Abstract
A body Shape index (ABSI), defined as waist circumference (WC)/(body mass index (BMI)2/3 × height1/2), is unique in that the ABSI is positively associated with visceral obesity and is independent of BMI. The ABSI has also been shown to be positively and linearly correlated with the amount of visceral adiposity in the general population and with all-cause and cardiovascular disease (CVD). However, it is uncertain whether ABSI is associated with periodontitis in hypertensive patients. A cross-sectional study of 2,482 hypertensive patients (mean age 65.2 ± 9.1 years) was conducted using the ABSI Z score, periodontitis as a dichotomous variable, the ABSI Z score as a continuous variable, and multiple covariates such as age, gender, and race. The data were analyzed using descriptive statistics, multiple regression model, subgroup analysis with EmpowerStats (version 4.2), and curve transformation plots were generated. In multiple regression model analysis, ABSI Z score showed a significant positive association with periodontitis in the hypertensive population in all three models. When ABSI Z score was divided into low, moderate, and high three groups, we observed that those with the highest ABSI Z score had a 20% increased risk of periodontitis among people with hypertension (OR 1.2; 95% CI 1.0, 1.5; p = 0.046). We used smooth curve fitting to confirm the results and found that these results were still supported, and additional subgroup analyses showed that the positive association between ABSI Z score and periodontitis in hypertensive population was stable and consistent in the general population. The present cross-sectional investigation showed a positive association between ABSI Z score and periodontitis in a hypertensive population.
Similar content being viewed by others
Introduction
Periodontitis is a prevalent disease that affects more than 40% of adults in the United States, and globally, the severe form of the disease affects 11.2% of the population, making it the sixth most common human disease in the world1,2. The main risk factors for periodontal disease are poor oral hygiene among others3. People with periodontal disease experience symptoms such as pain and discomfort in the mouth, and if the condition is not treated, it can lead to loss of attachment resulting in periodontitis4.
Periodontitis and hypertension are among the most common non-communicable chronic diseases in the world5. In addition to common risk factors, a growing body of evidence supports a possible association between the two diseases6. The inflammatory response caused by periodontitis may lead to elevated levels of systemic inflammation, which can affect vascular function and blood pressure regulation7. Periodontitis and hypertension share common risk factors, including genetic predisposition, advanced age, and unhealthy lifestyle choices like poor dietary habits and lack of physical activity5. These factors may play an important role in the development of both diseases.
In recent years, the ABSI has emerged as a pivotal indicator for assessing body fat distribution and its health implications, offering a more comprehensive approach than the traditional BMI8. The ABSI’s multidimensional measurement, which includes waist circumference data, provides a nuanced assessment that reveals a positive correlation with visceral obesity9, cardiovascular disease risk, and all-cause mortality10. Unlike BMI, which does not differentiate between muscle and fat11,12, the ABSI considers the ratio of waist circumference to BMI and height, offering a more accurate representation of body fat distribution and its association with chronic disease risk13. This index has proven to be a more effective predictor of the health effects of obesity, where an increase in ABSI is linked to a significant increase in mortality, highlighting the insufficiency of relying solely on body weight for health risk prediction14. In addition the ABSI is important in assessing roundness and visceral fat accumulation, and its waist circumference as a proportion of the roundness index has received attention, emphasizing its scientific relevance in assessing the health effects of obesity15. Furthermore, periodontal diseases, closely intertwined with overall health, including cardiovascular aspects like hypertension16, has prompted researchers to explore the relationship between ABSI and various health outcomes. While the ABSI has been primarily used to assess cardiovascular disease, revealing a strong association17, its application in evaluating periodontitis has been less explored.
This study addresses this gap by investigating the relationship between ABSI Z score and periodontitis in a hypertensive population. Given the ABSI’s unique value in assessing the potential impact of obesity on chronic inflammatory diseases18, we believe it to be an excellent choice of indicator for this research. By doing so, we aim to contribute to a better understanding of how body fat distribution, as measured by ABSI, may influence periodontal health, thereby enriching the evidence base for preventive and clinical strategies in both hypertension and periodontal disease management.
