Abstract
Barrett’s esophagus (BE) predisposes for the malignant condition of esophageal adenocarcinoma (EAC). Since BE patients have few or no symptoms, most of these patients are not identified and not included in surveillance programs. These BE patients are at risk of developing advanced-stage EAC. At present, non-invasive tests to identify BE patients from the general population are lacking. We and others showed that Bone Morphogenetic Protein 4 (BMP4), and other BMPs are upregulated in BE. We aimed to determine if circulating BMPs can be identified and used as blood biomarkers to identify BE patients at high risk in the general population. In this study, we could detect the different BMPs in the blood of 112 BE patients and 134 age- and sex-matched controls. Concentration levels of BMP2, BMP4, and BMP5 were elevated in BE patients, with BMP2 and BMP5 significantly increased. BMP5 remained significant after multivariate analysis and was associated with an increased risk for BE with an OR of 1.49 (p value 0.01). Per log (pg/mL) of BMP5, the odds of having BE increased by 50%. Future optimization and validation studies might be needed to prove its utility as a non-invasive method for the detection of BE in high-risk populations and screening programs.
Similar content being viewed by others
Introduction
Barrett’s esophagus (BE) is a premalignant condition in which the normal epithelial squamous mucosa of the distal esophagus acquires an intestinal columnar phenotype1,2. This metaplastic condition has clinical importance due to its association with an increased risk of esophageal adenocarcinoma (EAC)3. The prevalence of BE is around 1–5% in Western populations1,4, with a yearly conversion rate for EAC between 0.1 and 0.9% in non-dysplastic BE patients5,6,7, 0.5–3% in patients with low-grade dysplasia (LGD)8,9, and 7–13.4% in patients with high-grade dysplasia (HGD)10,11,12. The overall 5-year survival rate of EAC is lower than 20%5,7,13.
Patients diagnosed with BE are included in endoscopic surveillance programs and subjected to periodic follow-up endoscopies for detection and treatment of EAC in the early stage1. As this can improve EAC overall 5-year survival to over 95%, identification of BE patients at risk to progress and subsequent inclusion in surveillance programs is highly important. However, only 5–10% of the EAC’s are detected in surveillance programs14. Thus, most EAC cases present as de novo cancers in advanced stage disease with poor prognosis14. BE by itself does not cause symptoms and is caused by gastro-esophageal reflux disease (GERD). BE patients are mostly diagnosed in case of accompanying symptoms of GERD for which they are examined by endoscopy15. To this end, the design of low-cost and efficient screening methods for the detection of BE in the general population is very desirable.
Blood biomarkers have become an essential tool for diagnosis and disease prognosis. They are simple, minimally invasive, economical, reliable, and rapidly obtainable measures of disease16. Therefore, the use of serologic biomarkers to detect BE is highly appealing since it could be applied for population screening programs to identify patients that need to undergo an endoscopic examination for the diagnosis of BE and should be included in surveillance programs. Consequently, this strategy would minimize the number of patients that will reach late EAC stage and improve the EAC survival rate. However, finding suitable serologic biomarkers for BE and EAC remains a major challenge. Due to methodological limitations, such as low sample size or lack of prospective validation studies, their introduction in the clinic is complicated17.
Bone morphogenetic proteins (BMPs) are multifunctional members of the TGFβ superfamily, which are involved in a wide range of biological processes18,19. BMP4 and its downstream targets have been reported to be present not only in the Barrett’s mucosa but also in the inflamed squamous epithelium as seen in GERD, while they have low expression in healthy squamous mucosa20,21. Proinflammatory factors, such as bile and gastric acids, lead to increased levels of BMP4 in the inflamed esophageal epithelium20,22. We presume that BMP4 may consequently activate stem cells, leading to initiation of gene transcription and enhancing the development of columnar epithelium23.
Several pieces of evidence make BMPs an attractive and suitable candidate as blood biomarkers for BE, since BMPs can be secreted extracellularly as soluble forms19. Previous studies have shown that BMP2, BMP4, BMP7, and BMP9 are present in the bloodstream and associated with several human diseases. For example, BMP2 is elevated in gastric cancer patients but is not associated with disease progression and development of a metastatic stage24,25. Similarly, BMP9 seems to have a role in fracture healing, as circulating levels of BMP9 were high in patients with fast fracture healing26. Furthermore, in patients with chronic kidney disease, circulating BMP2 plays an essential role in calcium deposition in vascular smooth muscles cells and vascular calcification27.
