Abstract
The aim of this study was to investigate the effect of zoledronic acid (ZA) on postoperative healing and functional rehabilitation in osteoporotic patients with rotator cuff (RC) injury. 96 Patients were divided into three groups according to bone mineral density and ZA use (Group A: normal BMD; Group B: osteoporosis and intravenous ZA use; Group C: osteoporosis, without ZA use). Radiologic, functional and Serological outcomes were evaluated 6 months after surgery. The functional scores in all groups exhibited significant improvement 6 months after surgery. Inter-group comparison showed that Constant Shoulder joint function Score (CSS) of group A not significantly differing from that of group B, the other indicators were significantly better than those of group B and C. There were no significant differences in shoulder forward flexion, abductive Range of Motion between group B and C. Other indicators of group B were significantly improved compared to group C. The retear rate in group C (30.3%, 10/33) was higher than group A (6.1%, 2/33) and group B (13.3%, 4/30). In conclusion, the application of ZA can significantly reduce the rate of RC retear in elderly patients with osteoporosis after surgery, which is significant for postoperative shoulder joint functional rehabilitation.
Similar content being viewed by others
Introduction
Rotator cuff (RC) tear is a common shoulder joint disease seen in clinical practice. Its incidence increases with age and is mostly characterized by symptoms such as shoulder joint pain, weakness, or limited activity. If the condition continues to progress, it can cause a decline in shoulder joint stability and disuse osteoporosis of the proximal humerus1,2. Recent studies have indicated that arthroscopic rotator cuff repair (ARCR) can lead to improved surgical outcomes and clinical improvement. However, failure of rotator cuff healing after repair is one of the most common and crucial complications that affect clinical outcomes, with reported rates ranging from 9 to 94% in the current literature3,4,5,6. Despite various efforts made to improve healing after surgical repair, such as the use of platelet-rich plasma, growth factors, exosomes, and stem cell therapy, these interventions have limited efficacy in reducing the failure rate of rotator cuff healing7,8,9. Several studies have demonstrated that the healing of the rotator cuff is influenced by multiple factors, such as age, smoking, BMI, fat infiltration, BMD, and others10. Of note, the retear rate is significantly higher in elderly patients than in younger people, which may be due to an unfavorable biological “healing environment.” Additionally, bone quality at the repair interface is a crucial factor recently observed to impact rotator cuff healing11,12,13,14. RC tears are frequently accompanied by a reduction in bone mineral density (BMD) of the greater tuberosity of the humerus, and this decrease in BMD can affect tendon-bone healing after ARCR, leading to retear after surgery2. Although the torn tendon is repaired surgically, the bone loss at the insertion site of the tendon is not fully restored. In recent years, researchers have turned their attention from osteoporotic fractures to tendon-bone healing in the elderly population, but there has been limited clinical research on their relationship to the prognosis after rotator cuff repair. As an independent risk factor affecting rotator cuff healing, osteoporosis should receive attention from surgeons11,13.
Structural failure after RC repair is defined as a failure of tendon-to-bone healing, and this failure may be related to both bone and tendon quality15. The unique structure of the tendon-bone junction leads to poor healing capability and extended healing time after surgical reconstruction. The duration of the healing process directly affects the early rehabilitation training of patients. Therefore, promoting tendon-bone healing is the primary focus of surgical reconstruction treatment and functional recovery16. Furthermore, aging is frequently associated with increased incidence of osteoporosis and RC injuries. RC tears are more common at older ages, and the elderly population, particularly postmenopausal women, are more prone to develop osteoporosis17,18. Given that the incidence of rotator cuff tear and osteoporosis increases with age, addressing osteoporosis in elderly patients with RC tears is a critical issue that requires attention.
Generally, bisphosphonates are recognized as anti-osteoclast drugs that enhance BMD by inhibiting the activation and maturation of osteoclast precursor cells to osteoclasts. They can also effectively prevent osteoblast and osteocyte apoptosis19. Research studies have demonstrated that treatment with 5 mg of intravenous zoledronic acid (ZA) once per year is effective in preventing excessive bone loss in patients with osteoporosis20,21. Furthermore, bisphosphonates have a strong bone affinity, can persist in the bone for extended periods, and have a good absorption effect, allowing for good clinical outcomes in increasing bone density. Numerous animal experimental studies have reported the benefits of reducing osteoclast density with bisphosphonates in promoting tendon-bone healing22,23. It is well-established in the literature that osteoporosis not only affects bone tissue but also significantly impacts muscle tissue, potentially leading to sarcopenia24. Moreover, bisphosphonates have been shown to influence muscle proliferation and function positively25.
Furthermore, bone formation requires the synergistic action of osteoclasts and osteoblasts. Bone metabolic markers are bone tissue metabolites that enter the human blood circulation, and their concentrations are influenced by the activities of osteoclasts and osteoblasts. These markers usually comprise bone formation markers and bone resorption markers. The former include Total Procollagen type 1 N-terminal propeptide (P1NP), Bone alkaline phosphatase (B-LAP), and Osteocalcin (OSTEOC), while the latter mainly consist of Serum Beta-Cross laps (βCross) and Tartrate-resistant Acid Phosphatase (TRACP). The dynamic balance of bone resorption and bone formation is the basis of BMD change, indicating that bone metabolic markers can predict BMD26. Vitamin D is a crucial element in bone formation, and its role in bone formation is well-known. The majority of osteoporosis patients have a deficiency of vitamin D, and determining the individual’s vitamin D levels is one of the effective methods to detect this deficiency. The detection of Total 25 Hydroxyitamin D (T-25 OHD) is a useful method for evaluating an individual’s vitamin D levels27.
