Abstract
There is little known about the contribution of exosomal microRNAs (exomiRs) in the children’s cardiac surgery-associated acute kidney injury (CSA-AKI). This study aimed to find diagnostic biomarkers for predicting CSA-AKI in children. A prospective observational study was conducted from April 2020 to March 2021.According to the changes of serum creatinine (SCr) value and urine volume within 48 h, the children were divided into acute kidney injury (AKI) group and non-AKI group. Serum samples were collected 4 h after cardiac surgery. Isolation of extracellular vesicles (EVs) and extraction of exomiRs from serum samples. Illumina high-throughput sequencing was used to quantify exomiRs and screen candidate microRNAs (miRNAs). Expression levels of candidate miRNAs were validated using droplet digital polymerase chain reaction (ddPCR). Normal and injuried rats’ kidney tissue were collected for tissue validation. In the pre-experimental stage (4 AKI vs. 4 non-AKI), hsa-miR-184, hsa-miR-4800-3p, hsa-miR-203a-3p and hsa-miR-6766-3p were selected as candidate genes. In the verification stage (8 AKI vs. 12 non-AKI), the expression of hsa-miR-184 in AKI group was significantly lower than that in non-AKI group (P = 0.031), and the expression of hsa-miR-4800-3p and hsa-miR-6766-3p in AKI group was significantly higher than that in non-AKI group (P = 0.01 and P = 0.047). There was no significant difference in the expression of hsa-miR-203a-3p between the two groups (P > 0.05). The expression of rats’ kidney tissue rno-miR-184 in AKI group was significantly lower than that in the normal group (P = 0.044). The area under the curve (AUC) of AKI predicted by hsa-miR-184 is 0.7865 and the AUC of hsa-miR-6766-3p is 0.7708. Combined with two kinds of miRNAs, the area under the curve of AKI is predicted to be 0.8646. The change of exomiRs level in circulatory system occurred in the early stage after cardiac operation, and the changes of hsa-miR-184 and hsa-miR-6766-3p content in circulatory system could predict CSA-AKI well.
Similar content being viewed by others
Introduction
Acute renal injury (AKI) is a clinical syndrome characterized by rapid increase of serum creatinine, decreased urine volume or both caused by a sharp decrease in glomerular filtration rate in a short time1. With the rapid development of critical care, the risk of death associated with AKI decreases significantly, but the long-term prognosis of surviving patients is still not optimistic2. Studies have shown that 8 ~ 16% of patients with acute renal injury will progress to chronic renal failure3. Moreover, AKI has become a major public health problem in the world4.
More than 2 million heart surgeries are performed worldwide each year5, The incidence of acute renal injury (CSA-AKI) after cardiac surgery is as high as 40%, which is the main cause of AKI, and about 3% of patients need at least temporary renal replacement therapy (RRT)6. Therefore, early screening of CSA-AKI patients will help to reduce perioperative mortality, reduce Intensive Care Unit (ICU) hospitalization days, and reduce medical expenses7.
Exosomes, originated from intraluminal vesicles produced by invagination of multivesicular bodies, and it is a kind of extracellular vesicles with a diameter of 50–150 nm and wrapped in lipid bilayers.The main function of exosomes is intercellular communication, transporting a wide range of biomolecules, including.
microRNAs (miRNAs)8. Exosomal miRNAs (exomiRs) is very stable in the circulatory system and has attracted wide attention as soon as it is discovered. Previous studies have found that exomiRs is usually tumor-specific9. In recent years, some scholars have found that miRNAs is also a good biomarker of skeletal system, respiratory system and other diseases10,11, but exomiRs as a biomarker in patients with AKI has not been reported.
Therefore, we designed a targeted experiment to study the changes of exomiRs in the circulatory system of children with CSA-AKI, looking for biomarkers that can early predict and diagnose the occurrence of AKI, with a view to early intervention to prevent disease progression.
