Abstract
This study compared the hospitalization expenses of patients with chronic bronchitis in a central province (Province A) in China to estimate the direct medical cost of the family. Our data included hospitalization records of 30,341 patients with chronic bronchitis from five urban general hospitals in Province A. Using descriptive statistics and regression analysis, we explored the relevant factors affecting hospitalization expenses. Our study results have indicated that from 2016 to 2020, the medical expenditure of patients with chronic bronchitis increased annually, with an average annual growth rate of 22.65%. Among all kinds of expenses, the hospitalization expenses, drug cost, bed cost, test cost and other cost of UEMI (Urban Employee Medical Insurance) are higher than that of other types of medical insurance. The check-up fees of CMI (Commercial Insurance) are lower than that of other types of insurance. Between 2016 and 2019, the average medical expenses per patient with chronic bronchitis increased by 44%, which is the highest average medical expenses among patients aged 60–70. And the highest average medical expenditure emerged when the number of service days is between 5 and 10 days. The increase in expenditure could be attributed to the rapid development of medical technology and the increasing medical demand of the people. Overall, the results of our study implied a significant increase in medical expenses for patients with chronic bronchitis from 2015 to 2020, indicating that chronic bronchitis could bring heavy economic pressures to patients, their families and society.
Similar content being viewed by others
Introduction
In recent years, with the rapid economic development and evolving lifestyle, the incidence of chronic diseases has continued to rise. Chronic disease is the main cause of death and disability in developed countries in the 21st century1, which consists of a group of diseases that usually persist for a long time, difficult to cure and aren’t disappear spontaneously, such as heart disease, stroke, cancer, diabetes, chronic respiratory diseases, etc. These diseases not only reduce the quality of life of patients significantly, but also lead to increased costs associated with disease management. Taking chronic bronchitis as an example, it is characterized by cough, expectoration, wheezing and other symptoms2, with high incidence, easy to repeat and long-term existence3. This disease with long duration will bring complications such as pulmonary hypertension, obstructive emphysema and pulmonary heart disease4, which could threaten the lives of patients. The disease has a huge psychological and physical impact on patients, and leads to increased medical costs and loss of working hours5. In China, there are few studies focusing on the medical expenses of chronic bronchitis6. And a large number of studies were conducted in a single medical institution. Due to the sample size, the representativeness of each study is relatively limited7, which restricted the value for policy makers to formulate national strategies for chronic bronchitis in the elderly. The high cost of health care not only increases the economic pressure on patients and their families, but also hinders the effective operation of health insurance funds, which could impact the sustainable development of medical insurance system. Therefore, a study on assessing the disease burden and medical costs of chronic bronchitis and collating hospitalization data is particularly important for recognizing its social and economic impact, and is of practical significance for improving control levels and formulating public health policies.
Previous studies mainly focused on epidemiology and analyzed the prevalence of chronic bronchitis across different dimensions and countries8,9. However, there is little international or domestic evidence on the hospitalization costs for patients with chronic bronchitis. Most of the previous studies focused on other common chronic diseases, such as atrial fibrillation-related stroke, chronic kidney disease, and diabetes10,11,12. Although these studies have promoted the development of cost analysis for chronic bronchitis hospitalizations, the lack on systematic representative sample or accounting framework influence the analysis on these expenses. A systematic accounting framework of the hospitalization costs of chronic bronchitis patients can improve measurement accuracy and comparability among different countries13. Province A belongs to the central region of China, with a permanent population of 61.027 million and a GDP of 386.806 billion yuan in 2020, ranking 11th in the country14. In terms of studying the hospitalization expenses of chronic diseases in Province A, it is highly representative.
