Abstract
Tryptophol (TOH), a fungal quorum-sensing molecule, that possesses anti-fungal activities for controlling the growth of human pathogenic fungi. In the present study, we developed TOH-containing emulgel formulations and examined the antifungal activities and potential use as topical treatments on the skin. The results showed that TOH-containing emulgel at 1000 μM has excellent physical characteristics as homogenous, stability, and inhibits the growth of 30 species of human pathogenic fungi in vitro. TOH-containing emulgel did not cause skin irritation in mouse model of irritation and in healthy human volunteers. Moreover, an increase in skin hydration and a decrease in trans-epidermal water loss (TEWL) were observed after TOH-containing emulgel treatment on human skin. Our findings indicated that TOH-containing emulgel can be utilize as an antifungal agent for topical treatment against fungal infections on the skin.
Similar content being viewed by others
Introduction
Fungi can communicate to their extracellular environments by producing and releasing their small diffusible chemical signaling molecules known as fungal quorum-sensing molecules (QSM)1. Fungal QSMs have been shown to have a variety of biological activities such as cell-to-cell communication, morphogenesis, biofilm formation, and virulence, which ultimately controls the growth of another fungi2. To date, they are 4 main groups of QSMs including farnesol (FOH), tyrosol (TYR), phenylethanol (PE), and tryptophol (TOH)3.
Tryptophol (C10H11NO, TOH; molecular weight, 161.20) is a QSM that can be isolated from yeasts such as Candida albicans and Saccharomyces cerevisiae4. Our previous studies have demonstrated that TOH can inhibit the growth of Candida albicans5 and Scedosporium apiospermum4. Thus, TOH has a high potential to be developed as an innovative product containing active antifungal agent for the treatment of fungal infections.
To develop a product containing TOH, vehicles that are used to incorporate TOH for dermal delivery are greatly concerns6. Repeated topical application of TOH may adversely cause skin irritation and contact dermatitis7. Emulsion-based formulations are currently the chosen formulation for topical delivery of active agents, which show good interaction on the skin8.
The aim of the study was to investigate the antifungal effects TOH-containing emulgel in vitro and skin irritation in vivo as well as on healthy human volunteers. Moreover, the cosmeceutical benefits of TOH-containing emulgel was also investigated.
Results
Formulation and evaluation of TOH-containing emulgel
With the aim to develop the TOH-containing emulgel from emulgel base recipe, the emulgel prototype products containing 100 μM and 1000 μM of TOH were successfully developed. The physical and chemical properties of TOH-containing emulgel were evaluated previously9. Moreover, an emulgel containing 1000 μM of voriconazole (VOZ) was also produced. The parameters of emulgel base, TOH- and VOZ-containing emulgel were presented in Table 1. The manufactured 100 μM and 1000 μM of TOH- and 1000 μM of VOZ- containing emulgel appeared as white, translucent, homogenous, and non-greasy. However, high concentrations of active compounds (TOH and VOZ) caused an increase in viscosity and reduced the spread ability of the products (Table 1). There was no phase separation found both all manufactured emulgel formulations. There were no color changes or physical instability involving phase separation or inconsistency increases. Nevertheless, the pH of the manufactured emulgel formulations were found to be in the acceptable range of 4.5-5.5.
Antifungal susceptibility of TOH-containing emulgel
In-Vitro antifungal activities of manufactured TOH-containing emulgel formulations were evaluated in 30 strains of fungal pathogens using the agar spot assay. Firstly, the colonies diameters of azole-resistant/or azole-sensitive strains including Scedosporium apiospermum (CBS 117410), S. boydii (CBS 120157), Lomentospora prolificans (CM324)9, Aspergillus fumigatus (CL-262)10, A. fumigatus (AF293), Candida albicans (ATCC 96901), and C. albicans (ATCC 90028) were determined after 14 days of incubation with emulgel base, 100 μM and 1000 μM of TOH- and 1000 μM of VOZ-containing emulgel (Table 2). Moreover, the results showed that 1000 μM of TOH-containing emulgel remarkedly lessened the growth rate of these azole-resistant strains than 100 μM of TOH- and 1000 μM of VOZ-containing emulgel. The colonies diameters of common fungal skin pathogens were further investigated. In the group of hyaline molds, 1000 μM of TOH-containing emulgel remarkedly lessened the growth rate of Trichophyton mentagrophytes (ATCC MYA-4439), T. rubrum (ATCC MYA-4438), T. verrucosum (ATCC 42898), T. tonsurans11, Microsporum canis11, M. gypseum12, and Epidermophyton floccosum (ATCC 52066) than 100 μM of TOH- and 1000 μM of VOZ-containing emulgel. In the group of dematiaceous molds, 1000 μM of TOH-containing emulgel remarkedly lessened the growth rate of A. recifei (ATCC 36328), Fonsecaea pedrosoi, E. dermatitidis (ATCC 76204), and Bipolaris maydis than 100 μM of TOH- and 1000 μM of VOZ-containing emulgel. Moreover, 1000 μM of TOH-containing emulgel remarkedly lessened the growth rate of dimorphic fungi (Sporothrix schenckii (ATCC 58251) and Talaromyces marneffei13) than 100 μM of TOH- and 1000 μM of VOZ-containing emulgel. In pathogenic yeasts, 1000 μM of TOH-containing emulgel remarkedly lessened the growth rate of Malassezia furfur (ATCC 12078), T. asahii (ATCC 90039), C. tropicalis, C. dubliniensis (ATCC MYA-646), Cryptococcus neoformans (ATCC 32045), C. gattii (ATCC 56992), Lodderomyces elongisporus (ATCC 11503), Mucor spp.13, Rhizopus spp., and Beauveria bassiana (ATCC 74040) than 100 μM of TOH- and 1000 μM of VOZ-containing emulgel. Thus, the effective concentration of TOH-containing emulgel at 1000 μM was chosen due to its board antifungal activities.