Hence, this study hypothesizes that administering postoperative intravenous zoledronate could enhance bone metabolism, decrease the re-tear rate of rotator cuff repair, and enhance functional recovery in elderly patients who have osteoporotic rotator cuff injury. To investigate this hypothesis, the study intends to analyze the impact of postoperative intravenous zoledronate on rotator cuff healing, retear rate, and clinical outcome in elderly patients with osteoporosis undergoing arthroscopic rotator cuff repair (ARCR) via a retrospective study of 96 patients.
Result
Comparison of general data
The demographic data of the three groups were not significantly different, except for BMD. The BMI was similar across the three groups (P = 0.21). The tear sizes measured by MRI in the three groups were 21.3 ± 7.1 and 22.9 ± 8.5 and 24.8 ± 6.7 mm. The tear size of the tendons was slightly larger in Group C than in Group A and B (P = 0.17) (Table 1).
Comparison of preoperative and postoperative VAS, ASES, UCLA, CSS scores and ROM of the shoulder joint among three groups
There was no significant difference in preoperative VAS, ASES, UCLA and CSS scores among three groups (P > 0.05).The functional scores, including ASES, UCLA and CSS, were significantly improved at 6 months after surgery in all groups (P < 0.05), and the VAS score showed a significant downward trend after surgery, indicating that surgical treatment was effective for all patients. There were significant differences in VAS, ASES, UCLA and CSS scores among the three groups at 6 months after operation (P < 0.05). Inter-group comparison showed no significant difference in CSS scores between group A and group B at 6 months after surgery, while other indicators showed significant differences (P < 0.05). Group A had better outcomes than group B, and group B had better outcomes than group C (Table 2 and Fig. 1).
Comparison of VAS /ASES/UCLA/CSS scores among three groups. (A–D) Inter-group comparison of VAS /ASES/UCLA/CSS scores at different time points among three groups. (E–H) Intra-group comparison of VAS /ASES/UCLA/CSS scores among three groups at different time points. *Indicates P < 0.05; **Indicates P < 0.01.
Before surgery, there was no significant difference in preoperative shoulder joint ROM (including abduction, forward flexion, and internal rotation) among the three groups (P > 0.05). At 6 months after surgery, ROM in all three groups showed significant improvement compared to before surgery (P < 0.05). Furthermore, there was a significant difference in ROM among the three groups at 6 months after surgery. The forward flexion and abduction motion of group A were significantly higher than those of group B and group C (P < 0.05), but there was no statistical significance between group B and group C (P > 0.05). The internal rotation motion of the three groups was 8.6 ± 2.4, 7.1 ± 2.2, and 5.4 ± 1.9, respectively. There was a significant difference in internal rotation motion among the three groups (F = 17.87, P < 0.001), where group A had better outcomes than group B, and group B had better outcomes than group C (P < 0.01) (Table 2 and Fig. 2).
Comparison of range of motion (ROM) of shoulder joint among three groups. (A–C) Inter-group comparison of ROM of shoulder joint at different time points among three groups. (D–F) Intra-group comparison of ROM of shoulder joint at different time points among three groups. *Indicates P < 0.05, **Indicates P < 0.01.
Comparison of serum bone metabolism markers between B and C groups before and 6 months after surgery
The level of bone metabolism before surgery was similar between the two groups, there was no significant difference (P > 0.05). However, it is worth noting that both groups of patients were in a state of vitamin D deficiency. 6 months after surgery, bone metabolism in group B was significantly improved compared with that before surgery, and all indexes except T-25 OHD were significantly decreased (P > 0.05); In group C, except for T-25 OHD, which increased from 16.1 ± 5.3 to 22.1 ± 6.4 (t = 4.16, P < 0.001), the other markers of bone metabolism were slightly lower than those before surgery, and were basically in stable state, without significant significance (P > 0.05). Inter-group comparison showed that bone metabolism in group B was significantly lower than that in group C (P < 0.01), and there was no significant difference in T-25 OHD level between the two groups (t = 0.76, P = 0.4509) (Table 3 and Fig. 3).
Comparison of the postoperative Retear rate and Retear pattern among three groups
6 months after surgery, the retear rates of the three groups were 6.1% (2/33) in group A, 13.3% (4/30) in group B and 30.3% (10/33) in group C, respectively, with significant differences (χ2 = 7.33, P = 0.0256). Inter-group comparison showed that there was significant difference between group A and group C (χ2 = 6.51, P = 0.0107), but there was no significant difference between A and B group (χ2 = 0.96, P = 0.3260) or B–C group (χ2 = 2.62, P = 0.1056). For the type of retear, all patients in group A were type I. In group B, there were 3 cases of type I and 1 case of type II. In group C, 6 cases were type I and 4 cases were type II. There was no statistical significance (χ2 = 1.34, P = 0.51) (Table 4).
Discussion
This is a retrospective study that aims to investigate the effects of intravenous ZA on rotator cuff healing in humans. Rotator cuff (RC) healing after surgery to repair failure is one of the most common and important complications of this structure, with failure rates ranging between 9 and 94%3,4,5,6. The present study’s overall failure rate of 16.7% is comparable to rates reported in previous studies. One of the study’s most significant findings is that osteoporosis can hinder RC healing after ARCR in elderly patients. What’s more, the study found that postoperative treatment with ZA in elderly patients with osteoporosis can effectively reduce the healing failure rate caused by bone loss, though the failure rate still remains higher than in patients with normal bone density.