This study based on the framework of ‘’Functional Health Cost Accounting System (SHA2011)’’. The goal is to analyze the data collected from multiple medical centers in Province A, calculate the hospitalization cost data, further understand the cost distribution of different time, gender and region in detail, and to evaluate the direct medical expenses of hospitalized patients with chronic bronchitis and its causes. Since the 2019 novel coronavirus pandemic has stimulated an increase in public health awareness, we will explore whether this is related to a decrease in the incidence of chronic bronchitis. UEMI (Urban Employee Medical Insurance) is one of the largest medical insurance plans in China, which originated in the mid-1990s15. However, by the beginning of the 21st century, the Chinese government set up two new insurance programs: NCMI (New Agricultural Cooperative Medical Insurance) for rural residents and URMI (Urban Residents Medical Insurance) for self-employed and unemployed urban residents16. Then in January 2019, NCMI and URMI were integrated into urban and rural residents’ medical insurance. Therefore, the NCMI-related data involved in this study were only collected in 2018. CMI (Commercial Medical Insurance) is the international and Chinese general medical insurance. It is necessary to explore the hospitalization expenses of patients with different types of medical insurance to evaluate the impact of insurance types on hospitalization costs. In addition, we will also focus on rural areas, because there are many patients and relatively scarce health resources, resulting in the health status of farmers is lower than that of urban residents. Significant urban-rural health resource gap, dual economic structure, income gap, and insufficient attention of local governments to public health are the catalytic factors of this phenomenon. The mortality rate in the northern region is higher than that in the southern region, which may be related to the temperature fluctuation in the north and the high exposure rate of occupational diseases. We will also clarify whether there are differences between men and women in the cost of hospitalization for chronic bronchitis in order to provide more accurate guidance for medical decision-making and provide better medical protection for such patients.
Materials and methods
Settings and data source
The data used in this study mainly come from field survey materials. The field survey data are mainly derived from the survey data of the sample institutions. In Province A, a three-stage cluster sampling method is used to determine the sampling points. First of all, according to their respective regional development status, all the cities in Province A are divided into five major groups. Second, the representative city was selected from each group: City M and T in the east, City L in the west, City C in the south, City B in the north, and City H in the middle. Third, in these cities, different medical institutions were randomly selected as our sampling points. As for the selection of sampling institutions, it combines public and private hospitals, disease prevention and control institutions, health supervision institutions, maternal and child health institutions, sanatoriums, specialist prevention and treatment institutions, family planning technical service institutions, health education institutions, and primary medical institutions (such as township hospitals, community health service centers/stations, outpatient departments, village clinics, etc.). Finally, in all of these medical institutions, all inpatient data for the six-year period from January 1, 2015 to December 31, 2020 were collated and collected. This work was approved by the Biomedical Ethics Committee of Anhui Medical University (No.83244641) to ensure that all participants provided informed consent before participation.
Study population
The study took into account socio-geographical variables including biological sex and age. We obtained clinical variables such as etiology and comorbidity from medical records of physical and imaging examinations, and recorded the costs of patients during hospitalization. In the diagnosis process, we identified any major discharge diagnosis in line with the International Classification of Diseases, 10th Edition (ICD-10) in patients with chronic bronchitis code for hospitalized patients with chronic bronchitis. All ICD-10 codes are uniformly reported by professionally trained medical staff through the electronic system of the medical institution to reduce errors. In addition, in order to ensure accuracy, a special computer program developed by the National Health and Health Development Commission is also used to proofread all ICD-10 codes from 2015 to 2020. Finally, we selected 30,341 eligible patients with chronic bronchitis who were hospitalized for at least one day in medical institutions in Province A, and recorded their demographics, the distribution of urban area, comorbidity, gender, age, medical insurance, hospitalization expenses, insurance reimbursement, and health facilities information.
Statistical analysis
The hospitalization expenses composed of the following parts: treatment expenses, drug expenses (including western medicine, Chinese patent medicine and Chinese herbal medicine), bed expenses, diagnosis expenses, examination expenses, operation expenses, laboratory expenses, nursing expenses and other expenses (except for the above expenses). In our study, we caculated the total cost of hospitalization based on the following formula:
R4.2.3 software was used to set the significance level of 5% for statistical analysis. In this analysis, the p-value of continuous variables is obtained by Student’s t test, while the p-value of categorical variables is calculated by chi-square test. Our goal is to explore the relationship between hospitalization expenses and their possible influencing factors by using multiple linear regression models. The model is :
The dependent variable (Y) is the hospitalization expenses, and the independent variables include the statistical year, age, gender, type of medical insurance, whether there are complications, urban regional distribution, geographical location of medical institutions, and the nature of medical institutions (public or private).
