Abstract
The cost fluctuations associated with chemotherapy, radiotherapy, and immunotherapy, as primary modalities for treating malignant tumors, are closely related to medical decision-making and impose financial burdens on patients. In response to these challenges, China has implemented the Diagnosis-Related Group (DRG) payment system to standardize costs and control expenditures. This study collected hospitalization data from patients with malignant tumors who received chemotherapy, radiotherapy, and immunotherapy at Hospital H from 2018 to 2022. The dataset was segmented into two groups: the intervention group, treated with traditional Chinese medicine (TCM) alongside standard therapies, and the control group, treated with standard therapies alone. Changes and trends in hospitalization costs under the DRG policy were analyzed using propensity-score matching (PSM), standard deviation (SD), interquartile range (IQR), and concentration index (CI). Findings showed a decreasing trend in the standard deviation of hospitalization costs across all treatment modalities. Radiotherapy exhibited the most significant decrease, with costs reducing by 2547.37 CNY in the control group and 7387.35 CNY in the intervention group. Following the DRG implementation, the concentration indexes for chemotherapy and radiotherapy increased, while those for immunotherapy did not exhibit this pattern. Costs were more concentrated in patients who did not receive TCM treatment. In summary, DRG reform positively impacted the cost homogeneity of inpatient treatments for malignant tumors, particularly in the control group not receiving TCM treatment. The effects of DRG reform varied across different treatment modalities. Although short-term fluctuations in hospitalization costs may occur, initial evidence during the study period shows the positive impact of DRG reform on cost homogeneity.
Similar content being viewed by others
Introduction
Hospitalization cost homogeneity means that the fees charged for treatment or medical services for the same type of disease or procedure are relatively stable and consistent across different regions and hospitals within acceptable margins1,2,3. With the global increase in healthcare service demand, cost homogeneity has emerged as a pivotal issue in healthcare management and policy formulation4,5. Cost homogeneity in healthcare largely reflects the rational allocation and utilization of medical resources, which is of great significance for promoting equity and reducing patients' financial burden. Yong et al.6 evaluated healthcare utilization and costs for stroke patients across 31 provinces in China. They found a significant correlation between resources and costs, advocating for balanced service prices to ensure rational resource allocation, promote equity, and reduce patient burdens. James Love-Koh et al.7 discerned that changes in National Health Service (NHS) spending in the UK could have health effects in specific areas, particularly those individuals from deprived areas are adversely affected, highlighting the importance of healthcare cost homogeneity in promoting health equity.
As a substantial component of healthcare expenses, the fluctuation in hospitalization costs profoundly influences the operational efficacy of healthcare entities, the economic steadiness of health insurance schemes, and the fiscal encumbrance on patients. Adrian Diaz et al.8 identified significant inpatient cost variations both between and within hospitals, resulting in high-risk surgery concentration and financial pressure. Greater internal cost variation led to higher average total inpatient costs. Brendon Herring et al.9, by analyzing the volatility of hospitalization costs, pointed out that cost volatility leads to cost differences of up to three times for some surgeons even when they perform the same procedure, which adversely affects healthcare organizations, health insurance, and patients' financial burden. Some scholars have highlighted that significant cost variations persist among patients with the same disease and undergoing identical treatment processes10,11,12. Poor cost homogeneity is linked to the medical decisions of healthcare providers and standardized service delivery within medical institutions, potentially imposing additional financial burdens on patients and undermining equity13,14. The uncertainty and volatility of healthcare costs in several countries and regions have stimulated the search for more effective cost containment and homogeneity strategies aimed at reducing the burden on patients by improving cost predictability, transparency, and promoting the quality of healthcare services and the sustainability of healthcare systems15,16.
The treatment of malignant tumors, a significant health concern, is often characterized by complexity and high costs, imposing a substantial financial burden on patients and their families17,18. Though treatment modalities such as chemotherapy, radiotherapy and immunotherapy have improved the therapeutic efficacy to a certain extent, they have also significantly increased the medical costs19,20. In this context, the integration of Traditional Chinese Medicine (TCM) as an adjunct therapy has gained widespread usage in China21,22. TCM treatment not only can alleviate some side effects during malignant tumor treatment and improve patients' quality of life23,24, but also offers the possibility of controlling the overall cost of treatment25,26. The treatment of malignant tumors with TCM has been proven to be effective in various aspects. Sumei Wang et al.27 showed that Chinese herbal medicine primarily treats cancer by modulating the immune system, thereby amplifying the effectiveness of conventional therapies and reducing the associated harm. Yixin Cui et al.28 elucidated the pharmacological foundations and mechanisms of TCM in treating malignant tumors by analyzing HQSJZD's effects on cancer-related fatigue (CRF). Li Ma et al.24 concluded through meta-analysis that the overall efficacy of integrating TCM with Western medicine for malignant tumors is superior to that of Western medicine alone. Studies have shown that TCM treatment can reduce hospitalization costs. Shun-Ku Lin et al.26 found that TCM users had lower hospitalization costs and shorter stays, with costs decreasing as TCM usage duration increased. Moran Dong et al.25 observed that hospitalized patients receiving TCM treatment had lower non-pharmacological treatment costs compared to those not receiving TCM treatment. Given the increasingly acknowledged efficacy of combined TCM treatment, investigating its economic impact in malignant tumor management is crucial for optimizing treatment protocols and lessening the financial strain on patients.