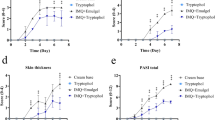
In vitro human foreskin fibroblast cell viability, and cytotoxicity
To further determine the potential use as topical TOH-containing emulgel, human foreskin fibroblasts (HFF-1) cell viability and cytotoxicity were investigated after incubating for 24 h with 100 μM and 1000 μM of TOH and 1000 μM of VOZ using MTT (3-(4,5- dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide), MitoGreen, lactate dehydrogenase (LDH), and dual Acridine Orange/Ethidium Bromide AO/EB staining assays. The results showed that HFF-1 cell viability did not show a significant change after treating with 100 and 1000 μM of TOH as determined by MTT and MitoGreen assays (Fig. 1a). However, HFF-1 cell viability (75 ± 7.50% and 70 ± 8.50%, respectively) was significantly decreased at 1000 μM of VOZ when compared to controls. Moreover, incubation of 100 and 1000 μM of TOH did not induce HFF-1 cell cytotoxicity as determined by LDH and dual AO/EB staining assays, whereas, 1000 μM of VOZ significantly increased HFF-1 cell cytotoxicity (20 ± 2.50% and 30 ± 4.50%, respectively) when compared to controls (Fig 1b). Thus, the results suggested that TOH at 1000 μM exhibits antifungal activates against common skin pathogenic fungi without compromising the health of human skin in vitro.
Cell viability (a) and cytotoxicity (b) of TOH-treated human foreskin fibroblasts (HFF- 1) cells at 37 °C as determined by MTT, Mitogreen, LDH, and dual AO/EB staining assays. Percentages of cell viability and cytotoxicity were shown as mean ± SD. *P < 0.05 and ****P < 0.0001 indicate significant differences compared with the control group (concentration 0). TOH Tryptophol, VOZ voriconazole.
Evaluation of TOH-containing emulgel on mouse skin irritation
Single irritation test on mouse skin was used examined an acute irritant contact dermatitis (AICD) of 1000 μM TOH-containing emulgel. After 24 h post-topical application, croton oil and 5% Sodium Lauryl Sulfate (SLS) were able to induce mild to moderate edema with loss of skin creases, whereas, emulgel cream base, commercial shielding cream, 1000 μM VOZ-containing emulgel and 1000 μM TOH-containing emulgel did not induce any skin changes as determined by visual assessment. The notable histological features of acute irritant contact dermatitis were spongiosis, accumulation of fluid in the epidermis, and inflammatory cells infiltrations in epidermis, dermis, and subcutaneous tissues in the group treated with croton oil (Fig. 2d) and lessened in the group treated with 5% SLS (Fig. 2e). No histological characteristics of AICD were found in the group treated with emulgel cream base (Fig. 2a), commercial shielding cream (Fig. 2b), 1000 μM VOZ-containing emulgel (Fig. 2c), and 1000 μM TOH-containing emulgel (Fig. 2f).
Representative H&E photographs of mouse skin after 24 h post-topical application with 1000 μM TOH-containing emulgel. (a) Emulgel cream base, (b) Commercial shielding cream, (c) 1000 μM VOZ emulgel, (d) croton oil, (e) 5% SLS, and (f) 1000 μM TOH emulgel. Arrows indicated the spongiosis at epidermis. Dash boxes magnified each specific Black and White arrowheads indicated inflammatory cells infiltration at the epidermis and dermis, respectively. Scale bar = 200 μm and = 50 μm.