Results
Basic information of the participants
As shown in Table 1, this study included 30,341 hospitalized patients with chronic bronchitis covered by insurance. The number of inpatients per year from 2015 to 2020 was 2839, 2686, 5888, 5917, 6586 and 6425, respectively. The average age of the sampled patients was 71.8 years (standard deviation 12.33 years), and the average length of hospital stay was 9.98 days (standard deviation 11.37 days). Male patients accounted for 42.33% of the total. Among these patients, 2169 (7.15%) were covered by Medical Insurance for Urban Workers (UEMI), while 10,924 (36.00%) were covered by Medical Insurance for Urban Residents (URMI), 15,009 (49.47%) by New Agricultural Cooperative Medical Insurance (NCMI), 376 (1.24%) by Commercial Insurance (CMI) and 2239 (7.38%) by Other Types of Insurance (OMI). About 67.73% of the patients in this study did not have comorbidities. In terms of regional distribution, the number of patients in the western, eastern and southern regions is close, the number of patients in the northern region is slightly higher, and the number of patients in the central region is the highest. 23,888 people (78.73%) were treated in public medical institutions, and 6453 people were treated in private health facilities.
Factors associated with hospitalization costs
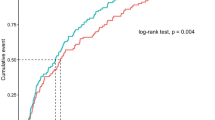
Through multiple regression analysis, it was found that gender, age, length of stay, comorbidity, type of medical insurance, type of medical institution, and urban distribution were associated with hospitalization costs, as shown in Table 2.
Medical expenses of inpatients and inpatients with different types of medical insurance
Table 3 lists the annual hospitalization expenses of each patient in detail, with an average cost of 4435.64 ± 7668.61 yuan. The funds are divided as follows: treatment cost 704.35 ± 2048.04 yuan, drug cost 1994.86 ± 2662.24 yuan, bed cost 268.79 ± 507.31 yuan, diagnosis cost 170.67 ± 357.21 yuan, examination cost 311.34 ± 523.48 yuan, operation cost 41.64 ± 272.10 yuan, laboratory cost 652.26 ± 910.89 yuan, nursing cost 202.47 ± 749.33 yuan, and other costs 634.44 ± 1656.53 yuan. Compared with other types of insurance, UEMI has a higher proportion and median in total hospitalization costs, drug costs, bed fees, examination costs, laboratory fees, and other costs. In addition, the diagnosis cost and surgery cost of URMI are also high. CMI inspection costs are relatively low. At the same time, the treatment costs and nursing fees of OMI also exceeds other types of medical insurance. The scatter plot of hospitalization expenses for chronic bronchitis patients revealed that 31.75% had expenses above the average, showing a skewed distribution toward higher costs. The highest expense reached 240,319.71 yuan (Fig. 1).
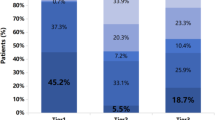
Between 2015 and 2020, the proportion of treatment costs and care costs continued to rise, however, the proportion of drug costs and other costs decreased annually (Fig. 2). In particular, the cost of medicines, which fell from 41% in 2015 to 25% in 2020.
Discussion
Considering the continuous aging of the population and the increase in the number of chronic diseases, public health strategies throughout the twenty-first century have been noticeably challenged. Although the respiratory disease is one of the most common public health problems, research on the economic impact of chronic bronchitis is still relatively scarce. Due to the increase in the incidence of chronic bronchitis as well as the improvement of people’s awareness on this disease and the promoted availability to medical services, more and more people have entered medical institutions for treatment. It is worth noting that most of the disease-related medical expenses are generated in hospitals17, which leads to the total cost of hospitalization becoming the main economic pressure for patients and their families. Therefore, it is critical for the government, medical insurance institutions and hospitals to control the surge in medical expenses. According to our research, the medical expenditure of patients with chronic bronchitis increased year by year from 2016 to 2020, with an average annual growth rate of 22.65%. This increase in medical expenses is likely to lead to an increase in other indirect costs, such as non-medical expenses of patients, home care costs, work losses, as well as transportation and accommodation costs caused by diseases. According to our research, the chronic bronchitis has brought considerable direct medical cost to individuals and society. It is worth noting that among the patients with chronic bronchitis, the differences in medical expenses among different subgroups are pronounced.