Diagnosis-related group (DRG) system is an internationally recognized advanced hospital management method, first pioneered in the United States in the 1960s29,30, and the implementation of the DRG payment system marks an important shift in healthcare cost control strategies. As a prepaid cost model, DRG aims to incentivize healthcare providers to improve their service delivery and reduce unnecessary healthcare consumption, thereby achieving effective control of healthcare costs, through the categorization of hospital treatment processes and fixing payment rates for each category31,32. The implementation of this payment system is particularly critical for the homogeneity and control of malignancy treatment costs, which can not only affect the quality and accessibility of healthcare services, but also directly relate to patients' financial burden and treatment choices33,34,35. Therefore, evaluating the effect of DRG payment system implementation in China, especially the actual impact on the control of malignant tumor treatment costs, has important practical and theoretical value for further optimizing the medical cost payment system and improving the quality of medical services.
Methods
Data source
Hangzhou City, Zhejiang Province, China, implemented a DRGs point payment system on January 1, 2020, and this medical insurance reform initiative has had a profound impact on hospitalization medical costs. In this study, a tertiary hospital in Hangzhou City was selected as the study population to explore the impact of DRG payment reform on the homogeneity of malignant tumor treatment costs. The study period spans from 2018 to 2022, according to confirmation from the hospital, the policy most significantly related to cost homogeneity during this period is the DRG reform. All discharged cases in the study period of 2018–2019 adopt the Fee-For-Service (FFS) payment method, and all discharged cases in 2020–2022 adopt the DRG payment method. Because of the widespread use of radiotherapy, chemotherapy, and immunotherapy as well as their significant effects among the treatment modalities for patients with malignant tumors, we selected three commonly used treatment modalities for malignant tumors, namely, radiotherapy (coded Z51.0), chemotherapy (coded Z51.1), and immunotherapy (coded Z51.8), to focus on the study. At the same time, we collected information on key variables including age, gender, ICD code, clinical pathway management, and whether or not combined with TCM treatment. All data were obtained from the patient's case homepage information and the billing records of the health insurance platform.
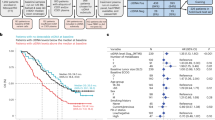
Study design
This study aims to explore the homogeneity in hospitalization costs across different treatment modalities for malignant tumors by longitudinally comparing annual changes and variations in hospitalization costs between 2018 and 2022, while also assessing the short-term effects of DRG payment reform on these costs. Changes and differences in hospitalization costs between the three treatment modalities were compared. In addition, patients were divided into an intervention group (combined TCM treatment) and a control group (no combined TCM treatment) using whether or not the treatment was combined with TCM treatment as an intervening factor to explore the cost concentration differences in hospitalization costs between the two groups. To ensure that the intervention and control groups were balanced and comparable, a 1:1 propensity-score matching (PSM) method was used by matching patients' age, gender and clinical pathway. The Caliper value for matching accuracy was 0.01. The specific selection and exclusion process of the study population is illustrated in Fig. 1.
Statistical analysis
This study evaluates the variations in hospitalization cost trends in the intervention and control groups before and after DRG implementation payments. Since the costs were incurred in different calendar years, the cost data were adjusted using the Consumer Price Index (CPI) of the respective years, with 2022 as the reference year36,37. The adjusted values are presented in Supplementary Table 1. The degree of variability in hospitalization costs was expressed as standard deviation (SD), box plot joint interquartile range (IQR). The smaller the value of standard deviation, the more concentrated the distribution of hospitalization costs, while the double-difference value was used to analyze the difference in the degree of variability between the intervention group and the control group. Similarly, a smaller interquartile range (IQR) signifies a more concentrated cost distribution, which is visualizable through a box plot. Furthermore, the concentration index was chosen to reflect the distribution of hospitalization costs under different treatment modalities. Meanwhile, the Kruskal–Wallis test was used to compare the concentration index in each year and calculate the P-value. The formula for calculating the concentration index is shown as follows.
In this formula, cov (h,ri) represents the covariance between the hospitalization cost per patient (h) and the rank of each patient within the sample (ri). The assignment to the intervention group (ri = 1) or the control group (ri = 0) served as the criterion variable, indicating the cost concentration differential between the TCM-combined treatment modality and the non-TCM-combined treatment modality. A larger absolute value of the concentration index signifies a more concentrated cost distribution, whereas a value closer to 0 indicates a less concentrated distribution of hospitalization costs. A concentration index below 0 suggests that hospitalization costs are predominantly concentrated within the intervention group, whereas an index above 0 suggests concentration in the control group32.