The incidence of RC tears is known to increase with age. According to a cross-sectional study conducted on the general population, the incidence of total RC tears was found to be 22.2%, with an increase in incidence corresponding to age; from 10.7% at age 50–62% at age 8028,29. Previous studies have suggested that bone loss in elderly patients can severely affect the remodeling process of the tendon-bone junction site, making it more susceptible to tendon re-tear after ARCR. This is believed to be due to the lowered bone density in patients with osteoporosis, which inevitably impacts the fixation strength of the tendon-bone repair site, resulting in the loosening of suture anchors and eventual withdrawal before adequate tendon-bone healing15,30. Tingart et al. conducted a cadaveric study that established a positive correlation between the pull strength of sutured anchors and the bone density of the greater tubercle. Their findings indicated that anchor placement in areas of low bone density may lead to anchor loosening, formation of tendon-bone space, and eventual failure in ARCR31. Djurasovic et al. reviewed 80 patients who underwent RCR revision and found that 8 cases failed due to loosening at the implant-bone interface32. In our study, we identified 2 cases of anchor failure, both of which were patients in group C, indicating a potential association between osteoporosis and anchor failure. This is similar to previous research. Studies have demonstrated that BMD measured by DXA can reflect the bone mass of the greater tubercle13. This finding have been supported by research from Park and Kim et al.33, who have shown that generalized BMD measurements can also offer a reliable indication of proximal humerus BMD, with strong correlations between lumbar spine BMD and proximal humerus BMD recorded across both male and female subjects (R = 0.55 and R = 0.58, respectively). It is worth noting that the density of the greater tuberosity of the humerus commonly decreases even further following RC injury. In such cases, high tendon retraction can also rapidly impact bone mass, further exacerbating the loss of BMD at the tendon-bone interface2. Therefore, researchers have focused on increasing the stability of the tendon-bone junction to enhance rotator cuff healing after ARCR, including increasing the number and diameter of anchors, using metal anchors, vertical insertion of anchors, and reinforcing anchors with bone grafting and cement34,35.
Furthermore, there appears to be a biological connection between osteoporosis and tendon-bone healing, as excessive osteoclast activity associated with osteoporosis or osteopenia can impede bone ingrowth at the tendon-bone attachment site, reducing biomechanical properties and weakening the overall site13. Rodeo et al. reported the application of nuclear factor receptor activator—K-β ligand (RANKL) can lead to increased increased osteoclast activity and decreased stiffness of rabbit tendon-bone junction22. In the initial 3-week healing stage, the heightened activity of osteoclasts can result in the structural weakening of bones at the tendon-bony interface36. Thus, given the adverse impact of osteoclasts on bone architecture, it may be beneficial to restrict their activity at the repair site in osteoporotic patients to help improve tendon-bone healing. Previous animal experimental studies have revealed that the activity of osteoclasts at the healing interface is notably heightened in animal models of osteoporosis, and this consequently disrupts early healing after RC injury. However, postoperative administration of bisphosphonates targeted at osteoporosis has been shown to diminish both the density and activity of osteoclasts in animal models of osteoporosis, thereby improving the healing of the RC22,23. Lee et al. also believed that ZA could reduce the re-tear rate by decreasing the activity of osteoclasts and promoting bone ingrowth at the bone-tendon junction6. In general, the healing of the tendon-to-bone connection is crucial in achieving favorable outcomes for various surgical procedures aimed at repairing injured tendons, and good healing between tendon and bone is integral to functional recovery16. In the present study, patients in group B were treated with ZA following surgery and were followed up for 6 months. MRI was performed at the final follow-up to evaluate the presence of re-tear events in all groups. Our findings revealed that structural failure of RC healing occurred in 4 patients in group B, whereas 10 patients in group C experienced the same outcome. The failure rate was significantly lower in group B than group C (13.3% vs. 30.3%). Additionally, 2 cases of structural failure were observed in group A (6.1%), which displayed a markedly lower re-tear rate compared to group B and group C (χ2 = 7.33, P = 0.0256). Inter-group comparison showed a considerable difference in the re-tear rate was also demonstrated between the A and C group (χ2 = 6.51, P = 0.0107). Although no statistically significant differences were observed in the re-tear rate between the A-B group and the B-C group, this may be due to the small sample size, the data above provide reliable evidence that postoperative anti-osteoporosis treatment with ZA significantly promotes tendon-bone healing and reduces the rate of re-tear while enhancing structural healing following ARCR in elderly patients with osteoporosis.
A recent prospective imaging study has highlighted that a considerable number of re-tears occur during the period spanning between 6 and 26 weeks after ARCR37. Kluger et al. proposed that the majority of recurrent tears happen within the initial 3 months following surgical repair. Furthermore, they indicated that evaluating the parameters of “recurrent tears” and “healed tendon” 6 months after surgery may have predictive value for 7-year clinical outcomes. The authors recommend placing emphasis on enhancing the healing process within the first 3 months post-operatively38. Therefore, we believe that the vast majority of retears can be detected by 6 months follow-up. However, obtaining a more comprehensive result requires longer follow-up of patients.