Our study revealed that from 2015 to 2020, the annual average medical expenses of chronic bronchitis were RMB 2839, RMB 2686, RMB 5888, RMB 5817, RMB 6586 and RMB 6425, respectively. Based on the data of the average household population (2.6 people) and the per capita disposable income of rural residents (RMB 17,131.5) in 2020, the average medical expenses of patients with chronic bronchitis account for 14.4% of the average annual income of rural households, which clearly points out that families with chronic bronchitis in China are under greater economic pressure, especially for low-income families. This further points to the seriousness of the waste of medical resources caused by unreasonable hospitalization behavior. The results showed that the proportion of drug costs in the hospitalization expenses of chronic bronchitis decreased from 41% in 2015 to 25% in 2020, but it was still the highest. As a common chronic non-communicable disease, chronic bronchitis has a long course of disease. Both surgical and non-surgical patients need to take medicine to stabilize the disease. Therefore, drug costs bring a greater direct medical cost to patients. Medical expenses are affected by multiple stakeholders such as government, health care management, medical institutions, patients, etc18. The government needs to adjust relevant policies, strengthen the management of the drug and medical supplies market, and reduce the cost of intermediate links, such as eliminating the inflated prices of high-priced drugs and medical supplies through a unified price negotiation and regulatory mechanism19. A strict surgical review system is established, and experts are regularly organized to conduct standardized evaluations of relevant behaviors of medical institutions20. In the results of this study, although the treatment fee and nursing fee are relatively low, the increasing tendency appears. The results indicate that the labor value of medical staff can be fully reflected, which reflects the improvement of the value recognition of technical services.
We found that age has an impact on hospitalization costs of chronic bronchitis. Therefore, after the first diagnosis of the patient, a more comprehensive treatment plan needs to be adopted. For this part of the focus group, long-term health education should be strengthened to improve their health knowledge level. As a long-term chronic disease, chronic bronchitis can prevent deterioration and hospitalization by changing behaviors and lifestyles. In particular, community health service institutions should strive to provide health management services for such groups, guide and intervene in their diet planning and physical exercise, and conduct regular health examinations, consultations and education. At the same time, real and effective health records should be established to strengthen the construction of disease prevention and control system. For patients who need long-term care, nursing institutions should provide them with professional nursing knowledge on time to prevent hospitalization due to chronic bronchitis.
When there is a significant positive skew (where the mean is much higher than the median), it indicates that a small number of patients with exceptionally high costs are driving the mean upward. In this study, a subset of patients incurred substantial hospitalization expenses, resulting in the average exceeding the median. In such cases, the median may provide a more accurate reflection of the distribution of patients’ costs. When formulating policies, the government should focus on patients with higher hospitalization costs, improve the medical insurance system, expand coverage, reduce out-of-pocket expenses, and ensure that the medical burden on patients with major illnesses and long-term hospitalizations is effectively reduced21.
Gender also has a certain impact on hospitalization costs. In response to this phenomenon, we need to take some measures to deal with it, such as increasing the frequency of medical monitoring for female patients, implementing active treatment and prevention, strengthening publicity and education, and advocating healthy behaviors and lifestyles. For male patients, quit smoking and limit alcohol, strengthen physical exercise, reduce the incidence of respiratory diseases, prevent the deterioration of diseases, and reduce the direct medical cost.
The length of hospital stay is usually regarded as an indicator of the consumption of medical resources22. The longer the patient ‘s hospital stay, the more medical resources are consumed, resulting in relatively high hospitalization costs. Studies at home and abroad have shown that hospitalization expenses are positively correlated with hospitalization time23. First of all, with the increase of hospitalization days, the cost of beds, nursing and other related costs will increase, and long-term hospitalization will increase the risk of nosocomial infection and complications. Repeated and prolonged hospitalization will lead to an increase in hospitalization costs. Secondly, the efficiency of the hospital system such as examination is not high, which leads to the prolongation of hospitalization days for patients waiting for examination, and the invalid hospitalization days such as preoperative hospitalization days will lead to an unnecessary increase in the total cost of hospitalization. Therefore, for patients with chronic bronchitis, medical institutions should be committed to improving the quality and level of medical services to shorten the average length of stay. In addition, it can also improve the bed rotation rate, thereby optimizing resource utilization and providing services to more patients, which plays an important role in strengthening and evaluating the quality management of hospital medical care. At the same time, attention should be paid to medical quality management to prevent excessive medical treatment. Wang and colleagues pointed out that the hospitalization time of medical insurance patients is often longer than that of non-medical insurance patients24. However, it can not be simply concluded that the longer the hospitalization time, the better the effect. Because with the extension of hospitalization time, the treatment intensity is often declining.