The significance level for statistical tests was established at α = 0.05, with all statistical analyses conducted using Stata 17.0.
Ethics approval statement
The data for this study were sourced from the DRG database of Zhejiang Hospital, referred to here as "Hospital H". In compliance with local database management protocols, all data from the hospital were anonymized prior to release. The hospital has authorized the use of this anonymized database for research purposes, and at no point during the study were any personal details or patient identities accessed. The research protocol was reviewed and approved by the Ethics Committee of Zhejiang University of Chinese Medicine, with a waiver for the requirement of individual informed consent based on the nature of the study. This project adheres strictly to the ethical standards prescribed by the Declaration of Helsinki, ensuring that all data handling methods meet the appropriate ethical requirements.
Informed consent statement
Since the data obtained has been replaced with specific codes for each patient by the hospital, not containing any personal information that could be associated with individual participants, informed consent is not required.
Results
Basic information about the sample
Table 1 presents data on the distribution of patients across various treatment modalities following propensity score matching based on gender, age, and completion of clinical pathways. In 2018–2022, there were a total of 12,539 patients with malignant tumors in the database, and according to the completeness of the data as well as the prevalence of the treatment modalities, patients with three treatment modalities, namely, chemotherapy, radiotherapy, and immunotherapy, were selected for the study. A total of 1776 patients were included after PSM, and they were divided into two groups, the control group and the intervention group, based on the use or non-use of TCM treatment. Among them, 852 patients were treated with chemotherapy, 284 patients were treated with radiotherapy, and 640 patients were treated with immunotherapy. Overall, the gender distribution of the patients was relatively even, and patients aged 61–70 years old accounted for the majority of the patients. The data showed that patients who had not completed the clinical pathway management accounted for a larger proportion of the patients in the treatment, with more than 60% of the patients under each treatment modality. The characteristics of patients under the three treatment modalities also differed slightly, with a larger gender distribution gap in immunotherapy and a greater concentration of patients in the age group of 61–70 years old. In terms of the proportion of clinical pathway management, a greater proportion of patients undergoing immunotherapy did not complete clinical pathway management, accounting for as much as 78.75% of the patients, indicating a lower degree of treatment standardization in immunotherapy, this may be attributed to the complexity of clinical treatment in immunotherapy.
Table 2 shows the differences in health output indicators between the control group and the intervention group for three treatment methods. This study selected discharge status and re-admission plans as the main indicators to reflect the differences in patients' health status after treatment and the long-term effects of the treatment. Specifically, health output indicators include the number of cases cured, improved, not improved, and deceased, while re-admission plans include the number of cases with or without re-admission plans. From the table, it can be seen that in all groups, the proportion of patients with improved discharge status is the highest, accounting for 90% of all patients. Re-admission plans are mostly "yes", with each group exceeding 90%. This may be due to the high efficiency of treatment, the complexity of malignant tumor patients' conditions requiring continuous treatment and monitoring, and the DRG reform policy encouraging more inpatient treatment. Among the three treatment methods, only chemotherapy showed statistically significant differences in discharge status and re-admission plans between the control group and the intervention group. Specifically, the control group had 406 patients with improved conditions, compared to 418 in the intervention group, indicating more positive outcomes in the intervention group. In terms of re-admission plans, the number of patients planning re-admission was significantly lower in the intervention group than in the control group. This may be attributed to the adjunctive role of additional treatments in chemotherapy, leading to better discharge outcomes and lower re-admission rates for patients receiving combined treatments. The proportion of patients with readmission plans for immunotherapy (97.03%) is higher than that for chemotherapy (95.42%) and radiotherapy (94.37%). This may be due to the clinical complexity of immunotherapy and the variability among immunotherapy patients.
Trends in the standard deviation (SD) of hospitalization costs
Table 3 displays the standard deviation (SD) of hospitalization costs for both intervention and control groups, delineating annual fluctuations and presenting the double-difference value to ascertain the disparity in annual trends between the two cohorts.
In terms of cost fluctuation trends, the SD of hospitalization costs for the chemotherapy treatment intervention group decreased the most in the first year (2020) after the reform of the DRG payment policy, by 7136.07 CNY, and the SD of hospitalization costs for the control group showed a fluctuating downward trend. For radiotherapy, the control group's hospitalization cost SD exhibited a generally declining trend, in contrast to the intervention group, which displayed a trend of initial decline followed by an increase. For immunotherapy, the control group's SD of hospitalization costs revealed a consistently decreasing trend, whereas the intervention group experienced an initial increase followed by a decrease in SD post-reform. Overall before and after the DRG reform of the three treatment modalities of chemotherapy, radiotherapy and immunotherapy, the SD of each treatment modality showed an overall fluctuating downward trend. This implies that the DRG policy's implementation might have contributed to diminishing the volatility of patients' hospitalization costs, thereby enhancing cost stability.
