Abstract
This randomized clinical trial aims to evaluate cryotherapy as a therapeutic option for pain prevention after endodontic treatment with and without foraminal enlargement, in patients with asymptomatic apical periodontitis.120 teeth of patients with preoperative Visual Analogue Scale score indicating zero were treated. Specimens were randomly allocated into 4 groups: Control, Cryotherapy (ICT), Foraminal Enlargement (FE), and Cryotherapy and Foraminal Enlargement (ICT + FE). Working length was determined with an Electronic Apex Locator (EAL). Cryotherapy groups passed through a final irrigation protocol using 20 ml (2.5 ℃) of cold saline solution delivered at working length for 5 min. In FE groups a #40 K-file was used up to the 0.0 mark on the EAL display. Obturation was performed and postoperative pain was checked at 6, 12, 24, 48, and 72 h and 7 days after endodontic treatment.All experimental groups showed an increase in the level of postoperative pain, which started to decrease after 12 h. Foraminal enlargement caused a statistically significant increase in postoperativepain compared to ICT and control groups within the first 6 h (p < 0.05). Cryotherapy did not influence postoperative pain, regardless of whether or not foraminal enlargement was performed.
Similar content being viewed by others
Introduction
Postoperative pain is a frequent consequence of root canal treatment, occurring in 3–58% cases1,2,3,4. Incessant or increased postoperative pain can cause great stress and discomfort for patients. Pain after root canal treatment originates from the apical third region due to the presence of dentin debris, irritant solutions, or microorganisms that may be pushed out from the root canal into periapical tissues during chemo mechanical preparation4,5.
Foraminal enlargement (FE) is an intentional and mechanical apical preparation technique that involves using a larger caliber instrument at the level of or slightly beyond the apical foramen to increase its diameter6,7. This approach can overcome the potential limits of root canal irrigation allowing a better penetration in the apical area, favoring root canal disinfection to reduce the microbial contingent to levels even more favorable to periapical repair6,8,9.
On the other hand studies suggests that the use of patency instruments and a larger preparation size might result in an unnecessary removal of dentin, leading to an apical transportation8,9, extrusion of debris, irrigant and/or sealer during instrumentation in comparison with the amount that would be extruded if instrumented up to 1 mm short from the apical foramen6.All these factors can induce an inflammatory response at the periapical level and increase the intensity of postoperative pain episodes2,8,9,10,11.
Pain assessment is important during clinical work and to evaluate treatment outcomes12. The visual analogue scale (VAS) is a simple, fast, and efficient pain index, providing a one-dimensional measurement for patients’ perception of pain intensity13. It consists of a 10 cm long horizontal line, with each centimeter being numbered according to the following criteria:0, no pain; 1–3, mild pain; 4–6, moderate pain; 7–9, severe pain; and 10, the worst pain experienced14.
Despite careful treatment, an acute exacerbation of pain might be experienced after endodontic treatment15,16. According to Ehrmann17, an increase of 2 points or more in the VAS may lead to the pain transitioning from mild to moderate or severe. These flare-ups may be caused by local tissue changes, immunological phenomena, and psychological and microbial factors15,18. Alacam and Tinaz19 did not report any statistical difference in the incidence of flare-up between patients receiving medication (analgesic), placebo, or no medication. Furthermore, Ehrmann et al. analyzed 195 cases and did not find any difference in the flare-up rates in the first 24 h after endodontic treatment between patients using Ledermix, calcium hydroxide, and no intracanal dressing17.
Non-steroidal anti-inflammatory drugs or corticosteroids are usually indicated for reducing pain or reversing the patient’s inflammatory condition after root canal treatment. However, despite being relatively safe, they can cause gastrointestinal intolerance and kidney, liver, or respiratory damage20,21.