We found that patients who rely on UEMI have significantly higher medical expenses than patients with other types of insurance. In view of the continuous growth of people’s demand for higher quality health care, there is still a lot of room for improvement in basic medical insurance and public health insurance for urban workers. However, due to the aging of the population, coupled with the increase in medical expenses and other complex factors, these two kinds of insurance are facing the pressure of capital payment. The fundamental purpose of medical insurance is to share the economic risk of disease among individuals to reflect fairness25. Therefore, the treatment gap between different types of medical insurance patients should be gradually reduced to further improve fairness.The medical insurance management department should incorporate multiple payment methods into the payment system, and implement multiple payment methods in combination with the medical payment system. At the same time, for different types of insured patients, medical institutions should formulate targeted cost control measures and play the role of third parties26,27. Therefore, it is very important to construct specific policies to improve the social medical insurance system, which will enable more people to have access to affordable medical services.
It was also recognized that comorbidity is related to hospitalization costs. As with the number of diseases increases, the complexity of health condition could rise, which may lead to higher diagnosis, drug, and treatment costs. For critically ill and complex patients, medical staff should actively apply the MDT (multidisciplinary diagnosis and treatment mode) to address issues promptly and reduce serious complications.
The hospitalization expenses of patients with chronic bronchitis vary significantly across different cities. This variation is related to regional differences in socioeconomic status and medical development. In cities with rapid growth in economy and medicine, the rate of acute and critical conditions in chronic bronchitis patients is higher than that in other cities and counties. Additionally, the charging standards of medical institutions are higher in highly developed areas, leading to more hospitalization expenses compared to other regions.
We found that the type of medical institutions also had an impact on hospitalization costs. The type of medical institution is closely related to its diagnosis and treatment level, scale, technical accessibility and other factors. However, these factors have also led to increased investment costs for institutions, which are passed on to patients, increasing the financial burden and consuming unnecessary medical resources28. Chronic bronchitis could have been prevented by changing patient behavior to further avoid hospitalization due to worsening conditions. The high hospitalization cost of chronic bronchitis not only means a major waste of medical resources, but also reflects the low utilization efficiency of medical services. In order to improve the resource utilization rate of medical institutions, it is necessary to guide the public to cultivate a reasonable concept of medical treatment and improve the patient ‘s medical experience simultaneously. In order to balance the medical needs of residents in public and private hospitals, the government can ensure fair competition in the quality and cost of medical services through policy support and resource allocation. In addition, optimize the medical insurance system, promote hierarchical diagnosis and treatment, encourage public-private cooperation, and strengthen information transparency and patient education to help residents make informed choices based on their own needs and hospital conditions, thereby improving the overall level of medical services.
Our study also has some limitations. Firstly, due to the retrospective design of the study, we cannot calculate non-medical costs and indirect costs directly. Secondly, since the patient data are all from hospitals in Province A of China, it may lead to selection bias and limit the generalizability of the data. For the calculation of hospitalization expenses of patients with chronic bronchitis, we rely on the hospitalization information reported by the functional health accounting monitoring agency, which may affect the accuracy of hospitalization cost estimation. Furthermore, we were unable to collect patient income information and therefore were unable to analyze the impact of medical expenses on the financial burden of patients with chronic bronchitis from 2015 to 2020.
We used patient-level data for different stages of development and socioeconomic status in this study to ensure the reliable of our results. Through a detailed analysis of the distribution of sources of medical expenditure, this study identified important factors affecting medical expenditure. Our study can offer a reference for other regions in China on developing effective strategies to reduce the direct medical cost of individuals, families, society and government.
Conclusions
From 2015 to 2020, the medical expenses of patients with chronic bronchitis increased significantly. Therefore, it is urgent to implement targeted measures to alleviate the economic pressure of these patients and families. In addition, SHA2011 can provide more macro and representative data for the health system. This study supplements the perspective of measuring the impact of hospitalization expenses on family direct medical cost.
Data availability
Enquiries about data availability should be directed to the corresponding author.