Methods
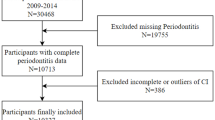
The study used data from the National Health and Nutrition Examination Survey (NHANES), approved by the Research Ethics Review Board of the National Center for Health Statistics. All methods were conducted in accordance with relevant guidelines, and all participants provided written permission at recruitment19 (NHANES—NCHS Research Ethics Review Board Approval (cdc.gov)). The initial analysis of the study involved periodontitis data from 30,468 participants from 2009 to 2014. Inclusion criteria for the study included participants being 30 years of age and older and taking anti-hypertensive medications; NHANES participants received waist circumference, BMI, and height measurements; and participants received a periodontal exam during the oral health screening portion of the program. Exclusion criteria included participants who did not receive a complete periodontal exam or who received an exam but were not taking hypertension medication; very few participants were missing covariates such as education, marriage, hypertension, and sleep disorders. Ultimately, after screening, the study yielded a sample of 2,482 eligible individuals (Fig. 1).
Classification of periodontitis
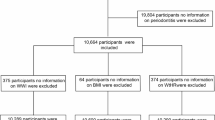
According to the NHANES guidelines, only subjects 30 years of age and older underwent a full-mouth periodontal examination in which the loss of attachment and pocket depth around each tooth was measured20. Based on criteria provided by the CDC/AAP Case Definitions (Centers for Disease Control and Prevention/American Academy of Periodontology), we categorized periodontal status as mild, moderate, severe periodontitis, and no periodontitis. The detailed method of grading periodontitis is shown in Fig. 221. Absence of periodontitis and mild inflammation were defined as having no periodontitis, whereas moderate and severe inflammation were defined as having periodontitis22.
Definition of a body shape index (ABSI)
The body shape index (ABSI) is an index used to assess the relationship between body shape and health risk, and was proposed by researchers at the City University of New York in 2012. ABSI normalizes waist circumference (WC) to body size by considering both weight and height, similar to how body mass index (BMI) normalizes weight in relation to height. ABSI is statistically independent of BMI, while the variability in non-normalized WC is largely explained by BMI23. We defined ABSI as derived from the NHANES reference population24:
where W refers to the weight, H refers to the height, and WC stands for waist circumference.
We converted the ABSI into ABSI Z score based on the scores and categorized them into low, moderate, and high groups: low (ABSI Z score < − 0.272), moderate (− 0.272 ≤ ABSI Z score < 0.229), and high (ABSI Z score ≥ 0.229)25, thus following the general formula:
Covariates
We combined 10 confounding factors that may influence the relationship between periodontitis and hypertension, including gender, age, race, education, marital status, annual alcohol consumption, general health condition, number of flossing/a week, fatigue/a week, general health condition26. A detailed description of the covariates can be found on the NHANES website.
Statistical analysis
We integrated and statistically analyzed the data using the EmpowerStats (version 4.2; https://www.empowerstats.net/cn/) and R software (version 4.3.2; https://www.r-project.org/) packages. Continuous data were described using mean, standard deviation (SD), and median; categorical variables were described using frequency. To illustrate disparities and association between Non-/mild periodontitis and Moderate/severe periodontitis, chi-square tests should be used for categorical variables, one-way analysis of variance for variables with a normal distribution, and Kruskal–Wallis test for variables with a skewed distribution. We developed a multiple regression model to investigate the independent relationship between ABSI Z score and moderate/severe periodontitis in a hypertensive population. The strength of the relationship was determined by calculating the odds ratio (OR) with 95% confidence intervals, and ABSI Z score was categorized into three classes, with the lower class serving as the reference. We developed three models: model I was not adjusted for covariates; model II was adjusted for gender, age, marital status, education level and race; and model III added other covariates to model II, such as annual alcohol consumption, general health condition, number of flossing/a week, fatigue/a week, general health condition. We also applied a smoothed curve transformation to explore the possible nonlinear relationship between ABSI Z score and periodontitis. In this study, p < 0.05 were considered statistically significant.
Results
General characteristics of the study population
A total of 2,842 patients were included after applying appropriate exclusion criteria. Figure 1 illustrates the process of screening participants. Covariates were dichotomously distributed according to no/mild or moderate/severe periodontitis. Table 1 summarizes the baseline characteristics of patients with and without periodontitis in the hypertensive population. Overall, there were significant differences between the no/mild periodontitis and moderate/severe periodontitis groups in terms of ABSI, ABSI Z-score, height, BMI, age, gender, race, marital status, education, number of flossing sessions, general health, and history of diabetes mellitus (p < 0.05). While there was no significant difference between waist circumference, Annual alcohol consumption, days of fatigue in a week, and sleep disorders (Table 1).