Cumulative irritation test on mouse skin was used examined a chronic irritant contact dermatitis (CICD) of 1000 μM TOH-containing emulgel. Severe epidermal hyperplasia, spongiosis, inflammatory cells infiltrations, and dilatation of dermal vessels were found in the group treated with croton oil after 7 days (Fig. 3d) and 14 days of application (Fig. 4d) and lessened in the group treated with 5% SLS after 7 days (Fig. 3e) and 14 days of application (Fig. 4e). No histological characteristics of CICD were found in the group treated with emulgel cream base (Figs. 3a and 4a), commercial shielding cream (Figs. 3b and 4b), 1000 μM VOZ-containing emulgel (Figs. 3c and 4c), and 1000 μM TOH-containing emulgel (Figs. 3f and 4f) after 7 days and 14 days of application, respectively. Therefore, the present study suggested that 1000 μM TOH-containing emulgel did not induce neither acute or chronic irritation in vivo.
Representative H&E photographs of mouse skin after 7 days of topical application with 1000 μM TOH-containing emulgel. (a) Emulgel cream base, (b) Commercial shielding cream, (c) 1000 μM VOZ emulgel, (d) croton oil, (e) 5% SLS, and (f) 1000 μM TOH emulgel. Arrows indicated the spongiosis at epidermis. Dash boxes magnified each specific Black arrowheads indicated inflammatory cells infiltration at the epidermis. Scale bar = 200 μm and = 50 μm.
Representative H&E photographs of mouse skin after 14 days of topical application with 1000 μM TOH-containing emulgel. (a) Emulgel cream base, (b) Commercial shielding cream, (c) 1000 μM VOZ emulgel, (d) croton oil, (e) 5% SLS, and (f) 1000 μM TOH emulgel. Arrows indicated the spongiosis at epidermis. Dash boxes magnified each specific Black arrowheads indicated inflammatory cells infiltration at the epidermis. Scale bar = 200 μm and = 50 μm.
Evaluation of TOH-containing emulgel on human skin irritation
Skin irritation test was determined in thirty healthy volunteers after topical treatment of 1000 μM TOH-containing emulgel. After 24 h post-topical application, no visual characteristics of skin irritation or dermatitis observed in the group treated with commercial shielding cream (Fig. 5a), 1000 μM TOH-containing emulgel (Fig. 5b), 1000 μM VOZ-containing emulgel (Fig. 5c), and emulgel cream base (Fig. 5d). Moreover, no skin irritation was observed after 72 h post-topical application in all treatments (Fig. 5). Therefore, the present study suggested that 1000 μM TOH-containing emulgel treatment did not cause skin irritation in human volunteers.
Evaluation of TOH-containing emulgel on human skin physiological properties
Hydration values measured on the skin of volunteers treated with 1000 μM TOH-containing emulgel are significantly higher than emulgel base and distilled water treated areas (Fig. 6a). Skin hydration was significantly increased after treated with 1000 μM TOH-containing emulgel (Fig. 6b). Moreover, treatment of 1000 μM TOH-containing emulgel significantly reduced transepidermal water loss (TEWL) than other products (Fig. 6c). Therefore, the present study suggested that 1000 μM TOH-containing emulgel treatment enhances other cosmeceutical benefits to the human skin.
Noninvasive assessments for (a) skin hydration, (b) percentage of hydration changes, and C TEWL readings at 14 days post-application of 1000 μM TOH-containing emulgel (n = 30). Data were shown as mean ± SD. **P < 0.01 and ****P < 0.0001 indicate significant differences compared with the control group (concentration 0). TOH Tryptophol.
Discussion
Superficial mycosis is caused by pathogenic fungi that affects superficial layer of the skin14. Several species of human pathogenic fungi can infect deeper than the superficial layer of the skin causing cutaneous mycosis15. These skin mycoses are common worldwide, which in some cases, causing cosmetically poor appearance with severe inflammation16. Antifungal drug such as voriconazole (VOZ), a triazole compound, is the drug-of-choice antifungal agent against fungal infections17. However, fungal infections that resistant to triazoles such as VOZ has become a concern with increases cases over the past decade18. Thus, the present study was conducted and developed to evaluate the effectiveness of alternative topical treatment to treat various pathogenic fungi as a tryptophol (TOH)-containing emulgel.
In general, TOH can be naturally found as a quorum sensing molecule (QSM) in seed plants, bacteria, and fungi19. TOH affects fungi morphogenesis, which provides a potential use as an antifungal agent various fungal pathogen species20. We have previously demonstrated that in vitro treatment of TOH suppresses the pathogenicity of C. albicans. In addition, treatment of TOH was found to induce C. albicans apoptosis via the transcriptional upregulation of caspase recruitment domain-containing protein (CARD)-9 and Noxa and the downregulation of Bcl-25. We also previously demonstrated that treatment of TOH at 100 μM reduces the germ tube length and biofilm formation of S. apiospermum in vitro. Moreover, TOH-containing emulgel was developed at 100 μM, which reduced S. apiospermum-induced eumycetoma formation in vivo9. Also the antifungal activity of TOH both in vitro and in vivo have been extensively studied, whether antifungal activity and safety of TOH-containing emulgel for clinical use remains to be elucidated.