Concerning cost differences before and after the DRG reform, the SD of chemotherapy and radiotherapy treatment costs exhibited more significant changes in both intervention and control groups. Specifically, within radiotherapy, the standard deviation (SD) of costs witnessed a significant decrease in the intervention group, whereas it altered minimally in the control group. In immunotherapy, the change in cost SD was smaller and the trend was less pronounced in both the intervention and control groups. This may indicate that the DRG reform had a relatively small impact on the cost of immunotherapy. Overall, the SD of hospitalization costs in the control group was essentially lower than the SD of the intervention group in the same group and year.
In terms of the change in the double-difference value, both chemotherapy and radiotherapy treatments showed a substantially greater decrease in hospitalization costs SD within the intervention group than in the control group in the first year of the DRG reform, and the double-difference value was negative, suggesting that the transient impact of the DRG policy on the intervention group exceeded that of the control group in chemotherapy and radiotherapy treatments. Then the double-difference value is positive, indicating that after the first year of the reform, the fluctuation of costs affected by the policy gradually decreases in the control group, and this state is shown more clearly than in the intervention group. Conversely, immunotherapy does not show this trend, suggesting that the DRG reform impacts immunotherapy hospitalization costs differently from those of chemotherapy and radiotherapy treatments.
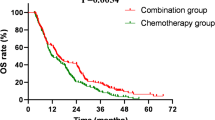
Trends in the interquartile range (IQR) of hospitalisation costs
Figure 2 demonstrates the distribution of hospitalization costs for patients with malignant tumors treated with chemotherapy, radiotherapy, and immunotherapy without combining TCM in their treatment (left-hand chart) and with combining TCM in their treatment (right-hand chart). The box plots present the interquartile range (IQR), median, upper and lower quartiles of hospitalization costs, reflecting the overall trend and degree of dispersion of hospitalization costs.
For chemotherapy patients, the control group showed an overall trend of decreasing IQR and median year by year from 2018 to 2022, along with a decreasing gap between the upper and lower quartiles, and the trend was more pronounced after the DRG reform was implemented, despite an initial increase in median cost in the first year following the reform (2019–2020). Similarly, the intervention group demonstrated a yearly decrease in both IQR and median costs from 2018 to 2022, indicating a reduction in costs and a narrowed cost variance. However, process-wise, the overall trend and dispersion of costs changed relatively more in the pre-DRG reform period (2018–2019), with a relatively large increase in both median and IQR, and an increase in median costs in the first year of reform (2019–2020). The median hospitalization costs were lower in the control group than in the intervention group, and the IQR also showed a more pronounced and sustained downward trend, suggesting that the combined TCM treatments may have had an impact on the homogeneity of hospitalization costs.
The Hospital H initiated radiotherapy treatments in 2019. From 2019 to 2022, the control group experienced a marginal increase in hospitalization costs, yet displayed a fluctuating overall trend. Notably, the IQR significantly decreased in the initial year of DRG reform implementation (2019–2020), indicating a heightened concentration of hospitalization costs in 2020. Despite a rise in 2021, the IQR subsequently diminished to its lowest levels for the year. Between 2019 and 2022, median hospitalization costs in the intervention group exhibited a yearly ascending trend. Following the implementation of DRG reforms (2020–2022), the IQR consistently declined, denoting an increasing concentration of hospitalization costs. Comparatively, post-DRG implementation, median hospitalization costs in the intervention group incrementally exceeded those in the control group. Subsequently, the cost distributions of both groups converged, illustrating the DRG payment system's incremental influence on cost containment. This convergence suggests that DRG reforms could positively affect cost distribution consistency over the long term, despite potential short-term fluctuations.
In patients undergoing immunotherapy, the control group exhibited a fluctuating trend in median hospitalization costs from 2018 to 2022. Following the DRG reform's introduction (2020–2022), the IQR demonstrated a decreasing trend, indicating a more concentrated cost distribution. Concurrently, the gap between the upper and lower quartiles progressively narrowed each year post-2018, with this trend becoming particularly pronounced following the DRG reform. Between 2018 and 2022, the intervention group's median hospitalization cost and IQR initially rose pre-DRG reform, followed by an annual decline, enhancing the cost distribution's consistency in 2022 relative to 2018. Before the DRG reform, median costs and IQR in the intervention group saw a significant increase in 2019 compared to 2018, followed by a gradual decrease, particularly between 2020 and 2021, after the reform's implementation. During this period, the control group consistently incurred lower median hospitalization costs than the intervention group, with a significant downward trend in their IQRs. This suggests that the DRG reforms potentially contributed positively to cost consistency improvement, despite possibly causing a temporary cost increase at the reform's outset.
Hospitalization costs concentration index
The concentration index of patients' hospitalization costs is shown in Table 4. The homogeneity of hospitalization costs is indicated by the magnitude of the concentration index's absolute value, while its sign (positive or negative) reflects variations in cost distribution.