BMPs were not yet studied as potential blood biomarkers for epithelial metaplasia disease, such as in BE. Wang et al.28, described that not only BMP4, but also BMP2, BMP5 and BMP6 gene expression is upregulated in BE. Thus, in this study, we aimed to determine whether BMP2, BMP4, and BMP5 are detected in the plasma of BE patients. When compared to age and sex-matched control groups, we found that BMP2, BMP4, and BMP5 circulating levels were elevated in the BE patient group, with BMP2 and BMP5 showing a significant increase compared to the control group. However, in multivariate analysis, only BMP5 remained significant.
Our results suggest that the detection of BMP5 in plasma could represent a novel, fast, and economical diagnostic strategy to detect BE patients in the overall population. Future studies using a control group with confirmed healthy epithelium is required to validate and further develop the clinical translatability of this test.
Results
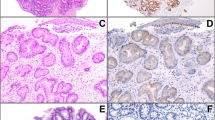
Gene expression analysis
Analysis of BMP2, BMP4 and BMP5 gene expression of BE and normal esophageal squamous epithelium (NS), obtained from the Gene Expression Omnibus (accession number GSE34619), was performed (Fig. 1). Differential expression analysis showed that 6,324 probes were differentially expressed between BE and NS, after excluding unannotated probes. The log fold changes (based on geometric mean) were: BMP2 = 2.63, BMP4 = 2.84, and BMP5 = 2.19.
Study population and patient characteristics
In this study, a total of 246 participants were included. From these, 112 participants were BE patients from Amsterdam University Medical Centers, and 134 participants were sex- and age-matched controls from Amsterdam Blood Biobank, Sanquin. Since active reflux can confound results in terms of BMP expression, 14 BE patients with active reflux were excluded from the study (Fig. 2). The controls and patient demographics and clinical baseline data are shown in Table 1. The baseline characteristics between the two groups were evenly distributed in terms of age and sex. The median age in the BE patient group was 62 years (IQR 54–68) and in the control group 60 years (IQR 57–63), with a high male proportion in both two groups (BE group = 78.6%; control group = 81.3%). All BE cases included in the study group had endoscopically visible BE and intestinal-type of metaplasia, confirmed histologically by at least one experienced pathologist. Patients were endoscopically classified according to the Prague classification, presenting a median circumferential segment (C) of 1 (IQR 0–3) and a median maximum Barrett’s extent (M) of 3 (IQR 2–5). Additional clinical data was only available for the BE cases. Median BMI was 25.6 kg/m2 (IQR 23.8–29.1), where 43.1% patients had a normal weight, 36.7% were overweight, and 20.2% obese. Half of the patients were active or former smokers, and 44% were current alcohol consumers (> 2 units/day).
BMP levels among study groups
The plasma levels of the different BMPs were measured using the ELISA sandwich method in combination with MSD technology. Figure 3 shows the box plots of the distribution of the BMP levels (log-transformed) for patients and controls. Among the analysis, the maximum percentage of imputed values was 2.85% (BMP2). The median concentration of the different biomarkers was generally higher in the patient group. Median concentration levels of BMP5 [2,251.9 pg/mL (IQR 1,210.4–6,865.1 pg/mL)] and BMP2 [317.9 pg/mL (IQR 198.7–475.8 pg/mL)] were significantly higher in patients than controls [BMP5 (1701 pg/mL (IQR 990.9–3,449 pg/mL), p value = 0.01] and BMP2 [248.8 pg/mL (IQR 171.1–393.3 pg/mL), p value = 0.03]. Although the median concentration of BMP4 was higher in the patient group [204.1 pg/mL (IQR 133.1–339.3 pg/mL)], the difference was not statistically significant [BMP4 control group: 173.5 pg/mL (IQR 117.1–252.5 pg/mL), p value = 0.11].
