Abstract
Arthroscopic capsular release is a most well-known technique with favorable outcomes for frozen shoulder. However, considering the surgical trauma and the improvement of multisite injection, we design a study to compare the pain relief and safety of multisite injection (MI) versus arthroscopic capsular release (ACR) for frozen shoulder. A total of 80 patients with unilater al frozen shoulder were enrolled in this study. Group RBT (n = 40) received multisite injection (0.5% lidocaine and triamcinolone acetonide, once a week, no more than 2 injections), while Group ACR received arthroscopic capsular release. The following parameters were employed to compare: visual analog scale (VAS), range of motion (ROM), the Disability of Arm, Hand, and Shoulder (DASH) score and Oxford shoulder score (OSS). Side effects were also recorded. The VAS, ROM, DASH and OSS all improved significantly (P < 0.001). Internal rotation and external rotation at 1 month after operation were better in ACR group (40.35 ± 4.79 Vs 36.58 ± 7.49, 40.55 ± 4.37 Vs 38.63 ± 4.01, P = 0.009,0.043). However, no significance in terms of functional results and ROM was found at 6 months after operation. The OSS, DASH and VAS in patients with diabetes were 44.25 ± 3.05, 2.29 ± 1.12 and 0.50 ± 0.72, compared with 43.89 ± 3.09, 2.34 ± 1.49 and 0.29 ± 0.56 in patients without diabetes (P = 0.636, 0.889, 0.157). Multisite injection and arthroscopic capsular release are both effective treatments in the treatment of frozen shoulder. However, multisite injection is a simple, cost effective and superior alternative.
Similar content being viewed by others
What is known what is new
As a common musculoskeletal problem, frozen shoulder usually manifests with spontaneous shoulder pain and the progressive loss of joint movements (especially forward flexion, abduction and external rotation movements ). Till now, the controversy still exists about the optimal therapeutic approach.
Multisite injection and arthroscopic capsular release are both effective treatments in the treatment of frozen shoulder. However, multisite injection may be recommended as a primary screening test before choosing arthroscopic capsular release. Because multisite injection is simple, safe, and lower cost-effective.
Introduction
As a common musculoskeletal problem, frozen shoulder usually manifests with spontaneous shoulder pain and the progressive loss of joint movements (especially forward flexion, abduction and external rotation movements ). It accounts about 2–5% of all shoulder pains and predominantly targets the fourth and sixth decade1. Till now, there is no consensus about the precise mechanism of frozen shoulder. However, adhesive capsulitis of the anterior portion of the glenohumeral joint capsule plays an important role in pain & restriction of motion. The thickened coracohumeral ligament and inflammatory vascularity of rotator interval are main pathological mechanisms2. The hypermetabolic lesions are also confirmed in the rotator interval, anterior joint capsule, and axillary recess by a PET/CT study3.
Most patients can improve spontaneously about 12–24 months. However, about 11% patients continued experience disability even after seven years, and appropriate treatment (such as physical therapy, intra-articular steroid injections, surgical treatment) could rapidly shorten the duration of disability4. Steroid injection is an effective conservative treatment to improve pain and shoulder disability, but inconsistencies should be paid attention also5. Early arthroscopic intervention is recommended in patients who can’t tolerate the severe pain and functional disability6.
To the best of our knowledge, there has been little literature about the effectiveness about multisite injection for frozen shoulder. The primary purpose was to compare the functional prognosis and pain relief in patients treated with multisite injection or arthroscopic capsular release. The safety of multisite injection was also evaluated as a secondary endpoint.
Materials and methods
This retrospective comparative study was designed and approved by the Ethics Review Committee (2023-LL-020 LW). All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from all enrolled individuals. The written informed consent was obtained before study.
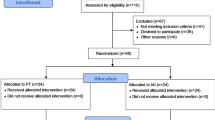
From Jun. 2020 to Dec. 2022, a total of 80 consecutive patients (45 females and 35 males) with unilateral frozen shoulder based on the American Shoulder and Elbow Surgeons consensus definition7, aged years (Range, 34 to 73 years), with a ratio of 1:1 case-matched, were enrolled in present study. MRI was performed in all patients in this study prior to intervention to exclude rotator cuff tear or other intrinsic shoulder pathology. G*Power was used to calculate the sample size. The sample size was estimated by G*Power. On the basis of our preliminary study, it was required to detect a significant difference (10 points) on DASH with a power of 80% at a type I error level of 0.05. Given an expected dropout rate of 20%, at least 40 patients were to be enrolled each group. All enrolled patients had persistent pain and limited motion despite conservative treatment including medications or physiotherapy. None patient has received a steroid injection before. These patients were divided into 2 groups based on treatment choice (MI or ACR). Group MI (n = 40) received regional injection (0.5% lidocaine and triamcinolone acetonide, once a week, no more than 2 injections), while Group ACR received arthroscopic capsular release. None significant difference was found in age, gender, side, body mass index (BMI), comorbidity (diabetics or not), dominant (yes/no), disease duration and range of motion in both groups (P < 0.05, Table 1). All patients undergo routine plain radiographs (true anteroposterior, 30 caudal tilt, and axial view) to detect calcific tendinitis or osteoarthritis.
Patients were excluded if they were secondary frozen shoulder, if they had other diseases before affecting the shoulder function, if they had rotator cuff tear or other intrinsic shoulder pathology based on magnetic resonance imaging (MRI) finding, if they had bilateral diseases, if they had hypersensitivity to steroids and lidocaine, if they had incomplete record of clinical data, if they were unable to adhere to entire trial procedures.
