Abstract
The primary objective of this study was to compare short-term outcomes between Intracorporeal ileocolic anastomosis (IIA) and extracorporeal ileocolic anastomosis (EIA) after laparoscopic right hemicolectomy in patients with visceral obesity. The secondary objective was to identify risk factors associated with prolonged postoperative ileus (PPOI) after laparoscopic right hemicolectomy. This single-center retrospective study analyzed visceral obesity patients who underwent laparoscopic right hemicolectomy for primary bowel cancer between January 2020 and June 2023. Patients were categorized into IIA and EIA groups based on the type of anastomosis, and a 1:1 propensity score-matched analysis was performed. A total of 129 patients were initially included in this study, with 45 patients in each group following propensity score matching. The IIA group had significantly longer anastomosis times (p < 0.001), shorter incision length (p < 0.001), and shorter length of stay (p = 0.003) than the EIA group. Meanwhile, the IIA group showed a shorter time to first flatus (p = 0.044) and quicker tolerance of a solid diet (p = 0.030). On multivariate analysis, postoperative use of opioid analgesics is an independent risk factor for PPOI (OR: 3.590 95% CI 1.033–12.477, p = 0.044), while IIA is an independent protective factor (OR: 0.195 95% CI 0.045–0.843, p = 0.029). IIA remains a safe and feasible option for visceral obesity patients. It is also associated with a quicker recovery of bowel function and shorter length of stay when compared to EIA. Additionally, IIA is an independent protective factor for PPOI.
Similar content being viewed by others
Introduction
Colorectal cancer ranks as the third most commonly diagnosed cancer in both men and women, with right-sided colon cancer often diagnosed at advanced stages1. As a standard surgical treatment, laparoscopic right hemicolectomy (LRC) has gained widespread adoption in the treatment of colorectal cancer due to the evidence of oncological safety and advantages in short-term surgical outcomes2,3,4. A consequent critical issue is that the restoration of intestinal continuity and functional integrity after bowel resection relies on safe and effective anastomotic techniques. Among these, intracorporeal ileocolic anastomosis (IIA) and extracorporeal ileocolic anastomosis (EIA) are commonly well-established techniques for LRC, with EIA being more prevalent albeit fraught with constant controversy.
Nowadays, IIA has garnered increasing attention with advancements in surgical instruments and techniques5. Some studies suggest that despite its technical challenges, IIA offers benefits such as faster postoperative recovery, reduced complications, and shorter hospital stays5,6,7. However, conflicting results have been reported in other studies8,9,10, leading to the ongoing debate regarding the superiority of IIA in short-term outcomes. Effective postoperative recovery, particularly the restoration of bowel function, is paramount in colorectal surgery. Normally, bowel function returns to baseline within 2–4 days11. However, delayed recovery, termed prolonged postoperative ileus (PPOI)12, can lead to discomfort, psychological distress, prolonged hospitalization, and increased costs13,14. Therefore, investigating factors influencing postoperative recovery, such as the choice of anastomotic technique, becomes imperative.
In addition, the increasing prevalence of obesity in the population means that physicians are more likely to encounter visceral obese (VO) patients15. It's important to note that VO is linked to increased operative technical risks, challenges, and complications when compared to non-obese patients16,17. Compared with normal patients, obese patients have heavier and shorter mesenteries. To date, there has been no study specifically addressing the use of IIA in VO patients. Thus, exploring the outcomes of IIA versus EIA after LRC in VO patients is essential for optimizing surgical approaches in this population.
Therefore, the primary objective of this study was to compare short-term outcomes between IIA and EIA after LRC in patients with VO. The secondary objective was to identify risk factors associated with PPOI after LRC.
