Abstract
The objective of this study was to evaluate the racial and ethnic disparities in delivery hospitalizations involving severe maternal morbidity (SMM) by location of residence and community income. We used the 2016 to 2019 Healthcare Cost and Utilization Project National Inpatient Sample. International Classification of Diseases, Tenth Revision, Clinical Modification codes were used to identify delivery hospitalizations with SMM. Using logistic regression models, we examined the association between race and ethnicity and delivery hospitalizations involving SMM. In adjusted analyses, the models were stratified by location of residence and community income and adjusted for patient and hospital characteristics. In rural areas, non-Hispanic Black women (AOR 1.50; 95% CI 1.25–1.79) and women of other races (AOR 1.32; 95% CI 1.03–1.69) had an increased odds of experiencing a delivery hospitalization involving SMM when compared to non-Hispanic White women. In micropolitan areas, non-Hispanic Black women (AOR 1.88; 95% CI 1.79–1.97), non-Hispanic Asian/Pacific Islander women (AOR 1.54; 95% CI 1.16–2.05), and women of other races (AOR 1.31; 95% CI 1.03–1.67) had an increased odds of experiencing a delivery hospitalization involving SMM when compared to non-Hispanic White women. Non-Hispanic Black women also had increased odds of experiencing a delivery hospitalization involving SMM in communities with the lowest income (quartile 1) (AOR 1.59; 95% CI 1.49–1.66), middle income (quartiles 2 and 3) (AOR 1.81; 95% CI 1.72–1.91), and highest income (AOR 2.09; 95% CI 1.90–2.29) when compared to non-Hispanic White women. We found that location of residence and community income are associated with racial and ethnic differences in SMM in the United States. These factors, outside of individual factors assessed in previous studies, provide a better understanding of some of the structural and systemic factors that may contribute to SMM.
Similar content being viewed by others
Introduction
The United States has some of the highest rates of maternal morbidity and mortality among high-income countries, a concern that has gained significant attention over the past decade due to the increased availability of data and research1,2,3,4. Between 2018 and 2021, the national maternal mortality rate nearly doubled, rising from 17.4 to 32.9 per 100,000 live births2. Severe maternal morbidities (SMM) have also increased, from 146.8 in 2008 to 179.8 per 100,000 hospital discharges in 20212. Alongside these increasing trends, significant racial and ethnic disparities exist. In 2021, Black and American Indian/Alaska Native women experienced the highest mortality rates, 64.5 and 97.5 per 100,000 live births, respectively2,5. Similar to maternal mortality, racial and ethnic disparities in SMM are persistent, with Black women experiencing SMM at rates that are significantly higher than White women6,7. Significant disparities in rates have also been identified for Asian/Pacific Islander women and Hispanic women6,7.
Racial and ethnic disparities in maternal health outcomes, including both SMM and maternal mortality, are influenced by a range of factors that are social, structural, medical, clinical care, and institutional6,8,9. These factors can play a role in whether women have access to respectful, quality, comprehensive, and culturally appropriate care9. Particularly, community-related factors, such as community income and location of residence (urbanicity/rurality), can play a role in whether women have access to maternal care resources such as obstetricians, nurse midwives, and other healthcare professionals. Those resources can be limited among rural communities and communities serving those of lower overall income9,10,11. Not having access to basic health care services during pregnancy can lead to delay in receiving care when needed the most. This delay in care can lead to complications that put pregnant women at an increased risk for SMM and maternal mortality. Examining disparities in severe maternal morbidity by community level factors can guide the development and implementation of prevention and care strategies tailored to specific communities and specific groups of pregnant women.
The purpose of this study was to examine the location of residence, community income, and their association with racial disparities in delivery hospitalizations involving severe maternal morbidity. Using data from a nationally representative sample of United States delivery hospitalizations, this study examined the association between racial and ethnic disparities in delivery hospitalizations involving severe maternal morbidity (SMM) by location of residence and community income.
Methods
Study data source
Using a cross-sectional study design, we analyzed data from the 2016 to 2019 National Inpatient Sample (NIS), developed for the Healthcare Cost and Utilization Project (HCUP). NIS is the largest, publicly available all-payer national inpatient care dataset in the United States. It is nationally representative of all community hospitals and contains a 20% stratified sample of all discharged patients across 47 states and the District of Columbia. The NIS is intended to develop national estimates rather than state-level estimates.