References
Yach, D., Hawkes, C., Gould, C. L. & Hofman, K. J. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA 291(21), 2616–2622. https://doi.org/10.1001/jama.291.21.2616 (2004).
Xiancai, Z. To explore the characteristics and treatment methods of respiratory medicine in treating chronic bronchitis. J. Cardiovasc. Dis. Integr. Trad. Chin. Western Med. 6(18), 47 (2018).
Shenfang, Y. Observation on the effect of standardized treatment in respiratory department of chronic bronchitis. Friends Health 18, 164–165 (2019).
Jihua, Z. Analysis on standardized treatment of respiratory medicine of chronic bronchitis. Health Today (2020).
Li, Y. Analysis on standardized treatment of respiratory medicine of chronic bronchitis. J. Cardiovasc. Dis. Integr. Trad. Chin. West. Med. 7(3), 158–160 (2019).
Yu, D. H. et al. Identifying patterns of non-communicable diseases in developed eastern coastal China: a longitudinal study of electronic health records from 12 public hospitals. BMJ Open 7(10), 9 (2017).
Liu, L. et al. Impact of Beijing healthcare reform on the curative care expenditure of outpatients with noncommunicable diseases based on SHA2011 and interrupted time series analysis. BMC Health Serv. Res. 21(1), 1045 (2021).
Varmaghani, M. et al. Prevalence of asthma, COPD, and chronic bronchitis in Iran: a systematic review and Meta-analysis. Iran. J. Allergy Asthma Immunol. 15(2), 93–104 (2016).
Jarhyan, P., Hutchinson, A., Khaw, D., Prabhakaran, D. & Mohan, S. Prevalence of chronic obstructive pulmonary disease and chronic bronchitis in eight countries: a systematic review and meta-analysis. Bull. World Health Organ. 100(3), 216–230. https://doi.org/10.2471/BLT.21.286870 (2022).
Hu, S. et al. Economic Burden of Individual suffering from atrial fibrillation-related stroke in China. Value Health Reg. Issues 2(1), 135–140. https://doi.org/10.1016/j.vhri.2013.02.008 (2013).
Davis-Ajami, M. L., Fink, J. C. & Wu, J. Nephrotoxic medication exposure in U.S. adults with Predialysis chronic kidney disease: Health services utilization and cost outcomes. J. Manag. Care Spec. Pharm. 22(8), 959–968. https://doi.org/10.18553/jmcp.2016.22.8.959 (2016).
Huang, Y., Vemer, P., Zhu, J., Postma, M. J. & Chen, W. Economic burden in Chinese patients with diabetes mellitus using electronic insurance claims data. PLoS ONE 11(8), e0159297. https://doi.org/10.1371/journal.pone.0159297 (2016).
Shi, X., Zhao, Y., Wan, Q., Chai, P. & Ma, Y. Curative care expenditure of outpatient anxiety disorder in Liaoning Province, 2015–2020-based on System of Health Accounts 2011. Front. Public Health 12, 1329596. https://doi.org/10.3389/fpubh.2024.1329596 (2024).
Song, T. et al. Analysis of the current status and influencing factors of cross-regional hospitalization services utilization by basic medical insurance participants in China—taking a central province as an example. Front. Public Health 11, 1246982. https://doi.org/10.3389/fpubh.2023.1246982 (2023).
Meng, Z. & Junli, Z. The impact of the upgrading of the industrial structure on the urban employee basic medical insurance fund: an empirical study in China. Risk Manag. Healthc. Policy. 14, 2133–2144 (2021).
Li, Y. et al. Differences exist across insurance schemes in China post-consolidation. PLoS ONE 12, e0187100 (2017).
Li, L. W. & Long, Y. Health Care Experience of Older Persons with Chronic Illness in Rural and Urban China: A Qualitative Study in Shandong, China. https://deepblue.lib.umich.edu/handle/2027.42/116798 (Accessed 15 September 2018) (2016)..
Lavanchy, D. Worldwide epidemiology of HBV infection, disease burden, and vaccine prevention. J. Clin. Virol. 34, S1–S3. https://doi.org/10.1016/S1386-6532(05)00384-7 (2005).
