Abstract
Brain metastases (BMs) are common in lung adenocarcinomas (ACs). Thyroid transcription factor 1 (TTF-1) is important in the diagnosis of AC. This study aimed to examine the relationship between TTF-1 and BM for the first time in literature. The data of 137 patients with AC that developed BM between 2009 and 2020 were retrospectively analyzed. A total of 137 patients, 120 (87.6%) male, and 17 (12.4%) female were examined. Their mean age was 59.78 ± 0.82 years. The Eastern Cooperative Oncology Group (ECOG) performance score was 0–1 (< 2) for 39 (28.5%) patients and 2–4 (≤ 2) for 98 (71.5%). TTF-1 was positive in 100 (73%) patients and negative in 37 (27%). More than five BMs were present in 102 (74.4%) patients and less than five in 35 (25.6%). All the patients received whole-brain radiotherapy. None of the patients was suitable for surgery or radiosurgery. The median survival time was 6.4 [95% confidence interval (CI), 5.67–7.1] months. The survival time was 7 (95% CI, 5.91–8.09) months for the TTF-1 (+) patients and 5.8 (95% CI, 4.1–7.5) months for the TTF-1 (−) patients. In the univariate analysis, there was a significant relationship between survival time and age (p = 0.047), TTF-1 (p = 0.024), and ECOG performance score (p = 0.002). The multivariance analysis revealed a significant relationship between survival and TTF-1 (p = 0.034) and ECOG score (p = 0.007). We found a correlation between survival time and ECOG performance score and TTF-1. TTF-1 can be used as a biomarker to monitor prognosis in the follow-up and treatment of patients with AC that develop BM.
Similar content being viewed by others
Introduction
Due to the advances in diagnosis and treatment in recent years, the life expectancy of cancer patients has been prolonged. However, there has been no decrease in the incidence of brain metastases (BM)1. Lung cancer constitutes 40–60% of BM2,3,4. The most common non-small cell lung cancer that metastasizes to the brain is lung adenocarcinoma (AC). Thyroid transcription factor 1 (TTF-1) is a transcription protein that is positive in 70–80% of ACs, and it is used in the diagnosis of AC5. In recent years, studies have shown that TTF-1 is not only an important diagnostic but also a prognostic and predictive marker in patients with Acs6. However, the relationship between BM in AC and TTF-1 remains unknown. Therefore, in this study, we retrospectively evaluated AC cases that developed BM during their follow-up in our center.
Materials and methods
Study population
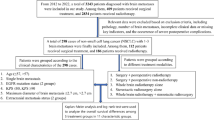
Patients who were followed up with a diagnosis of AC and developed BM between 2009 and 2020 in the Medical Oncology Department of Manisa City Hospital were retrospectively analyzed. The study included patients with stage 4 AC, aged 18 years or older, who were found to have BM at the time of diagnosis or developed BM during their follow-up. The patients were negative for c-ros oncogene 1(ROS-1), anaplastic lymphoma kinase (ALK), and epidermal growth factor receptor (EGFR) mutation. The BM diagnosis was made based on brain magnetic resonance images.
Data collection
The patient's demographic characteristics, such as age and sex, ECOG performance scores, number of BM, TTF-1 results, and their relationship with survival were examined. TTF-1 was examined from the first lung biopsies of the patients at the time of diagnosis in all patients Sections of 3–5 micron thickness were prepared for the immunohistochemical examination. Ventana brand fully automatic staining device (Ventana Medical System, Tucsons, AZ, USA) was used for immunohistochemical studies. TTF-1 (Clone SPT24, NovaCastra, 1:50 dilution) as primary antibody was manually instilled and incubated at 37 °C. Pneumocytes were evaluated as an internal control for TTF-1, and nuclear staining was considered positive. The patients were divided into groups according to the number of BM (< 5 and ≥ 5), the Eastern Cooperative Oncology Group (ECOG) performance score (< 2 and ≥ 2), and age (< 65, ≥ 65). To obtain the survival time of the patients, the time from the date of diagnosis to mortality or the time to the last follow-up for the patients who survived was calculated.
Statistical analysis
Descriptive statistics were presented as mean, standard deviation, median, minimum and maximum values for numerical variables, and as numbers and percentages for categorical variables. The comparison of numerical variables between two independent groups was performed using Student’s t-test in case of normal distribution and the Mann–Whitney U test otherwise. Rates were compared between the groups using the chi-square analysis and Fisher’s exact test. Survival analyses were undertaken with the Kaplan–Meier method. Determinative factors were examined using the Cox regression analysis. p < 0.05 was considered as significant in all statistical analyses.