Regarding cost concentration, chemotherapy and radiotherapy treatments' cost homogeneity has increased. Despite a sudden decline in the absolute value of inpatient hospitalization costs in the reform's first year, the concentration index's absolute value has been rising annually post-DRG implementation. In particular, the increase in the concentration index was statistically significant in 2021 and 2022 (P < 0.05). In contrast, immunotherapy's hospitalization cost concentration index has been trending downward in absolute terms year after the DRG was implemented. Despite a brief upward trend in 2020, the downward trajectory stabilized in subsequent years. This indicates that the DRG policy's relatively weak cost-containment impact on immunotherapy might be attributable to the treatment's inherent specificity and cost volatility.
On the analysis of differences in cost distribution, the concentration index was less than 0 only in radiotherapy treatment in 2020 and in immunotherapy treatment in 2018, but neither of them was statistically significant (P > 0.05). The rest of the concentration indices were all greater than 0, showing that the hospitalization costs were more concentrated in the different treatment modalities without combined TCM treatment, which may be related to the cost characteristics of TCM treatment and its use by patients.
Discussion
This study provides a detailed analysis of the DRG reform's impact on malignancy treatment costs, focusing particularly on the differential responses of hospitalization cost concentration indices across chemotherapy, radiotherapy, and immunotherapy. The goal of DRG reform is to optimize resource allocation and enhance treatment efficiency by standardizing payment rates. Previous research has indicated that DRGs can diminish treatment cost fluctuations, thereby facilitating cost control38,39. Study findings indicate an upward trend in the hospitalization cost concentration index for chemotherapy and radiotherapy, suggesting that costs for these traditional treatments have become more concentrated post-DRG implementation. Numerous studies corroborate these findings. For instance, Siyu Zeng et al.40 observed that DRG's controlling effect manifested as reduced cost variation coefficients and diminished upper cost limits for patients, evidencing a greater centralization of healthcare costs post-DRG implementation. Conversely, the concentration index for immunotherapy exhibited a yearly decreasing trend, not constrained by standard DRG payment limits, which may be attributed to the continuous rapid advancements in immunotherapy technology and drugs41,42,43. Since 2018, Hospital H has continuously introduced various new drugs and technologies in immunotherapy, such as sintilimab, camrelizumab, tislelizumab, and atezolizumab, as well as CAR-T therapy and tumor vaccine technology. These advancements may lead to increased complexity in medical cost management. The results of this study indicate that immunotherapy, compared to other treatment methods, has a higher proportion of patients who did not complete the clinical pathway and a higher proportion of patients with readmission plans. This may reflect the variability among immunotherapy patients and the complexity of immunotherapy, which also affects the constraints of DRG on the homogeneity of inpatient costs for immunotherapy44,45. This discovery indicates variability in the cost impact of DRG reforms across different treatments, suggesting the necessity for nuanced adjustments in payment system reforms to accommodate diverse treatment modalities.
Furthermore, this study delved into the economic implications of incorporating Traditional Chinese Medicine (TCM) in malignant tumor treatments. The potential of TCM to alleviate therapeutic side effects and enhance quality of life is increasingly acknowledged. For instance, Zimei Yang et al.46 highlighted TCM's significance in clinical practice by identifying the antitumor properties of Chinese herbs and natural medicines in triple-negative breast cancer (TNBC). Yanleng Huang et al.47 summarized TCM's efficacy in migraine treatments, highlighting strategies such as activating blood circulation, calming the liver, and enhancing qi, underscoring its substantial benefits for chronic conditions like migraines. Thus, analyzing the hospitalization costs associated with combined TCM treatments becomes particularly crucial. Study findings indicate that while combined TCM treatments may initially lead to increased fluctuations in hospitalization costs, they tend to ensure cost stability and predictability over the long term. This underscores the necessity of contemplating combined treatment modalities in healthcare cost assessments and highlights the complexities involved in evaluating TCM's value within contemporary healthcare systems.
The Chinese government's DRG reform primarily aims to control unreasonable cost increases effectively, concurrently ensuring healthcare service quality48,49. This study underscores the imperative of balancing cost control with the preservation of healthcare service quality in the implementation of the DRG payment system, considering its potential impact. Prior research has identified physicians' behavior as a crucial determinant in healthcare cost variations, noting that these behavioral cost differences surpass inter-hospital cost disparities50,51. Under the DRG system, the relationship between hospitalization costs and service quality is not linear, being subject to a multiplicity of influencing factors. The DRG system fosters the rational allocation of healthcare resources and cost management, enhancing service efficiency. However, it may also precipitate adverse effects; cost containment efforts might prompt hospitals and physicians to reduce service breadth, curtail bed utilization, or expedite patient turnover, potentially diminishing service quality52,53,54,55,56. While DRG reforms can mitigate cost volatility and enhance care efficiency and quality, the design of provider incentives and management mechanisms must be meticulously crafted to sidestep potential drawbacks. Within this framework, key strategies for curtailing cost overruns include symptom-focused treatments, stringent adherence to standardized clinical pathways, and the efficient, judicious utilization of healthcare resources57,58. It necessitates policymakers to account for varied treatments and patient group specifics in DRG payment system implementation, aiming to control healthcare service costs without compromising quality, thereby achieving effective healthcare resource utilization and the system's sustainable development.