Material and methods
Patient selection
We retrospectively obtained data from prospectively collected data recorded of patients who underwent LRC at the Second Affiliated Hospital of Dalian Medical University from January 2021 to June 2023. Inclusion criteria were as follows: (1) pathological diagnosis of adenocarcinoma; (2) VO (visceral fat area ≥ 100 cm2)18; (3) age ≥ 18 years. Exclusion criteria were as follows: (1) the presence of distant metastasis; (2) emergency surgery due to bleeding, perforation, or obstruction; (3) preoperative chemotherapy or chemoradiotherapy; (4) multiple tumors; (5) simultaneous surgery for other diseases. All procedures were performed by a surgeon (Shuangyi Ren) with experience performing more than 2000 laparoscopic surgeries.
Surgical technique
The initial steps of both procedures were standardized. The surgical approach began with a medial-to-lateral movement of the right colon, followed by bowel resection and lymph node clearance. Notably, all patients underwent D3 lymph node dissection, ensuring comprehensive nodal clearance. Major vessels were meticulously managed using titanium clips for secure hemostasis.
In cases of EIA, the intestine was extracted by extending the incision of the camera port, which was located in the supraumbilical midline. Following bowel resection, an ileocolic side-to-side isoperistaltic anastomosis was performed using a linear stapler. Subsequently, a 3–0 V-Loc barbed knotless suture was employed to reinforce closing the defect with sutures of the anastomosis with a continuous double-layer suture before returning the bowel to the abdominal cavity.
In cases of IIA, bowel resection and anastomosis were conducted intracorporeally. The ileocolic side-to-side isoperistaltic anastomosis was created using a linear stapler, with the closure of the enterotomy using laparoscopic sutures primarily. The specimen was removed by placing it in a specimen bag and extracted through a Pfannenstiel incision. The steps of IIA are summarized in Fig. 1.
(a) One enterotomy was created near the transection side of the colon (b) One enterotomy was created on the terminal ileum (c) Inserted the jaws of the staples and stapled side-to-side ileocolonic anastomosis (d) Closed the common channel of the enterotomy with a barbed knotless suture by 3–0 V-Loc (e) Laparoscopic view of the completed anastomosis.
Perioperative management
Since 2017, our institution has been following the principles of Enhanced Recovery After Surgery (ERAS) and making adjustments according to clinical needs, as detailed in Table S1. All patients were treated by the same perioperative enhanced recovery care program. Preoperative evaluation included clinical examination, serological assessment, colonoscopy, and abdominal computed tomography (CT). The diagnosis of colon cancer was based on pathological results.
Pain was quantified using the visual analog scale (ranging from 0 to 10) to assess pain after surgery. The administration of postoperative opioid analgesics was also evaluated as a consequence of pain tolerance in patients. Complications were classified using the Clavien–Dindo classification.
Variable and definition
The CT images at the third lumbar vertebrae level were imported into slice Omatic 5.0 (Tomovision) medical imaging analysis software for body composition analysis (Fig. 2)19. Fat tissue was quantified by using recognized Hounsfield unit thresholds (− 190 to − 30 HU)20,21 and the visceral fat area was measured after differentiation from the subcutaneous fat area.
We adopted the definition of PPOI as proposed by Vather et al.22. PPOI was diagnosed when patients met at least two of the following five criteria on or after postoperative day 4: (1) nausea or vomiting; (2) inability to tolerate a solid oral diet over the last 24 h; (3) abdominal distension; d. absence of flatus over the last 24 h; (3) ileus noted on computed tomography (CT) scans.
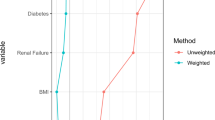
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 25 (IBM Corp, Armonk, New York, USA). The two groups were matched according to the anastomosis technique using a 1:1 nearest neighbor propensity score matching (PSM), with a caliper of 2 percent. Normally distributed continuous data were analyzed by Student's t-test and expressed as mean (± standard deviation [SD]); non-normally distributed data were analyzed by Wilcoxon rank-sum test and expressed as median (interquartile range [IQR]). Categorical data were compared using chi-squared test or Fisher’s exact test and expressed as n (%). Univariate logistic regression analysis was performed to initially assess associations of various indexes with PPOI. All indexes with p < 0.2 were included in the multivariate analysis. All of the statistical analyses were two-sided, and the statistical significance was set at p < 0.05.