Cryotherapy has been described since the times of Hippocrates, who recommends the use of ice locally or systemically for therapeutic reasons22. Since 1960 it has been used in different fields of medicine such as orthopedics, physiotherapy, traumatology, neurology and dental surgery22,23. There are 3 physiological tissue responses after the application of cold: decrease in local blood flow, inhibition of neural receptors in the skin and subcutaneous tissues, and a decrease in metabolic activity23,24. Cryotherapy has also been reported to be effective at decreasing edema, pain, muscle spasms, connective tissue distension, hemorrhage, inflammation, and nerve conductivity14,25. In relation to contraindications, there are some documented in the literature, such as Raynaud’s disease and hemoglobinuria21. It is also controversial in patients with certain systemic diseases or cardiac conditions, such as arrhythmia, angina pectoris, and hypertension, because vasoconstriction can elevate blood pressure21.
Vera et al. (2015) proposed an “Intracanal Cryotherapy” (ICT) irrigation protocol using cold saline solution at 2.5°℃ which demonstrated the ability to reduce the temperature of the external root surface by up to 10 ℃ for a period of 5 min24. Intracanal cryotherapy protocol is a local therapy option free of pharmacological side effect21,24. It has a positive effect in cases of swelling, pain, and inflammation due to a decrease in blood flow, tissue metabolism, and sensory activity22,26,27.
Recent studies have focused on evaluating the effect of ICT in symptomatic patients who are already experiencing pain22. In a study conducted by Vera et al.21 on patients with a pain level of 8–10 on the VAS, ICT reduced postoperative pain in cases of necrotic pulp and symptomatic apical periodontitis. A high preoperative pain level may also explain the high postoperative pain relief21. According to the results of CT studies, it is associated mainly with pain relief but not pain prevention; thus, it may result in reduced consumption of medications and side effects21,22,23.
Considering the positive effect of ICT on pain relief in symptomatic cases28, this study aimed to evaluate cryotherapy as a therapeutic option for pain prevention after endodontic treatment in patients with and without FE in patients with asymptomatic apical periodontitis. The null hypothesis is that ICT does not interfere in the prevention of postoperative pain in asymptomatic apical periodontitis.
Materials and methods
This prospective randomized clinical trial was approved by the local ethics committee (protocol 5.024.031) and registered with the International Standard Randomized Controlled Trial (number 16939754; Date 09/28/2022; https://doi.org/https://doi.org/10.1186/ISRCTN16939754). The study is being reported following the 2010 CONSORT statement and checklist (www.consort-statement.org/). One endodontist experienced in the techniques, materials, and technologies analyzed participated in the study.
Inclusion and exclusion criteria
The study population was selected from a sample of Brazilian patients referred to a dental clinic for endodontic treatment. Only one tooth per patient was included in the trial. All patients were informed about the study design and objectives, and written informed consent was obtained before treatment initiation. Patient sex, age, teeth, and arch locations were recorded. The inclusion criteria were as follows: age ≥ 18 years; single-rooted teeth diagnosed with pulp necrosis with asymptomatic apical periodontitis and digital radiographic evidence of apical periodontitis (minimum 2 × 2 mm). Pulp vitality was assessed before treatment initiation using Endo Ice Spray (Maquira, Maringá, Brazil).Among the exclusion criteria were considered individuals with acute apical pain, those with chronic use of corticosteroids, analgesics, or antibiotics, those with systemic disease(s), allergic reactions, pregnancy, those who underwent previous root canal treatment, vital teeth, anatomical foramen of tooth (assessed during root canal treatment) with a diameter > #20 K-type instrument or < of a #10 K-type instrument, teeth with root resorption that compromised the apical region and root canals with extreme curvature (> 30°).Those patients who stopped responding or who responded inadequately were also excluded.
The Consort diagram (Fig. 1) summarizes the processes carried out in this study. A total of 316 patients were evaluated between January 2021 and December 2022. A hundred and eighty patients were excluded because they did not meet the inclusion criteria, thereby, leaving a total of 136 patients. All patients fulfilling the inclusion criteria who agreed to participate in the study received a consecutive number. This number was previously generated as part of a random sequence between 1 and 136 (www.random.org) and assigned to a control group or three experimental groups. An assistant checked the list to verify the group to which that patient would be assigned and shared the result with the clinician only after the shaping procedure. All participants received a questionnaire based on VAS to record their assessment of their pain at treatment and 6 h, 12 h, 24 h, 48 h, 72 h, and 7 days post-treatment; the scores were recorded from 0 to 10, where 0 and 10 correspond to complete absence of pain and unbearable pain, respectively18. The number of patients with a pain level between 0 and 10 in the period from 6 h to 7 days was recorded. Only patients with preoperative scores of 0 were included.