Ethical approval
The study was conducted by the principles of the Declaration of Helsinki and reviewed and approved by the Health Sciences Ethics Committee of Manisa Celal Bayar University (Decision no: 20.478.486, Date 05.02.2020). This study was designed retrospectively. Informed consent has been waived by the Health Sciences Ethics Committee of Manisa Celal Bayar University.
Results
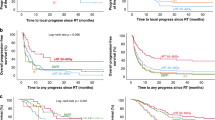
A total of 137 patients, 120 (87.6%) male, and 17 (12.4%) female were examined. Their mean age was 59.78 ± 0.82 years. Thirty-nine (28.5%) patients had an ECOG performance score of 0–1 while 98 (71.5%) had an ECOG performance score of 2–4. TTF-1 was positive in 100 (73%) patients and negative in 37 (27%). More than five BM were present in 102 (74.4%) patients and less than five in 35 (25.6%) (Table 1). All the patients received radiotherapy to the whole brain. None of the patients was suitable for surgery or radiosurgery. The median survival time of the patients was 6.4 (95% CI, 5.67–7.1) months. The survival time was 7 (95% CI, 5.91–8.09) months for the TTF-1 (+) patients and 5.8 (95% CI, 4.1–7.5) months for the TTF-1 (−) patients. In the univariate analysis, survival time had a significant relationship with age (p = 0.047), TTF-1 (p = 0.024), and ECOG performance score (p = 0.002) (Figs. 1 and 2). The multivariance analysis showed a significant relationship between survival and TTF-1 (p = 0.034) and ECOG performance score (p = 0.007) (Table 2).
Discussion
BM is an important cause of mortality and morbidity. With the development of BM, the life expectancy of patients is significantly shortened, reducing to four to six months. Studies have also found that the prognosis of these patients is related to the number of BM, their performance score, the presence or absence of metastasis outside the brain, and advanced age. These clinical and radiological findings are frequently used in daily practice7,8,9,10,11. However, a standard biomarker that will show the prognosis in patients with BM has not yet been found. Therefore, we conducted this study to examine the relationship between TTF-1 and BM.
TTF-1 is a transcription protein involved in the embryogenic development of the lung. It contributes to surfactant production, the development of the respiratory unit and alveoli, and normal lung functions11,12. TTF-1 has both oncogene and tumor suppressor properties13. TTF is positive in 50–60% of AC cases and it is frequently used in the diagnosis and differential diagnosis of AC5. It is not only a diagnostic but also a prognostic and predictive marker6. However, its role in patients with BM remains unknown; therefore, in the current study, for the first time in the literature, we evaluated the survival times of patients with AC with BM and their relationship with TTF-1.
In our study, the survival time of the patients was 6.4 months, consistent with previous studies. Similar to the literature, we found that patients with poor ECOG performance had a shorter survival time. We also determined that the survival time of TTF-1 (+) patients was longer, and this was statistically significant in the multivariance analysis independent of the number of BM, ECOG performance score, and age. This study is important since there is no previous research examining this relationship.
Studies examining the relationship between AC and TTF-1 have reported that TTF-1 (+) patients have a better response to chemotherapy and have longer life expectancy in both early and advanced stages14,15,16,17,18,19,20,21,22,23. These results have also been supported by meta-analyses24,25,26. TTF-1-positive lung cancers have a better prognosis. It is unknown why TTF-1-positive patients have a better prognosis. However, Myong et al. showed that TTF-1 expression was inversely proportional to the Ki-67 proliferation index27. The inverse correlation of Ki-67 with TTF expression may be one reason for the difference between TTF-1 positive and TTF-1 negatives. Although all of the patients in our study were negative for EGFR mutation, it has been reported in the literature that higher rate of EGFR mutations were detected in TTF-1 positive patients than in TTF-1 negative patients28,29. Patients with EGFR mutations have a longer life expectancy with the use of tyrosine kinase inhibitor drugs29,30,31,32. This may be another reason for the difference between TTF-1 positives and TTF-1 negatives. On the other hand, the respiratory tract is divided into the terminal respiratory unit (TRU), which plays a role in oxygen-carbon dioxide exchange, and the non-TRU, which plays a role in conducting air intake. TRU contains TTF-1-expressing cells, while non-TRU contains non-TTF-1-expressing cells15,33. TTF-1-positive and TTF-1-negative tumors may develop from different parts of the respiratory tract and may show different clinical courses. Another reason for the difference between TTF-1 positive and TTF-1 negative tumors may be that TTF-1 positive and negative tumors developed from different regions of the respiratory tract.