Interestingly, Cancienne et al. reported a low efficacy of bisphosphonates in reducing the failure rate after ARCR in osteoporosis patients39. However, they solely relied on the administrative claims database which may have contained miscoded and uncoded data, leading to misleading results. Conversely, other studies have demonstrated that treatment with ZA can effectively combat osteoporosis and substantially enhance tendon-bone healing6,23,40. Our study also yielded similar results, indicating the significance of postoperative intravenous ZA in promoting tendon healing and enhancing shoulder function in patients. Furthermore, bone metabolism markers displayed dynamic changes within a month of treatment, enabling the prediction of therapeutic efficacy between 3 and 6 months. Compared to the change cycle of BMD over a year, the early changes observed in bone metabolism markers offer valuable insight for early evaluation by clinical professionals41. In our study, we observed a significant decrease in the bone resorption marker β Cross in group B at 6 months post-surgery, in contrast to the pre-surgery levels (P < 0.05), suggesting the considerable inhibition in osteoclast function. Additionally, P1NP, OSTEOC, and B-LAP levels were also significantly reduced (P < 0.05), indicating that ZA also inhibited some activity of osteoblasts in the short term. These results are consistent with those of Uehara et al.42, who reported similar findings in their previous study and the activity of osteoblast will recover rapidly after a short period of inhibition. Meanwhile, Camille et al. pointed out that muscle weakness is an important influencing factor of rotator cuff injury43, and the use of ZA not only improves bone metabolism, but also helps to improve muscle quality. Based on these findings, the preoperative and postoperative VAS, ASES, UCLA, and CSS scores of the three groups were compared. The analysis demonstrated significant clinical improvement in the functional outcome indices of all patients at the final follow-up compared to before surgery, irrespective of whether the structure had failed or not. This result indicated that ARCR had a positive clinical effect on RC injury. These conclusions are consistent with previous research in this field4,6,44. The inter-group comparison revealed significant differences in functional outcome indices among the three groups. Compared with groups B and C, group A demonstrated significantly better results in VAS, ASES, and UCLA scores (P < 0.05). Although there was no significant difference in CSS scores between groups A and B (P > 0.05). These findings suggest that the use of ZA improves the metabolic balance of bones and promotes further healing of tendon-bone. Good tendon-bone healing and muscle strength is essential for the ultimate success of various surgical procedures for repairing the injured tendon, which is closely related to patients’functional rehabilitation in the later stage.
In a recent prospective cohort study conducted by Paul et al., they found that there is a dissociation between MRI-based healing grade and functional recovery of the shoulder joint. This means that patients with poor structural integrity after ARCR surgery can also have good functional outcomes45. Our study demonstrated that the postoperative range of motion (ROM) of the shoulder joint (forward flexion, abduction, and pronation) in all three groups significantly improved compared to preoperative levels, indicating the positive clinical effect of ARCR on rotator cuff injury. However, significant differences were observed among the three groups, with group A demonstrating significantly better outcomes compared to Groups B and C, which was positively correlated with the lower retear rate in Group A. Compared to Group C, although Group B’s re-tear rate improved, abduction and forward flexion activities in Group B were not significantly improved, only the internal rotation activities were significantly better than Group C (P < 0.05). These findings are consistent with the study by Paul et al.45, which suggested that even if some patients exhibited tendon re-tearing on MRI 6 months after ARCR surgery, their clinical function outcomes may partially improve due to partial healing of tendon-bone or scar healing. Overall, the shoulder ROM in Group C was significantly different from that in patients with a normal bone density or those who received zoledronic acid. Future studies with longer follow-up periods are necessary to confirm the relationship between structural and functional outcomes.
In conclusion, our study demonstrated the effect of BMD and intervention of BMD on the postoperative efficacy of RC injury. We believe that BMD can be artificially controlled and managed through joint efforts of patients and doctors. For example, maintaining adequate calcium and vitamin D intake, taking phosphate drugs, maintaining a healthy weight, quitting smoking, reducing alcohol consumption, and undertaking strengthening exercises can all improve BMD and delay the development of osteoporosis. Furthermore, improving osteoporosis through active management of BMD in daily life is significant for improving the healing rate and postoperative efficacy after ARCR.
In addition, there are some limitations to this study. Firstly, this is a retrospective study with a short-term follow-up period, larger and longer follow-up randomized controlled trials are required to confirm the findings of this study. Secondly, the study did not account for other systemic diseases as confounding factors. In Group B, one patient with retear had diabetes. Among the ten patients with retear in Group C, two had diabetes, one had dyslipidemia, and one had hypothyroidism. Although no independent factors were found to have influenced the results, the study may benefit from accounting for confounding variables in future studies. Furthermore, although we compared the BMI of the patients in the three groups, and previous studies have indicated a significant linear relationship between the degree of rotator cuff tendon fat infiltration and BMI46, it would be beneficial to consider the degree of tendon steatosis as an independent factor to arrive at a more effective conclusion. Finally, we did not perform the corresponding histological analysis of the tendon-bone interface. Although similar to previous animal studies, we have not been able to identify any clear micro-improvement in vivo.
Conclusion
In summary, osteoporosis substantially impacts the rehabilitation of patients undergoing surgery for rotator cuff injuries. Among elderly patients with osteoporosis who undergo rotator cuff repair, the re-tear rate is significantly higher. However, the use of zoledronic acid can significantly reduce the incidence of re-tear, aid in shoulder joint function recovery after surgery, particularly in cases involving tears smaller than 3CM. Furthermore, it is recommended that patients and clinicians actively manage and control bone mineral density through lifestyle interventions to improve the healing rate following shoulder arthroscopic rotator cuff repair. This approach can lead to maximal benefits for patients.