Study population
ICD-10-CM/PCS diagnosis codes and their diagnostic-related groups (DRGs) were used to identify the study population, which comprised of discharges with DRGs related to pregnancy, specifically to labor and delivery (Supplemental Tables 1 and 2). DRGs use a patient classification system that categorizes patients into groups that are clinically coherent and homogenous with respect to resources used. Each delivery hospitalization has one assigned DRG. Our study was reviewed by the institutional review board at the University of Georgia in Athens, Georgia, and was considered exempt because of the deidentified nature of the dataset.
Outcome and dependent measures
The primary outcome of interest of this study was an SMM ocurring during a delivery hospitalization. SMM during a delivery hospitalization was determined by the presence of at least one of the 21 conditions or procedures a pregnant woman may experience during a delivery hospitalization based on the United States Centers for Disease Control and Prevention’s 21 SMM indicators12. A delivery hospitalization could experience multiple indicators of SMM. However, to be consistent with previous studies, this variable was dichotomized into (1) delivery hospitalization with SMM and (2) delivery hospitalization without SMM13,14. One factor, blood transfusion, may not always reflect SMM in the absence of other factors. Because of this, blood transfusion was excluded from our SMM definition15.
Independent measures
The primary independent measure of this study was race and ethnicity. HCUP created a combined categorization of race and ethnicity16. Race and ethnicity were partitioned into the following categories: (1) Hispanic of any race, (2) non-Hispanic White, (3) non-Hispanic Black, (4) non-Hispanic Asian/Pacific Islander, and (5) non-Hispanic Other (including mixed race and American Indian and Alaska Native). Race and ethnicity were missing for 4% of the discharge records; only data with complete records of race/ethnicity were included in our analyses. Non-Hispanic White women were chosen as the reference group since it was the largest represented group. American Indian and Alaska Native women were combined with women of other races for analyses because there is limited reporting of the population in HCUP data.
This study stratified by community income (categorized in quartiles provided by HCUP) and location of residence (as rural, micropolitan, small metropolitan, and large metropolitan). Community income is based on the median household income of the patient’s zip code of residence16. Quartiles are defined so that the total United States population is evenly distributed. Cut-offs for the quartiles are determined annually using zip code demographic data. For this study, we combined quartile 2 and quartile 3 into a single quartile 2 and 3 (middle income) category because there was little difference in unadjusted SMM rates.
The location of residence was based on urban influence codes developed by the United States Department of Agriculture Economic Research Service16. Rural was defined as areas of less than 10,000 residents. Micropolitan include areas of 10,000 residents to 49,999 residents. Small metropolitan areas have from 50,000 residents to 999,999 residents. Large metropolitan area denote areas of at least 1 million residents.
Covariates
A group of covariates related to patient characteristics included maternal age and primary expected payer. Maternal age in years was categorized as (a) 12–19, (b) 20–24, (c) 25–34, and (d) 35–55. Primary expected payer was categorized into (a) Medicaid, (b) Private Insurance, (c) Self-pay or no charge, and (d) Other. Medicaid includes patients covered by fee-for-service and managed care Medicaid16. Private insurance includes commercial carriers, private health maintenance organizations (HMOs), and preferred provider organizations (PPOs)16. Self-pay or no charge includes an insurance status of self-pay and no charge16. Other includes workers compensation, TRICARE/CHAMPUS, CHAMPVA, Title V, and other government programs16.
Another group of covariates related to hospital characteristics included hospital region, hospital teaching status, and hospital ownership. Hospital region was categorized into (a) Northeast, (b) Midwest, (c) South, and (d) West based on the United States Census Bureau classification16. Hospital teaching status included non-teaching hospitals and teaching hospitals, and hospital ownership included government and private16. Teaching hospitals are hospitals that are members of the University Health System Consortium or the Council of Teaching Hospitals16.