In the present study, we demonstrated that TOH at 100 μM and 1000 μM was successfully incorporated into emulgel base containing SEPIGEL 3059. Moreover, TOH-containing emulgel in the present study exhibited excellent in cosmeceutical levels including homogeneity, consistency, and stability with pH range of 5.5, which compromised with the pH of the skin21. Interestingly, we further demonstrated that 1000 μM TOH-containing emulgel exhibited excellent in antifungal activity against 30 pathogenic fungi including azole-resistant strains, hyaline and dematiaceous molds, dimorphic fungi, and yeasts than 1000 μM VOZ-containing emulgel in vitro. Thus, our study suggested that the manufactured TOH-containing emulgel at 1000 μM was optimal for topical use in vivo with antifungal activity against wide ranges of human cutaneous pathogenic fungi.
In this report, we demonstrated that TOH caused less cytotoxic to human foreskin fibroblast (HFF-1) cells than VOZ in vitro suggesting that TOH is safe to use as topical treatment in vivo. We further determined the safety use of TOH-containing emulgel in human volunteers by determining both acute irritant contact dermatitis (AICD) and chronic irritant contact dermatitis (CICD) caused by 1000 μM TOH-containing emulgel prior to commercialize the product. From the present study, our results suggested that either single or repeated exposure of 1000 μM TOH-containing emulgel does not cause skin irritation or any histological changes, which suitable for long term use22.
No skin irritation was observed in human volunteers after 1000 μM TOH-containing emulgel treatments. Moreover, skin hydration and less water loss were gained after 1000 μM TOH-containing emulgel treatments. Therefore, our present study showed that 1000 μM TOH-containing emulgel is suitable to be used as an alternative antifungal product for topical treatment. Hence, it is possible to infer that the 1000 μM TOH-containing emulgel was safe for topical application on human skin without skin adverse effects. Nevertheless, the antifungal activity of 1000 μM TOH-containing emulgel need to be evaluated further in patients with cutaneous fungal infections, which we plan to investigate in the near future.
Conclusions
The study confirmed positive effects of 1000 μM TOH-containing emulgel that exhibits antifungal activities and cosmeceutical benefits without causing skin irritation to human. The potential use of 1000 μM TOH-containing emulgel in patients with skin mycoses may be investigated in the future. Further, this study showed an innovative approach to utilize TOH-containing emulgel as a topical application for treating fungal infections as being in accordance with the growing use of emulgels in cosmeceutical and pharmacological products.
Methods
Materials
Tryptophol (TOH; C10H11NO,), voriconazole (VOZ,), absolute ethanol (EtOH), Tween™ 20, glycerin, propylene glycol, allantoin, phenoxyethanol, Acridine Orange/Ethidium Bromide (AO/EB), Sodium Lauryl Sulfate (SLS), and croton oil were purchased from Sigma-Aldrich (St. Louis, MO, USA). SEPIGEL 305™ was purchased from Seppic Inc. (Fairfield, NJ, USA). Triethanolamine was purchased from Dow Chemical (Thailand). Deionized (DI) water used in all experiments was produced from in-house Milli-Q® IQ 7000 Ultrapure Water System (EMD Millipore, Bedford, MA, USA). Sabouraud Dextrose Agar (SDA) and Potato Dextrose Agar (PDA) were purchased from Oxoid Ltd. (Hampshire, UK). Roswell Park Memorial Institute 1640 medium (RPMI-1640), Fetal Bovine Serum (FBS), Penicillin-streptomycin (Pen-strep), Phosphate-Buffered Saline (PBS), and Trypsin-EDTA were purchased from Gibco™ (Grand Island, NY, USA). MTT (3-(4,5- dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) was purchased from Bio Basic Inc. (Canada). CytoPainter MitoGreen (#ab176830) was purchased from Abcam. CytoTox 96® Non-Radioactive Cytotoxicity assay for measuring the release of lactate dehydrogenase (LDH) was purchased from Promega (Madison, WI, USA). All the reagents used in this study were of high purity or HPLC grade.
Preparation of TOH-containing emulgel formulation
The emulgel formulations were prepared with either tryptophol or voriconazole according to Kitisin et al.9. Optimization of all the emulgel formulations were performed by evaluating the effect of different concentrations of excipients based on visual changes in appearance, homogeneity, consistency, viscosity, stability, and any change in the physical characteristics prior to manufacturing the final formulations. The compositions of all the optimized emulgel formulae are provided in Table 3.
Manufacturing process for emulgel
The emulgel base was manufactured with a constant mechanical stirring of the gel-based SEPIGEL 305™. TOH at 100 µM and 1000 µM or VOZ at 1000 µM were accurately prepared and added to the emulgel base and vigorously mixed until a smooth emulgel was formed9.