Ethics approval
This study was conducted in accordance with the ethical principles outlined in the 1964 Declaration of Helsinki. Ethical approval for this study was obtained from the Institutional Review Board Ethics Committee at The Second Affiliated Hospital of Dalian Medical University.
Informed consent
Confirm that informed consent was obtained from all participants or their legal guardians.
Results
Patients' characteristics
A total of 165 patients were reviewed, of which 129 were included in our study (Fig. 3). In our cohort, 79 patients underwent EIA and 50 patients underwent IIA. Patients' characteristics according to the anastomosis technique are listed in Table 1. No significant differences were found between the EIA and IIA groups, except for Body mass index (BMI). After PSM, this study enrolled 45 patients in each group, and no significant differences were observed. The mean visceral fat area was 145.3 ± 27.3 cm2 in the IIA group and 148.2 ± 22.4 cm2 in the EIA group (p = 0.853).
Operative and pathological parameters
Operative parameters are shown in Table 2. In comparison to the EIA group, the IIA group had a longer anastomosis time (p < 0.001), but the difference in overall operation time did not reach statistical significance (p = 0.071). Additionally, in the IIA group, all patients had their specimens extracted via Pfannenstiel incision, while in the EIA group, patients had their specimens extracted via the midline abdominal incision. The incision length was shorter in the IIA group (p < 0.001).
The analysis of pathological parameters demonstrated adequate results in both groups (Table 2). In detail, there is no significant difference between the two groups in terms of the length of tumor diameter (p = 0.390), number of harvested lymph nodes (p = 0.258), and tumor stage (p = 0.943).
Short-term postoperative outcomes
Early postoperative outcomes are listed in Table 3. There were no statistically significant differences in the rates of overall complications (IIA vs. EIA: 11.1% vs. 20.0%, p = 0.344) and severe complications (IIA vs. EIA: 2.2% vs. 8.9%, p = 0.361) between the two groups. In addition, postoperative opioid analgesic requirements were also lower in the IIA group, but the difference did not reach significance (IIA vs. EIA: 26.7% vs. 44.4%, p = 0.078).
There was no significant difference in the time to first stool between the two groups (p = 0.197). However, the IIA group showed a shorter time to the first flatus (p = 0.044) and quicker tolerance of a solid diet (p = 0.030). Additionally, PPOI occurred in 5 cases in the IIA group while 14 cases in the EIA group (p = 0.037). In terms of the length of stay, patients who underwent IIA observed a shorter length of stay (IIA vs. EIA: 6 [5–7] vs. 7 [6–9], p = 0.003).
Univariate and multivariate logistic analysis of PPOI risk factors
Univariate and multivariate logistic analyses of factors influencing PPOI are reported in Table 4. Univariate analysis showed that age, smoking history, previous abdominal surgery, hypoalbuminemia, anastomosis technique, postoperative use of opioid analgesic, and estimated blood loss were potential predictors of PPOI. Subsequent multivariate logistic regression analysis showed that postoperative use of opioid analgesics is an independent risk factor for PPOI (OR: 3.590 95% CI 1.033–12.477, p = 0.044), while IIA is an independent protective factor (OR: 0.195 95% CI 0.045–0.843, p = 0.029).
Discussion
Nowadays, with innovations in surgical instrumentation, IIA using linear staples and barbed suture material allows for the increasing application of total laparoscopic right hemicolectomies. However, due to the greater technical difficulty and associated risk of intra-abdominal infection with IIA, many surgeons still hesitate to use it for LRC, and EIA remains the technique of choice23.
Some researchers have suggested that IIA may offer potential advantages in obese patients due to its avoidance of the need for bowel exteriorization during anastomosis, which could be exceedingly challenging when dealing with a short and thick mesentery24,25. Vignali et al.26 conducted a comparison between IIA and EIA in obese patients (BMI > 30) and reported that IIA in obese patients is associated with a lower incidence of incisional hernias, and might reduce the risk of hospital readmission. In LRC, the procedure takes place within the visceral cavity and the surgical technique may be influenced by intra-abdominal anatomy and physical conditions. VO, defined as a large accumulation of visceral adipose tissue, is considered a more reliable indicator than BMI in reflecting obesity in Asians27. Specifically, excessive adipose tissue may hinder finding and maintaining an accurate anatomical plane during surgery and pose difficulties for surgical procedures, such as space limitation, constraints on visualization of mesenteric vascular structures, intraoperative stretching of the bowel, and lymph node dissection28. To our knowledge, the present study is the first to compare IIA and EIA in patients with VO.