BMP5 is associated with an increased risk of having BE
Initially, we performed univariate logistic regression to assess the effect of each BMP on the risk of having BE separately (Table 2). The higher concentration of BMP5 was significantly associated with an increased risk of BE. The odds ratio (OR) was 1.44 (95% CI 1.12–1.87; p value = 0.01) per pg/mL increase in log-transformed BMP5. Although higher concentrations of BMP4 [OR = 1.11 (95% CI 0.86–1.43; p value = 0.44)] and BMP2 [OR = 1.34 (95% CI 0.98–1.87; p value = 0.07)] were observed in association with risk of having BE as well, these associations were not significant. Additionally, we performed multivariate logistic regression to assess the effect of all BMPs on BE. The OR for having BE decreased for BMP4 (OR = 0.83, 95% CI 0.58–1.15) and BMP2 (OR = 1.23, 95% CI 0.82–1.86), while BMP5 slightly increased (OR = 1.47, 95% CI 1.09–2.02) (Table 2). When adjusting the data for the effect of age and sex, the OR per log-transformed for BMP4 and BMP2 remained the same, while BMP5 improved (OR = 1.49, 95% CI 1.10–2.05) (Table 3). In all logistic regression analyses, the high concentration levels of BMP5 were significantly associated with the increased risk of the presence of BE. Our data suggest that per pg/mL increase in the natural logarithm of plasma concentration of BMP5, the odds of having BE increases by 50%.
Effect of risk factors on BMP5 among BE patients
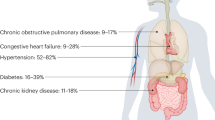
Besides active reflux, increased age (50 years or older), male sex, other risk factors associated with the presence of BE includes high body mass index (BMI), Caucasian race, smoking, and a family history of BE or EAC29,30.
Since BMP5 was the most promising BMP associated with the risk of developing BE, we subsequently performed multivariate analyses of different known risk factors associated with BE together with plasma levels of BMP5 (Table 4). No significant association was observed between BMP5 levels and different patient characteristics. Active smokers showed a weak negative association (β = − 0.38; p value = 0.28), while in patients that consumed alcohol, we observed a weak positive association (β = 0.17; p value = 0.45) with the levels of BMP5.
Discussion
The incidence of EAC is increasing, while the majority of patients with BE, a significant risk factor for EAC, are not diagnosed12. BE patients that are not included in periodic endoscopic surveillance are at risk of developing the advanced stage EAC which is associated with poor outcomes. One way to prevent advanced stage EAC is to detect BE patients in population screening programs. For such programs, efficient, non-invasive and cost-effective tools are required. A potential attractive approach is the use of blood biomarkers as a screening tool for BE.
We and others have previously described the role of BMP4 in BE metaplasia20,21,31,32. Therefore, the use of BMP4 as a candidate circulating biomarker for BE is of great interest. To our knowledge, this is the first study analysing circulating BMPs as a potential biomarker to be used as a screening tool for BE patients. Over the past years, several studies have identified blood-based biomarker candidates33. Some promising studies focused on the determination of single microRNAs or circulating glycoproteins as biomarker candidates34,35. However, most of the studies described in the literature have limited sample size, no age and sex-matched controls, and lack of validation studies, which limits their establishment in the clinic.
BMPs can be secreted as soluble forms in intracellular spaces such as in the esophageal mucosa and detected in the bloodstream19. In the present study, we were able to detect BMP4, BMP2, and BMP5 in the plasma of BE patients, using the MSD detection technology. The MSD detection platform contributed to higher sensitivity and greater range to detect our analytes of choice with a stronger and specific signal when compared with the conventional sandwich ELISA detection method (data not shown). We observed elevated concentration levels of all three BMPs in the patient group when compared with the control group, with a significant difference for BMP2 and BMP5. After multivariate analysis BMP5 proved to remain significant and was the strongest risk factor.
BMP5 has an important role during embryonic musculoskeletal development and has been associated with different human diseases36. In the gastrointestinal system, BMP5 has been described as one of the key proteins to maintain colon crypt stem cell niche in both normal and neoplastic conditions37. Furthermore, BMP5 has been linked as an important tumour suppressor in human colorectal cancer38 and may play an important role in esophageal tumorigenesis in human esophageal squamous cell carcinoma39. However, the levels and role of BMP5 can differ among tumours. Additionally, BMP5 together with BMP4 have a dualistic role in some pancreatic cancer cell lines, acting simultaneously as anti-proliferative factors inhibiting cell growth as well as pro-metastatic factors through stimulation of cell migration and invasion40. Although BMP5 has been seen in osseous metaplasia in colon cancer patients, in esophageal metaplastic diseases, such as BE, the role of BMP5 has not been described41. As far as we know, this is the first association of BMP5 with BE. To better understand the role of BMP5 in BE, further molecular studies should be performed.