Endodontic treatment
Endodontic treatment was performed by a single endodontic specialist during a single visit. Patients were anesthetized using 1.8 mL of 2% mepivacaine with 1:100,000 epinephrine. This technique involves buccal infiltration of the maxillary and mandibular teeth. A supplemental injection of local anesthetic, via buccal, palatal, or lingual infiltration, was administered when required. The teeth were isolated with a rubber dam, and cavity access was performed using a diamond round bur at highspeed. The root canals were pre-flared using a ProTaper SX (Dentsply Sirona, Ballaigues, Switzerland). Thecanals were explored using an instrument (type K #10). The working length (WL) was determined using an electronic apex locator (“Root ZX II”; J Morita, Tokyo, Japan) and a K-type instrument with the most suitable diameter for the anatomy of the canal. The WL was set 1 mm short of the 0.0 mark on the locator display. Root canal preparation was performed using a Reciproc R50 (VDW, Munich, Germany) instrument (50.05) mounted on a Smart plus motor (Dentsply Sirona, Ballaigues, Switzerland). The canals were irrigated with 15 ml of 2.5% sodium hypochlorite. Debris on the instrument was removed using gauze soaked in 70% alcohol after every three pecking movements.
Groups
FE group
After reaching the WL with the reciprocating instrument, a #40 K file was used to prepare the canal up to the 0.0 mark on the locator display in the patients from this group. Despite the final preparation, the canal remained obturated in the pre-established WL.
ICT group
Patients assigned to this group received a final irrigation of 20 ml cold sterile saline solution (2.5°℃) at the WL through a sterile cold 28-gauge microcannula attached to a negative pressure irrigation system “EndoVac” (Kerr Endo, Orange Country, CA) for 5 min21. Both the saline solution and microcannulas were stored in a calibrated refrigerator at 2.5°℃ until used21,24.
ICT + FE group
The patients in this group were treated following the same protocol as group “FE”. Additionally, an ICT group protocol was applied.
Control
Non final ICT irrigation protocol or FE was performed.
In all groups, a single round of irrigation was performed in each root canal using 5 mL of 17% ethylenediaminetetraacetic acid (EDTA), which was gently delivered 1 mm from the WL as the final irrigant and maintained intracanally for 1 min. For ICT and ICT + FE groups, this EDTA irrigation was performed before the cold saline application. All canals were dried with sterile paper points, followed by obturating by a matching single cone (Reciproc, VDW, Germany) and AH Plus sealer (Dentsply Sirona, Ballaigues, Switzerland). The access cavity was temporarily sealed with glass ionomer cement (FGM; Joinvile, SC, Brazil). Obturation quality was assessed by an intraoral periapical radiograph to ensure pre-established working length was maintained.
The patients were informed about the possibility of experiencing pain in the following days and were given a questionnaire, with six VASs included, to take home. They were instructed to record their pain level after 6 h, 12 h, 24 h, 48 h, 72 h, and 7 days on the VAS and were also contacted by phone at each time interval as a reminder to complete the VAS data. Patients were also instructed to contact the investigators in a case of severe pain so they will be prescribed with 400 mg Ibuprofen which would also be recorded in the questionnaire22,29.
Statistical analysis
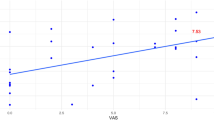
A sample size calculation was performed using the G*Power 3.1 software (Heinrich-Heine, Dusseldorf, Germany), with an alpha error of 0.05 and a beta power of 0.95. Sample size calculation estimated the desired size at 30 individuals per group. This research was determined by conducting a pilot study with 30 patients, the power effect size for a pilot study was 88, 30%. The sample was adjusted to account for approximately 10% of patients who may not respond the VAS forms. Therefore, the 136 patients who met the inclusion criteria were invited to participate in this randomized clinical trial. 16 patients were lost to follow up (patient did not come to follow up session). A total of 120 patients were analyzed. The Kolmogorov-Smirnov test was performed to verify whether the data were normally distributed. As the data referring to the level of pain were not homogeneous, the Kruskal-Walli’s test was used to compare the VAS scores between protocols at different timepoints of the study (P = 0.05). Dunn’s test for pair wise comparisons was performed for patients with a statistically significant difference within moments. The Friedman Test was performed to assess the differences between different moments within each protocol, and the confidence interval was set at 95% for the tests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This prospective randomized clinical trial was approved by the local ethics committee (protocol 5.024.031) and registered with the International Standard Randomized Controlled Trial (number 16939754).