The study results indicate that although the difference in surgical time between the two groups did not reach significance (p = 0.071), the IIA group required more time for anastomosis compared to the EIA group8. However, the increase in surgical time did not lead to a higher incidence of postoperative complications; the overall rate and severity of postoperative complications were similar in both groups. These findings align with the conclusions of several previous studies and confirm the non-inferiority of IIA5,6. It is noteworthy that in this study, all IIA procedures utilized a Pfannenstiel incision. Previous research has reported that Pfannenstiel incisions can reduce postoperative pain, minimize incisional infections, and decrease the occurrence of incisional hernias28,29,30. However, in our study, no association was observed between EIA and increased incisional infections, possibly due to the use of incision protectors during surgery.
In this study, the length of hospital stay was significantly shorter in the IIA group, indicating an overall better recovery compared to the EIA group. This superior recovery with IIA was characterized by less wound pain and improved bowel function31,32,33,34. The research findings indicate that PPOI is unavoidable even within the context of ERAS protocols35. Similarly, our study on PPOI remains informative for laparoscopic rectal surgery within the ERAS protocols. Notably, we observed that IIA was identified as an independent protective factor for PPOI. The following reasons may explain the low frequency of PPOI in patients who underwent IIA. First, for EIA, due to the anatomical characteristics of the transverse mesocolon, which is centrally located and relatively short, mobilization of the transverse colon is usually required to extract the colon. Experiments have shown that excessive intestinal processing can increase the inflammatory response of the intestinal muscular layer, which may lead to the occurrence of postoperative intestinal obstruction and slow down the recovery of intestinal function36,37. In contrast, IIA does not require exteriorization of bowel and mesentery, resulting in a lesser impact on gastrointestinal motility20.
Second, IIA is associated with less postoperative pain and less use of opioid analgesics5. In the present study, postoperative opioid analgesic was used in 44.4% of patients in the EIA group compared to 26.7% in the IIA group. The relationship between opioid use and PPOI has been well described by previous studies, and the present study arrived at a similar conclusion38,39. While opioid administration may vary depending on the type of anastomosis performed, the postoperative pain management strategies within the ERAS protocols are adaptable and diverse. Therefore, even with advancements in surgical techniques, the potential improvement in laparoscopic surgical outcomes by opioid-sparing approaches remains noteworthy40. Additionally, less pain allows the patient to mobilize and walk around the ward early, which may promote bowel movements.
Obviously, the present study has several limitations. The major limitation lies in its retrospective nature and lack of randomization, even if PSM was used to reduce the potential selection bias. Second, due to the retrospective nature of this study, data on total intravenous fluid administration were limited, which may have influenced our results. Despite the above-mentioned limitations, this study provides evidence for the advantages in postoperative recovery and safety of IIA in patients with VO.
Conclusion
IIA remains a safe and feasible option for patients with VO. It is also associated with a quicker recovery of bowel function and shorter length of stay when compared to EIA. Additionally, IIA is an independent protective factor for PPOI.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
GBD 2017 Colorectal Cancer Collaborators. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 4, 913–933 (2019).
Arezzo, A. et al. Laparoscopic right colectomy reduces short-term mortality and morbidity: Results of a systematic review and meta-analysis. Int. J. Colorectal Dis. 30, 1457–1472 (2015).
Buunen, M. et al. Survival after laparoscopic surgery versus open surgery for colon cancer: Long-term outcome of a randomized clinical trial. Lancet Oncol. 10, 44–52 (2009).
Yamamoto, S. et al. Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann. Surg. 260, 23–30 (2014).