Upregulated levels of BMP4 at the protein and mRNA level in BE biopsy samples compared with squamous biopsies have been previously described20,42. In this case–control study, the levels of circulating BMP4 were surprisingly lower when compared with BMP2 and BMP5, and presented no significant difference between BE patients and controls. One possible explanation is that BMP4 is less secreted compared to the other BMPs or that the secreted form is immobilized or masked through binding to other proteins, such as fibrinogen, which is part of plasma composition and known to form complexes with different growth factors such as BMPs43. The relatively lower circulating levels of BMP4 in BE patients might also be the result of their recruitment to the inflamed esophageal epithelium. Therefore, circulating BMP4 may not reflect the alterations occurring in the tissue. A similar situation was observed for other proteins. For instance, cathepsin E mRNA is significantly higher in BE tissue compared to its expression in normal esophageal tissue, yet no significant difference was observed in its serum levels of BE patients and controls44. Additionally, Vrielin et al.45, showed that the mRNA levels of the IGF-system components were significantly higher in the colorectum tissue, while serum IGF-I/-II concentration was not. These observations suggest that local and circulating protein levels can be differently regulated.
For our study, we were able to collect blood samples from a large number of BE patients. Our control samples were obtained from the same geographical region as the BE patients. One limitation of our study, due to privacy matters, is that only information regarding age and sex was provided for the control samples. Therefore, patients with diagnosed or undiagnosed BE are potentially included in the control group. In the geographical region, from which patients were included, it is estimated that 10–20% of the persons have GERD, of which 5–15% may have BE9. Moreover, this might even be an underestimation of the percentage of BE patients in the control group, as the prevalence of BE is even higher in males of 50 years, and older46. Since our control group mainly consisted of middle-aged males, it is most likely that a subset of the controls had BE or active GERD. This limitation probably confounded our results and could explain the high levels of circulating BMPs in specific individuals within the control group. From our patient group we obtained more detailed information about the BE risk factors. When associating the BMP5 levels with these risk factors, none of them was significantly associated with increased BMP5 plasma levels. Thus, BMP5 seems to be an independent risk factor for BE.
In summary, we found that BMP2, BMP4, and BMP5 were higher in the blood of BE patients when compared with sex and age-matched controls. Plasma levels of BMP5 were significantly higher and associated with the risk of BE. In addition, large cohort studies of blood sampling in conjunction with endoscopic analyses in asymptomatic participants would be required to determine whether circulating BMP5 might represent a tool to detect asymptomatic BE. Thus, our study, represents an important stepping stone for the use of circulating BMP5 as a diagnostic test. However, our results need to be validated in larger independent cohorts before implementation in population screening programs.
Methods
Study populations
A total of 112 BE patients were included in our study. All included patients were on long-term proton pump inhibition therapy and had a confirmed diagnosis of BE by endoscopy and histology. BE patients with active reflux were excluded from the study (n = 14). The median age of all patients included was 62 years (range, 54–68 years), and 78.6% of the patients were male.
Peripheral blood samples were collected during the routine surveillance program at the Gastroenterology and Hepatology Department, Amsterdam University Medical Center. Agreed written inform consent was obtained from all patients to participate in this study. The ethical board of the Gastroenterology and Hepatology Department at the Amsterdam University Medical Center granted approval, and the study was conducted according our institution ethical guidelines and the Helsinki Declaration.
Control blood samples of 134 individuals were purchased from Sanquin Blood Supply (The Netherlands). Age and sex in the control group were matched with the patient group, with a median age of 60 years (range 57–63 years) and 81.3% of males.
Blood sample collection and storage
Blood samples from all human participants were collected into 5 mL vacutainer tubes (BD Vacutainer) with Ethylenediaminetetraacetic acid as an anticoagulant. Samples were separated within 2 h of the collection while kept on ice. Samples were spun at 1,500 rpm for 15 min at − 4 °C, aliquoted and stored at − 80 °C until further analysis.