Consent to participate
All participants were informed by word and in writing about the study and the investigations and had to give their verbal and written consent to participate.
Results
According to the metric analysis of variance the mean age of the patients was 46.71 (16.85) for the female patients and 43.82 (13.92) years for the male patients, with no statistical difference between the groups (P˃0.05). The age range was 18–65 years. The chi-squared test indicated no association between the level of postoperative pain among the 4 groups and sex, age and location range (P˃0.05) Table 1. Among the teeth treated, 30% (n = 36) were incisors, 8.33% (n = 10) canines, and 61.66% (n = 74) premolars.
Table 2 presents the descriptive differences (mean and standard deviation) between the pre and postoperative VAS pain scores according to different protocols and time intervals. A statistically significant difference was observed between protocols in the first 6 h (P < 0.05). In order to determine the protocols that differed from each other, Dunn’s test showed a statistically significant difference between the control and enlarged experimental groups as well as between the cryotherapy and enlarged groups in the 6 h interval. A total of 30% patients in the FE group experienced an increase in pain levels in the first 12 h. Despite this result, no patient related any analgesic intake during this trial.
Discussion
Management of postoperative pain in endodontics is usually performed using different pharmacological strategies, including non-steroidal anti-inflammatory medication (NSAIDs) and corticosteroids30,31. A systematic review and meta-analysis evaluate the efficacy of corticosteroids in postoperative endodontics. The study concluded that corticosteroids might reduce the incidence of postoperative pain up to 24 h32 On the contrary, the use of corticosteroids can result in toxicity due to abrupt suspension of the drug administration or continuous use of supraphysiological doses. Furthermore, a risk of gastrointestinal bleeding due to the appearance of a peptic ulcer exists, especially in patients consuming acetylsalicylic acid33.
The goal of this randomized, controlled, prospective clinical trial study was to assess the effect of ICT after endodontic treatment and evaluate its viability as an adjuvant for the prevention of postoperative pain. It is an economical and accessible resource that does not have as many contraindications or risks of side effects as NSAIDs and corticosteroids22.
Vera et al. reported a reduction in postoperative pain levels with cryotherapy and the need for medication in patients with necrotic pulp and symptomatic apical periodontitis with severe pain (VAS 8-10)21. In addition, a study performed by Gundogdu et al. on patients with vital pulp registering a VAS score > 6 showed a significant reduction in postoperative pain levels in the first 24 h after endodontic treatment22. This suggests that patients who have already experienced moderate or severe pain are more likely to experience a reduction in pain.
Although the pain may become severe in single-visit treatments, the flare-up rate in non-vital teeth after single-visit treatments is the same as that after multi-visit treatments34. In this study, procedures on all patients were performed in a single visit. Similar to the results of the study by Ehrmann et al.17, none of the cases in this study presented flare-ups. The results showed that most cases of increased sensitivity after root canal treatment occurred in the FE groups either with or without ICT. Although there was no statistically significant difference, FE without ICT involved in the highest pain scores during the analyzed period (6–72 h). The direct effect of ICT on preventing postoperative pain could not be established, even with FE. These results suggest that inflammation severity of the periradicular tissue caused by FE is not statistically significant when compared with ICT + FE, but it could be clinically relevant because the values of ICT + FE were less than that of FE group for all the times analyzed.
In contrast to other studies that used teeth with morphological variations for evaluating postoperative pain3,21,22, our study only included single root teeth to prevent any variation due to anatomical differences, especially in FE cases. This criterion for standardizing the anatomy is important, as FE did not interfere with postoperative pain levels after the first 12 h, and the pain remained mild for up to 72 h.