Visual evaluation
The visual appearance of manufactured emulgel formulations were examined for their physical appearances including color, homogeneity, consistency, and phase separation23.
Measurement of viscosity and pH
The viscosity of manufactured emulgel formulations was evaluated at room temperature using a Brookfield viscometer (Brookfield, Model programmable DV2, USA) with a volume sample of 0.5 g9. The formulated emulgel samples were left for equilibrium (30 min) at 25 °C. Measurements with the spindle were determined at 100 rpm for 10 min. The viscosity reading of each sample was recorded. Moreover, the pH of all manufactured emulgel formulations was measured by a digital pH meter (Thermo Fisher Scientific, Waltham, MA, USA)23. Prior measurement, pH meter was calibrated using standard pH buffers at 4, 7, and 10. Then, the pH for all the emulgel formulations was recorded. The pH meter probe was washed after each measurement with DI water and 70% (v/v) EtOH. Data were analyzed in tripiclate.
Measurement of spreadability
The spreadability of manufactured emulgel formulations was investigated to determine the competence of each emulgel formulation, which is able to spread evenly after smeared on the affected skin24. To measure the spreadability of emulgel samples, 1 g of each formulated emulgel was placed onto the ground fixed glass plate and covered with another glass plate and placed on a wooden block. A definite load of about 20 g was then placed on the top of the slides for 1 min to provid the basis for the slip and drag characteristics of the emulgel. The time in seconds required to separate the two slides was recorded and analyzed in triplicate. The spreadability was calculated using the following equation: S = m * l/t; where S stands for spreadability, m stands for weight tied on upper slide; l is the length of glass slides; t, the time (s) requires to separate the slides completely25.
Measurement of stability
Physical stability studies were investigated for all the formulations using using centrifugation and temperature cycle tests9. For centrifugation test, approximately 10 g of sample was centrifuged at 9000 rpm for 30 min. In addition, 2 g of each prepared emulgel samples was subject to a temperature cycle test by storing in 24 h/a cycle at − 4 °C (8 h) and 40 °C (16 h) for 10 cycles. After cooling-heating and freeze-thaw, the emulgel samples were evaluated for stability changes. All measurements were performed in triplicate. Physical stability of these emulgels formulations was evaluated at the end of these tests.
Fungal strain and growth condition
Scedosporium apiospermum (CBS 117410), S. boydii (CBS 120157), and Lomentospora prolificans (CM324) used in this study were kindly provided by Dr. Ana Alastruey-Izquierdo (Servicio de Micologίa, Instituto de Salud. Carlos III, Madrid, Spain)9. Aspergillus fumigatus (CL-262; an azole resistant clinical strain carrying the M220I mutation in Cyp51A gene) was kindly provided by Asst. Prof. Dr. Marut Tangwattanachuleeporn (Faculty of Allied Health Sciences, Burapha University, Chonburi, Thailand)10. Bipolaris maydis was kindly provided by Dr. Songbai Zhang, (College of Agriculture, Yangtze University, Hubei, China)26. Microsporum canis11, M. gypseum12, Trichophyton tonsurans11, Talaromyces marneffei13, Mucor spp.13, Candida tropicalis (unpublished data), Fonsecaea pedrosoi (unpublished data), and Rhizopus spp. (unpublished data) used in this study were clinical or environmental isolates that previously collected and identified from our laboratory.
A. fumigatus (AF293; ATCC MYA-4609, CBS 101355; an azole sensitive strain), Candida albicans (ATCC 90028; an azole sensitive strain), C. albicans (ATCC 96901; an azole resistant strain), C. dubliniensis (ATCC MYA-646, CBS 7987), T. mentagrophytes (ATCC MYA-4439), T. rubrum (ATCC MYA-4438), T. verrucosum (ATCC 42898), Epidermophyton floccosum (ATCC 52066), Acremonium recifei (ATCC 36328), Exophiala dermatitidis (ATCC 76204), Sporothrix schenckii (ATCC 58251), Malassezia furfur (ATCC 12078), T. asahii (ATCC 90039), Cryptococcus neoformans (ATCC 32045), C. gattii (ATCC 56992), Lodderomyces elongisporus (ATCC 11503), and Beauveria bassiana (ATCC 74040) were provided by the American Type Culture Collection (ATCC) (Manassas, VA, USA). Fungal strains were cultured in SDA for yeasts at 37 ± 1 °C and PDA for molds at 25 ± 1 °C.