The association between ABSI Z-score and periodontitis in the hypertensive population
The relationship between ABSI Z-score and periodontitis in the hypertensive population is shown in Table 2, which is the result of multiple regression model. In the original model, ABSI Z-score was significantly and positively correlated with periodontitis, with a ratio of 1.2 (95 CI 1.1, 1.3, p < 0.001). The robust and favorable association in Model 2 remained highly significant (OR 1.1; 95% CI 1.0, 1.2; p = 0.006) after accounting for factors such as gender, age, and race. Then in Model 3, which was built on the basis of Model 2, after adjusting for all variables, the correlation between ABSI and periodontitis remained statistically significant (OR 1.1; 95% CI 1.0, 1.2; p = 0.015). After converting ABSI Z score from continuous to categorical variables, we observed a striking result. In all three models, the association between the high ABSI Z score group and periodontitis showed a statistically significant association. Participants in the highest group had a significant 20% increased risk of periodontitis compared to those in the low ABSI Z score group (OR 1.2; 95% CI 1.0, 1.5; p = 0.046). This study found that increased ABSI Z-score were positively associated with the risk of developing periodontitis in hypertensive population and we confirmed the results using smoothed curve fitting as shown in Fig. 3 and found that the multiple regression model of the results was still supported.
Subgroup analysis
To evaluate the stability of the relationship between ABSI score and periodontitis in hypertensive populations, as well as to identify potential differences between the two in different populations, subgroup analyses were conducted. The results of these analyses are presented in Fig. 4. Except for those who were male, widowed or divorced, rarely flossing, moderately flossing, and in excellent health, the ABSI Z score was significantly positively associated with periodontitis in hypertensives. Furthermore, we observed that the ‘interaction p-value’ was greater than 0.05, suggesting that the positive correlation between the ABSI Z score and periodontitis in the hypertensive population is typically stable and consistent across the general population.
Discussion
This cross-sectional study reveals for the first time a positive correlation between ABSI Z scores and periodontitis among hypertensive patients. By analyzing 2,482 participants, we found that as ABSI Z scores increased, so did the risk of periodontitis. This association remained significant after controlling for confounders such as age, gender, race, marital status, education, frequency of flossing and general health. The findings highlight the potential role of the ABSI in the development of periodontitis and provide important clues for future research and interventions.
In the past, the medical community used to widely use the body mass index, BMI, to measure the degree of obesity27. BMI is calculated as the weight divided by the square of the height, and the normal range of this index is from 18.5 to 24, and if it is more than 24, it is overweight, and if it is more than 28, it is obese28. In addition, the waist circumference indicator is used to measure central obesity29, men with a waist circumference of more than 90 centimeters and women with a waist circumference of more than 85 centimeters are abdominal obese30. It is evident that BMI, as well as WC, are relatively broad standards24,31. Therefore, scholars have been seeking more reliable and easy-to-use indicators. In recent years, the indicators used to measure the accumulation of visceral fat and its impact have become increasingly recognized31,32. Among them, the widely acknowledged indicator is the Body Shape Index (ABSI)33. ABSI was proposed by scholars from the City College of New York in 201224. ABSI has been suggested as an alternative parameter to reflect differences in body shape. Studies have indicated a positive correlation between ABSI and visceral fat, cardiovascular disease risk34, and all-cause mortality8. Many scholars have analyzed studies on large sample sizes in the US population, such as Aoki et al. who found that ABSI could predict the risk of CVD manifestations more significantly than BMI35. This was also confirmed in a study by Wu et al.36, who observed that anthropometric indicators including BMI, ABSI, etc. were strongly associated with hypertension risk, and that these new anthropometric indicators should be emphasized for better prevention and treatment of hypertension. Furthermore, a cross-sectional study by Lin et al.37 found that the score of ABSI was linearly correlated with the risk of kidney stone prevalence, which can be used as an important indicator for assessing the risk of kidney stones. Kuang et al.12. found that ABSI may help define the risk of sarcopenia in overweight/obese individuals. In addition, some scholars have found that the ABSI combined with BMI best identifies the risk of obesity-related non-alcoholic fatty liver disease (NAFLD) and is significantly better than BMI or WC or ABSI38. Therefore, ABSI should be more closely monitored and preventive medical management than BMI. In addition hypertension is one of the major risk factors for cardiovascular disease, Hamza et al.39. noted that genetic factors promote an individual’s predisposition to cardiovascular disease (hypertension, atherosclerosis, etc.) through epigenetic modifications including DNA methylation, and that periodontal disease such as chronic inflammation promotes DNA methylation and has been shown to be associated with an increased risk of cardiovascular disease40, therefore it is hypothesized that periodontitis and hypertension may also be determined by a combination of genetic factors and multiple risk factors. Therefore, this study was chosen to be conducted in a hypertensive population; however, no one has yet conducted an in-depth study of the relationship between the ABSI Z score and periodontitis in a hypertensive population, so there is no reason why the relationship between the ABSI Z score and periodontitis should not be explored. If feasible, the ABSI Z score could also be used as an indicator to assess oral health, especially periodontal health. Where possible, every effort has been made to explain how they are linked. The possible reasons are summarized as follows.