Statistical analysis
We first examined the distribution of SMM by race and ethnicity. We calculated descriptive frequencies and percentages to examine the distribution of delivery hospitalizations with SMM by race and ethnicity for each patient characteristic, hospital characteristic, and community factor. We examined the association between race and ethnicity and delivery hospitalizations involving SMM using logistic regression. In adjusted analyses, the models were stratified by location of residence and community income and adjusted for patient and hospital characteristics. Each regression model adjusted for age group, primary expected payer, hospital region, hospital teaching status, and hospital ownership and estimated the odds of experiencing SMM by race and ethnicity for location of residence and community income. All analyses accounted for the complex sampling design of the NIS by weighting observations by their survey weights. Analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
Results
Among a total of 14,961,125 delivery hospitalizations between the years 2016 and 2019, 128,540 (1%) met the CDC definition of SMM and had a race and ethnicity classification. The prevalence of SMM was highest among non-Hispanic Black women at 1.49% followed by 0.92% among women of other races, 0.82% among Hispanic women, 0.79% among non-Hispanic Asian/Pacific Islander women, and 0.76% among non-Hispanic White women. Baseline patient, community, and hospital characteristics stratified by race and ethnicity are shown in Table 1. Of the deliveries involving SMM, 45% were among non-Hispanic White women, 25% were non-Hispanic Black women, 19% were Hispanic women, 5.50% were non-Hispanic Asian/Pacific Islander women, and 5.50% were among women of other races (Table 1).
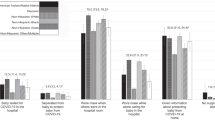
Figure 1 shows the adjusted regression models examining the racial and ethnic disparities in SMM by location of residence. In large metropolitan areas, non-Hispanic Black women had increased odds of experiencing SMM (AOR 1.88; 95% CI 1.79–1.97), being 88% more likely to experience a delivery hospitalization involving an SMM when compared to non-Hispanic White women. Also, in large metropolitan areas, women of other races were 12% more likely to experience a delivery hospitalization involving an SMM when compared to non-Hispanic White women (AOR 1.12; AOR 1.04–1.22). In small metropolitan areas, non-Hispanic Black women had increased odds of experiencing SMM (AOR 1.63; 95% CI 1.50–1.72) being 63% more likely to experience a delivery hospitalization involving a SMM when compared to non-Hispanic White women. In micropolitan areas, non-Hispanic Black women had increased odds of experiencing SMM (AOR 1.76; 95% CI 1.51–2.05) being 76% more likely to experience a delivery hospitalization involving an SMM compared to non-Hispanic White women. Women of other races residing in micropolitan areas were 31% more likely to experience a delivery hospitalization involving an SMM when compared to non-Hispanic White women (AOR 1.31; AOR 1.03–1.67). Also, in micropolitan areas, non-Hispanic Asian and Pacific Islander women had increased odds of experiencing SMM (AOR 1.54; 95% CI 1.16–2.05), being 54% more likely to experience a delivery hospitalization involving an SMM when compared to non-Hispanic White women. In rural areas, non-Hispanic Black women had increased odds of experiencing SMM (AOR 1.50; 95% CI 1.25–1.80) being 50% more likely to experience a delivery hospitalization involving a SMM when compared to non-Hispanic White women. Also, in rural areas, women of other races were 32% more likely to experience a delivery hospitalization involving a SMM when compared to non-Hispanic White women (AOR 1.32; AOR 1.03–1.69) (Fig. 1, Supplemental Table 3).
Adjusted coefficient plots for racial and ethnic disparities among delivery hospitalizations involving severe maternal morbidity by location of residence, 2016–2019. Each multivariable logistic regression model adjusted for age, primary expected payer, community income, hospital region, teaching status, and ownership of hospital.
Figure 2 shows the adjusted regression models examining the racial and ethnic disparities in SMM by community income. In communities with the lowest median household level income (Quartile 1), non-Hispanic Black women had increased odds of experiencing SMM (AOR 1.59; 95% CI 1.49–1.69) being 59% more likely to experience a delivery hospitalization involving a SMM when compared to non-Hispanic White women. In communities that contain the middle-income group for median household level income (Quartiles 2 and 3), non-Hispanic Black women had increased odds of experiencing SMM (AOR 1.81; 95% CI 1.72–1.91) being 81% more likely to experience a delivery hospitalization involving a SMM when compared to non-Hispanic White women. Also, in communities with the highest median household level income (Quartile 4), non-Hispanic Black women had increased odds of experiencing SMM (AOR 2.09; 95% CI 1.90–2.29) having over twice the odds of a delivery hospitalization involving SMM when compared to non-Hispanic White women. Women of other races were 25% more likely to experience a delivery hospitalization involving a SMM when compared to non-Hispanic White women (AOR 1.25; AOR 1.11–1.40) in communities with the highest median household level income as well (Fig. 2, Supplemental Table 4).
