Abstract
Relapsing polychondritis (RP) is a systemic immune mediated disease characterized by recurrent episodes of inflammation in various cartilage-rich areas. RP may cause extensive tissue destruction and is associated with significant morbidity and mortality. In this multicenter study, we considered the remission status and long-term outcomes of RP in patients who were followed-up in six referral rheumatology centers in Iran. Outcomes of disease was assessed by remission status and RP induced damage. A total of 29 patients with RP were examined for enrollment in the study, and 26 patients with a minimum follow-up period of 6 months were included in the RP outcome analysis. Median time to control of symptoms and sustained remission were 5 and 23 weeks, respectively. Prednisolone was discontinued in 8 (30.8%) patients and medication-free remission was achieved in 7 (23.1%) patients. Regarding the disease course, 34.6% of patients had a relapsing–remitting course, 42.3% had a monophasic course, and 23.1% had an always-active course. Despite extensive treatment with immunosuppressive medications, RP induced damage was developed in 21 (80.8%) patients. Ear deformity and osteoporosis were the most common RP induced damage. Long-term remission and medications-free remission in RP is accessible. However, RP related damage occur in majority of patients.
Similar content being viewed by others
Introduction
Relapsing polychondritis (RP) is a systemic immune mediated disease characterized by recurrent episodes of inflammation in various cartilage-rich areas, such as the ears, nose, joints and respiratory tract1. Although the exact cause of RP is unknown, it is thought to be an autoimmune disorder, as circulating autoantibodies against collagens II, IX, XI, cartilage oligomeric matrix proteins, and matrilin-1 have been identified in these patients2. RP is a rare disease, with an estimated prevalence of 3.5–4.5 cases per million people2. It can affect peoples of any age, but it most commonly presents in ages of 40 and 60, and both males and females can be affected equally2,3.
RP may cause extensive tissue destruction and is associated with significant morbidity and mortality1,2. Considering the relapsing remitting course of RP, the goal of treatment in this disease is to control the inflammatory crisis to prevent further tissue damage and long-term suppression of immune-mediated pathogenic mechanisms to prevent disease recurrence2,4. Due to the rarity of the disease and lack of controlled studies, there are no evidence-based guidelines for the treatment of RP. However, non-steroidal ant-inflammatory drugs (NSAIDs) and glucocorticoids (GCs) used for control of acute inflammation and conventional synthetic disease modifying antirheumatic drugs (csDMARDs) including azathioprine, methotrexate, cyclophosphamide, and cyclosporine and biologic DMARDs (bDMARDs) used for control of immune system activity with variable results2,4.
Despite numerous case reports and case series on the clinical manifestations and treatments of RP, there are few data on the long-term outcomes of RP treatment. In this multicenter study, we considered the remission status and long-term outcomes of RP.
Methods
Study population
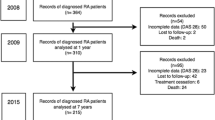
This retrospective multicenter study was conducted to investigate the long-term outcomes of RP in patients who were followed-up from July 2014 to October 2023 in six referral rheumatology centers in Iran including, Tabriz, Mashhad, Urmia, Tehran, Kashan, and Isfahan universities of medical sciences. Patients were included in the study if (i) were older than 18 years at disease onset, (ii) met the McAdam's criteria5 modified by Damian and Levine6 for RP, (iii) had at least 3 visits per year and (iv) had at least 6 months follow-up. Patients with insufficient data, irregular follow-up and loss to follow-up were excluded. The study protocol was approved by the ethics committee of Tabriz University of Medical Sciences (Ethical code: IR.TBZMED.REC.1402.294). Informed consent was obtained from all participants. This study was conducted in accordance with the Declaration of Helsinki.