Limitations
The limitations of this study suggest directions for future research. Although this study provides initial insights into the impact of DRG reform, limitations in the scope of data collection and the choice of analytic methods may have affected the broad applicability of the results. Furthermore, this study primarily focuses on the impact of DRG reform on cost homogeneity, potentially overlooking other factors that might influence cost variations. Due to methodological constraints, the study cannot fully address the influence of concurrent policies. Future studies could further explore the impact of DRG reform on the cost of malignancy treatment by expanding the sample size, covering a wider range of treatments and providers, and employing more sophisticated statistical analysis techniques. In addition, considering the rapid development of medical technology and the continuous evolution of healthcare policies, continuous evaluation of the DRG payment system and its adaptability and effectiveness in different healthcare settings will be important for improving the quality of healthcare services and controlling healthcare costs.
Conclusions
The implementation of the DRG reform has significantly improved cost homogeneity in the treatment of malignant tumors. Our findings indicate that DRG reform effectively stabilized and concentrated hospitalization costs, especially for chemotherapy and radiotherapy. However, the impact of DRG reform on the cost of immunotherapy remains limited, likely due to the high variability among patients, the continuous innovation of new therapies, and the complexity of clinical applications. The integration of TCM with conventional treatments showed initial cost fluctuations but ultimately improved cost homogeneity over the study period. This underscores the importance of including combined treatment modalities in healthcare cost assessments. Overall, the DRG reform has enhanced cost control and efficiency in healthcare resource allocation. Continuous evaluation and adaptation of the DRG system are essential to accommodate diverse treatments and ensure the sustainability of healthcare systems.
Data availability
The data analyzed in this study were obtained from Hospital H, and because we are using them with permission for this study, their availability is limited and they are not publicly available. However, data supporting the findings of this study can be obtained by contacting the corresponding author if reasonably requested.
Change history
17 December 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-82652-9
References
Sutzko, D. C., Andraska, E. A., Gonzalez, A. A., Chakrabarti, A. K. & Osborne, N. H. Examining variation in Medicare payments and drivers of cost for carotid endarterectomy. J. Surg. Res. 228, 299–306 (2018).
Black, G. B. et al. Temporal structures that determine consistency and quality of care: A case study in hyperacute stroke services. BMJ Qual. Saf. https://doi.org/10.1136/bmjqs-2022-015620 (2023).
Smeulers, M. et al. Quality indicators for safe medication preparation and administration: A systematic review. PLOS ONE 10, e0122695 (2015).
Haas, L. et al. Introduction of DRG-based reimbursement in inpatient psychosomatics—An examination of cost homogeneity and cost predictors in the treatment of patients with eating disorders. J. Psychosom. Res. 73, 383–390 (2012).
Shin, D. G. et al. Differences of medical costs by classifications of severity in patients of liver diseases. Health Policy Manag. 23, 35–43 (2013).
Yang, Y. et al. An equity evaluation in stroke inpatients in regard to medical costs in China: A nationwide study. BMC Health Serv. Res. 21, 425 (2021).
Love-Koh, J., Cookson, R., Claxton, K. & Griffin, S. Estimating social variation in the health effects of changes in health care expenditure. Med. Decis. Making 40, 170–182 (2020).
Diaz, A., Nuliyalu, U., Dimick, J. B. & Nathan, H. Variation in surgical spending among the highest quality hospitals for cancer surgery. Ann. Surg. 276, e728–e734 (2022).
Herring, B. et al. Wide provider variation in cost for thyroidectomy: Potential benefits of standardizing practice?. J. Surg. Res. 267, 9–16 (2021).
Ogino, M. et al. Prevalence, treatments and medical cost of multiple sclerosis in Japan based on analysis of a health insurance claims database. Clin. Exp. Neuroimmunol. 8, 318–326 (2017).
Hampson, L. A., Odisho, A. Y. & Meng, M. V. Variation in laparoscopic nephrectomy surgical costs: Opportunities for high value care delivery. Urol. Pract. 5, 334–341 (2018).
Hall, B. L., Campbell, D. A., Phillips, L. R. S. & Hamilton, B. H. Evaluating individual surgeons based on total hospital costs: Evidence for variation in both total costs and volatility of costs. J. Am. Coll. Surg. 202, 565–576 (2006).
Xu, X. et al. Hospital variation in cost of childbirth and contributing factors: a cross-sectional study. Bjog- Int. J. Obstet. Gynaecol. 125, 829–839 (2018).
Jonas, J. A. et al. Regional variation in standardized costs of care at children’s hospitals. J. Hosp. Med. 12, 818–825 (2017).
Abdelsattar, Z. M., Birkmeyer, J. D. & Wong, S. L. Variation in medicare payments for colorectal cancer surgery. J. Oncol. Pract. 11, 391–395 (2015).