Obesity is characterized as a low-grade chronic inflammatory state41, and excessive accumulation of visceral adipose tissue contributes to vascular inflammation42, in which the body’s immune system is activated, leading to the release of inflammatory mediators and the onset of an inflammatory response43. These inflammatory mediators can circulate through the bloodstream to all parts of the body, including the periodontal tissues in the oral cavity44. In periodontal tissues, the release of inflammatory mediators causes vasodilatation, increased permeability, and infiltration of inflammatory cells, leading to an inflammatory response and damage to localized tissues45. The inflammatory response caused by vascular inflammation in the periodontal tissues may lead to symptoms such as red, swollen, and bleeding gums, which eventually develop into periodontitis46. In addition, changes in hormone levels, such as estrogen and cortisol, can affect the health of periodontal tissues47. Also, obesity may alter the composition of the oral microbiota, which may increase an individual’s susceptibility to periodontitis48. The effect of obesity on immune cell function should not be overlooked, as macrophages and lymphocytes, among others, play a crucial role in the pathogenesis of periodontitis49.
Limitations
Our study has three related limitations. First, due to the cross-sectional design, we were unable to establish a causal relationship between ABSI and periodontitis in a hypertensive population. Therefore, future studies should consider the use of longitudinal data to enhance understanding of changes in ABSI and its long-term effects on periodontal health. Second, the ABSI and periodontal examination data used in this study were derived from the 2009–2014 NHANES database, and we will continue to follow up on NHANES updates, if applicable, and perform relevant analyses to validate the most recent data. Finally, we were unable to apply the most recent classification criteria for periodontitis due to the lack of necessary imaging data. These limitations suggest that our understanding of the relationship between ABSI and periodontitis requires further study.
Conclusion
Data analysis revealed a significant positive correlation between ABSI Z scores and the risk of periodontitis in hypertensive patients. Specifically, hypertensive patients with higher ABSI Z scores had a 20% increased risk of periodontitis. This finding emphasizes the importance of maintaining a healthy weight for oral health in hypertensive patients. Therefore, these patients should receive more frequent periodontal examinations and aggressive treatment, including regular cleanings and lifestyle modifications. Suggesting that the ABSI Z score can be a valid predictor of the risk of periodontitis in specific populations, this study may help physicians manage the oral health of hypertensive patients more effectively and reduce the risk of worsening periodontitis.
Data availability
The complete dataset is accessible through the NHANES database, which can be located at the following link: https://www.cdc.gov/nchs/nhanes/index.htm.
Abbreviations
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- ABSI:
-
Body shape index
- NHANES:
-
National Health and Nutrition Examination Survey
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- AL:
-
Attached level
- CDC-AAP:
-
The Centers for Disease Control and Prevention and the American Academy of Periodontology
- NAFLD:
-
Non-alcoholic fatty liver disease
References
Kwon, T., Lamster, I. B. & Levin, L. Current concepts in the management of Periodontitis. Int. Dent. J. 71, 462–476. https://doi.org/10.1111/idj.12630 (2021).
Sanz, M. et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 47, 268–288. https://doi.org/10.1111/jcpe.13189 (2020).
Santacroce, L. et al. Oral microbiota in human health and disease: A perspective. Exp. Biol. Med. (Maywood N. J.) 248, 1288–1301. https://doi.org/10.1177/15353702231187645 (2023).
Janorkar, D. A. et al. Association between BMI and periodontitis in women living with or at risk for HIV. Spec. care Dent. Off. Publ. Am. Assoc. Hosp. Dent. Acad. Dent. Handicap. Am. Soc. Geriatr. Dent. 42 486–493. https://doi.org/10.1111/scd.12711 (2022).