You, C. H., Kang, S., Kwon, Y. D. & Choi, J. H. Time trend of out-of-pocket expenditure among cancer inpatients: evidence from Korean tertiary hospitals. Asian Pac. J. Cancer Prev. 14, 6985–6989. https://doi.org/10.7314/APJCP.2013.14.11.6985 (2013).
Duan, W. et al. How great is the medical burden of disease on the aged? Research based on system of Health Account 2011. Health Qual. Life Outcomes 15, 134. https://doi.org/10.1186/s12955-017-0709-6 (2017).
Wei, S. Q. et al. Hospitalization expenses of patients with lung cancer from 2015 to 2020 and its influencing factors——Take a tertiary hospital of Shandong Province as an example. Chin. Rural Health Serv. Adm.. 41, 658–662.https://doi.org/10.19955/j.cnki.1005-5916.2021.09.011 (2021).
Lai, C-I., Hung, W-J., Lin, L-P., Chien, W-C. & Lin, J-D. A retrospective population-based data analyses of inpatient care use and medical expenditure in people with intellectual disability co-occurring schizophrenia. Res. Dev. Disabil. 32, 1226–1231. https://doi.org/10.1016/j.ridd.2010.12.024 (2011).
Nakamura, K. et al. Treated and untreated hypertension, hospitalization, and medical expenditure: an epidemiological study in 314,622 beneficiaries of the medical insurance system in Japan. J. Hypertens. 31, 1032–1042. https://doi.org/10.1097/HJH.0b013e32835f5747 (2013).
Hung, W-J., Lin, L-P., Wu, C-L. & Lin, J-D. Cost of hospitalization and length of stay in people with Down syndrome: evidence from a national hospital discharge claims database. Res. Dev. Disabil. 32, 1709–1713. https://doi.org/10.1016/j.ridd.2011.02.024 (2011).
Wu, J., Liu, J., Zhu, B. & Mao, Y. Comparative analysis on the out-of-pocket expenditure among patients suffering from chronic kidney disease between medical insurance covered and uncovered areas in China. Value Health 19, A846. https://doi.org/10.1016/j.jval.2016.08.499 (2016).
Wang, X., Sun, Y., Mu, X., Guan, L. & Li, J. How to improve the equity of health financial sources? Simulation and analysis of total health expenditure of one Chinese province on system dynamics. Int. J. Equity Health 14, 73. https://doi.org/10.1186/s12939-015-0203-x (2015).
Yang, Y. et al. Medical economic burden of the ageing population: a multistage sampling analysis of 3 532 517 cases. Lancet 388, S79. https://doi.org/10.1016/S0140-6736(16)32006-2 (2016).
Lin, W-Y. et al. Hospice shared-care saved medical expenditure and reduced the likelihood of intensive medical utilization among advanced cancer patients in Taiwan—a nationwide survey. Support Care Cancer 22, 1907–1914. https://doi.org/10.1007/s00520-014-2168-54 (2014).
Funding
This study was supported by the horizontal cooperation project “Research on Accounting for Total Health Costs in Anhui Province” (No. K2021209) of Anhui Provincial Health Commission.
Author information
Authors and Affiliations
Contributions
GMZ was involved in the framework design, review of the article, analysis of the data, writing and revision of the manuscript. LZH contributed in the literature search and review, and the revision of the article, and LZH contributed to the work equally and should be regarded as co-first author. STY was responsible for collecting data. MRF was responsible for sorting out data. LBL critically revised the manuscript. ZXG further revised the results. ZTM further revised the summary part. CYT further calculated the data. All authors read and approved the final manuscript. TZR led the conduct of the study and guided the writing process of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved by the Biomedical Ethics Committee of Anhui Medical University with approval number 83,244,631. Participants provided informed consent prior to participation. The research method strictly abode by the prescribed standards and protocols, and had been recognized by the Biomedical Ethics Committee of Anhui Medical University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, M., Li, Z., Song, T. et al. Analysis of hospitalization expenditures and influencing factors for inpatients with chronic bronchitis based on SHA2011 in a central Province of China. Sci Rep 14, 23495 (2024). https://doi.org/10.1038/s41598-024-74521-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74521-2
Keywords
This article is cited by
-
Key factors associated with China’s basic medical insurance fund revenue-expenditure balance: a grey relational analysis
Cost Effectiveness and Resource Allocation (2025)