Methods
Study design
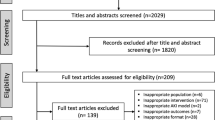
In this prospective study, we collected blood samples from children under the age of 18 who underwent heart surgery at Shanghai Children’s Medical Center between April 2020 and March 2021. The exclusion criteria were preoperative renal dysfunction and urinary diseases such as renal tumor, independent kidney, nephritis and so on. The children were divided into two groups by comparing the preoperative and postoperative serum creatinine (SCr) levels and postoperative urine volume. The baseline SCr value was the latest SCr measurement before the cardiac operation, and the blood SCr level was measured 24 and 48 h after the operation. According to 2012 Kidney Disease: Improving Global Outcomes (KDIGO) AKI Guide12, children with AKI are those who meet the following conditions:1. increase in SCr by ≥ 0.3 mg/dl (≥ 26.5 µmol/l) within 48 h; or 2. increase in SCr to ≥ 1.5 times baseline, which is known or presumed to have occurred within the prior 7 days; or 3. urine volume < 0.5 ml/kg/hour for 6 h. Those who do not meet the above conditions are children with non-AKI. Finally, there were 30 children were initially enrolled in this study, 2 children did not meet the inclusion criteria. 8 serum samples (4 AKI and 4 non-AKI) were used in discovery phase and 20 samples (8 AKI and 12 non-AKI children) in validation phase.
Serum samples collection
At 4 h after cardiac surgery, blood samples were collected for about 4 ml. Peripheral venous blood was collected in Ethylenediaminetetraacetic acid-tube (EDTA-tube) (BD Vacutainer SST ™). After standing at room temperature for 30 min, blood samples were centrifuged at 3000 g at room temperature for 10 min. The upper liquid (serum) was frozen at − 80 °C until further analysis.
Exosomes isolation and identification
Exosome extraction was performed according to the protocol of the PureExo® Exosome Isolation kit (for serum). Detailed steps can be found in the supplementary material. After isolating the exosomes, we measured the exosome particle size and concentration using nanoparticle tracking analysis (NTA) at VivaCell Shanghai with ZetaView PMX 110 (Particle Metrix, Meerbusch, Germany) and corresponding software ZetaView 8.04.02. Isolated exosome samples were appropriately diluted using 1X phosphate buffer saline (PBS) buffer (Biological Industries, Israel) to measure the particle size and concentration. NTA measurement was recorded and analyzed at 11 positions. The ZetaView system was calibrated using 110 nm polystyrene particles. Temperature was maintained around 25℃. In addition, exosomes were fixed with 2.5% glutaraldehyde for 2 h. After cleaning, the centrifuge radius was 12.8 cm, 10,000×g 4℃, centrifuged for 1 h, then re-suspended, then placed on the copper net, washed with double distilled water, negatively stained with 3% phosphotungstic acid at room temperature for 1 min, and observed under transmission electron microscopy (TEM) after drying.
miRNAs illumina sequencing
In this step, we sequenced the miRNAs in each individual sample one by one. About 2644 miRNAs were detected in each sample and 692 of them showed significant difference, which false discoverer rate (FDR) < 0.05. Detailed steps and sequencing result can be found in the supplementary material. Total RNA was extracted using exoRNeasy Midi Kit (Cat#77144, Qiagen). RNA quality was checked using Agilent 4200 TapeStation (Agilent technologies, Santa Clara, CA, US) according to standard procedures. Quantification of exomiRs using Illumina high-throughput sequencing. Sequencing libraries were constructed by QIAseq miRNA Library Kit for Illumina (Cat #331505, Qiagen) according to manufacturer’s instructions. The sequencing was performed on an Illumina NovaSeq platform (Illumina, San Diego, CA, USA). Finally, the expression of miRNA, piRNA and SmallRNA was normalized to CPM, which was calculated and analysed by edgeR.
