dis. Child. 99, 114–118 (2014).
Nguyen, A. K. D., Murphy, L. E., Kocak, M., Tylavsky, F. A. & Pagani, L. S. Prospective associations between infant sleep at 12 months and autism spectrum disorder screening scores at 24 months in a community-based birth cohort. J. Clin. Psychiatry 79, 16m11127 (2018)
Sun, Y., Hons, B., Cistulli, P. A. & Hons, M. Childhood Health and Educational Outcomes Associated With Maternal Sleep Apnea : A Population Record-Linkage Study (2014)
Tasnim, N., Mahmud, G. & Akram, S. Predictive accuracy of intrapartum cardiotocography in terms of fetal acid base status at birth. J. Coll. Physicians Surg. Pak. 19, 632–635 (2009).
Curzen, P., Bekir, J. S., McLintock, D. G. & Patel, M. Reliability of cardiotocography in predicting baby’s condition at birth. Obstet. Gynecol. Surv. 40, 344–345 (1985).
Beard, R. W., Filshie, G. M., Knight, C. A. & Roberts, G. M. The significance of the changes in the continuous fetal heart rate in the first stage of labour. BJOG An Int. J. Obstet. Gynaecol. 78, 865–881 (1971).
Ernst, G. Heart-rate variability—more than heart beats?. Front. Public Heal. 5, 1–12 (2017).
Fink, A. M., Bronas, U. G. & Calik, M. W. Autonomic regulation during sleep and wakefulness: a review with implications for defining the pathophysiology of neurological disorders. Clin. Auton. Res. 28, 509–518 (2018).
Harder, R. et al. Heart rate variability during sleep in children with autism spectrum disorder. Clin. Auton. Res. 26, 423–432 (2016).
Precenzano, F., Ruberto, M. & Parisi, L. Sleep habits in children affected by autism spectrum disorders: a preliminary case-control study. Acta Medica Mediterr. 33, 405–409 (2017).
Richdale, A. L. & Prior, M. R. The sleep/wake rhythm in children with autism. Eur. Child Adolesc. Psychiatry 4, 175–186 (1995).
Morokuma, S. et al. Non-reassuring foetal status and neonatal irritability in the Japan Environment and Children’s Study: a cohort study. Sci. Rep. 8, 1–7 (2018).
Michikawa, T. et al. Baseline profile of participants in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 28, 99–104 (2018).
Kawamoto, T. et al. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health 14, 25 (2014).
Okai, T. et al. Intrapartum management guidelines based on fetal heart rate pattern classification. J. Obstet. Gynaecol. Res. 36, 925–928 (2010).
Galland, B. C., Taylor, B. J., Elder, D. E. & Herbison, P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med. Rev. 16, 213–222 (2012).
Kessler, R. C. et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189 (2003).
Toshia, F., Norito, K., Mari, S. & Yutaka, O. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 17, 152–158 (2008).
Sakurai, K., Nishi, A., Kondo, K., Yanagida, K. & Kawakami, N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin. Neurosci. 65, 434–441 (2011).
DiPietro, J. A., Ghera, M. M. & Costigan, K. A. Prenatal origins of temperamental reactivity in early infancy. Early Hum. Dev. 84, 569–575 (2008).
Mirmiran, M., Maas, Y. G. H. & Ariagno, R. L. Development of fetal and neonatal sleep and circadian rhythms. Sleep Med. Rev. 7, 321–334 (2003).
Acknowledgements
We would like to express our gratitude to all the participants in this study and all the individuals involved in data collection. The idea of this work was obtained from other works supported by RIKEN Healthcare and Medical Data Platform Project and JSPS KAKENHI (Grant numbers: JP 16H01880, JP 16K13072, JP 18H00994, JP18H03388). The Japan Environment and Children's Study was funded by the Ministry of the Environment, Japan. The findings and conclusions of this article are solely the responsibility of the authors and do not represent the official views of the Ministry of the Environment.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design: S.M. Statistical analyses: T.M. Drafting of the manuscript and approval of the final content: K.N., S.M., and T.M. Critical revision of the manuscript for important intellectual content and manuscript review: K.N., T.M., S.M., M.O., K.K.(Kiyoko Kato), M.S.(Masafumi Sanefuji), E.S., M.T., M.S.(Masayuki Shimono), T.K., S.O., K.K.(Koichi Kusuhara), and the JECS Group members.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakahara, K., Michikawa, T., Morokuma, S. et al. Non-reassuring foetal status and sleep problems in 1-year-old infants in the Japan Environment and Children’s Study: a cohort study. Sci Rep 10, 11432 (2020). https://doi.org/10.1038/s41598-020-67856-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-67856-z