In our study, TTF-1 was evaluated from the first lung biopsies at the time of diagnosis. TTF-1 may differ between primary tumors and metastasis. But Brain metastasis is not biopsied in lung cancers because radiological findings are often sufficient in the diagnosis of brain metastases and the clinical conditions of the patients are not suitable for cranial biopsy in daily practice. This is one of the weaknesses of this study. In addition, grading data could not be obtained In this study. Because all of our cases had advanced diseases. For this reason, they were diagnosed with biopsies instead of surgical applications. Materials taken for diagnostic biopsies are usually small, so grading and differentiation are not always appropriate. Since our study was retrospective, a new biopsy could not be taken again. This is another weak point of the study.
Examination of TTF-1 only in lung biopsies in the study, and the retrospective, single-centered study with a small number of patients are the limitations of our study. However, our study is important because it is the first study to show the relationship between TTF-1 and BM.
In conclusion, TTF-1 presents as an easily obtained, inexpensive, and useful biomarker to determine prognosis in patients with AC that develop BM, when used together with the ECOG performance score.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Tabouret, E. et al. Recent trends in epidemiology of brain metastases: An overview. Anticancer Res. 32, 4655–4662 (2012).
Nayak, L., Lee, E. Q. & Wen, P. Y. Epidemiology of brain metastases. Curr. Oncol. Rep. 14, 48–54 (2012).
Fox, B. D., Cheung, V. J., Patel, A. J., Suki, D. & Rao, G. Epidemiology of metastatic brain tumors. Neurosurg. Clin. N. Am. 22, 1–6 (2011).
Chason, J. L., Walker, F. B. & Landers, J. W. Metastatic carcinoma in the central nervous system and dorsal root ganglia: A prospective autopsy study. Cancer 16, 781–787 (1963).
Yatabe, Y., Mitsudomi, T. & Takahashi, T. TTF-1 expression in pulmonary adenocarcinomas. Am. J. Surg. Pathol. 26, 767–773 (2002).
Wang, X. et al. Prognostic and predictive value of thyroid transcription factor-1, cd56, p40 and other clinical characteristics in small cell lung cancer patients. Zhongguo Fei Ai Za Zhi 20, 522–527 (2017).
Gaspar, L. et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int. J. Radiat. Oncol. Biol. Phys. 37, 745–751 (1997).
Sperduto, P. W., Berkey, B., Gaspar, L. E., Mehta, M. & Curran, W. A new prognostic index and comparison to three other indices for patients with brain metastases: An analysis of 1960 patients in the RTOG database. Int. J. Radiat. Oncol. Biol. Phys. 70, 510–514 (2008).
Lagerwaard, F. J. et al. Identification of prognostic factors in patients with brain metastases: A review of 1292 patients. Int. J. Radiat. Oncol. Biol. Phys. 43, 795–803 (1999).
Weltman, E. et al. Radiosurgery for brain metastases: A score index for predicting prognosis. Int. J. Radiat. Oncol. Biol. Phys. 46, 1155–1161 (2000).
Stahlman, M. T., Gray, M. E. & Whitsett, J. A. Expression of thyroid transcription factor-1(TTF-1) in fetal and neonatal human lung. J. Histochem. Cytochem. 44, 673–678 (1996).
Lazzaro, D., Price, M., de Felice, M. & Di Lauro, R. The transcription factor TTF-1 is expressed at the onset of thyroid and lung morphogenesis and in restricted regions of the foetal brain. Development 113, 1093–1104 (1991).
Mu, D. The complexity of thyroid transcription factor 1 with both pro- and anti-oncogenic activities. J. Biol. Chem. 288, 24992–25000 (2013).
Saad, R. S., Liu, Y. L., Han, H., Landreneau, R. J. & Silverman, J. F. Prognostic significance of thyroid transcription factor-1 expression in both early-stage conventional adenocarcinoma and bronchioloalveolar carcinoma of the lung. Hum. Pathol. 35, 3–7 (2004).
Puglisi, F. et al. Prognostic value of thyroid transcription factor-1 in primary, resected, non-small cell lung carcinoma. Mod. Pathol. 12, 318–324 (1999).
Ma, Y. et al. The expression of TTF-1 and Napsin A in early-stage lung adenocarcinoma correlates with the results of surgical treatment. Tumor Biol. 36, 8085–8092 (2015).