Meso Scale Discovery (MSD) electrochemiluminescence detection
We developed an MSD-based screening platform to quantify circulating BMP2, BMP4, and BMP5. The MSD platform used in this study was a 96-well sandwich immunoassay that incorporated electrochemiluminescence as the basis for detection. A combination of capture and detection antibodies was initially screened for optimal antibody orientation for the sandwich immunoassay to achieve better dynamic range, sensitivity, and specificity. Ultimately, the antibody pairs of the R&D DuoSet ELISA for the respective BMPs were used (BMP4: Cat. No. DY314; BMP2: Cat. No. DY355; BMP5: Cat. No. DY615B; all R&D Systems). The protocol was adapted and performed following the MSD assay workflow steps. Briefly, a quickplex 96-well high-bind plate (Cat. No. L55XB-3, MSD) was coated with 30 µL of coating antibody overnight. The plate was washed four times with washing buffer (Phosphate-Buffered Saline (PBS) with 0.05% Tween-20) and blocked with blocking solution [PBS with 5% Blocker A (Cat. No. R93BA-4, MSD)] and incubated for 1 h. Afterward, plates were washed, and 25 µL of sample or standard were added to the wells and incubated for 2 h at room temperature (RT) with shaking. Samples were discarded, and wells washed. Next, 25 µL of the detection antibody was added and incubated for 2 h at RT with shaking. Subsequently, the detection antibody was discarded, and plates washed. 25 µL of Streptavidin-SulfoTAG (Cat. No. R32AD-5, MSD) was added to the wells and incubated for 1 h at RT with shaking. As a final step, 150 µL of MSD reading buffer (2 × concentrated; Cat. No. R92TC-1, MSD) was added, and the plate was read using the MESO QuickPlex SQ 120 imager and analysed using MSDs Discovery Workbench Software, version 4.0.
Bioinformatics analysis
Gene expression profiles of Barrett’s esophagus and esophageal squamous epithelium were downloaded from the Gene Expression Omnibus (accession number GSE34619). Data had been generated using Affymetrix Human Gene 1.0 ST array and was already pre-processed. 10 profiles from Barrett’s biopsies were compared to 8 profiles from adjacent squamous epithelium. Chip annotation GPL6244 was used for annotation of the probe sets. Differential expression analysis was performed using the Limma package. Probesets with multiple-test corrected p value < 0.05 were considered significantly differentially expressed. The z-scores of the genes of interest were visualized in a heatmap.
Statistical analysis
The concentration of the different biomarkers was imputed when measurements were out of range of the calibration curve (either too low [bellow lower limit of detection (< LOD)] or too high) based on a maximum likelihood estimation procedure47. Imputation is a statistic strategy that produces unbiased estimations to minimize extreme data values. For the imputation of samples < LOD, we used the empirical LOD across all plates as the upper bound. For imputation of samples with a concentration exceeding the calibration curve, we used a value of twice the highest observed concentration that was not out of range as the upper bound. Categorical variables were expressed as counts and corresponding percentages, continuous data were presented as the median and interquartile range (IQR).
To reduce the effect of extreme values, log-transformation of the different proteins has been used in all analyses. The concentration of the biomarkers between BE patients and the control group were first compared using the Mann–Whitney test. Additionally, to assess the effect of protein biomarkers on developing BE, univariate and multivariate logistic regression was performed. The analysis was performed in statistical software R (version 3.5.1). p values < 0.05 were considered statistically significant.
References
Spechler, S. J. & Souza, R. F. Barrett’s esophagus. N. Engl. J. Med. 371, 836–845 (2014).
Wild, C. P. & Hardie, L. J. Reflux, Barrett’s oesophagus and adenocarcinoma: burning questions. Nat. Rev. Cancer 3, 676–684 (2003).
Bird-Lieberman, E. L. et al. Population-based study reveals new risk-stratification biomarker panel for Barrett’s esophagus. Gastroenterology 143, 927–935 (2012).
Amadi, C. & Gatenby, P. Barrett’s oesophagus: current controversies. World J. Gastroenterol. 23, 5051–5067 (2017).
Parasa, S. et al. Estimating neoplasia detection rate (NDR) in patients with Barrett’s oesophagus based on index endoscopy: a systematic review and meta-analysis. Gut https://doi.org/10.1136/gutjnl-2018-317800 (2019).
di Pietro, M., Fitzgerald, R. C. & BSG Barrett’s guidelines working group. Revised British Society of Gastroenterology recommendation on the diagnosis and management of Barrett’s oesophagus with low-grade dysplasia. Gut 67, 392–393 (2018).
Thrift, A. P. The epidemic of oesophageal carcinoma: where are we now?. Cancer Epidemiol. 41, 88–95 (2016).