De Freitas et al.35 reported an increase in postoperative pain levels and the need for painkillers in the first 24 h after treatment in patients treated with FE. Similarly, a study by Yailali et al.7 stated that FE caused more pain after 48 h in patients with pulp necrosis. De Freitaset al. and Yailaliet al. used files up to a size of 25/07 or 40/05 in their studies, which are smaller than the R50 (50/05) files used in our study. However, the pain score for the FE group in our study was significantly higher only in the first 6 h after treatment. This result might be explained by the obturation length used in both studies, which was performed at the 0.0 display mark of the electronic apex locator. Obturation performed over the apical constriction with FE is expected to result in a higher rate of apical extrusion of the obturation material, which may lead to a severe inflammatory reaction in periapical tissues36.
In this study, although the WL preparation was also set in the 0.0 EAL display mark, the obturation remained 1 mm short from the 0.0 mark in order to have better control in relation to the extrusion factors found in the FE. For irrigation, a negative pressure system, such as an EndoVac, is an effective method for delivering irrigants into the apical third of the canal system, reducing the risk of irritant extrusion37.
Depending on the intensity and duration of the inflammatory events, caused by bacteria, trauma (foraminal enlargement) or both conditions, the apical periodontitis may develop an acute character. The morphological changes characterizing acute apical periodontitis, hyperemia, vascular congestion, edema, extravasation of neutrophils and monocytes and limited bone resorption, involve the apical periodontal ligament and the neighboring spongiosa38. The mechanism of action expected from the ICT is that it could represent a positive effect to prevent cases of swelling and inflammation due to a decrease in blood flow, tissue metabolism, and sensory activity22,26,27.
ICT during endodontic treatment is a simple and cheap supplementary method that decreases tissue temperature to minimize postoperative pain. Decreased vascular permeability is a key factor for reducing the amount of fluid leaking into the periradicular tissue as exudate or transudate, thereby reducing tissue edema and swelling, which commonly occurs in periapical tissue after chemomechanical preparation21.
For a clinical decision, the ICT may reduce postoperative pain in teeth with symptomatic apical periodontitis21,22, on the other hand in this study, for asymptomatic apical periodontitis, ICT as a therapeutic option for pain preventiondoes not play an important role, regardless of whether or not foraminal enlargement was performed.
One limitation of clinical studies that evaluate postoperative pain is the subjectivity of the assessment, however, in this study the patients were instructed to record the pain levels on the VAS and were also contacted by phone at each time interval as a reminder to complete the VAS data The different teeth used (incisors, canines and premolars) could be a limitation too, despite, in this study, the chi-square test indicated that regarding the level of postoperative pain in the four groups there was no association in gender, age and location range. Other limitation of this study was not using normal saline irrigation at room temperature for final irrigation in the control group. We preferred to simulate a clinical routine, without saline irrigation at room temperature, mainly to compare the results with the enlargement foramen group.
To the best of our knowledge, this is the first study to investigate postoperative endodontic pain, cryotherapy, and FE. Clinically, ICT does not have a positive effect on preventing postoperative pain. In endodontic practice, the protocol involving FE does not cause an increase in postoperative pain, suggesting that performing each clinical step with maximum precision is more important than using a single isolated procedure for preventing postoperative pain.
Data availability
All datasets used and analyzed in this study are available from the corresponding author on request. The data analyzed in this study was included as Supplementary Information.
References
Sathorn, C., Parashos, P. & Messer, H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment: A systematic review. Int. Endod. J. 41, 91–99 (2008).
Silva, E. J., Menaged, K., Ajuz, N., Monteiro, M. R. & de Souza Countinho-Filho, T. Postoperative pain after foraminal enlargement in anterior teeth with necrosis and apical periodontitis: A prospective and randomized clinical trial. J. Endod. 39(2), 173–176 (2013).
Al-Nahlawi, T., Hatab, T. A., Alrazak, M. A. & Al-Abdullah, A. Effect of intracanal cryotherapy and negative irrigation technique on post endodontic pain. J. Contemp. Dent. Pract. 17(12), 990–996 (2016).