Zhang, H., Sun, N., Fu, Y. & Zhao, C. Intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: Updated meta-analysis of randomized controlled trials. BJS open 5, zrab133 (2021).
Allaix, M. E. et al. Intracorporeal or extracorporeal ileocolic anastomosis after laparoscopic right colectomy: A double-blinded randomized controlled trial. Ann. Surg. 270, 762–767 (2019).
Bollo, J. et al. Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br. J. Surg. 107, 364–372 (2020).
Dohrn, N. et al. Intracorporeal versus extracorporeal anastomosis in robotic right colectomy: A multicenter, triple-blind, randomized clinical trial. Ann. Surg. 276, 294-e301 (2022).
Małczak, P., Wysocki, M., Pisarska-Adamczyk, M., Major, P. & Pędziwiatr, M. Bowel function after laparoscopic right hemicolectomy: A randomized controlled trial comparing intracorporeal anastomosis and extracorporeal anastomosis. Surg. Endosc. 36, 4977–4982 (2022).
Trépanier, M. et al. Intracorporeal versus extracorporeal anastomosis for right colectomy does not affect gastrointestinal recovery within an enhanced recovery after surgery program. Surg. Endosc. 34, 4601–4608 (2020).
Wells, C. I. et al. Post-operative ileus: Definitions, mechanisms and controversies. ANZ J. Surg. 92, 62–68 (2022).
Bragg, D., El-Sharkawy, A. M., Psaltis, E., Maxwell-Armstrong, C. A. & Lobo, D. N. Postoperative ileus: Recent developments in pathophysiology and management. Clin. Nutr. 34, 367–376 (2015).
Lin, Z., Li, Y., Wu, J., Zheng, H. & Yang, C. Nomogram for prediction of prolonged postoperative ileus after colorectal resection. BMC Cancer 22, 1273 (2022).
Mao, H. et al. Prolonged postoperative ileus significantly increases the cost of inpatient stay for patients undergoing elective colorectal surgery: Results of a multivariate analysis of prospective data at a single institution. Dis. Colon Rectum 62, 631–637 (2019).
Pan, X. F., Wang, L. & Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 9, 373–392 (2021).
Aytac, E. et al. Single-port laparoscopic colorectal resections in obese patients are as safe and effective as conventional laparoscopy. Surg. Endosc. 28, 2884–2889 (2014).
Baastrup, N. N. et al. Visceral obesity and short-term outcomes after laparoscopic rectal cancer resection. Surg. Endosc. 34, 177–185 (2020).
Imai, Y. et al. Visceral fat area is a better indicator of surgical outcomes after laparoscopic gastrectomy for cancer than the body mass index: A propensity score-matched analysis. Surg. Endosc. 36, 3285–3297 (2022).
Chin, E. C. et al. Effects of one-year once-weekly high-intensity interval training on body adiposity and liver fat in adults with central obesity: Study protocol for a randomized controlled trial. J. Exerc. Sci. Fit. 20, 161–171 (2022).
Pedrazzani, C. et al. Impact of visceral obesity and sarcobesity on surgical outcomes and recovery after laparoscopic resection for colorectal cancer. Clin. Nutr. 39, 3763–3770 (2020).
Reisinger, K. W. et al. Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann. Surg. 261, 345–352 (2015).
Vather, R., Trivedi, S. & Bissett, I. Defining postoperative ileus: results of a systematic review and global survey. J. Gastrointest. Surg. 17, 962–972 (2013).
Milone, M. et al. Recovery after intracorporeal anastomosis in laparoscopic right hemicolectomy: A systematic review and meta-analysis. Langenbeck’s Arch. Surg. 403, 1–10 (2018).
Chen, F. et al. Intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: A retrospective study. World J. Surg. Oncol. 21, 154 (2023).
Hikage, M. et al. Advantages of a robotic approach compared with laparoscopy gastrectomy for patients with high visceral fat area. Surg. Endosc. 36, 6181–6193 (2022).