Anagnostou, V. K., Syrigos, K. N., Bepler, G., Homer, R. J. & Rimm, D. L. Thyroid transcription factor 1 is an independent prognostic factor for patients with stage I lung adenocarcinoma. J. Clin. Oncol. 27, 271–278 (2009).
Zhou, C., Zhao, J., Shao, J. & Li, W. Prognostic relevance of TTF-1 expression in stage I adenocarcinoma. Oncotarget 8, 107462–107468 (2017).
Barlési, F. et al. Positive thyroid transcription factor 1 staining strongly correlates with survival of patients with adenocarcinoma of the lung. Br. J. Cancer. 93, 450–452 (2005).
Martins, S. J. et al. Prognostic relevance of TTF-1 and MMP-9 expression in advanced lung adenocarcinoma. Lung Cancer 64, 105–109 (2009).
Grønberg, B. H., Lund-Iversen, M., Strøm, E. H., Brustugun, O. T. & Scott, H. Associations between TS, TTF-1, FR-α, FPGS, and overall survival in patients with advanced non-small-cell lung cancer receiving pemetrexed plus carboplatin or gemcitabine plus carboplatin as first-line chemotherapy. J. Thorac. Oncol. 8, 1255–1264 (2013).
Sun, J.-M., Han, J., Ahn, J. S., Park, K. & Ahn, M.-J. Significance of thymidylate synthase and thyroid transcription factor 1 expression in patients with nonsquamous non-small cell lung cancer treated with pemetrexed-based chemotherapy. J. Thorac. Oncol. 6, 1392–1399 (2011).
Doherty, M. K. et al. Absence of thyroid transcription factor-1 expression is associated with poor survival in patients with advanced pulmonary adenocarcinoma treated with pemetrexed-based chemotherapy. Ir. J. Med. Sci. 188, 69–74 (2019).
Qian, H.-H., Xu, T.-S., Cai, X.-Q., Ji, T.-L. & Guo, H.-X. Prognostic value of TTF-1 expression in patients with non-small cell lung cancer: A meta-analysis. Clin. Chim. Acta. 451, 208–214 (2015).
Kim, J. H. et al. Prognostic impact of TTF-1 expression in non-squamous non-small-cell lung cancer: A meta-analysis. J. Cancer 9, 4279–4286 (2018).
Berghmans, T. et al. Thyroid transcription factor 1—a new prognostic factor in lung cancer: A meta-analysis. Ann. Oncol. 17, 1673–1676 (2006).
Myong, N. H. Thyroid transcription factor-1 (TTF-1) expression in human lung carcinomas: Its prognostic implication and relationship with expressions of p53 and Ki-67 proteins. J. Korean Med. Sci. 18, 494–500 (2003).
Park, J. H. et al. EGFR mutations as a predictive marker of cytotoxic chemotherapy. Lung Cancer 77, 433–437 (2012).
Park, J. Y. et al. Thyroid transcription factor-1 as a prognostic indicator for stage IV lung adenocarcinoma with and without EGFR-sensitizing mutations. BMC Cancer 19, 574 (2019).
Zhang, Y. et al. Negative thyroid transcription factor 1 expression defines an unfavorable subgroup of lung adenocarcinomas. J. Thorac. Oncol. 10, 1444–1450 (2015).
Chung, K.-P. et al. Clinical significance of thyroid transcription factor-1 in advanced lung adenocarcinoma under epidermal growth factor receptor tyrosine kinase inhibitor treatment. Chest. 141, 420–428 (2012).
Zhang, R., Li, Y., Nie, X., Dong, X. & Wu, G. Prognostic implications of immunohistochemistry markers for EGFR-TKI therapy in Chinese patients with advanced lung adenocarcinoma harboring EGFR mutations. Onco. Targets Ther. 9, 355–366 (2016).
Travis, W. D. et al. International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 6, 244–285 (2011).
Funding
The authors declare that they did not receive any funding for this study.
Author information
Authors and Affiliations
Contributions
Concept—S.M. Design—S.M. Supervision—S.M., E.K. Resources—S.M., E.K. Materials—E.K., S.M. Data Collection and/or Processing—S.M., E.K. Analysis and/or Interpretation—E.K. Literature Search—E.K., S.M. Writing Manuscript—E.K.; Critical Review—S.M., E.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kut, E., Menekşe, S. Relationship between brain metastasis and thyroid transcription factor 1. Sci Rep 13, 1945 (2023). https://doi.org/10.1038/s41598-023-29236-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-023-29236-1