Data collection and outcome assessment
The demographic, clinical, laboratory, therapies and outcomes data of the patients were obtained from their charts. The follow-up time was determined from the date of entering the cohort to the last visit. In case of incomplete data or loss to follow-up, we tried to obtain information through direct or telephone interviews. Disease activity was assessed using the Relapsing Polychondritis Disease Activity Index (RPDAI)7. Remission in all patients was assessed by an expert rheumatologist. Outcomes of disease was assessed by remission status and RP induced damage. Control of symptoms was defined as control of inflammatory symptoms (chondritis, arthritis, skin lesions, fever, etc.) with any dose of prednisolone and DMARDs for at least 4 weeks. Sustained remission was defined to control of inflammatory symptoms, prednisolone dose ≤ 7.5 mg/d for at least 12 weeks. DMARDs were permitted. The control of the inflammatory symptoms in chondritis was defined as the disappearance of pain, swelling and erythema, which was checked by examination and, if necessary, bronchoscopy and imaging. Arthritis control was defined as the absence of pain and swelling in the joint as assessed by a clinician. Relapse of RP was defined as (1) worsening or development of new RP-related symptoms identified by physical examination or imaging studies and leading to treatment escalation or (2) an increase in C-reactive protein (CRP) and erythrocyte sedimentation rate from baseline levels, which is considered due to RP activity and led to treatment intensification8. In patients with multiple remissions and relapses, the remission with the longest duration was used in the analysis of duration of remission. RP induced damage was assessed using the Relapsing Polychondritis Damage Index (RPDAM)9.
Statistical analysis
Statistical analysis was performed using SPSS software version 16.0 (SPSS, Inc., USA). The normal distribution of data was assessed using the Kolmogorov–Smirnov test. Normally and non-normally distributed continuous variables were reported as mean ± standard deviation (SD) and median (25–75% interquartile range [IQR]), respectively. Categorical variables were reported as frequency and percentage. Kaplan–Meier test was used for survival analysis. P-values less than 0.05 were considered as statistically significant.
Results
A total of 29 patients with RP were examined for enrollment in the study, whose demographic, clinical and laboratory characteristics are shown in Table 1. Finally, 26 patients with a minimum follow-up period of 6 months were included in the RP outcome analysis (Table 2). Mean age of the participants at the time of diagnosis was 42.8 ± 15.3 years and female:male ratio was 1.6. The median (IQR) duration of follow-up was 41 (19, 73) months. Auricular chondritis, nose chondritis, laryngeal chondritis, fever, arthralgia/arthritis, scleritis and uveitis were the most frequent clinical manifestations (Table 1). At least one auto-antibodies including perinuclear antineutrophilic cytoplasmic antibody (P-ANCA), cytoplasmic ANCA (C-ANCA), anti-nuclear antibody (ANA) and rheumatoid factor (RF) was positive in 17 (58.6%) patients (Table 1).
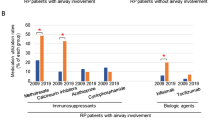
All patients were treated with GCs and/or DMARDs. Prednisolone was the most commonly used medication (Table 2). Other frequently used medications were azathioprine (53.8%), methotrexate (50.0%), and cyclophosphamide (19.2%). As initial therapy, all but 2 patients were treated with DMARDs. Monotherapy with DMARDs was performed in 21 (80.8%) patients and combination therapy was performed in 3 (11.5%) patients. However, during the course of the disease, a second DMARD was added to the treatment regimen in 7 (26.9%) patients, and the first DMARD was changed to another DMARD in 8 (30.8%) patients. Treatment with GCs and DMARDs lead to control of symptoms in 84.6% of patients and sustained remission in 76.9% of patients. Median time to control of symptoms and sustained remission were 5 and 23 weeks, respectively (Table 2 and Fig. 1). In all patients who responded to treatment, the response occurred within 12 months of diagnosis and initiation of treatment (Fig. 1). None of the demographic and clinical characteristics of the participants were predictive of sustained remission (Table 3). Although delay in diagnosis was shorter in patients with sustained remission, the difference did not reach significant levels (Table 3). Prednisolone was discontinued in 8 patients (30.8%) and medication-free remission was achieved in 7 (23.1%) patients. Regarding the disease course, 34.6% of patients had a relapsing–remitting course, 42.3% had a monophasic course, and 23.1% had an always-active course.