Methods
Subjects and grouping
The study selected 96 patients from a total of 121 patients with rotator cuff injury who received treatment at the First and the Second Affiliated Hospital of Xi 'an Jiaotong University between June 2020 and June 2022. The selection process was strictly based on the following inclusion criteria: (1) rotator cuff injury that was diagnosed by two physicians with senior professional titles in sports medicine through preoperative MRI and intraoperative arthroscopy examination, with tear larger than 1.5 cm and no large fat infiltration; (2) age over 50 years old; (3) non-traumatic injury; (4) total arthroscopic rotator cuff repair was performed; (5) able to cooperate with doctors to complete bone densitometry, shoulder joint clinical efficacy score and other work, follow up at least 6 months after surgery with complete data, and voluntarily sign informed consent.
Exclusion criteria are as follows: (1) patients who do not meet the inclusion criteria; (2) patients with humerus greater tubercle fracture, severe glenohumeral joint degeneration, upper pelvis and lip injury requiring fixation, and acromioclavicular arthritis requiring resection of the distal clavicle; (3) patients who have mechanical impingement factors such as type III acromion patients; (4) patients with brachial plexus nerve injury and axillary nerve entrapment, affecting the shoulder joint function score; (5) those with large or huge rotator cuff tear (tear > 4 cm); (6) patients with complications affecting the joint, such as rheumatoid arthritis, bone tumor, traumatic arthritis, etc.; (7) those with serious primary diseases such as cardiovascular and cerebrovascular diseases and mental illnesses that cannot tolerate surgery; (8) those who have previously used anti-osteoporosis agents, other than vitamin D or calcium supplements; and (9) patients with incomplete follow-up data or unable to provide informed consent.
After screening, a total of 96 patients were included in the study and were divided into three groups based on their bone mineral density and postoperative treatment status. Group A included 33 patients with normal bone density. Group B consisted of 30 patients with osteoporosis who received postoperative intravenous zoledronic acid treatment. Group C had 33 patients with osteoporosis who did not receive zoledronic acid treatment after surgery. The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Xi’an Jiaotong University.
General data
The demographic and clinical characteristics of all three groups of patients were recorded, which included age, sex, side of injury, duration of the disease, body mass index (BMI), occupation, smoking history, bone mineral density (BMD), type of acromion, tear size in millimeters, acromial index (AI), and acromium-humeral distance (AHD). All patients underwent bone mineral density examination before surgery using dual energy X-ray absorptiometry, and their lumbar spine (L1-4) T scores were recorded. A T-score of < − 2.5 was defined as having “osteoporosis”.
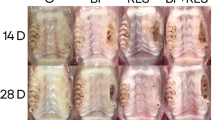
Surgical procedure and rehabilitation
All patients underwent surgery under general anesthesia and were positioned in lateral decubitus position. A conventional posterior approach was used, and an arthroscope was inserted to examine the rotator cuff tears. If dislocation or tearing of the long head of the bicep tendon was found, a biceps tenodesis was performed. The upper surface of the rotator cuff was meticulously explored to identify the tear. An anterolateral approach was then established, and the edges of the tear and its imprint were freshened. To repair the rotator cuff tear, two inner row absorbable anchors were screwed into the cartilage edge of the humeral head, while two outer row absorbable anchors were screwed into 1.5 cm below the outer edge of the greater tuberosity of the humerus. The double-row suture technique was used for the rotator cuff repair (Fig. 4).
Surgical diagram, preoperative MRI and intraoperative photos. (A) Two inner row anchors (Blue arrow) were screwed into the cartilage edge of the humeral head. (B) Reduction of torn rotator cuff tendon. (C) Two outer row anchors (Red arrow) were screwed into the 1.5 cm below the outer edge of the greater tuberosity of the humerus. (D) Preoperative MRI oblique coronal view, the yellow arrow is a ruptured supraspinatus tendon. (E) Subacromial space was explored arthroscopically to deal with acromial impingement, and the green arrow is the polished acromion. (F) The ruptured supraspinatus tendon was observed in the subacromial space (Yellow arrow). (G) The rotator cuff tear was repaired by double-row suture technique (Red arrow: the site of outer row anchor; Blue arrow: the site of inner row anchor). (H) The oblique coronal MRI of shoulder joint 6 months after surgery showed good healing of tendon bone (White arrow).
Postoperative treatment and follow-up
Negative pressure drainage tubes were removed within 24 h after surgery, and all patients were required to wear shoulder joint braces for 6 weeks to prevent excessive motion of the operated shoulder. The patients underwent passive motion training of the wrist, elbow, and shoulder joints from one to 6 weeks after surgery. Active joint mobility training was initiated from six to twelve weeks after surgery, and from twelve to sixteen weeks after surgery, weight training (0–3 kg) was added to active joint mobility training. At 16 weeks after the operation, shoulder joint endurance and strength training were gradually increased to improve the patient’s shoulder function.
In group B, all patients were administered 5 mg of zoledronic acid intravenously on the third postoperative day. Patients were closely monitored for any side effects, such as fever, myalgia, arthralgia, and headache. Ibuprofen suspension was given to alleviate any symptoms if needed. None of the patients in group C received ZA treatment after surgery, the main reasons included severe renal dysfunction of patients who could not tolerate this drug and the negligence of some doctors. However, both group B and group C patients received oral active vitamin D and calcium tablets as part of their basic treatment after being discharged from the hospital.
To evaluate the patients’ postoperative recovery, follow-up was conducted via telephone or outpatient visits. All patients underwent MRI review 6 months following surgery.