Sinaiko, A. D. et al. What drives variation in spending for breast cancer patients within geographic regions?. Health Serv. Res. 54, 97–105 (2019).
Zhao, L. & Tang, J. Analysis of the composition and influencing factors of hospitalization expenses for 1517 patients with lung malignant tumors in Beijing. Medicine (Baltimore) 103, e37385 (2024).
Park, T. & Hwang, M. Health care use and expenditures attributable to cancer: A population-based study. Res. Soc. Adm. Pharm. 17, 1300–1305 (2021).
Yu, W.-D., Sun, G., Li, J., Xu, J. & Wang, X. Mechanisms and therapeutic potentials of cancer immunotherapy in combination with radiotherapy and/or chemotherapy. Cancer Lett. 452, 66–70 (2019).
Giuliani, J. & Fiorica, F. Cost-effectiveness of immune checkpoint inhibitors and radiotherapy in advanced non-small cell lung cancer. J. Oncol. Pharm. Pract. 27, 2004–2006 (2021).
Zhang, X., Qiu, H., Li, C., Cai, P. & Qi, F. The positive role of traditional Chinese medicine as an adjunctive therapy for cancer. Biosci. Trends 15, 283–298 (2021).
Zhang, Y., Lou, Y., Wang, J., Yu, C. & Shen, W. Research status and molecular mechanism of the Traditional Chinese Medicine and antitumor therapy combined strategy based on tumor microenvironment. Front. Immunol. 11, 609705 (2021).
Su, X.-L. et al. Clinical application and mechanism of traditional Chinese medicine in treatment of lung cancer. Chin. Med. J. (Engl.) 133, 2987–2997 (2020).
Ma, L., Wang, B., Long, Y. & Li, H. Effect of traditional Chinese medicine combined with Western therapy on primary hepatic carcinoma: a systematic review with meta-analysis. Front. Med. 11, 191–202 (2017).
Dong, M. et al. Hospitalization COSTS of COVID-19 cases and their associated factors in Guangdong, China: A cross-sectional study. Front. Med. 8, 655231 (2021).
Lin, S.-K., Lo, P.-C., Chen, W.-C. & Lai, J.-N. Integrating traditional Chinese medicine healthcare into dementia care plan by reducing the need for special nursing care and medical expenses. Medicine (Baltimore) 98, e14468 (2019).
Wang, S., Long, S., Deng, Z. & Wu, W. Positive role of Chinese Herbal Medicine in cancer immune regulation. Am. J. Chin. Med. 48, 1577–1592 (2020).
Retracted: Network Pharmacology Analysis on the Mechanism of Huangqi Sijunzi Decoction in Treating Cancer-Related Fatigue. J. Healthc. Eng. 2023, 1–1 (2023).
Fetter, R. B., Shin, Y., Freeman, J. L., Averill, R. F. & Thompson, J. D. Case mix definition by diagnosis-related groups. Med. Care 18(iii), 1–53 (1980).
Busse, R. et al. Diagnosis related groups in Europe: Moving towards transparency, efficiency, and quality in hospitals?. BMJ 346, f3197–f3197 (2013).
Sheaff, R. et al. Managerial workarounds in three European DRG systems. J. Health Organ. Manag. 34, 295–311 (2020).
Li, Q., Fan, X. & Jian, W. Impact of Diagnosis-Related-Group (DRG) payment on variation in hospitalization expenditure: Evidence from China. BMC Health Serv. Res. 23, 688 (2023).
Liu, X. et al. Performance evaluation of medical service for breast cancer patients based on diagnosis related groups. BMC Health Serv. Res. 21, 496 (2021).
Polonsky, J. et al. Equity in community health insurance schemes: Evidence and lessons from Armenia. Health Policy Plan. 24, 209–216 (2009).
Bodhisane, S. & Pongpanich, S. The impact of National Health Insurance upon accessibility of health services and financial protection from catastrophic health expenditure: A case study of Savannakhet province, the Lao People’s Democratic Republic. Health Res. Policy Syst. 17, 99 (2019).
Tsutsué, S., Tobinai, K., Yi, J. & Crawford, B. Comparative effectiveness study of chemotherapy in follicular lymphoma patients in the rituximab era: A Japanese claims database study. Future Oncol. Lond. Engl. 17, 455–469 (2021).
Tsutsué, S., Suzuki, T., Kim, H. & Crawford, B. Real-world assessment of myelodysplastic syndrome: Japanese claims data analysis. Future Oncol. Lond. Engl. 18, 93–104 (2022).
Helmi, M. A. & Burton, S. Cost control under the DRG system. Hosp. Health Serv. Adm. 33, 263–269 (1988).
Sun, X. & Zhu, Y. DRG-oriented mathematical calculation model and method of integrated medical service cost. Comput. Math. Methods Med. 2020, 1–9 (2020).
Zeng, S., Luo, L., Fang, Y. & He, X. Cost control of treatment for cerebrovascular patients using a machine learning model in Western China. J. Healthc. Eng. 2021, 1–8 (2021).