Droplet digital polymerase chain reaction (ddPCR) in validation phase
ddPCR technology is based on Poisson distribution to absolutely quantify the miRNAs without relying on calibration curve, which uses the same primers, probes, Taq polymerase, and reagents as conventual PCR to amplify the target DNA fragment, but its sensitivity and repeatability are more significant, Candidate miRNAs with |log2foldchange(FC)|≥3.0 and p-value < 0.05 were selected to validate their circulating expression levels by droplet digital polymerase chain reaction (ddPCR). Primers of miRNAs were synthesized by Sangon Biotech. Reverse transcription of miRNA was performed using miRNA 1st Strand cDNA Synthesis Kit (by tailing A) (Vazyme Cat#: MR201-02, Nanjing, Jiangsu, China). EvaGreen Supermix (Biorad Cat#: 186–4035)10 µl, forward and reverse primers 0. 2 µl (10µM), cDNA, and RNase free water were mixed in 20 µl solution. The automated Droplet G enerator (Bio-Rad) was used for emulsification. After the 96-well plate was loaded on to and read by a QX200 Droplet Reader (Bio-Rad), results were analyzed using QuantaSoft™Analysis Pro (Bio-Rad). miR-126-3p was selected as internal miRNA to adjust for loading error. The ddPCR uses absolute quantitative principles, so each miRNA expression level was normalized using the following formula: miRNA expression/the average of the internal miRNAs expression. The ddPCR result can be found in the supplementary material.
Rat tissue real-time polymerase chain reaction (rtPCR) in validation phase
Due to the homology between hsa-miR-184 and rno-miR-184, we selected 16 male Sprague-Dawley rats (SD rats) aged 8 weeks (180–200 g), purchased from Shanghai Jihui Experimental Animal Breeding Co., Ltd, for animal experiments. All the experimental rats lived in a suitable temperature and humidity environment with a normal diet and were randomly divided into two groups of eight animals each. A mid-abdominal incision was adopted for removal of right kidney and occlusion of left renal pedicle for 45 min, which was retained as AKI group specimen 24 h later. Normal left kidney tissues were extracted directly from 8 rats as normal group specimens. All samples were frozen at −80 ℃ until rtPCR. miRNAs were extracted by TRIzol reagent (Invitrogen), cDNA was synthesized by M-MLV reverse transcriptase (Promega), and ABI Steponeplus was used for fluorescence quantitative PCR analysis. All the SD rats were euthanized by carbon dioxide asphyxiation.
Statistical analysis
Continuous variables were presented as means ± standard deviation in the case of normal distribution or median (interquartile range; IQR1–3) in the case of non-normally distribution. Student’s t-test or Mann–Whitney U test was used to analyze the differences between continuous variables. Categorical variables were presented as numbers (percentages) and were compared using the Chi-square test. The receiver operating characteristic (ROC) curve and the area under the curve (AUC) were plotted to evaluate the predictability of miRNAs for AKI. A p-value of less than 0.05 was considered statistically significant. All statistical analysis was performed with SPSS 26.0 statistical software (IBM, Chicago, IL, USA) and figures were drawn.
using GraphPad Prism GraphPad Prism 9 software (Graph pad software Inc., San Diego, CA, USA).
Results
Demographic and clinical characteristics of the study population
Demographic data of the validating cohort are presented in Table 1. We found that there were no significant difference in age, sex, BMI, type of primary disease, mean arterial pressure, operative temperature, bypass time, aortic cross-clamping time, preoperative hematocrit (HCT), blood urea nitrogen (BUN) and SCr levels between the two groups.
NTA and TEM result of exosomes
The NTA and TEM results of exosomes of the two groups of samples are shown in Fig. 1.
Expression of miRNAs
In the discovery phase, there were significant differences in the expression of 31 miRNA (P < 0.05 and |log2FC|≥3.0, Fig. 2A). Figure 2B shows a hierarchical clustering heat map of differential genes. Excluding the miRNA with very low expression in most of the samples, we finally chose hsa-miR-184, hsa-miR-4800-3p, hsa-miR-203a-3p and hsa-miR-6766-3p for ddPCR verification.
Validation of miRNAs
The relative expression of miRNAs in the two groups is shown in Fig. 3. The expression of hsa-miR-184 in AKI group was significantly lower than that in non-AKI group (P = 0.031), while the expression of hsa-miR-4800-3p and hsa-miR-6766-3p in AKI group was significantly higher than that in non-AKI group (P = 0.01,P = 0.047). There was no significant difference in the expression of hsa-miR-203a-3p between the two groups (P = 0.27).