Del Pinto, R. et al. Periodontitis and hypertension: Is the association causal? High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 27, 281–289. https://doi.org/10.1007/s40292-020-00392-z (2020).
Macedo Paizan, M. L. & Vilela-Martin, J. F. Is there an association between periodontitis and hypertension? Curr. Cardiol. Rev. 10, 355–361. https://doi.org/10.2174/1573403x10666140416094901 (2014).
Ozmeric, N. et al. Interaction between hypertension and periodontitis. Oral Dis. 30, 1622–1631. https://doi.org/10.1111/odi.14543 (2024).
Kazemian, E., Mehran, L., Masoumi, S., Amouzegar, A. & Azizi, F. Association of trajectory of body shape index with all-cause and cause-specific mortality: 18 years follow-up. Front. Endocrinol. 14, 1259849. https://doi.org/10.3389/fendo.2023.1259849 (2023).
Bouchi, R. et al. Indirect measure of visceral adiposity ‘A body shape index’ (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. BMJ open. Diabetes Res. Care 4, e000188. https://doi.org/10.1136/bmjdrc-2015-000188 (2016).
Lu, C. Y., Chen, H. H., Chi, K. H. & Chen, P. C. Obesity indices and the risk of total and cardiovascular mortality among people with diabetes: A long-term follow-up study in Taiwan. Cardiovasc. Diabetol. 22, 345. https://doi.org/10.1186/s12933-023-02072-3 (2023).
Heymsfield, S. B., Scherzer, R., Pietrobelli, A., Lewis, C. E. & Grunfeld, C. Body mass index as a phenotypic expression of adiposity: Quantitative contribution of muscularity in a population-based sample. Int. J. Obes. 33, 1363–1373. https://doi.org/10.1038/ijo.2009.184 (2009).
Biolo, G. et al. Inverse relationship between a body shape index (ABSI) and fat-free mass in women and men: Insights into mechanisms of sarcopenic obesity. Clin. Nutr. 34, 323–327. https://doi.org/10.1016/j.clnu.2014.03.015 (2015).
Kim, B. et al. The a body shape index might be a stronger predictor of chronic kidney disease than BMI in a senior population. Int. J. Environ. Res. Public Health 18. https://doi.org/10.3390/ijerph182412874 (2021).
Sardarinia, M., Ansari, R., Azizi, F., Hadaegh, F. & Bozorgmanesh, M. Mortality prediction of a body shape index versus traditional anthropometric measures in an Iranian population: Tehran lipid and glucose study. Nutrition (Burbank Los Angeles Cty. Calif). 33, 105–112. https://doi.org/10.1016/j.nut.2016.05.004 (2017).
Ahima, R. S., Lazar, M. A. & Physiology The health risk of obesity—Better metrics imperative. Science 341, 856–858. https://doi.org/10.1126/science.1241244 (2013).
Herrera, D. et al. Periodontal diseases and cardiovascular diseases, diabetes, and respiratory diseases: Summary of the consensus report by the European Federation of Periodontology and WONCA Europe. Eur. J. Gen. Pract. 30, 2320120. https://doi.org/10.1080/13814788.2024.2320120 (2024).
Kajikawa, M. et al. A body shape index as a simple anthropometric marker of abdominal obesity and risk of cardiovascular events. J. Clin. Endocrinol. Metab. https://doi.org/10.1210/clinem/dgae282 (2024).
Mirzababaei, A. et al. The mediatory effect of inflammatory markers on the association between a body shape index and body roundness index with cardiometabolic risk factor in overweight and obese women: A cross-sectional study. Front. Nutr. 10, 1178829. https://doi.org/10.3389/fnut.2023.1178829 (2023).
NCHS Ethics Review Board (ERB). Approval. https://www.cdc.gov/nchs/nhanes/irba98.htm.
Eke, P. I., Borgnakke, W. S. & Genco, R. J. Recent epidemiologic trends in periodontitis in the USA. Periodontology 2000 82, 257–267. https://doi.org/10.1111/prd.12323 (2020).
Eke, P. I., Page, R. C., Wei, L., Thornton-Evans, G. & Genco, R. J. Update of the case definitions for population-based surveillance of periodontitis. J. Periodontol. 83, 1449–1454. https://doi.org/10.1902/jop.2012.110664 (2012).
