Abstract
Logistic regression analysis has widespread applications in clinical disease diagnosis, but it has not yet been applied to assess the acceptance of radiotherapy and chemotherapy in patients with lung cancer. A prediction model was established to investigate the influencing factors of radiotherapy and chemotherapy in lung cancer patients in order to provide useful information for clinicians to develop targeted and effective treatment. A sample was admitted of lung cancer patients to Binzhou Medical University Hospital stays from January 2020 to June 2021. After investigating doctors, nurses, patients, managers and conducting expert demonstration, the questionnaire was formed. The questionnaire was filled out by the patient or the patient's family members. The factors in the questionnaire data of patients accepting and not accepting radiotherapy and chemotherapy were compared for univariate analysis, and the significantly different single factor were analyzed by multifactor logistic regression analysis, explored the influencing factors of radiotherapy and chemotherapy in lung cancer patients established a predictive model and drew the receiver operating characteristic curve (ROC curve). The factors of two groups had statistically significant differences or no statistically significant differences. After multifactor logistic regression analysis was conducted, own personality, self-care ability, disease course classification, own attitude towards disease treatment, and family attitude towards disease treatment were included in the influencing factors of radiotherapy and chemotherapy in patients with lung cancer. Then, a predictive model was established. The area under the ROC curve of the predicted model was 0.973, the 95% confidence interval was 0.952–0.995, the optimal critical value was 0.832, the sensitivity was 91.84%, the specificity was 89.09%, and the accuracy was 90.85%. Based on logistic regression analysis, the prediction model could predict the extent of accepting radiotherapy and chemotherapy in patients with lung cancer. Understanding the factors related to patients with lung cancer accepting radiotherapy and chemotherapy could provide useful information for the targeted and effective treatment by clinicians.
Similar content being viewed by others
Introduction
Cancer incidence and mortality rates have been rising in China, and starting from 2010, cancer has become the number one cause of death in China and a major public health problem in the country1. In this past year alone, lung cancer occurred in approximately 135,000 patients, and it was responsible for 132,000 deaths in the United States2. Lung cancer has remained the leading cause of cancer deaths worldwide3.
Thus far, the four main treatments for lung cancer are surgery, radiotherapy, chemotherapy, and bio-targeted therapy4,5,6,7,8. Patients with early lung cancer, that is stages 1 and 2, could first consider surgical treatment in accordance with the treatment norms9,10. Adjuvant treatment after surgery and inoperable lung cancer need radiotherapy and chemotherapy11. According to statistics, approximately 60% of all patients with lung cancer may need to accept radiotherapy and chemotherapy, which play a very important role in the treatment of lung cancer12. Radiotherapy and chemotherapy could kill cancer cells and reduce the chance of spreading13,14. A certain course of radiotherapy and chemotherapy treatment could improve the control of the disease, and it has a positive treatment significance for delaying the development speed of the disease and improving the quality of life15. For various reasons such as anxiety, worry about the quality of life, many patients with lung cancer are not willing to accept radiotherapy and chemotherapy treatment16,17. In order to improve the quality of life of lung cancer patients, it is necessary for clinicians to make the best diagnosis and treatment plan for lung cancer patients, and to further understand the influencing factors of lung cancer patients receiving radiotherapy and chemotherapy. In some past studies, it has been shown that the most important factors affecting patients receiving chemotherapy are age, sex, financial status, whether reimbursement is provided, rural and urban of patients. Logistic regression analysis generally starts with a univariate analysis, which can provide information about the characteristics of the data distribution. The main purpose of univariate analysis is to explore the form of independent variables into the model to better describe the relationship between dependent variables and the second, some potentially meaningless variables can be eliminated to reduce the number of variables in multivariate analysis and ensure the stability and simplicity of the results. Multivariate analysis is more complex than univariate analysis, and it is favored by researchers, considering the correlation among various variables. In the present study, to understand the degree of acceptance of radiotherapy and chemotherapy for patients with lung cancer, the intention of recent patients with lung cancer to accept radiotherapy and chemotherapy was investigated. Logistic regression analysis of the influencing factors was also conducted to provide useful information for clinicians to carry out targeted and effective treatment for the benefit of more patients.
Methods
Setting, participants, and study design
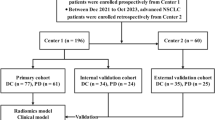
A total of 160 patients with lung cancer who were hospitalized at the Binzhou Medical University Hospital from January 2020 to June 2021 were randomly selected. The inclusion criteria were as follows: pathologically diagnosed with lung cancer, with informed consent, and under voluntary cooperation. Patients with cognitive dysfunction were excluded. This study was approved by the Ethics Committee.