Expression of rats’ tissue miRNA
The expression of miR-184 in SD rats’ kidney tissue is shown in Fig. 4. The expression of rno-miR-184 in AKI group was significantly lower than that in the normal group (P = 0.044).
ROC of miRNAs
According to the verification results, we choose hsa-miR-184 and hsa-miR-6766-3p as biomarkers to predict AKI. The ROC curves of the two miRNAs are shown in Fig. 5. The area under curve (AUC) of AKI predicted by hsa-miR-184 alone was 0.7865 and hsa-miR-6766-3p was 0.7708, while the area under curve of AKI was predicted by combining two kinds of miRNAs to be 0.8646. Table 2 shows the cutoff value, sensitivity, specificity and Jordan index of miRNA as a marker. For the prediction of AKI, the performance of two miRNA combines is higher than that of separate diagnosis of the two kinds of miRNA.
Discussion
The incidence of CSA-AKI is high due to vascular changes, organ ischemia-reperfusion injury or nephrotoxic agents after cardiac surgery13. The study found that cardiac surgery is the second largest risk factor for the occurrence of AKI in intensive care unit14,15. Through this prospective study, we found that the content of serum exosomal miRNA changed significantly in the early stage of CSA-AKI. At 4 h after cardiac surgery, the level of hsa-miR-184 in AKI group was significantly lower than that in non-AKI group, while hsa-miR-6766-3p increased significantly. The changes of these two miRNA levels were significantly correlated with the occurrence of AKI, especially when the two miRNAs were combined, the diagnostic efficiency was higher, the AUC was 0.8646. This result suggests that the change of miRNA level can well predict the occurrence of AKI in the early stage after cardiac surgery (4 h after surgery).
In the screening stage, we found that the content of miR-4800-3p in AKI group was lower than that in non-AKI group (P < 0.05, |log2FC|≥3). However, in the verification stage, the content in AKI group was higher than that in non-AKI group (p = 0.01). The possible reasons are: (1) measurement error caused by low exomiRs content in screening stage, or (2) systematic error caused by outliers of miRNAs content in verification phase (Fig. 2). The difference in the content of miRNA between the two groups still needs to be verified by more samples, so we did not conduct further ROC analysis of the gene.
In order to clarify the expression difference of miRNA in kidney tissues, and the reason that human kidney tissues were difficult to obtain, we chose animal experiments for verification finally. At the same time, due to the homology of human and mouse genes, only hsa-miR-184 was selected for verification. We found that the expression level of hsa-miR-184 in the kidney tissues of the two groups of SD rats was significantly lower in the AKI group than in the normal group, which was consistent with the results in serum samples.
The role of hsa-miRNA-184 and hsa-miR-6766-3p in CSA-AKI is yet unclear. In order to understand the biological function of differentially expressed genes, we performed enrichment analysis based on the KEGG database. The signal pathways of enrichment include Prion diseases, Thyroid hormone signaling pathway, Circadian entrainment, other types of O-glycan biosynthesis, arginine and proline metabolism (Fig. 6). Studies have shown that hsa-miR-184 is among the top downregulated microRNAs in the blood of patients following ischemic stroke. The expression of hsa-miR-184 is significantly altered in the brain following ischemic stroke in rats16 and promote the occurrence of brain injury by targeting PPAP2B after ischemic stroke in male rats17. In addition, some studies have shown that hsa-miR-184 regulates glucose metabolism by targeting PKM2 pathway and plays a role in renal clear cell carcinoma18. Hsa-miR-6766-3p regulates hepatic fibrosis by targeting TGFβ RII-SMADS pathway19. As for the pathogenic mechanism of these two miRNAs in AKI, further experimental study is still needed.
This is not the first experiment to study the change of miRNA level during AKI. But the unique features of this study are that the research objects are children without complicated diseases, that patients’ serum samples are used at all stages of the experiment, and that the changes of miRNAs level were detected within 4 h after surgery, thus achieving early diagnosis. At the same time, the application of ddPCR technology reduces the systematic error20.