Adjusted coefficient plots for racial and ethnic disparities among delivery hospitalizations involving severe maternal morbidity by community income, 2016–2019. Each multivariable logistic regression model adjusted for age, primary expected payer, community income, hospital region, teaching status, and ownership of hospital.
Discussion
Overall, the prevalence of SMM in our study population was highest among non-Hispanic Black women at 1.49%, which is similar to other studies7,13. We found that there are significant racial and ethnic disparities among delivery hospitalizations involving SMM by community characteristics, particularly location of residence and community income.
For location of residence, there were significant racial and ethnic disparities in large metropolitan, small metropolitan, micropolitan, and rural areas. Results of this study show that non-Hispanic Black women and women of other races in rural areas were more likely to experience a delivery hospitalization involving SMM when compared to non-Hispanic White women. Also, for micropolitan areas, non-Hispanic Black women, women of other races, and non-Hispanic Asian/Pacific Islander women were more likely to experience a delivery hospitalization involving SMM when compared to non-Hispanic White women. It is well documented that rural Americans make up at least 15% to 20% of the United States population and face inequities that result in worse health care than that of urban and suburban residents. Rural areas have fewer physicians, have higher levels of poverty, and their remote locations contribute to a lack of access to care17,18. Also, rural areas face great challenges when they experience hospital closures. When hospitals or obstetric units close, rural and underserved areas lose the infrastructure that supports providers like obstetrician-gynecologists, specialists, and licensed midwives17,18. This means that pregnant women who live in rural areas may have less frequent prenatal and maternal care prior to delivery if the long travel distances to obtain care are prohibitive or costly17. Like rural areas, micropolitan communities also experience economic adversity and decreased equitable access to quality care that present challenges for maternal health17.
There were also significant disparities among residents in metropolitan areas (both small and large). Contrary to conventional thought, these results show that these racial and ethnic maternal health disparities are still observed in areas with better access to maternal care and maternal health outcomes.
There were also significant racial and ethnic disparities, regardless of community income. In communities with the lowest median income, middle median income, and highest median income, non-Hispanic Black women were more likely to experience a delivery hospitalization involving SMM when compared to non-Hispanic White women. This association was not observed for any of the other racial and ethnic groups. As community income increased, the odds in having a delivery hospitalization with SMM increased. So, regardless of community income, non-Hispanic Black women were more likely to experience a delivery hospitalization involving SMM.
Healthcare settings in the United States can be sites of racism and discrimination for some women and structural racism has been acknowledged as a contributor to adverse health outcomes19,21,21. Structural racism is the ways in which some societies foster racial discrimination through policies and processes that impact the distribution of resources and create differential opportunities by race22,23. To tackle racial and ethnic disparities in SMM, a multi-faceted approach to address racism (including structural racism) and discrimination will be needed. Understanding how racism and discrimination plays a role in SMM can help guide the development and implementation of policy and program interventions that address racial disparities during delivery admissions.
Investing in healthcare infrastructure in rural and low-income communities could help in addressing racial and ethnic disparities in SMM. Although this study did not assess the quality of care available, rather just community characteristics, being able to provide risk-appropriate maternal care through telemedicine, virtual visits, or remote patient monitoring could help provide quality services to those with limited access. Also, ensuring that women who experience complications or with high-risk conditions are transferred to facilities that can provide specialty services, could help limit the occurrence of SMM during a delivery hospitalization for those in rural or micropolitan with barriers to accessing resources. Also, funding to expand the obstetric care workforce to support doula and midwifery programs can increase access to culturally appropriate care24,25.
Conclusion
Our study shows that there are stark racial and ethnic disparities in SMM by community income and location of residence, suggesting that there are systemic and structural factors that are associated with SMM. Even in instances when there could be adequate resources and access to quality care, the disparities within minority racial and ethnic groups still persist at alarming rates. Therefore, these disparities are unlikely to be associated with the characteristics of the patient but rather a characteristic of the care they receive.
Our study should be interpreted considering its limitations. First, all diagnoses are based on ICD-10-CM/PCS codes from hospital discharge data. Since records in this database are de-identified, it is not possible to confirm diagnoses, so misclassification is possible due to some cases being missed or miscoded. Also, given the nature of hospital discharge data, other important variables such maternal education or readmission were not captured. Since follow-up beyond the delivery hospitalization was not available, postpartum outcomes after the delivery hospitalization were not available.