Solomon, R. V., Paneeru, S. P., Swetha, C. & Yatham, R. Comparative evaluation of effect of intracanal cryotherapy and corticosteroid solution on post endodontic pain in single visit root canal treatment. J. Clin. Exp. Dent. 16(3), 250–256 (2024).
Tinaz, A. C., Alacam, T., Uzun, O., Maden, M. & Kayaoglu, G. The effect of disruption of apical constriction on periapical extrusion. J. Endod. 31(7), 533–535 (2005).
Machado, R. et al. Extrusion of debris with and without intentional foraminal enlargement–a systematic review and meta-analysis. Aust. Endod. J. 47(3), 741–748 (2021).
Yaylali, I. E., Teke, A. & Tunca, Y. M. The effect of foraminal enlargement of necrotic teeth with a continuous rotary system on postoperative pain: A randomized controlled trial. J. Endod. 43(3), 359–363 (2017).
Vieira, M. L. et al. Morphologic changes of apical foramen and microcrack formation after foraminal enlargement: A scanning electron microscopic and micro–computed tomographic analysis. J. Endod. 46(11), 1726–1732 (2020).
Fatima, S., Kumar, A., Andrabi, S. M. U. N., Mishra, S. K. & Tewari, R. K. Effect of apical third enlargement to different preparation sizes and tapers on postoperative pain and outcome of primary endodontic treatment: A prospective randomized clinical trial. J. Endod. 47(9), 1345–1351 (2021).
Cailleteau, J. G. & Mullaney, T. P. Prevalence of teaching apical patency and various instrumentation and obturation techniques in United States dental schools. J. Endod. 23(6), 394–396 (1997).
Machado, R., Comparin, D., Aparecido, S. I. & Da Silva, U. X. Postoperative pain after endodontic treatment of necrotic teeth with large intentional foraminal enlargement. Restor. Dent. Endod. 46(3), 1–13 (2021).
Jensen, M. P., Karoly, P. & Braver, S. The measurement of clinical pain intensity: A comparison of six methods. Pain 27(1), 117–126 (1987).
Fernandes, L. A. et al. Root canal treatment postoperative pain assesment in head and neck postirradiated patients: A controlled clinical trial. Oral Health Dent. Manag. 19(4), 1–4 (2020).
Keskin, C., Özdemir, Ö., Uzun, İ & Güler, B. Effect of intracanal cryotherapy on pain after single-visit root canal treatment. Aust. Endod. J. 43(2), 83–88 (2017).
Rimmer, A. The flare-up index: A quantitative method to describe the phenomenon. J. Endod. 19(5), 255–256 (1993).
Ajeesh, K., Jayasree, S., James, E. P., Pooja, K. P. & Jauhara, F. Comparative evaluation of the effectiveness of intracanal and intraoral cryotherapy on postendodontic pain in patients with symptomatic apical periodontitis: A randomized clinical trial. J. Conserv. Dent. Endod. 26(5), 555–559 (2023).
Ehrmann, E. H., Messer, H. H. & Clark, R. M. Flare-ups in endodontics and their relationship to various medicaments. Aust. Endod. J. 33, 119–130 (2007).
Aoun, C., El Osta, N., Naaman, A., Zogheib, C. & Khalil, I. Post-endodontic flare-ups after a single-visit treatment using the FUI scoring method and associated factors: A clinical prospective study. J. Contemp. Dent. Pract. 20(9), 1033–1040 (2019).
Alaçam, T. & Tinaz, A. Interappointment emergencies in teeth with necrotic pulps. J. Endod. 28(5), 375–377 (2002).
Canalda, C. S. & Aguadé, E. B. Endodoncia: Técnicas Clínicas y Bases Científicas 4th edn. (Elsevier, 2019).
Vera, J. et al. Intracanal cryotherapy reduces postoperative pain in teeth with symptomatic apical periodontitis: A randomized multicenter clinical trial. J. Endod. 44(1), 4–8 (2018).
Gundogdu, E. C. & Arslan, H. Effects of various cryotherapy applications on postoperative pain in molar teeth with symptomatic apical periodontitis: A preliminary randomized prospective clinical trial. J. Endod. 44(3), 349–354 (2018).