Luo, S. et al. The associations of two novel inflammation indexes, systemic immune-inflammation index (SII) and system inflammation response index (SIRI), with periodontitis: evidence from NHANES 2009–2014. Clin. Oral Invest. 28, 129. https://doi.org/10.1007/s00784-024-05529-1 (2024).
Christakoudi, S. et al. A body shape index (ABSI) achieves better mortality risk stratification than alternative indices of abdominal obesity: Results from a large European cohort. Sci. Rep. 10, 14541. https://doi.org/10.1038/s41598-020-71302-5 (2020).
Krakauer, N. Y. & Krakauer, J. C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 7, e39504. https://doi.org/10.1371/journal.pone.0039504 (2012).
Özlem, K. & Selçuk, K. High ABSI values and association with AF recurrence after AF ablation: A prospective single-center study. Eur. Rev. Med. Pharmacol. Sci. 26, 7151–7160. https://doi.org/10.26355/eurrev_202210_29901 (2022).
Li, W., Song, J. & Chen, Z. The association between dietary vitamin C intake and periodontitis: Result from the NHANES (2009–2014). BMC Oral Health 22, 390. https://doi.org/10.1186/s12903-022-02416-7 (2022).
James, W. P. What are the health risks? The medical consequences of obesity and its health risks. Exp. Clin. Endocrinol. Diabetes Off. J. Ger. Soc. Endocrinol. Ger. Diabetes Assoc. 106 (Suppl 2), 1–6. https://doi.org/10.1055/s-0029-1212028 (1998).
Tzamaloukas, A. H. et al. Classification of the degree of obesity by body mass index or by deviation from ideal weight. JPEN J. Parenter. Enteral. Nutr. 27, 340–348. https://doi.org/10.1177/0148607103027005340 (2003).
Bacopoulou, F., Efthymiou, V., Landis, G., Rentoumis, A. & Chrousos, G. P. Waist circumference, waist-to-hip ratio and waist-to-height ratio reference percentiles for abdominal obesity among Greek adolescents. BMC Pediatr. 15, 50. https://doi.org/10.1186/s12887-015-0366-z (2015).
Hwaung, P. et al. Optimum waist circumference-height indices for evaluating adult adiposity: an analytic review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 21, e12947. https://doi.org/10.1111/obr.12947 (2020).
Liu, Y. et al. Body roundness index is a superior obesity index in predicting diabetes risk among hypertensive patients: A prospective cohort study in China. Front. Cardiovasc. Med. 8, 736073. https://doi.org/10.3389/fcvm.2021.736073 (2021).
Endukuru, C. K., Gaur, G. S., Dhanalakshmi, Y., Sahoo, J. & Vairappan, B. Cut-off values and clinical efficacy of body roundness index and other novel anthropometric indices in identifying metabolic syndrome and its components among southern-indian adults. Diabetol. Int. 13, 188–200. https://doi.org/10.1007/s13340-021-00522-5 (2022).
Nagayama, D. et al. New index of abdominal obesity, a body shape index, is BMI-independently associated with systemic arterial stiffness in real-world Japanese population. Int. J. Clin. Pharmacol. Ther. 58, 709–717. https://doi.org/10.5414/cp203778 (2020).
Calderón-García, J. F. et al. Effectiveness of body roundness index (BRI) and a body shape index (ABSI) in Predicting Hypertension: A systematic review and meta-analysis of Observational studies. Int. J. Environ. Res. Public Health 18. https://doi.org/10.3390/ijerph182111607 (2021).
Aoki, K. C. & Mayrovitz, H. N. Utility of a body shape index parameter in predicting cardiovascular disease risks. Cureus 14, e23886. https://doi.org/10.7759/cureus.23886 (2022).
Wu, L. D., Kong, C. H., Shi, Y., Zhang, J. X. & Chen, S. L. Associations between novel anthropometric measures and the prevalence of hypertension among 45,853 adults: A cross-sectional study. Front. Cardiovasc. Med. 9, 1050654. https://doi.org/10.3389/fcvm.2022.1050654 (2022).
Lin, G., Zhan, F., Ren, W., Pan, Y. & Wei, W. Association between novel anthropometric indices and prevalence of kidney stones in US adults. World J. Urol. 41, 3105–3111. https://doi.org/10.1007/s00345-023-04582-x (2023).
Kuang, M. et al. The value of combining the simple anthropometric obesity parameters, body mass index (BMI) and a body shape index (ABSI), to assess the risk of non-alcoholic fatty liver disease. Lipids Health Dis. 21, 104. https://doi.org/10.1186/s12944-022-01717-8 (2022).