HCUP does not include Indian Health Service facility data. Although over 75% of Native American delivers occur outside of these facilities, Indian health facilities may refer more complex deliveries to other hospitals included in HCUP19. In addition, HCUP data may undercount or misclassify Native American women due to missing race and ethnicity data. Because of this, Native American women estimates were included in the other race and ethnicity category19. We were also missing race/ethnicity for 4% of the hospital discharges; therefore, these records were not included in the analysis. Since individual-level income data are unavailable, community income was used as a proxy for individual-level income.
Despite these limitations, our study has several strengths. The primary strength of this study is that the NIS is the largest all-payer national inpatient care data set for the United States. This dataset offers a unique opportunity to investigate SMM in a nationally representative sample of women in the United States. This large sample also allows for the adjustment of multiple potential confounders in logistic regression models and to examine these associations over various racial and ethnic groups in the United States. Using the United States Centers for Disease Control and Prevention’s method to identify severe maternal morbidity using ICD-10-CM/PCS codes is another strength. This method has been validated by other studies.
Although racial inequities in SMM are well documented in the literature, these inequities continue to persist. In addition to documenting and reporting the trends and associations, next steps should involve translating data into action for new interventions or examining the impact of existing interventions. Future studies are also needed to identify the root causes of inequities that exist in delivery hospitalizations involving SMM. It is critical to continue to understand why racial and ethnic minorities experience poorer maternal health outcomes when compared to other racial and ethnic groups regardless of location, resources, hospital location or type, and socio-economic status. Future studies should examine hospital quality of care and access to risk-appropriate maternal care for these populations.
Data availability
The data used for this study is publicly available and can be purchased from the Healthcare Cost and Utilization Project (HCUP) website. Complete database availability and pricing information are included in the online HCUP Central Distributor Database Catalog https://www.distributor.hcup-us.ahrq.gov/Databases.aspx. The datasets analyzed during the current study can be made available from the corresponding author on reasonable request.
References
Declercq, E. & Zaphyrin, L. Severe maternal morbidity in the United States: A primer. Commonwealth Fund https://doi.org/10.26099/r43h-vh76 (2021).
Fink, D. A. et al. Trends in maternal mortality and severe maternal morbidity during delivery-related hospitalizations in the United States, 2008 to 2021. JAMA Netw Open. 6(6), e2317641. https://doi.org/10.1001/jamanetworkopen.2023.17641 (2023).
Gunja, M. Z., Gumas, E. D. & Masitha, R. Insights into the U.S. maternal mortality crisis: An international comparison. Commonwealth Fund https://doi.org/10.26099/cthn-st75 (2024).
Tikkanen, R., Gunja, M. Z., Fitzgerald, M. & Zephyrin, L. Maternal mortality and maternity care in the United States. Commonwealth Fund https://doi.org/10.26099/411v-9255 (2020).
U. S. Department of Health and Human Services. Reduce Maternal Deaths. Healthy People 2030 https://health.gov/healthypeople/objectives-and-data/browse-objectives/pregnancy-and-childbirth/reduce-maternal-deaths-mich-04
Creanga, A. A., Bateman, B. T., Kuklina, E. V. & Callaghan, W. M. Racial and ethnic disparities in severe maternal morbidity: A multistate analysis, 2008–2010. Am. J. Obstet. Gynecol. 210(5), 435.e1–8. https://doi.org/10.1016/j.ajog.2013.11.039 (2014).
Leonard, S. A., Main, E. K., Scott, K. A., Profit, J. & Carmichael, S. L. Racial and ethnic disparities in severe maternal morbidity prevalence and trends. Ann. Epidemiol. 33, 30–36. https://doi.org/10.1016/j.annepidem.2019.02.007 (2019).
Bryant, A. et al. The association of maternal race and ethnicity and the risk of postpartum hemorrhage. Anesth. Analg. 115(5), 1127–1136. https://doi.org/10.1213/ANE.0b013e3182691e62 (2012).
Crear-Perry, J. et al. Social and structural determinants of health inequities in maternal health. J. Womens Health (Larchmt) 30(2), 230–235. https://doi.org/10.1089/jwh.2020.8882 (2021).
Larson, C. P. Poverty during pregnancy: Its effects on child health outcomes. Paediatr. Child Health 12(8), 673–677. https://doi.org/10.1093/pch/12.8.673 (2007).