Previous studies have also found changes in the content of different miRNA in the course of AKI. For example, Liu et al.21 found that hsa-miR-452 is an effective biomarker of septic AKI, AUC = 0.8985. Gaede et al.22 found that the content of hsa-miR-21 before cardiac surgery can predict the occurrence of AKI. However, most of the subjects in these studies are middle-aged or even elderly patients, who are often associated with other underlying diseases. The difference of baseline characteristics will affect the accuracy of the results. Also, the target miRNA of Liu et al. was discovered in vitro, and Gaede et al. selected the target gene obtained from cancer disease23, which does not guarantee that the two targets miRNA are the most significant differences in the process of AKI.
As mentioned earlier, the particularity of the research objects, the homogeneity of the experimental samples and the accuracy of the experimental method all make our experimental results reliable, and it could also provide reference for later research.
Conclusion
To sum up, this study found that there were changes in the level of exomiRs in the circulatory system in the early stage after cardiac operation, and the changes of hsa-miR-184 and hsa-miR-6766-3p in the circulatory system could be a good predictor of CSA-AKI.
Data availability
The sequencing data were deposited in the Genome Expression Omnibus (GEO) under accession GSE268959 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi).
References
Masewu, A. et al. Acute kidney injury is a powerful independent predictor of mortality in critically ill patients: A multicenter prospective cohort study from Kinshasa, the Democratic Republic of Congo. BMC Nephrol. 17(1):118. Published 2016 Aug 24. doi: (2016). https://doi.org/10.1186/s12882-016-0333-4
Al-Jefri, M., Lee, J. & James, M. Predicting Acute kidney Injury after surgery. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc.2020, 5606–5609. https://doi.org/10.1109/EMBC44109.2020.9175448 (2020).
Hoste, E. A. J. et al. Global epidemiology and outcomes of acute kidney injury. Nat. Rev. Nephrol.14(10), 607–625. https://doi.org/10.1038/s41581-018-0052-0 (2018).
Ba Aqeel, S. H., Sanchez, A. & Batlle, D. Angiotensinogen as a biomarker of acute kidney injury. Clin. Kidney J.10(6), 759–768. https://doi.org/10.1093/ckj/sfx087 (2017).
Yu, Y. et al. Diagnosis, pathophysiology and preventive strategies for cardiac surgery-associated acute kidney injury: A narrative review. Eur. J. Med. Res.28(1), 45. https://doi.org/10.1186/s40001-023-00990-2 (2023). Published 2023 Jan 24.
Vandenberghe, W. et al. Acute kidney injury in cardiorenal syndrome type 1 patients: A systematic review and Meta-analysis. Cardiorenal Med.6(2), 116–128. https://doi.org/10.1159/000442300 (2016).
Ortega-Loubon, C., Fernández-Molina, M., Carrascal-Hinojal, Y. & Fulquet-Carreras, E. Cardiac surgery-associated acute kidney injury. Ann. Card Anaesth.19(4), 687–698. https://doi.org/10.4103/0971-9784.191578 (2016).
van Niel, G., D’Angelo, G. & Raposo, G. Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell. Biol.19(4), 213–228. https://doi.org/10.1038/nrm.2017.125 (2018).
Falcone, G., Felsani, A. & D’Agnano, I. Signaling by exosomal microRNAs in cancer. J. Exp. Clin. Cancer Res.34(1), 32. https://doi.org/10.1186/s13046-015-0148-3 (2015). Published 2015 Apr 2.
Ciuffi, S. et al. Circulating MicroRNAs as biomarkers of osteoporosis and fragility fractures. J. Clin. Endocrinol. Metab.107(8), 2267–2285. https://doi.org/10.1210/clinem/dgac293 (2022).
Vázquez-Mera, S. et al. Serum exosome inflamma-mirs are surrogate biomarkers for asthma phenotype and severity. Allergy 78(1), 141–155. https://doi.org/10.1111/all.15480 (2023).