In-vitro antifungal activity studies
In-vitro antifungal activity studies of manufactured emulgel formulations were evaluated using the agar spot assay according to Horváth et al.27 for yeasts and according to Muangkaew et al.28 for filamentous fungi with some modifications. Briftly, ten µl of each fungal conidia at concentration about about 5 × 106 conidia/ml were mixed with 10 µl of each manufactured emulgel formulations (TOH at 100 or 1000μM or VOZ at 1000 μM) and spotted on the surface of SDA plates. Then, the plates were incubated at 37 ± 1 °C for 14 days. The colony diameter (mm) were measured in millimeters using a vernier caliper4,9. Uninoculated SDA plate was used as a negative control. The experiment was performed in triplicate.
Cell culture, viability, and cytotoxicity
Human foreskin fibroblasts (HFF-1) cell line (ATCC #SCRC-1041™) was used to investigate cell viability and cytotoxicity after TOH treatments. HFF-1 cells were cultured in RPMI-1640 supplemented with 10% FBS and 100 U/ml of Pen-strep and incubated under humidified conditions with 5% CO2 at 37 °C. Measurements of cell viability and cytoxicity after TOH treatments were carried using MTT9, CytoPainter MitoGreen, LDH9, and dual AO/EB staining assays. As previously described, HFF-1 were seeded at a concentration of 1 × 105 cells/ml in a 96 well plate and after 24 h were treated with 100 μl of TOH at 100 or 1000μM or VOZ at 1000 μM or with absolute EtOH and RPMI 1640 at 1% (v/v) as diluent controls. Untreated HFF-1 cells were used as negative controls (100% viable). After incubation for 24 h, 10 μl of 0.5 μg/μl MTT solution or 50 μl of CytoTox 96® reagent were added and measured spectrophotometrically at 540 nm or 490 nm, respectively (Sunrise Tecan, Grödig, Austria). To label cell viability and toxicity, treated HFF-1 cells were stained with 100 μl of MitoGreen indicator or 25 μl of 100 μg/μl AO/EB solution, respectively. Cellular morphology and apoptotic cell numbers were examined by a Zeiss Axio Imager fluorescence microscope (ZEISS, Germany). All of the experiments were performed in triplicate.
In vivo evaluation of the emulgel formulations on mouse skin irritation
Female BALB/c mice were purchased from Nomura Siam International Co, Ltd. (Thailand) and used to evaluate skin irritation of manufactured emulgel formulations. Each group included 5 animals (aged 6-8-week-old, body weight: 20–25 g) The skin irritation mouse model was produced and validated as described previously with some modification22. Briefly, all mice were topically treated with various concentrations of manufactured emulgel formulations (including emulgel base, 1000 µM of TOH or VOZ containing emulgels) that do not cause necrosis of the epidermis. Five percentage of SLS and croton oil were used as irritants. Commercial shielding cream was applied as controls. For single irritation, 15 μl of the irritants were put on the 8 mm Finn Chambers on Scanpor tape (Epitest Ltd., Finland), which were then applied on the dorsal skin of the animals. Polyurethane film (3M™ Tegaderm™, NY, USA) was used to fix them and Finn Chambers were then removed after 24 h post-application. For cumulative irritation, the procedure was repeated once a day for 1 and 2 weeks. After removing the Finn Chambers, mice were sacrificed, and skin samples were collected. The specimens were fixed in 10% buffered formalin and processed for haematoxylin and eosin (H&E) stain. All skin sections were examined with a light microscope (BH-2, Olympus, Japan). All animal experiments were conducted in accordance with the Animals for Scientific Purposes Act, B.E. 2558 (A.D. 2015), Thailand. Experiments on mice were approved by Institutional Animal Care and Use Committee (IACUC) of the University of Phayao, Thailand (approval number: UP-AE64-01-04-017).
In vivo evaluation of the emulgel formulations on human skin irritation
To evaluate the sensitization potential of manufactured emulgel formulations toward human skin, a skin irritation test was performed by 30 healthy volunteers29. A single irritation test of the manufactured emulgel formulations (emulgel base, 1000 µM of TOH or VOZ containing emulgels) were put on the 8 mm Finn Chambers on the back of arm skin of the volunteers and fixed with polyurethane film. Commercial shielding cream was applied as controls. Finn Chambers were then removed after 24 h post-application. Treated areas of volunteer skin were observed immediately and 72 h after removing Finn Chambers. All in vivo studies with healthy volunteers are complied with the 2013 Declaration of Helsinki and was approved Ethics Committee (EC) at the Faculty of Tropical Medicine, Mahidol University, Thailand (approval number: MUTM 2022-036-01). Written informed consent was obtained from all the participants.
In vivo evaluation of the emulgel formulations on human skin hydration, trans-epidermal water loss (TEWL), and skin color
To evaluate the effects of manufactured emulgel formulations on human skin physiological functions including skin hydration and trans-epidermal water loss (TEWL), treated skins of 30 healthy volunteers with manufactured emulgel formulations were investigated using DermaLab® with a hydration probe and a TEWL probe (Cortex Technology, Hadsund, Denmark)30. After manufactured emulgel treatments, measurements of the skin hydration and TEWL were performed in 2 × 2 cm squares on the middle forearms, next to each other, with an interval of 5 s between each measurement. Three measurements were taken in each square.