Merkt, P. T. et al. Urban-rural differences in pregnancy-related deaths, United States, 2011–2016. Am. J. Obstet. Gynecol. 225(2), 183.e1-183.e16. https://doi.org/10.1016/j.ajog.2021.02.028 (2021).
Centers for Disease Control and Prevention. How Does CDC Identify Severe Maternal Morbidity? https://www.cdc.gov/maternal-infant-health/php/severe-maternal-morbidity/icd.html
Fingar, K. R., Hambrick, M. M., Heslin, K. C., Moore, J. E. Trends and disparities in delivery hospitalizations involving severe maternal morbidity, 2006–2015: Statistical brief #243, in Healthcare Cost and Utilization Project (HCUP) Statistical Briefs (Agency for Healthcare Research and Quality, 2006).
Brown, C. C., Adams, C. E., George, K. E. & Moore, J. E. Mental health conditions increase severe maternal morbidity By 50 percent and cost $102 million yearly in the United States. Health Aff. (Millwood) 40(10), 1575–1584. https://doi.org/10.1377/hlthaff.2021.00759 (2021).
Kuklina, E. V. et al. Ranked severe maternal morbidity index for population-level surveillance at delivery hospitalization based on hospital discharge data. PLoS One. 18(11), e0294140. https://doi.org/10.1371/journal.pone.0294140 (2023).
U.S Agency for Healthcare Research and Quality (AHRQ). NIS Description of Data Elements (2023). https://hcup-us.ahrq.gov/db/nation/nis/nisdde.jsp
Novak, N. L. et al. Health equity in midsize rural communities: Challenges and opportunities in a changing rural America. Am. J. Public Health 110(9), 1342–1343. https://doi.org/10.2105/ajph.2020.305824 (2020).
Warshaw, R. Health Disparities Affect Millions in Rural U.S. Communities https://www.aamc.org/news-insights/health-disparities-affect-millions-rural-us-communities
Williams, D. R. & Rucker, T. D. Understanding and addressing racial disparities in health care. Health Care Finance Rev. Summer 21(4), 75–90 (2000).
Groos, M., Wallace, M., Hardeman, R. & Theall, K. P. Measuring inequity: A systematic review of methods used to quantify structural racism. J. Health Disparities Res. Pract. 11(2), 13 (2018).
Sim, W. et al. The perspectives of health professionals and patients on racism in healthcare: A qualitative systematic review. PLoS One 16(8), e0255936. https://doi.org/10.1371/journal.pone.0255936 (2021).
Bailey, Z. D., Feldman, J. M. & Bassett, M. T. How structural racism works - Racist policies as a root cause of U.S. racial health inequities. N. Engl. J. Med. 384(8), 768–773. https://doi.org/10.1056/NEJMms2025396 (2021).
American Medical Association. What is structural racism? Health Equity https://www.ama-assn.org/delivering-care/health-equity/what-structural-racism
Fontenot, J., Brigance, C., Lucas, R. & Stoneburner, A. Navigating geographical disparities: Access to obstetric hospitals in maternity care deserts and across the United States. BMC Pregnancy Childbirth 24(1), 350. https://doi.org/10.1186/s12884-024-06535-7 (2024).
Stoll, K., Titoria, R., Turner, M., Jones, A. & Butska, L. Perinatal outcomes of midwife-led care, stratified by medical risk: A retrospective cohort study from British Columbia (2008–2018). Cmaj 195(8), E292-e299. https://doi.org/10.1503/cmaj.220453 (2023).
Author information
Authors and Affiliations
Contributions
M.D.C., N.D.H.G., S.L.R., and J.F.C. contributed to the analysis, interpretation of the data, and drafting of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Claridy, M.D., Hernandez-Green, N., Rathbun, S.L. et al. Community level factors and racial inequities in delivery hospitalizations involving severe maternal morbidity in the United States, 2016–2019. Sci Rep 14, 19297 (2024). https://doi.org/10.1038/s41598-024-70130-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70130-1
Keywords
This article is cited by
-
The impact of social determinants of health on infant and maternal health using a reproductive justice lens
BMC Pregnancy and Childbirth (2025)
-
Championing maternal health and reducing maternal mortality: a global multidisciplinary imperative
Scientific Reports (2025)
-
Structural Racism, Geographies of Opportunity, and Maternal Health Inequities: A Dynamic Conceptual Framework
Journal of Racial and Ethnic Health Disparities (2025)