Clinical outcome assessment
To evaluate the clinical outcomes of the surgical intervention, all patients underwent assessments using the visual pain analogue scale (VAS), American Shoulder and Elbow Surgery Shoulder Function score (ASES), Health Survey Scale (UCLA), Constant Shoulder function Score (CSS), and shoulder range of motion (ROM) before surgery and 6 months after surgery. ROM was measured for forward flexion, abduction, and internal rotation. For internal rotation, the highest vertebral level that could be reached by the thumb tip was recorded, with vertebrae numbered sequentially from below the sacrum (0) to the fourth thoracic vertebra (14). Higher scores in this assessment indicated better range of motion. The VAS score ranged from 0 to 10, with higher scores indicating more severe pain. Scores for ASES (0–100 points), UCLA (0–45 points), and CSS (0–100 points) were proportional to shoulder joint function, with higher scores indicating better shoulder joint function. These assessments were conducted before surgery and at the 6-month follow-up appointment to evaluate the effectiveness of the surgery.
Imaging evaluation
To assess the status of the rotator cuff, all patients underwent an MRI before surgery and 6 months after surgery. The T2-weighted oblique coronal MRI scan of Sugaya was used to classify the integrity of the tendon47. Type I indicated that the repaired rotator cuff had sufficient thickness and a uniformly low signal on each image. Type II indicated sufficient thickness associated with partial areas of high signal intensity. Type III indicated insufficient thickness without discontinuity. Type IV showed slight discontinuities across multiple sections of the image, suggesting a small tear. Type V displayed major discontinuities in each image, suggesting medium or large tears. Retear was defined as types IV and V according to the Sugaya classification.
Retear patterns were further classified into two types based on T2-weighted oblique sagittal plane scanning images by Cho et al.48 Type I referred to the absence of residual tendon tissue at the greater tubercle, while type II indicated retear with the rotator cuff stump remaining at the greater tubercle.
Serological indexes evaluation
In group B and C, serum bone metabolism markers were measured at two time points—before surgery and 6 months after surgery. These markers included total Procollagen type 1 N-terminal Propeptide (P1NP), Bone alkaline phosphatase (B-LAP), Osteocalcin (OSTEOC), Serum Beta-Cross laps (βCross), and total 25 hydroxyvitamin D (T-25 OHD). The purpose of measuring these markers was to observe the effectiveness of zoledronic acid in the treatment of osteoporosis. The dynamic changes in serum bone metabolism markers between group B and C were compared at different time points to assess the effectiveness of the treatment.
Statistical methods
The data was analyzed using SPSS 23.0 statistical software. Shaumpire Wilk test was used to test for normal distribution, while Levene test was used to test for homogeneity of variance. Measurement data was expressed as mean (\(\overline{x}\) ± S), and analysis of variance (ANOVA) was used to compare differences among the three groups. In instances where the variance analysis difference was statistically significant, SNK-q (Student–Newman–Keuls) test was used for pairwise comparison between the groups. The t-test was used to compare scores of all indexes before and after surgery. Count data was represented as n (%) and analyzed through the Chi-square test. Statistical significance was set at P < 0.05.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jiang, Y. B. et al. Trabecular microstructure and surface changes in the greater tuberosity in rotator cuff tears. Skelet. Radiol. 31, 522–528. https://doi.org/10.1007/s00256-002-0536-6 (2002).
Cadet, E. R., Hsu, J. W., Levine, W. N., Bigliani, L. U. & Ahmad, C. S. The relationship between greater tuberosity osteopenia and the chronicity of rotator cuff tears. J. Shoulder Elbow Surg. 17, 73–77. https://doi.org/10.1016/j.jse.2007.04.017 (2008).
Boileau, P. et al. Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal?. J. Bone Jt. Surg. 87, 1229–1240. https://doi.org/10.2106/JBJS.D.02035 (2005).
Lafosse, L., Brozska, R., Toussaint, B. & Gobezie, R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J. Bone Jt. Surg. 89, 1533–1541. https://doi.org/10.2106/JBJS.F.00305 (2007).
Kim, Y. K., Jung, K. H., Kim, J. W., Kim, U. S. & Hwang, D. H. Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: A retrospective cohort study. J. Shoulder Elbow Surg. 27, 1012–1020. https://doi.org/10.1016/j.jse.2017.11.016 (2018).
Lee, J. H., Yoon, J. Y. & Lee, Y. B. The use of intravenous zoledronate may reduce retear rate after rotator cuff repair in older female patients with osteoporosis: A first in-human prospective study. J. Clin. Med. https://doi.org/10.3390/jcm11030836 (2022).
Atesok, K. et al. Augmentation of tendon-to-bone healing. J. Bone Jt. Surg. Am. 96, 513–521. https://doi.org/10.2106/jbjs.m.00009 (2014).
Chen, W. et al. Conditioned medium of human bone marrow-derived stem cells promotes tendon-bone healing of the rotator cuff in a rat model. Biomaterials. https://doi.org/10.1016/j.biomaterials.2021.120714 (2021).
Connor, D. E. et al. Therapeutic potential of exosomes in rotator cuff tendon healing. J. Bone Miner. Metab. 37, 759–767. https://doi.org/10.1007/s00774-019-01013-z (2019).
Abtahi, A. M., Granger, E. K. & Tashjian, R. Z. Factors affecting healing after arthroscopic rotator cuff repair. World J. Orthop. 6, 211–220. https://doi.org/10.5312/wjo.v6.i2.211 (2015).