Vignali, A. et al. Intracorporeal versus extracorporeal anastomoses following laparoscopic right colectomy in obese patients: A case-matched study. Dig. Surg. 35, 236–242 (2018).
Hotouras, A. et al. The influence of obesity and body mass index on the outcome of laparoscopic colorectal surgery: A systematic literature review. Colorectal Dis. 18, 337–366 (2016).
Bège, T. et al. Impact of obesity on short-term results of laparoscopic rectal cancer resection. Surg. Endosc. 23, 1460–1464 (2009).
Martinek, L. et al. Does laparoscopic intracorporeal ileocolic anastomosis decreases surgical site infection rate? A propensity score-matched cohort study. Int J Colorectal Dis. 33, 291–298 (2018).
Squillaro, A. I. et al. Intracorporeal or extracorporeal anastomosis after minimally invasive right colectomy: A systematic review and meta-analysis. Tech Coloproctol. 27, 1007–1016 (2023).
Shapiro, R. et al. Laparoscopic right hemicolectomy with intracorporeal anastomosis: Short- and long-term benefits in comparison with extracorporeal anastomosis. Surg. Endosc. 30, 3823–3829 (2016).
Biondi, A. et al. Totally laparoscopic right colectomy versus laparoscopically assisted right colectomy: A propensity score analysis. Surg. Endosc. 31, 5275–5282 (2017).
Bou Saleh, N. et al. Intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy: results from the CLIMHET study group. Tech. Coloproctol. 24, 585–592 (2020).
Widmar, M. et al. Intracorporeal anastomoses in minimally invasive right colectomies are associated with fewer incisional hernias and shorter length of stay. Dis. Colon Rectum 63, 685–692 (2020).
Alhashemi, M. et al. Incidence and predictors of prolonged postoperative ileus after colorectal surgery in the context of an enhanced recovery pathway. Surg. Endosc. 33, 2313–2322 (2019).
Mari, G. M. et al. Intracorporeal anastomosis reduces surgical stress response in laparoscopic right hemicolectomy: A prospective randomized trial. Surg. Laparosc. Endosc. Percutaneous Tech. 28, 77–81 (2018).
Zhang, M. et al. Comparison of short-term outcomes between totally laparoscopic right colectomy and laparoscopic-assisted right colectomy: A retrospective study in a single institution on 300 consecutive patients. Surg. Endosc. 36, 176–184 (2022).
Chapman, S. J., Pericleous, A., Downey, C. & Jayne, D. G. Postoperative ileus following major colorectal surgery. Br. J. Surg. 105, 797–810 (2018).
Ju, H., Shen, K., Li, J. & Feng, Y. An increased total postoperative opiate dose is an independent risk factor for prolonged postoperative ileus after laparoscopic colorectal surgery: a case-control study. Korean J. Anesthesiol. (2023).
Gedda, C. et al. Multimodal analgesia bundle and postoperative opioid use among patients undergoing colorectal surgery. JAMA Netw. Open 6, e2332408 (2023).
Funding
Wu Jieping Medical Foundation Clinical Research Special Funding Fund (No. 320.6750.2022-18-13).
Author information
Authors and Affiliations
Contributions
F.L.G. and C.X. conceived the study design. Y.M. and Z.H.W. acquired the data for the study. R.Q.W. analyzed and interpreted the data. F.L.G. drafted the manuscript. S.Y.R. and Q.S.Z. revised the manuscript for important intellectual content. All authors revised and approved the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, F., Xia, C., Wang, Z. et al. Short-term outcome of intracorporeal ileocolonic anastomosis in patients with visceral obesity. Sci Rep 14, 13247 (2024). https://doi.org/10.1038/s41598-024-63966-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-63966-0
Keywords
This article is cited by
-
Design and validation of a simulation-based training module for ileo-transverse intracorporeal anastomosis
Surgical Endoscopy (2025)
-
A multicenter trial evaluating the short-term outcomes of intracorporeal versus extracorporeal anastomosis in laparoscopic colectomy for overweight and obese patients with colon cancer: a secondary analysis of the ICAN study
Surgery Today (2025)