Singh, S. et al. Incidence of esophageal adenocarcinoma in Barrett’s esophagus with low-grade dysplasia: A systematic review and meta-analysis. Gastrointest. Endosc. 79, 897 (2014).
Shaheen, N. J., Falk, G. W., Iyer, P. G. & Gerson, L. B. ACG clinical guideline: diagnosis and management of Barrett’s esophagus. Am. J. Gastroenterol. 111, 30 (2015).
Singh, T., Sanaka, M. R. & Thota, P. N. Endoscopic therapy for Barrett’s esophagus and early esophageal cancer: where do we go from here?. World J. Gastrointest. Endosc. 10, 165–174 (2018).
Curvers, W. L. et al. Low-grade dysplasia in Barrett’s esophagus: overdiagnosed and underestimated. Am. J. Gastroenterol. 105, 1523–1530 (2010).
Rastogi, A. et al. Incidence of esophageal adenocarcinoma in patients with Barrett’s esophagus and high-grade dysplasia: a meta-analysis. Gastrointest. Endosc. 67, 394–398 (2008).
Rhee, H. & Wang, D. H. Cellular origins of Barrett’s esophagus: the search continues. Curr. Gastroenterol. Rep. 20, 51 (2018).
Di Pietro, M., Alzoubaidi, D. & Fitzgerald, R. C. Barrett’s esophagus and cancer risk: how research advances can impact clinical practice. Gut Liver 8, 356–370 (2014).
di Pietro, M., Chan, D., Fitzgerald, R. C. & Wang, K. K. Screening for Barrett’s esophagus. Gastroenterology 148, 912–923 (2015).
Pepe, M. S. et al. Phases of biomarker development for early detection of cancer. J. Natl. Cancer Inst. 93, 1054–1061 (2001).
Yazbeck, R., Jaenisch, S. E. & Watson, D. I. From blood to breath: new horizons for esophageal cancer biomarkers. World J. Gastroenterol. 22, 10077–10083 (2016).
Davis, H., Raja, E., Miyazono, K., Tsubakihara, Y. & Moustakas, A. Mechanisms of action of bone morphogenetic proteins in cancer. Cytokine Growth Factor Rev. 27, 81–92 (2016).
Bragdon, B. et al. Bone morphogenetic proteins: a critical review. Cell. Signal. 23, 609–620 (2011).
Milano, F. et al. Bone morphogenetic protein 4 expressed in esophagitis induces a columnar phenotype in esophageal squamous cells. Gastroenterology 132, 2412–2421 (2007).
Mari, L. et al. A pSMAD/CDX2 complex is essential for the intestinalization of epithelial metaplasia. Cell Rep. 7, 1197–1210 (2014).
Badreddine, R. J. & Wang, K. K. Barrett esophagus: an update. Nat. Rev. Gastroenterol. Hepatol. 7, 369–378 (2010).
Conteduca, V. et al. Barrett’s esophagus and esophageal cancer: An overview. Int. J. Oncol. 41, 414–424 (2012).
Park, Y. et al. The Bone Morphogenesis Protein-2 (BMP-2) is associated with progression to metastatic disease in gastric cancer. Cancer Res. Treat. 40, 127–132 (2008).
Park, Y. et al. Bone morphogenetic protein-2 levels are elevated in the patients with gastric cancer and correlate with disease progression. Med. Oncol. 27, 1192–1199 (2010).
van Baardewijk, L. J. et al. Circulating bone morphogenetic protein levels and delayed fracture healing. Int. Orthop. 37, 523–527 (2013).
Rong, S. et al. Vascular calcification in chronic kidney disease is induced by bone morphogenetic protein-2 via a mechanism involving the Wnt/β-catenin pathway. Cell. Physiol. Biochem. 34, 2049–2060 (2014).
Wang, J. et al. Differential gene expression in normal esophagus and Barrett’s esophagus. J. Gastroenterol. 44, 897–911 (2009).
Sami, S. S. & Iyer, P. G. Recent advances in screening for Barrett’s esophagus. Curr. Treat. Options Gastroenterol. 16, 1–14 (2018).
Inadomi, J. et al. Recent advances in Barrett’s esophagus. Ann. N. Y. Acad. Sci. https://doi.org/10.1111/nyas.13909 (2018).
Castillo, D. et al. Activation of the BMP4 pathway and early expression of CDX2 characterize non-specialized columnar metaplasia in a human model of Barrett’s esophagus. J. Gastrointest. Surg. 16, 227–237 (2012).