Lecocq, Q. et al. Theranostics in immuno-oncology using nanobody derivatives. Theranostics 9, 7772–7791 (2019).
Yang, L., Ning, Q. & Tang, S. Recent advances and next breakthrough in immunotherapy for cancer treatment. J. Immunol. Res. 2022, 1–9 (2022).
Nesline, M. K., Knight, T., Colman, S. & Patel, K. Economic burden of checkpoint inhibitor immunotherapy for the treatment of non-small cell lung cancer in US Clinical Practice. Clin. Ther. 42, 1682-1698.e7 (2020).
Wu, X. et al. Immunotherapy improved cancer related pain management in patients with advanced Hepato-Pancreatic Biliary Cancers: A propensity score-matched (PSM) analysis. Front. Oncol. 12, 914591 (2022).
Lee, J. et al. Are there any ethnic differences in the efficacy and safety of immune checkpoint inhibitors for treatment of lung cancer?. J. Thorac. Dis. 12, 3796–3803 (2020).
Yang, Z. et al. The signaling pathways and targets of traditional Chinese medicine and natural medicine in triple-negative breast cancer. J. Ethnopharmacol. 264, 113249 (2021).
Huang, Y. et al. Progress in Traditional Chinese Medicine for the treatment of migraine. Am. J. Chin. Med. 48, 1731–1748 (2020).
Wu, S.-W., Pan, Q. & Chen, T. Research on diagnosis-related group grouping of inpatient medical expenditure in colorectal cancer patients based on a decision tree model. World J. Clin. Cases 8, 2484–2493 (2020).
Zhang, L. & Sun, L. Impacts of diagnosis-related groups payment on the healthcare providers’ behavior in China: A cross-sectional study among physicians. Risk Manag. Healthc. Policy 14, 2263–2276 (2021).
Kazberouk, A., Sagy, I., Novack, V. & McGuire, K. Understanding the extent and drivers of interphysician cost variation for spine procedures. Spine 41, 1111–1117 (2016).
Tsugawa, Y., Jha, A. K., Newhouse, J. P., Zaslavsky, A. M. & Jena, A. B. Variation in physician spending and association with patient outcomes. JAMA Intern. Med. 177, 675 (2017).
Huerta, T. R., Ford, E. W., Peterson, L. T. & Brigham, K. H. Testing the hospital value proposition: An empirical analysis of efficiency and quality. Health Care Manage. Rev. 33, 341–349 (2008).
Cheng, S.-H., Chen, C.-C. & Chang, W.-L. Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy 92, 158–164 (2009).
Siciliani, L., Sivey, P. & Street, A. Differences in length of stay for hip replacement between public hospitals, specialised treatment centres and private providers: Selection or efficiency?. Health Econ. 22, 234–242 (2013).
Dafny, L. & Dranove, D. Do report cards tell consumers anything they don’t know already? The case of Medicare HMOs. Rand J. Econ. 39, 790–821 (2008).
Moriya, A. S., Vogt, W. B. & Gaynor, M. Hospital prices and market structure in the hospital and insurance industries. Health Econ. Policy Law 5, 459–479 (2010).
Yu, L. & Lang, J. Diagnosis-related Groups (DRG) pricing and payment policy in China: Where are we?. Hepatobiliary Surg. Nutr. 9, 771–773 (2020).
Al-Khalil, O., Valeri, F., Senn, O., Rosemann, T. & Di Gangi, S. Effects of a DRG-based hospital reimbursement on the health care utilization and costs in Swiss primary care: A retrospective “quasi-experimental” analysis. PLOS ONE 15, e0241179 (2020).
Funding
The funding for this research was provided by the 2024 Hangzhou Philosophy and Social Science Planning Project (Z24YD055) and the Zhejiang Provincial College Student Science and Technology Innovation Activity Program (2024R410A053). The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by X.H.M., D.W., T.P., X.H.L., W.L., and X.Y.Z., who also designed its framework. X.Y.Z., X.Y.X., and K.Y.S. performed the data analysis, ensuring data integrity and accuracy. The manuscript was crafted by X.Y.Z., X.Y.X., and K.Y.S., integrating findings with scholarly discourse. X.H.M. and D.W. provided supervision and project leadership. All authors approved the final manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the affiliation, which was incorrectly given as ‘College of Humanities and Management, Zhejiang University of Chinese Medicine, Hangzhou 311402, China’. The correct affiliation is: ‘College of Humanities and Management, Zhejiang Chinese Medical University, Hangzhou 311402, China’.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zheng, X., Xiao, X., Shen, K. et al. Impact of Diagnosis-Related Groups (DRG) reform on cost homogeneity of treatment for patients with malignant tumours. Sci Rep 14, 21212 (2024). https://doi.org/10.1038/s41598-024-71917-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-71917-y
Keywords
This article is cited by
-
Impact of a new case-based payment scheme on volume distribution across public hospitals in Zhejiang, China: does ‘Same disease, same price’ matter
International Journal for Equity in Health (2025)