Sadaf, D., Ahmad, M. Z. & Onakpoya, I. J. Effectiveness of intracanal cryotherapy in root canal therapy: A systematic review and meta-analysis of randomized clinical trials. J. Endod. 46(12), 1811–1823 (2020).
Vera, J. et al. Effect of intracanal cryotherapy on reducing root surface temperature. J. Endod. 41(11), 1884–1887 (2015).
Hespanhol, F. G., Guimarães, L. S., Antunes, L. A. A. & Antunes, L. S. Effect of intracanal cryotherapy on postoperative pain after endodontic treatment: Systematic review with meta-analysis. Restor Dent. Endod. 47(3), 1–15 (2022).
Schaubel, H. J. The local use of ice after orthopedic procedures. Am. J. Surg. 72(5), 711–714 (1946).
Abramson, D. I. et al. Effect of tissue temperatures and blood flow on motor nerve conduction velocity. JAMA 198(10), 1082–1088 (1966).
Monteiro, L. P. B. et al. Effect of intracanal cryotherapy application on postoperative endodontic pain: A systematic review and meta analysis. Clin. Oral Investig. 25, 23–35 (2021).
Alharthi, A. A., Aljoudi, M. H., Almaliki, M. N., Almalki, M. A. & Sunbul, M. A. Effect of intra-canal cryotherapy on post-endodontic pain in single-visit RCT: A randomized controlled trial. Saudi Dent. J. 31(3), 330–335 (2019).
Whitten, B. H., Gardiner, D. L., Jeansonne, B. G. & Lemon, R. R. Current trends in endodontic treatment: Report of a national survey. J. Am. Dent. Assoc. 127(9), 1333–1341 (1996).
Shirvani, A., Shamszadeh, S., Eghbal, M. J. & Asgary, S. The efficacy of non-narcotic analgesics on post-operative endodontic pain: A systematic review and meta-analysis: The efficacy of non-steroidal anti-inflammatory drugs and/or paracetamol on post-operative endodontic pain. J. Oral Rehabil. 44(9), 709–721 (2017).
Shamszadeh, S., Shirvani, A., Eghbal, M. J. & Asgary, S. Efficacy of corticosteroids on postoperative endodontic pain: A systematic review and meta-analysis. J. Endod. 44(7), 1057–1065 (2018).
Grosser, T., Smyth, E. & Fitzgerald, G. A. Goodman and Gilman’s, The Pharmacological Basis of Therapeutics 12th edn. (Mc Graw Hill Medical, 2011).
Trope, M. Flare-up rate of single-visit endodontics. Int. Endod. J. 24, 24–27 (1991).
De Freitas, F. S. et al. Effect of foraminal enlargement on postoperative pain in necrotic single-rooted teeth: A randomized clinical trial. J. Endod. 47(7), 1046–1051 (2021).
Ricucci, D. & Langeland, K. Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int. Endod. J. 31(6), 394–409 (1998).
Mitchell, R. P., Yang, S. & Baumgartner, J. C. Comparison of apical extrusion of naocl using the endovac or needle irrigation of root canals. J. Endod. 36(2), 338–341 (2010).
Márton, I. J. & Kiss, C. Protective and destructive immune reactions in apical periodontitis. Oral Microbiol. Immunol. 15(3), 139–150 (2000).
Acknowledgements
The authors deny any conflicts of interest related to this study. The authors thank to Dr. Sérgio Aparecido Ignácio for his assistance with the statistical analysis.
Author information
Authors and Affiliations
Contributions
MFIN contributed to sample collection, MFIN and AVKS contributed to data aquisition and analysis, and drafted the manuscript; MAHD contributed to conception, data interpretation and critically reviewed the manuscript; UXSN and VPDW contributed to analysis and critically reviewed the manuscript, EC contributed to conception, data analysis and interpretation, drafted and critically reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Iparraguirre Nuñovero, M.F., Hungaro Duarte, M.A., Kaled Segato, A.V. et al. The effect of intracanal cryotherapy with and without foraminal enlargement on pain prevention after endodontic treatment: a randomized clinical trial. Sci Rep 14, 19905 (2024). https://doi.org/10.1038/s41598-024-70901-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70901-w