The research team consulted the literature; investigated doctors, nurses, patients, and managers; and conducted expert demonstration to form a questionnaire. The research content included whether to accept radiotherapy and chemotherapy, gender, age, cultural level, own personality, own income, acceptance of payment ratio, family economy, self-care ability, disease course classification, understanding of radiotherapy and chemotherapy, own attitude towards disease treatment, family attitude towards disease treatment, and knowledge of lung cancer. The investigation study was divided into two groups on the basis of whether to accept radiotherapy and chemotherapy. The questionnaire belongs to a descriptive study.
Data analysis
SPSS 25.0 software was used in all statistical analyses. The observation data were counting data, represented by examples. The factors in the questionnaire data of patients accepting and not accepting radiotherapy and chemotherapy were compared for univariate analysis. χ2 test was used to compare the differences between groups. Multifactor logistic regression analysis was conducted to analyze two statistically significant groups, the influencing factors of radiotherapy and chemotherapy among patients with lung cancer were explored, and a predictive model was established. The receiver operating characteristic (ROC) curve was used to determine the predictive value of the regression model. P < 0.05 indicated statistically significant difference.
Ethics approval and consent to participate
The study was reviewed and approved by the Review Boards of the Binzhou Medical University Hospital. The research methods and questionnaires used in this study were performed in accordance with the relevant guidelines of Binzhou Medical University Hospital on scientific research and the regulations of Binzhou Medical University Hospital on questionnaire survey and return visit. All participants agreed to and signed the written informed consent form prior to enrollment into the study.
Results
General information
In this survey, 160 questionnaires were issued, and 160 questionnaires were recovered, with a recovery rate of 100%. Upon excluding incomplete questionnaires, 153 questionnaires were analyzed, with an efficiency of 95.63%. A total of 96 questionnaires belonged to the accept group (62.75%), and 57 questionnaires belonged to the not-accept group (37.25%).
Univariate analysis of the two groups
In the two groups of data, age, own personality, own income, family economy, self-care ability, disease course classification, understanding of radiotherapy and chemotherapy, own attitude towards disease treatment, family attitude towards disease treatment, and knowledge of lung cancer showed statistical significance (P < 0.05). On the contrary, gender, cultural level, acceptance of payment ratio exhibited no statistically significant difference (P > 0.05), as shown in Table 1.
Multifactor logistic regression analysis
This study established a multi-factor logistic regression model to determine whether or not to receive radiotherapy and chemotherapy is the stress variable, assigned as 1 = yes and 2 = No. The indicators of P < 0.05 in the univariate analysis (Table 1) were taken as independent variables. Age, own personality, and other 10 factors were taken as independent variables (variable assignment in Table 2). The regression process adopted gradual regression method and included independent variable selection and elimination. P > 0.05 values were excluded, while P < 0.05 values were selected.
Regression results. The multifactor logistic regression analysis found that own personality, self-care ability, disease course classification, own attitude towards disease treatment, and family attitude towards disease treatment were factors affecting the radiotherapy and chemotherapy of patients with lung cancer. As shown in Table 3, the prediction model expression is as follows: Logit (P) = − 18.785 + 1.854X1 + 1.93X2 + 1.691X3 + 2.03X4 + 2.418X5, where covariates X1, X2, X3, X4, and X5 refer to own personality, self-care ability, disease course classification, own attitude towards disease treatment, and family attitude towards disease treatment, respectively.
Comparison of ROC curves of prediction model and various factors
The area under the ROC curve of the predicted model was 0.973, the 95% confidence interval (CI) was 0.952–0.995, the optimal critical value was 0.832, the sensitivity was 91.84%, the specificity was 89.09%, and the accuracy was 90.85%. Further details are shown in Table 4 and Fig. 1.
Discussion
As a clinically important treatment means and strategy, the radiotherapy and chemotherapy for lung cancer, similar to other treatment methods, has advantages and disadvantages18,19. They reflect the basic principles of multidisciplinary comprehensive treatment of tumors20. Patients have the greatest clinical benefit, which could not only quickly remove peripheral circulating cancer cells and hidden metastatic metastases but also rapidly reduce local primary lesions to relieve local oppression and local invasion symptoms and improve the quality of life of patients21. Clinically, the side effects of radiotherapy and chemotherapy could not be underestimated, including the so-called body injury side, such as eating difficulties caused by radioactive esophagitis22, cough and breathing difficulties caused by radioactive pneumonia23, abnormal brain cognitive behavior caused by radiotherapy and chemotherapy24, and gastrointestinal dysfunction25. Doctors need to weigh the pros and cons clinically, combined with the situation of the family members, and make calm and rational choices rather than the same synchronization26. A specific individualized treatment plan must be established in accordance with each patient’s own situation, psychological condition, the disease itself, and the specific situation of the family members..