Hamza, S. A., Asif, S., Khurshid, Z., Zafar, M. S. & Bokhari, S. A. H. Emerging role of epigenetics in explaining relationship of periodontitis and cardiovascular diseases. Diseases (Basel Switzerland) 9. https://doi.org/10.3390/diseases9030048 (2021).
Page, R. C. The pathobiology of periodontal diseases may affect systemic diseases: Inversion of a paradigm. Ann. Periodontol. 3, 108–120. https://doi.org/10.1902/annals.1998.3.1.108 (1998).
Murguía-Vázquez, M., Salgado-Bustamante, M., Lima-Rogel, V., Flores-García, J. A. & Pierdant-Pérez, M. Association between pro-inflammatory cytokine levels (IL-1β, IL-6, and TNF-α) in human colostrum and maternal body composition components. Breastfeed. Med. Off. J. Acad. Breastfeed. Med. 19, 349–356. https://doi.org/10.1089/bfm.2023.0263 (2024).
Ellulu, M. S., Patimah, I., Khaza’ai, H., Rahmat, A. & Abed, Y. Obesity and inflammation: The linking mechanism and the complications. Arch. Med. Sci. AMS 13, 851–863. https://doi.org/10.5114/aoms.2016.58928 (2017).
Lastra, G. & Sowers, J. R. Obesity and cardiovascular disease: Role of adipose tissue, inflammation, and the renin-angiotensin-aldosterone system. Horm. Mol. Biol Clin. Investig. 15, 49–57. https://doi.org/10.1515/hmbci-2013-0025 (2013).
Abdulkhaleq, L. A. et al. The crucial roles of inflammatory mediators in inflammation: A review. Vet. World 11, 627–635. https://doi.org/10.14202/vetworld.2018.627-635 (2018).
Cekici, A., Kantarci, A., Hasturk, H. & Van Dyke, T. E. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontology 2000 64, 57–80. https://doi.org/10.1111/prd.12002 (2014).
Correction macrophage-specific TLR2 signaling mediates pathogen-induced TNF-dependent inflammatory oral bone loss. J. Immunol. (Baltimore Md. 1950) 209, 1617. https://doi.org/10.4049/jimmunol.2200589 (2022).
Deasy, M. J. & Vogel, R. I. Female sex hormonal factors in periodontal disease. Ann Dent. 35, 42–46 (1976).
Lê, S. et al. Obesity is associated with the severity of Periodontal inflammation due to a specific signature of subgingival microbiota. Int. J. Mol. Sci. 24. https://doi.org/10.3390/ijms242015123 (2023).
Kayar, N. A. et al. Immunologic burden links periodontitis to acute coronary syndrome: Levels of CD4+ and CD8+ T cells in gingival granulation tissue. Clin. Oral Investig. 28, 199. https://doi.org/10.1007/s00784-023-05448-7 (2024).
Acknowledgements
We appreciate that the full dataset is accessible through the NHANES database, which can be located at the following link: https://www.cdc.gov/nchs/nhanes/index.htm.
Funding
Guizhou Provincial Science and Technology Fund (ZK [2024] General 598); Guiyang Science and Technology Fund ([2022] 4).
Author information
Authors and Affiliations
Contributions
Xuanyan Gu was responsible for study design, data collection, data merging, and data analysis, as well as drafting the manuscript. Shiyi Luo provided expertise in data interpretation. Fuqian Jin assisted in data merging. Zhu Chen, Jukun Song and Jiangling Sun contributed to the review and editing process. All authors have reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The NHANES repository is both representative and openly available at no cost. Approval for the study’s methodology was granted by the Research Ethics Review Board of the National Center for Health Statistics.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gu, X., Luo, S., Sun, J. et al. Association between “a body shape index” (ABSI) with periodontitis in a hypertension population from the NHANES 2009–2014. Sci Rep 14, 23378 (2024). https://doi.org/10.1038/s41598-024-73998-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-73998-1
Keywords
This article is cited by
-
Inflammatory markers mediate the association between alternative adiposity indices and mortality in patients with rheumatoid arthritis: data from NHANES 1999–2018
Lipids in Health and Disease (2025)
-
Association between conicity index and prevalence of periodontitis in US adults: the 2009–2014 NHANES cross-sectional study
Scientific Reports (2025)