Sun, Y.-G., Wang, H.-B., Wang, W.-Q., Wang, X.-W. & Fang, D.-C. Acid and bile salt up-regulate BMP4 expression in human esophageal epithelium cells AU—Zhou, Gang. Scand. J. Gastroenterol. 44, 926–932 (2009).
O’Donovan, M. & Fitzgerald, R. C. Screening for Barrett’s esophagus: are new high-volume methods feasible?. Dig. Dis. Sci. 63, 2105–2114 (2018).
Bus, P. et al. Profiling of circulating microRNAs in patients with Barrett’s esophagus and esophageal adenocarcinoma. J. Gastroenterol. 51, 560–570 (2016).
Shah, A. K. et al. Evaluation of serum glycoprotein biomarker candidates for detection of esophageal adenocarcinoma and surveillance of Barrett’s esophagus. Mol. Cell. Proteom. 17, 2324–2334 (2018).
Wang, R. N. et al. Bone morphogenetic protein (BMP) signaling in development and human diseases. Genes Dis. 1, 87–105 (2014).
Kosinski, C. et al. Gene expression patterns of human colon tops and basal crypts and BMP antagonists as intestinal stem cell niche factors. Proc. Natl. Acad. Sci. 104, 15418–15423 (2007).
Chen, E. et al. Alteration of tumor suppressor BMP5 in sporadic colorectal cancer: a genomic and transcriptomic profiling based study. Mol. Cancer 17, 176 (2018).
Zhou, J. et al. Gene expression profiles at different stages of human esophageal squamous cell carcinoma. World J. Gastroenterol. 9, 9–15 (2003).
Virtanen, S., Alarmo, E. L., Sandström, S., Ampuja, M. & Kallioniemi, A. Bone morphogenetic protein-4 and -5 in pancreatic cancer-Novel bidirectional players. Exp. Cell Res. 317, 2136–2146 (2011).
Liu, X., Xu, J. & Chen, L. Colorectal carcinoma with osseous metaplasia. Oncotarget 8, 65407–65413 (2017).
Kestens, C., Siersema, P. D., Offerhaus, G. J. A. & van Baal, J. W. P. M. BMP4 signaling is able to induce an epithelial-mesenchymal transition-like phenotype in Barrett’s esophagus and esophageal adenocarcinoma through induction of SNAIL2. PLoS ONE 11, e0155754 (2016).
Martino, M. M., Briquez, P. S., Ranga, A., Lutolf, M. P. & Hubbell, J. A. Heparin-binding domain of fibrin(ogen) binds growth factors and promotes tissue repair when incorporated within a synthetic matrix. Proc. Natl. Acad. Sci. https://doi.org/10.1073/pnas.1221602110 (2013).
Fisher, O. M. et al. High expression of cathepsin E in tissues but not blood of patients with Barrett’s esophagus and adenocarcinoma. Ann. Surg. Oncol. 22, 2431–2438 (2015).
Vrieling, A. et al. Expression of insulin-like growth factor system components in colorectal tissue and its relation with serum IGF levels. Growth Horm. IGF Res. 19, 126–135 (2009).
Kuipers, E. J. & Spaander, M. C. Natural history of Barrett’s esophagus. Dig. Dis. Sci. 63, 1997–2004 (2018).
Lubin, J. H. et al. Epidemiologic evaluation of measurement data in the presence of detection limits. Environ. Health Perspect. 112, 1691–1696 (2004).
Acknowledgements
This work was supported by the European Research Council (ERC) starting grant: ERC-StG 282079 TargetS4Barrett and ERC-POC 632258 BMP4EAC.
Author information
Authors and Affiliations
Contributions
A.C.P.C., S.C., and K.K.K. designed experiments; A.C.P.C. and M.C.S.-S. performed experiments; A.C.P.C collected data; A.C.P.C and N.M. conducted the statistical analysis; S.J.H and P.S.K organized and collected patient material; A.C.P.C., S.C., and K.K.K interpreted the data; and A.C.P.C. wrote the manuscript with input from all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Correia, A.C.P., Calpe, S., Mostafavi, N. et al. Detection of circulating BMP5 as a risk factor for Barrett’s esophagus. Sci Rep 10, 15579 (2020). https://doi.org/10.1038/s41598-020-70760-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-70760-1