Univariate analysis of the two groups of data showed statistical significance in age, own personality, own income, family economy, self-care ability, disease course classification, understanding of radiotherapy and chemotherapy, own attitude towards disease treatment, family attitude towards disease treatment, and knowledge of lung cancer (P < 0.05), whereas no statistical difference was found in gender, cultural level, and acceptance of payment ratio (P > 0.05). The findings demonstrated that these three factors have no effect on whether or not patients with lung cancer accept radiotherapy and chemotherapy. Further logistic regression analysis of factors with statistical significance found that five indicators, such as own personality, self-care ability, disease course classification, own attitude towards disease treatment, and family attitude towards disease treatment, were retained in the regression model (P < 0.05). Age, income, family economy, understanding of radiotherapy and chemotherapy, and knowledge of lung cancer were excluded. In the past 10 years, the level of population education in China has made a new and relatively significant leap, and we can gain more "population quality dividend" in the era of the popularization of higher education. The improvement of people's education level has enhanced the understanding of disease treatment, and given full play to their own initiative.
In Chinese custom, a previous preference for men over women exists. However, in this study, gender was not an influencing factor, indicating that Chinese people today have basically eliminated the preference for men over women and treat both genders equally. Age was also not an influencing factor, indicating that the idea of respecting and loving the elderly in traditional social culture has always existed and that treatment has not been given up because of their old age, different from the African diaspora27. All of the above factors were not affected by the level of knowledge and culture. Therefore, cultural level was excluded. Acceptance of payment ratio, own income, and family economy were three factors related to treatment cost, which was not an influencing factor as it did not affect whether or not patients with lung cancer accept radiotherapy and chemotherapy. Treatment cost is related to the improvement of people’s living standards, the substantial growth of gross national product, and the implementation of national medical care since the reform and opening up. The understanding of radiotherapy and chemotherapy and the knowledge of lung cancer were not included, indicating that treating a disease is necessary, seeing a doctor is deeply rooted in the hearts of sick people, and the people’s awareness of seeking medical treatment is gradually improved28. Logistic analysis showed that among the five factors, own personality, which is a psychological factor; self-care ability; disease classification, which is the disease itself; and own and family attitudes towards disease treatment further affected the decision of patients with lung cancer to accept radiotherapy and chemotherapy factors. The above factors could help clinicians determine further treatment.
The limitations of the study are based on a small sample size belonging to a population of cultural background (China). If the same study were conducted in the populations of other countries of different cultural, economic, and social environments, then the results would be different outcomes. It would be impactful if such studies and models were used for similar objectives in different parts of the world to have a more wholesome understanding of influencing factors. In the future, we will further expand the sample size, increase the depth and breadth of the questionnaires, introduce more effects into the study, and improve the reliability of the conclusions.
Conclusions
The five indicators (including own personality, self-treatment ability, disease course classification, own attitude towards the treatment of disease, and family attitude towards the treatment of disease) are the main factors for accepting radiotherapy and chemotherapy treatment among patients with lung cancer. The predictive model based on logistic regression analysis could better predict the extent of accepting radiotherapy and chemotherapy. Understanding the factors related to patients with lung cancer could provide useful information for the targeted and effective treatment by clinicians.
Data availability
Datasets are available in the manuscript. Any additional information and data are available upon reasonable request. The data and materials can be shared with corresponding author upon reasonable request.
Abbreviations
- ROC:
-
Receiver operating characteristic
- CI:
-
Confidence interval
References
Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J. Clin. 66, 115–132 (2016).
Siegel, R. L. et al. Cancer statistics, 2021. CA Cancer J. Clin. 71, 7–33 (2021).
Xu, R. et al. The momentous role of N6-methyladenosine in lung cancer. J. Cell Physiol. 236, 3244–3256 (2021).
Scherpereel, A. et al. ERS/ESTS/EACTS/ESTRO guidelines for the management of malignant pleural mesothelioma. Eur. Respir. J. 55, 1900953 (2020).
Passaro, A. et al. Severity of COVID-19 in patients with lung cancer: Evidence and challenges. J. Immunother. Cancer 9, e002266 (2021).
Fiore, M. et al. Histologic transformation to small-cell lung cancer following gefitinib and radiotherapy in a patient with pulmonary adenocarcinoma. Tumori. J. 105, P12–P16 (2019).
Yang, Z. M. et al. Analysis of CEA expression and EGFR mutation status in non-small cell lung cancers. Asian Pac. J. Cancer Prev. 15, 3451–3455 (2014).