Despite extensive treatment with immunosuppressive medications, RP induced damage was developed in 21 (80.8%) patients (Table 4). Sixteen (61.5%) were damaged due to the inflammatory process, 11 (42.3%) were damaged due to treatment complications and 6 (23.1%) suffered from both (Table 4). Median (IQR) RPDAM was 1 (0.8, 2). Ear deformity and osteoporosis were the most common RP induced damage (Table 4). One of the most debilitating RP induced damage is tracheobronchial which occurred in 3 patients (11.5%), and one of them required tracheostomy. We compared the demographic and clinical characteristics of patients with and without damage. Except for the higher frequency of damage in patients with trachea laryngeal involvement, none of the demographic and clinical characteristics of the participants were predictor of damage (Table 5). Surgery was performed in 3 patients (11.5%) for corneal transplant (n = 1), total hip replacement (n = 1) and tracheobronchial stenosis (n = 1). Although delay in diagnosis and time to remission was shorter in patients without damage, the difference did not reach significant levels. Damage severity assessed by RPDAM was lower in patients with sustained remission than in patients with no sustained remission (Table 3) Five years survival rate was 95.5%. One patient died during follow-up due to pneumonia.
Discussion
Management of RP poses significant challenges due to its rarity and the heterogeneity of symptoms and disease course. This study aimed to evaluate the outcomes and treatment patterns in a cohort of RP patients, shedding light on the current understanding of this complex disease. The results of this study showed that RP was diagnosed 22 weeks after the onset of symptoms and treatment with GCs and DMARDs resulted in symptom control and sustained remission in most patients (85% and 77%). Response to treatment occurred in majority of patients in 5 months and in all patients within 12 months. These results are encouraging, as achieving remission is a primary therapeutic goal in RP to prevent further damage to cartilage structures. Medication-free remission was achieved in 23% of patients. However, relapse occurred in 25% of patients after discontinuation of prednisolone and in 50% of patients after discontinuation of DMARDs, suggesting the need for ongoing monitoring and management to prevent relapse.
Although there was no significant difference in the demographic characteristics and clinical manifestations of the studied patients with previous studies8,10,11,12,13,14,15,16, it is difficult to compare treatment results with previous reports due to differences in outcome definitions and lack of data on the remission rate in most studies (Table 6). Disease activity in our study as measured by the RPDAI was 31, which is higher than the only study in which disease activity was measured by this instrument, study Yoshida et al.8. There was a significant difference in the treatment strategy between the different studies, so that the rate of treatment with biological drugs in the studied patients was lower than the more recent reports8,15,16. Despite the availability of many biological drugs in Iran, such as TNFis, rituximab and tocilizumab, the lack of approval of these drugs in the treatment of RP by insurance organizations is a possible reason for the underuse of them in studied patients. Of the 5 patients treated with bDMARDs in this report, sustained remission was achieved in 3 patients, which is comparable to the results of Sangle et al.16 report. However, there was no significant difference in the rate of sustained remission in patients treated with bDMARDs versus patients not treated with bDMARDs. Nevertheless, the five years survival rate in our study (95.5%) was consistent with recent studies from other countries8,14,15. In Shimizu et al. report GCs, csDMARDs and bDMARDs were used in 91, 60 and 14 percent of RP patients15. They reported increase in the prescription of csDMARDs and bDMARDs in 2019 compared to 2009 and a decrease in RP mortality from 22 to 3% during this time period15. Sangle et al.16 in a retrospective study reported a diagnosis delay of 55 weeks. Combination therapy with prednisolone and DMARDs was performed in 97% of patients and 63% eventually required biological drugs16. However, mortality was 18%16. Recent evidences shows that improvements in diagnostic methods and treatment of RP have led to earlier diagnosis and an increase in the 10-year survival rate from 55% in 198610 to 91% in 201614. In a single center study from Japan diagnosis delay was 22 weeks8. Although 26% of patients experienced sustained remission, relapse occurred in the remaining 74%8. Higher CRP level and monotherapy with GCs was associated with relapse8.