Statistical analysis
All the data was statistically analyzed using GraphPad Prism, version 6.05, (GraphPad Software, San Diego, CA, USA). All experiments were performed in triplicate. Data were expressed by mean ± SD. A P-value of < 0.05 was considered as statistically significant using an independent t-test or analyses of variance (ANOVA) followed by Tukey’s multiple comparison test.
Institutional review board statement
All animal experiments were conducted in accordance with the Animals for Scientific Purposes Act, B.E. 2558 (A.D. 2015), Thailand. Experiments on mice were approved by Institutional Animal Care and Use Committee (IACUC) of the University of Phayao, Thailand (approval number: UP-AE64-01-04-017). Human studies were approved by Ethics Committee (EC) at the Faculty of Tropical Medicine, Mahidol University, Thailand (approval number: MUTM 2022-036-01).
Informed consent
Informed consent was obtained from all human subjects involved in the study.
Data availability
The data collected and analyzed in the current study are available from the corresponding authors on reasonable request.
References
Mehmood, A. et al. Fungal quorum-sensing molecules and inhibitors with potential antifungal activity: A review. Molecules 24, 1950. https://doi.org/10.3390/molecules24101950 (2019).
Kovács, R. & Majoros, L. Fungal quorum-sensing molecules: A review of their antifungal effect against Candida biofilms. J. Fungi (Basel) 6, 99. https://doi.org/10.3390/jof6030099 (2020).
Wongsuk, T., Pumeesat, P. & Luplertlop, N. Fungal quorum sensing molecules: Role in fungal morphogenesis and pathogenicity. J. Basic Microbiol. 56, 440–447. https://doi.org/10.1002/jobm.201500759 (2016).
Kitisin, T., Muangkaew, W., Ampawong, S. & Sukphopetch, P. Tryptophol coating reduces catheter-related cerebral and pulmonary infections by Scedosporium apiospermum. Infect. Drug Resist. 13, 2495–2508. https://doi.org/10.2147/IDR.S255489 (2020).
Singkum, P. et al. Suppression of the pathogenicity of Candida albicans by the quorum-sensing molecules farnesol and tryptophol. J. Gen. Appl. Microbiol. 65, 277–283. https://doi.org/10.2323/jgam.2018.12.002 (2020).
Otto, A., du Plessis, J. & Wiechers, J. W. Formulation effects of topical emulsions on transdermal and dermal delivery. Int. J. Cosmet. Sci. 31, 1–19. https://doi.org/10.1111/j.1468-2494.2008.00467.x (2009).
Tadić, V. M. et al. Enhanced skin performance of emulgel vs. cream as systems for topical delivery of herbal actives (immortelle extract and hemp oil). Pharmaceutics 13, 1919. https://doi.org/10.3390/pharmaceutics13111919 (2021).
Ajazuddin, et al. Recent expansions in an emergent novel drug delivery technology: emulgel. J. Control. Release 171, 122–132. https://doi.org/10.1016/j.jconrel.2013.06.030 (2013).
Kitisin, T. et al. Development and efficacy of tryptophol-containing emulgel for reducing subcutaneous fungal nodules from Scedosporium apiospermum eumycetoma. Res. Pharm. Sci. 17, 707–722. https://doi.org/10.4103/1735-5362.359437 (2022).
Wongsuk, T. & Sukphopetch, P. Effect of quarum sensing molecules on Aspergillus fumigatus. Walailak J. Sci. Tech. 17, 348–358. https://doi.org/10.48048/wjst.2020.6172 (2020).
Muangkaew, W., Wongsuk, T. & Luplertlop, N. Common dermatophytes and in vitro anti-fungal susceptibility testing in patients attending the Dermatological Clinic at the Hospital for Tropical Medicine, Bangkok. New Microbiol. 40, 175–179 (2017).
Suwanmanee, S., Kitisin, T. & Luplertlop, N. In vitro screening of 10 edible Thai plants for potential antifungal properties. Evid. Based Complement. Alternat. Med. 2014, 138587. https://doi.org/10.1155/2014/138587 (2014).
Kitisin, T. et al. Isolation of fungal communities and identification of Scedosporium species complex with pathogenic potentials from a pigsty in Phra Nakhon Si Ayutthaya, Thailand. New Microbiol. 44, 33–41 (2021).
White, T. C. et al. Fungi on the skin: Dermatophytes and Malassezia. Cold Spring Harb. Perspect. Med. 4, a019802. https://doi.org/10.1101/cshperspect.a019802 (2014).
Samaila, M. O. & Abdullahi, K. Cutaneous manifestations of deep mycosis: An experience in a tropical pathology laboratory. Indian J. Dermatol. 56, 282–286. https://doi.org/10.4103/0019-5154.82481 (2011).