Wang, G. D. et al. X-Ray induced photodynamic therapy: A combination of radiotherapy and photodynamic therapy. Theranostics 6, 2295–2305 (2016).
Okami, J. Treatment strategy and decision-making for elderly surgical candidates with early lung cancer. J. Thorac. Dis. 11, S987–S997 (2019).
Kang, N. et al. Treatment modality and outcomes among early-stage non-small cell lung cancer patients with COPD: A cohort study. J. Thorac. Dis. 12, 4651–4660 (2020).
Ramella, S. et al. Radiotherapy in Italy for non-small cell lung cancer: Patterns of care survey. Tumori. J. 98, 66–78 (2012).
Chu, D. T. et al. Patient attitudes towards chemotherapy and survival: A prospective observational study in advanced non-small cell lung cancer. Lung Cancer 66, 250–256 (2009).
Cao, G. D. et al. The oncolytic virus in cancer diagnosis and treatment. Front Oncol. 10, 1786 (2020).
Hosoya, N. & Miyagawa, K. Targeting DNA damage response in cancer therapy. Cancer Sci. 105, 370–388 (2014).
Correa, D. D. et al. Longitudinal cognitive assessment in patients with primary CNS lymphoma treated with induction chemotherapy followed by reduced-dose whole-brain radiotherapy or autologous stem cell transplantation. J. Neurooncol. 144, 553–562 (2019).
Jacobsen, M. M. et al. Timeliness of access to lung cancer diagnosis and treatment: A scoping literature review. Lung Cancer 112, 156–164 (2017).
Hammad, A. et al. “NRF2 addiction” in lung cancer cells and its impact on cancer therapy. Cancer Lett. 467, 40–49 (2019).
Negi, H. et al. Anterior Gradient-2 monoclonal antibody inhibits lung cancer growth and metastasis by upregulating p53 pathway and without exerting any toxicological effects: A preclinical study. Cancer Lett. 449, 125–134 (2019).
Linton, A. et al. Geographic and socioeconomic factors in patients with malignant pleural mesothelioma in New South Wales and their impact upon clinical outcomes. Respirology 22, 978–985 (2017).
Storey, C. L., Hanna, G. G. & Greystoke, A. Practical implications to contemplate when considering radical therapy for stage III non-small-cell lung cancer. Br. J. Cancer 123, 28–35 (2020).
Mitchell, K. G. et al. Improved overall survival with comprehensive local consolidative therapy in synchronous oligometastatic non-small-cell lung cancer. Clin. Lung Cancer 21, 37–46 (2020).
Qiu, Y. et al. Effect of whole-course nutrition management on patients with esophageal cancer undergoing concurrent chemoradiotherapy: A randomized control trial. Nutrition 69, 110558 (2020).
Li, N. et al. Analysis of related factors of radiation pneumonia caused by precise radiotherapy of esophageal cancer based on random forest algorithm. Math. Biosci. Eng. 18, 4477–4490 (2021).
Parente, A. et al. Delayed effects of a single-dose whole-brain radiation therapy on glucose metabolism and myelin density: A longitudinal PET study. Int. J. Radiat. Biol. 96(9), 1135–1143 (2020).
Andreyev, H. et al. The FOCCUS study: A prospective evaluation of the frequency, severity and treatable causes of gastrointestinal symptoms during and after chemotherapy. Support Care Cancer 29, 1443–1453 (2021).
Anna, M. et al. Professional duties are now considered legal duties of care within genomic medicine. Eur. J. Hum. Genet. 28, 1301–1304 (2020).
Mouton, C. P. & Southerland, J. H. Elder Abuse in the African diaspora: A review. J. Natl. Med. Assoc. 109, 262–271 (2017).
Saloner, B. & Maclean, J. C. Specialty substance use disorder treatment admissions steadily increased in the four years after medicaid expansion. Health Aff. (Millwood) 39, 453–461 (2020).
Acknowledgements
We would like to thank the library of Binzhou Medical University, In particular, we wish to acknowledge the efforts of many individuals who participated as volunteers in the clinical study reported here.
Funding
This work was supported by Shandong Province Medical and Health Science and Technology Development Plan (2019ws611, 202009010691).
Author information
Authors and Affiliations
Contributions
Project initiation: Y.L., supervision of clinical study: M.C. Statistical methodology and Data analysis: C.X. Clinical sample and data collection, processing: C.X. Review & editing of manuscript: all authors. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Y., Xu, C., Xing, C. et al. Influencing factors and prediction methods of radiotherapy and chemotherapy in patients with lung cancer based on logistic regression analysis. Sci Rep 12, 21094 (2022). https://doi.org/10.1038/s41598-022-25592-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-25592-6