This study was a multicenter study that, to the best of our knowledge, focused for the first time on remission rates and medications-free remission in RP. However, due to the small sample size, we were unable to analyze predictors of medication-free remission.
Conclusion
Long-term remission and medications-free remission in RP is accessible. However, RP induced damage occur in majority of patients.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Lahmer, T. et al. Relapsing polychondritis: An autoimmune disease with many faces. Autoimmun. Rev. 9, 540–546 (2010).
Borgia, F., Giuffrida, R., Guarneri, F. & Cannavò, S. P. Relapsing polychondritis: An updated review. Biomedicines 6, 84 (2018).
Horváth, A. et al. A nationwide study of the epidemiology of relapsing polychondritis. Clin. Epidemiol. 8, 211–230 (2016).
Arnaud, L., Mathian, A., Haroche, J., Gorochov, G. & Amoura, Z. Pathogenesis of relapsing polychondritis: A 2013 update. Autoimmun. Rev. 13(2), 90–95 (2014).
McAdam, L. P., O’Hanlan, M. A., Bluestone, R. & Pearson, C. M. Relapsing polychondritis: Prospective study of 23 patients and a review of the literature. Medicine (Baltimore) 55, 193–215 (1976).
Damiani, J. M. & Levine, H. L. Relapsing polychondritis-report of ten cases. The Laryngoscope 89, 929–946 (1979).
Arnaud, L. et al. The relapsing polychondritis disease activity index: Development of a disease activity score for relapsing polychondritis. Autoimmun. Rev. 12, 204–209 (2012).
Yoshida, T. et al. Risk factors for the recurrence of relapsing polychondritis. Arthritis Res. Ther. 24, 127 (2022).
Mertz, P. et al. The relapsing polychondritis damage index (RPDAM): Development of a disease-specific damage score for relapsing polychondritis. Jt. Bone Spine 86, 363–368 (2019).
Michet, C. J., McKenna, C. H., Luthra, H. S. & O’Fallon, W. M. Relapsing polychondritis. Survival and predictive role of early disease manifestations. Ann. Intern. Med. 104, 74–78 (1986).
Kong, K. O., Vasoo, S., Tay, N. S. W. T. & Chng, H. H. Relapsing polychondritis: An oriental case series. Singap. Med. J. 44, 197–200 (2003).
Mathew, S. D., Battafarano, D. F. & Morris, M. J. Relapsing polychondritis in the department of defense population and review of the literature. Semin. Arthritis Rheum. 42, 70–83 (2012).
Sharma, A. et al. Relapsing polychondritis: Clinical presentations, disease activity and outcomes. Orphanet. J. Rare Dis. 9, 198 (2014).
Dion, J. et al. Relapsing polychondritis can be characterized by three different clinical phenotypes: Analysis of a recent series of 142 patients. Arthritis Rheumatol. 68, 2992–3001 (2016).
Shimizu, J., Yamano, Y., Kawahata, K. & Suzuki, N. Nationwide cross-sectional survey of patients with relapsing polychondritis in 2019 demonstrates reduction of airway involvement compared with that in 2009. Sci. Rep. 12, 465 (2022).
Sangle, S. R. et al. Relapsing polychondritis: A single centre study in the United Kingdom. Autoimmun. Rev. 22, 103352 (2023).
Acknowledgements
We thank all the participants of this study who contributed with us and Connective Tissue Diseases Research Center for supporting this study.
Funding
This study was founded by the Connective Tissue Diseases Research Center.
Author information
Authors and Affiliations
Contributions
Conceptualization and designing the study: M.J. and A.K. Data acquisition: M.S., M.S., S.S., M.S., S.H., T.F., K.E., M.H., S.K., Z.M., A.K. Drafting the manuscript: M.J., A.K. and M.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jafarpour, M., Saberivand, M., Saemi, M. et al. A multicenter study of long-term outcomes of relapsing polychondritis in Iran. Sci Rep 14, 16486 (2024). https://doi.org/10.1038/s41598-024-67530-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-67530-8
Keywords
This article is cited by
-
What are risk factors for relapse in relapsing polychondritis? A retrospective study
Clinical Rheumatology (2025)