Entezari, V. & Lazarus, M. Surgical considerations in managing osteoporosis, osteopenia, and vitamin D deficiency during arthroscopic rotator cuff repair. Orthop. Clin. N. Am. 50, 233–243. https://doi.org/10.1016/j.ocl.2018.10.006 (2019).
Hong, J. P. et al. Osteoporosis increases the risk of rotator cuff tears: A population-based cohort study. J. Bone Miner. Metab. 40, 348–356. https://doi.org/10.1007/s00774-021-01293-4 (2022).
Chung, S. W., Oh, J. H., Gong, H. S., Kim, J. Y. & Kim, S. H. Factors affecting rotator cuff healing after arthroscopic repair: Osteoporosis as one of the independent risk factors. Am. J. Sports Med. 39, 2099–2107. https://doi.org/10.1177/0363546511415659 (2011).
Ma, C. B. Editorial commentary: Aging and rotator cuff tears. Arthroscopy 35, 2321. https://doi.org/10.1016/j.arthro.2019.04.024 (2019).
Chen, X. et al. Effect of bone mineral density on rotator cuff tear: An osteoporotic rabbit model. PLoS One. https://doi.org/10.1371/journal.pone.0139384 (2015).
Genin, G. & Thomopoulos, S. The tendon-to-bone attachment: Unification through disarray. Nat. Mater. 16, 607–608. https://doi.org/10.1038/nmat4906 (2017).
Garnero, P., SornayRendu, E., Chapuy, M. C. & Delmas, P. D. Increased bone turnover in late postmenopausal women is a major determinant of osteoporosis. J. Bone Miner. Res. 11, 337–349. https://doi.org/10.1002/jbmr.5650110307 (1996).
Manolagas, S. C. From estrogen-centric to aging and oxidative stress: A revised perspective of the pathogenesis of osteoporosis. Endocr. Rev. 31, 266–300. https://doi.org/10.1210/er.2009-0024 (2010).
Plotkin, L. I., Bivi, N. & Bellido, T. A bisphosphonate that does not affect osteoclasts prevents osteoblast and osteocyte apoptosis and the loss of bone strength induced by glucocorticoids in mice. Bone 49, 122–127. https://doi.org/10.1016/j.bone.2010.08.011 (2011).
Dhillon, S. Zoledronic acid (Reclast(®), Aclasta(®)): A review in osteoporosis. Drugs 76, 1683–1697. https://doi.org/10.1007/s40265-016-0662-4 (2016).
Black, D. M. et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N. Engl. J. Med. 356, 1809–1822. https://doi.org/10.1056/NEJMoa067312 (2007).
Rodeo, S. A. et al. The effect of osteoclastic activity on tendon-to-bone healing: An experimental study in rabbits. J. Bone Jt. Surg. Am. 89, 2250–2259. https://doi.org/10.2106/JBJS.F.00409 (2007).
Xu, J. et al. The effect of antiosteoporosis therapy with risedronate on rotator cuff healing in an osteoporotic rat model. Am. J. Sports Med. 49, 2074–2084. https://doi.org/10.1177/03635465211011748 (2021).
Fagundes Belchior, G., Kirk, B., Pereira da Silva, E. A. & Duque, G. Osteosarcopenia: Beyond age-related muscle and bone loss. Eur. Geriatr. Med. 11, 715–724. https://doi.org/10.1007/s41999-020-00355-6 (2020).
Huang, C.-F., Shiao, M.-S. & Mao, T.-Y. Retrospective study of the effects of zoledronic acid on muscle mass in osteoporosis patients. Drug Des. Dev. Therapy 15, 3711–3715. https://doi.org/10.2147/dddt.s328858 (2021).
Löfman, O., Magnusson, P., Toss, G. & Larsson, L. Common biochemical markers of bone turnover predict future bone loss: A 5-year follow-up study. Clin. Chimica Acta Int. J. Clin. Chem. 356, 67–75. https://doi.org/10.1016/j.cccn.2004.12.014 (2005).
Holick, M. et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metabol. 96, 1911–1930. https://doi.org/10.1210/jc.2011-0385 (2011).
Hinsley, H., Ganderton, C., Arden, N. & Carr, A. Prevalence of rotator cuff tendon tears and symptoms in a Chingford general population cohort, and the resultant impact on UK health services: A cross-sectional observational study. BMJ Open 12, e059175. https://doi.org/10.1136/bmjopen-2021-059175 (2022).
Minagawa, H. et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J. Orthop. 10, 8–12. https://doi.org/10.1016/j.jor.2013.01.008 (2013).
Kirchhoff, C. et al. Assessment of bone quality within the tuberosities of the osteoporotic humeral head relevance for anchor positioning in rotator cuff repair. Am. J. Sports Med. 38, 564–569. https://doi.org/10.1177/0363546509354989 (2010).
Tingart, M. J., Apreleva, M., Lehtinen, J., Zurakowski, D. & Warner, J. J. P. Anchor design and bone mineral density affect the pull-out strength of suture anchors in rotator cuff repair: Which anchors are best to use in patients with low bone quality?. Am. J. Sports Med. 32, 1466–1473. https://doi.org/10.1177/0363546503262644 (2004).
Djurasovic, M. et al. Revision rotator cuff repair: Factors influencing results. JBJS 83, 1849–1855 (2001).
Park, J. & Kim, M. Changes in bone mineral density of the proximal humerus in Koreans: Suture anchor in rotator cuff repair. Orthopedics 27, 857–861. https://doi.org/10.3928/0147-7447-20040801-22 (2004).