Grover, S. & Roy, P. Clinico-mycological profile of superficial mycosis in a hospital in North-East India. Med. J. Armed Forces India 59, 114–116. https://doi.org/10.1016/S0377-1237(03)80053-9 (2003).
Jeu, L., Piacenti, F. J., Lyakhovetskiy, A. G. & Fung, H. B. Voriconazole. Clin. Ther. 25, 1321–1381. https://doi.org/10.1016/s0149-2918(03)80126-1 (2003).
Fisher, M. C. et al. Tackling the emerging threat of antifungal resistance to human health. Nat. Rev. Microbiol. 20, 557–571. https://doi.org/10.1038/s41579-022-00720-1 (2022).
Palmieri, A. & Petrini, M. Tryptophol and derivatives: Natural occurrence and applications to the synthesis of bioactive compounds. Nat. Prod. Rep. 36, 490–530. https://doi.org/10.1039/c8np00032h (2019).
Sajid, I., Shaaban, K. A. & Hasnain, S. Identification, isolation and optimization of antifungal metabolites from the Streptomyces Malachitofuscus ctf9. Braz. J. Microbiol. 42, 592–604. https://doi.org/10.1590/S1517-838220110002000024 (2011).
Proksch, E. pH in nature, humans and skin. J. Dermatol. 45, 1044–1152. https://doi.org/10.1111/1346-8138.14489 (2018).
Moon, S. H. et al. Pathological findings in cumulative irritation induced by SLS and croton oil in hairless mice. Contact Dermat. 44, 240–245. https://doi.org/10.1034/j.1600-0536.2001.044004240.x (2001).
Manian, M., Jain, P., Vora, D. & Banga, A. K. Formulation and evaluation of the in vitro performance of topical dermatological products containing diclofenac sodium. Pharmaceutics 14, 1892. https://doi.org/10.3390/pharmaceutics14091892 (2022).
Abdallah, M. H. et al. Quality by design for optimizing a novel liposomal jojoba oil-based emulgel to ameliorate the anti-inflammatory effect of brucine. Gels 7, 219. https://doi.org/10.3390/gels7040219 (2021).
Sabale, V., Kunjwani, H. & Sabale, P. Formulation and in vitro evaluation of the topical antiageing preparation of the fruit of Benincasa hispida. J. Ayurveda Integr. Med. 2, 124–128. https://doi.org/10.4103/0975-9476.85550 (2011).
Sukphopetch, P., Suwanmanee, S., Pumeesat, P. & Ampawong, S. In vitro characterization of chrysovirus-1-induced hypovirulence of Bipolaris maydis. Walailak J. Sci. Tech. 18, 6564. https://doi.org/10.48048/wjst.2021.6564 (2021).
Horváth, E., Sipiczki, M., Csoma, H. & Miklós, I. Assaying the effect of yeasts on growth of fungi associated with disease. BMC Microbiol. 20, 320. https://doi.org/10.1186/s12866-020-01942-0 (2020).
Muangkaew, W. et al. Effects of UVC Irradiation on growth and apoptosis of Scedosporium apiospermum and Lomentospora prolificans. Interdiscip. Perspect. Infect. Dis. 2018, 3748594. https://doi.org/10.1155/2018/3748594 (2018).
Fischer, T. & Maibach, H. Finn chamber patch test technique. Contact Dermat. 11, 137–140. https://doi.org/10.1111/j.1600-0536.1984.tb00957.x (1984).
Hua, W. et al. Comparison of two series of non-invasive instruments used for the skin physiological properties measurements: the DermaLab® from Cortex Technology vs. the series of detectors from Courage & Khazaka. Skin Res. Technol. 23, 70–78. https://doi.org/10.1111/srt.12303 (2017).
Acknowledgements
This research was financed by Mahidol University and Mahidol University (Basic Research Fund: fiscal year 2021) to Thitinan Kitisin and Mahidol University (Basic Research Fund: fiscal year 2022), The National Research Council of Thailand (Grant number: NRCT 230/2564), and Health Systems Research Institute (Grant number: HSRI 64-051) to Passanesh Sukphopetch.
Author information
Authors and Affiliations
Contributions
P.S. designed and supervised the project. N.T. involved in planning and supervising the work. T.K., W.M., N.T., and A.P. collected, analyzed, and interpreted the data. T.K. drafted the manuscript. P.S. and T.K. revised and completed the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kitisin, T., Muangkaew, W., Thitipramote, N. et al. The study of tryptophol containing emulgel on fungal reduction and skin irritation. Sci Rep 13, 18881 (2023). https://doi.org/10.1038/s41598-023-46121-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-023-46121-z
This article is cited by
-
A tryptophol-containing emulgel ameliorates imiquimod-induced mice psoriasis
Scientific Reports (2025)