Kellum, J. A., Lameire, N. & KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit Care. 17(1):204. Published 2013 Feb 4. doi: (2013). https://doi.org/10.1186/cc11454
Wang, Y. & Bellomo, R. Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat. Rev. Nephrol.13(11), 697–711. https://doi.org/10.1038/nrneph.2017.119 (2017).
Mao, H. et al. Cardiac surgery-associated acute kidney injury. Cardiorenal Med.3(3), 178–199. https://doi.org/10.1159/000353134 (2013).
Hobson, C. E. et al. Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119(18), 2444–2453. https://doi.org/10.1161/CIRCULATIONAHA.108.800011 (2009).
Kojabad, A. A. et al. Droplet digital PCR of viral DNA/RNA, current progress, challenges, and future perspectives. J. Med. Virol.93(7), 4182–4197. https://doi.org/10.1002/jmv.26846 (2021).
Liu, Z. et al. Discovery and validation of miR-452 as an effective biomarker for acute kidney injury in sepsis. Theranostics10(26), 11963–11975. https://doi.org/10.7150/thno.50093 (2020). Published 2020 Oct 25.
Gaede, L. et al. Plasma microRNA-21 for the early prediction of acute kidney injury in patients undergoing major cardiac surgery. Nephrol. Dial Transpl.31(5), 760–766. https://doi.org/10.1093/ndt/gfw007 (2016).
Lai, J. Y. et al. MicroRNA-21 in glomerular injury. J. Am. Soc. Nephrol.26(4), 805–816. https://doi.org/10.1681/ASN.2013121274 (2015).
Wang, N. et al. 3D hESC exosomes enriched with miR-6766-3p ameliorates liver fibrosis by attenuating activated stellate cells through targeting the TGFβRII-SMADS pathway. J. Nanobiotechnol. 19(1):437. Published 2021 Dec 20. doi: (2021). https://doi.org/10.1186/s12951-021-01138-2
Wang, K. et al. Melatonin enhances the therapeutic effect of plasma exosomes against cerebral Ischemia-induced pyroptosis through the TLR4/NF-κB pathway. Front. Neurosci.14, 848. https://doi.org/10.3389/fnins.2020.00848 (2020). Published 2020 Aug 18.
Yang, H. et al. Mir-184 contributes to Brain injury through targeting PPAP2B following ischemic stroke in male rats. Front. Mol. Neurosci.14, 613887. https://doi.org/10.3389/fnmol.2021.613887 (2021). Published 2021 Mar 23.
Zanchi, C. et al. MicroRNA-184 is a downstream effector of albuminuria driving renal fibrosis in rats with diabetic nephropathy. Diabetologia60(6), 1114–1125. https://doi.org/10.1007/s00125-017-4248-9 (2017).
Acknowledgements
This work was supported by grants from the Pudong New Area Science and Technology Development Fund (PKJ2020-Y04), and Natural Science Foundation of Fujian Province (2023J01183). the Tai-Shan Scholar Program from Shandong Province (tsqn202103116), and Program of Scientific and Technological Development of Weifang 2023GX026.
Author information
Authors and Affiliations
Contributions
XYZ and JS contributed to conception and design of the study.PTL organized the database, FY and WG performed the statistical analysis.PTL and KPB wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Approval of the research protocol by an institutional Reviewer Board
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Shanghai Children’s Medical Center (protocol code SCMCIRB-K2019068-1). All patients or their guardians have signed relevant informed consent forms. The animal study protocol was approved by the Ethics Committee of Shanghai Ch’ldren’s Medical Center (protocol code SCMCIRB-Y2019005 and 2019 of approval), and all methods were carried out in accordance with relevant guidelines and regulations and reported in accordance with ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pengtao, L., Kaiping, B., Fei, Y. et al. Plasma-derived exosomal hsa-miR-184 and hsa-mir-6766-3p as promising diagnostic biomarkers for early detection of children’s cardiac surgery-associated acute kidney injury. Sci Rep 14, 22387 (2024). https://doi.org/10.1038/s41598-024-72737-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-72737-w