Giori, N. J., Sohn, D. H., Mirza, F. M., Lindsey, D. P. & Lee, A. T. Bone cement improves suture anchor fixation. Clin. Orthop. Relat. Res.® 451, 236–241. https://doi.org/10.1097/01.blo.0000223984.67325.af (2006).
Milano, G. et al. Arthroscopic rotator cuff repair with metal and biodegradable suture anchors: A prospective randomized study. Arthrosc. J. Arthrosc. Relat. Surg. 26, S112–S119. https://doi.org/10.1016/j.arthro.2010.01.030 (2010).
Ma, R. et al. Effect of dynamic changes in anterior cruciate ligament in situ graft force on the biological healing response of the graft-tunnel interface. Am. J. Sports Med. 46, 915–923. https://doi.org/10.1177/0363546517745624 (2018).
Iannotti, J. P. et al. Time to failure after rotator cuff repair: A prospective imaging study. J. Bone Jt. Surg. Am. 95, 965–971. https://doi.org/10.2106/JBJS.L.00708 (2013).
Kluger, R., Bock, P., Mittlbock, M., Krampla, W. & Engel, A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am. J. Sports Med. 39, 2071–2081. https://doi.org/10.1177/0363546511406395 (2011).
Cancienne, J. M., Brockmeier, S. F., Kew, M. E., Deasey, M. J. & Werner, B. C. The association of osteoporosis and bisphosphonate use with revision shoulder surgery after rotator cuff repair. Arthroscopy 35, 2314–2320. https://doi.org/10.1016/j.arthro.2019.03.036 (2019).
Lui, P. P., Lee, Y. W., Mok, T. Y., Cheuk, Y. C. & Chan, K. M. Alendronate reduced peri-tunnel bone loss and enhanced tendon graft to bone tunnel healing in anterior cruciate ligament reconstruction. Eur. Cell Mater. 25, 78–96. https://doi.org/10.22203/ecm.v025a06 (2013).
Henriksen, K., Christiansen, C. & Karsdal, M. A. Role of biochemical markers in the management of osteoporosis. Clim. J. Int. Menopause Soc. 18(Suppl 2), 10–18. https://doi.org/10.3109/13697137.2015.1101256 (2015).
Uehara, M., Nakamura, Y., Suzuki, T., Nakano, M. & Takahashi, J. Efficacy and safety of oral ibandronate versus intravenous zoledronic acid on bone metabolism and bone mineral density in postmenopausal Japanese women with osteoporosis. J. Clin. Med. https://doi.org/10.3390/jcm10225420 (2021).
Tooth, C. et al. Risk factors of overuse shoulder injuries in overhead athletes: A systematic review. Sports Health Multidiscip. Approach 12, 478–487. https://doi.org/10.1177/1941738120931764 (2020).
Haque, A. & Pal Singh, H. Does structural integrity following rotator cuff repair affect functional outcomes and pain scores? A meta-analysis. Shoulder Elbow 10, 163–169. https://doi.org/10.1177/1758573217731548 (2018).
Paul, S., Goyal, T. & Yadav, A. K. Association between functional outcome scores and MRI-based structural integrity after rotator cuff repair: A prospective cohort study. Arch. Orthop. Trauma Surg. 142, 1117–1123. https://doi.org/10.1007/s00402-021-03938-5 (2022).
Lee, S. et al. Magnetic resonance rotator cuff fat fraction and its relationship with tendon tear severity and subject characteristics. J. Shoulder Elbow Surg. 24, 1442–1451. https://doi.org/10.1016/j.jse.2015.01.013 (2015).
Sugaya, H., Maeda, K., Matsuki, K. & Moriishi, J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J. Bone Jt. Surg. Am. 89, 953–960. https://doi.org/10.2106/jbjs.f.00512 (2007).
Cho, N. S., Yi, J. W., Lee, B. G. & Rhee, Y. G. Retear patterns after arthroscopic rotator cuff repair. Am. J. Sports Med. 38, 664–671. https://doi.org/10.1177/0363546509350081 (2009).
Acknowledgements
We would like to thank Image center from the First Affiliated Hospital of Xi 'an Jiaotong University and the Second Affiliated Hospital of Xi 'an Jiaotong University, for performing the Image data. We express our acknowledgement to Youdao Translation Company for their polish to this article.
Funding
The APC was funded by the National Natural Science Foundation of China (Grant No. 81772355).
Author information
Authors and Affiliations
Contributions
Conceptualization, Z.Y. and F.L.H.; methodology, Z.Y. and Z.Y.K.; validation, Z.Y., S.D.L. and G.Z.L.; formal analysis, S.D.L.; investigation, G.Z.L.; resources, S.Q.C. and W.J.Y.; data curation, Z.Y.K. and W.J.Y.; writing—original draft preparation, Z.Y. and L.D.; writing—review and editing, all authors; supervision, F.Z.L.; project administration, SZB and FLH; funding acquisition, F.L.H. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, Y., Shang, D., Zhang, Y. et al. The effectiveness of intravenous zoledronic acid in elderly patients with osteoporosis after rotator cuff repair: a retrospective study. Sci Rep 14, 20891 (2024). https://doi.org/10.1038/s41598-024-68246-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68246-5
Keywords
This article is cited by
-
The effect of applying anti-osteoporosis drugs on the rehabilitation of patients with rotator cuff tears after arthroscopic rotator cuff repair: a meta-analysis
Journal of Orthopaedic Surgery and Research (2025)
-
Challenges Posed by Osteoporosis in Arthroscopy and Sports Injury Management
Indian Journal of Orthopaedics (2025)