Multisite injection regime
The injections are administered and performed by one experienced orthopaedic surgeon at initial session. In the multisite-injection technique, 5 ml of triamcinolone acetonide (40 mg/ mL) and 5 ml of lidocaine (2%) was mixed in a 10 ml syringe. Usually, 4 ml was enough applied during the same session. Three following injection sites were used: (1) biceps long head, (2) posteroinferior capsule, and (3) coracohumeral ligament. If needed, other trigger point injections were added. All injections are administered by anatomical landmarks alone but not imaging guidance.
Patients with unsatisfactory improvement after 1 week were injected again, but no more than two injections were administered. To prevent and monitor potential adverse reactions, the patients are required to stay in hospital for half an hour after injection therapy.
Arthroscopic capsular release
The ACR was performed under general anesthesia by one experienced surgeon major in shoulder arthroscopy. Limited synoviectomy was performed using radiofrequency (RF) probe when proliferative synovitis was found. Arthroscopic selective capsular release is a gradual release process to avoid iatrogenic injury. The contracted rotator interval and anterior capsule were released. After operation, the inferior release was performed by gentle manipulation to prevent damage to the axillary nerve. If needed, posterior capsular release and/or subacromial decompression can be added to achieve better function8.
Physiotherapy regime
All patients underwent the same stepwise physiotherapy regime. It contained 6 sessions and performed every 2 days. Physiotherapy package included soft-tissue mobilization, joint mobilization and stretching exercises. The affected shoulder is manipulated with pain-free stretching to release the tight capsule.
Home exercise program is taught and carried out at home by themselves to preserve ROM two times a day (20 min each round)9. Celecoxib (200 mg PO) was administered twice daily for 1 week after treatment.
Parameters
The follow-up duration was defined as the interval between the last procedure and the latest follow-up. Patients were followed up with a minimum of 6 months.
All patents got followed-up at 1, 3, and 6 months.
Oxford shoulder score (OSS)
A patient self-reported assessment of shoulder function with 12-items measure. The total score ranges from 0 (indicating worst) to 48 (indicating best)10.
Disabilities of arm shoulder and hand (QuickDASH) score
QuickDASH was used to assess functional limitation measures of shoulder11.
Pain intensity
Visual analogue scale (VAS) score was employed to assess pain level form 0(indicating no pain) to 10 (indicating worst pain)12.
Range of motion (ROM)
ROM (including active forward flexion, abduction, internal rotation (IR), and external rotation (ER) values) were measured with a goniometer. by one orthopaedic physician blinded to both groups13.
Side effects
All side effects (including wound Healing; infections; injuries of nerve or blood vessel; septic arthritis) were also recorded.
Statistical analysis
Data analysis was undertaken by SPSS 24.0 (SPSS Inc, Chicago, IL, USA). The distribution was evaluated by Kolmogorov–Smirnov test. Continuous variables were reported as mean (standard deviation) or median (interquartile range) based on the normality distribution or not. Categorical variables were reported as numbers or percentages. Comparisons of both groups were evaluated by the independent Student t-test or χ2 test as appreciate. Repeated-measures analysis was used to evaluate the overall effect at different time. Statistical significance was set at P < 0.05.
Results
Of the 80 patients, 24 patients had diabetes (30.0%, 24 of 80 patients). The OSS, DASH and VAS in patients with diabetes were 44.25 ± 3.05, 2.29 ± 1.12 and 0.50 ± 0.72, compared with 43.89 ± 3.09, 2.34 ± 1.49 and 0.29 ± 0.56 in patients without diabetes (P = 0.636, 0.889, 0.157). 4 patients (10.0%) in MI group and 3 patients in ACR group (7.5%) complained that some of the original gained ROM had lost. 6 patients (15.0%) in MI group and 5 patients in ACR group (12.5%) had undergone second injections for pain relief. No more than 2 injections were given in all patients.
Pain
The VAS improved significantly from baseline in both groups (P < 0.001). At 6 months after operation, the VAS in MI group was 0.38 ± 0.63, compared with 0.33 ± 0.61 in ACR group (P = 0.720). 2 patients receiving multisite injection in MI group failed to get pain relief and got ACR eventually.
Range of motion
Internal rotation and external rotation at 1 month after operation were better in ACR group (40.35 ± 4.79 Vs 36.58 ± 7.49, 40.55 ± 4.37 Vs 38.63 ± 4.01, P = 0.009,0.043, Table 2). In term of ROM, none difference was found in any other times.
Functional scores
The OSS and DASH all improved significantly from baseline in both groups (P < 0.001), but no significant difference between both groups was found at 6 months after operation (P = 0.069, 0.107, Table 3).
Complications
None serious complication (such as infection, chondrolysis, dislocation and nerve injury) occurred. One patient had fat liquefaction, and healed after dressing changes.
Discussion
The main finding of this study was that we didn’t detect any significant difference in overall results at 6 months after operation. Patients in ACR group had better internal rotation and external rotation at 1 month after operation, but there was no significant difference in ultimate results.
Frozen shoulders typically affect multiple tissues, including glenohumeral joint capsule, rotator cuff tendons, and biceps long head. As an anterosuperior part of the joint capsule, thickened coracohumeral ligament (CHL) is an important manifestation of frozen shoulder, which is correlated with shoulder restriction. CHL can restraint against external rotation of shoulder. Entire coracohumeral ligament should be released preferentially to achieve better shoulder function and pain relief14. In present study, the site of coracohumeral ligament was injected in MI group, while the coracohumeral ligament was released during operation. The release of entire coracohumeral ligament can promote smooth movement of the supraspinatus, infraspinatus tendons and subscapularis tendon. And it can also regain ROMs in various directions15.
Till now, the controversy still exists about the optimal extent of capsular release. Jerosch et al. pointed that circumferential arthroscopic capsular release brought better prognosis in all patients with frozen shoulder16. In contrast, Snow et al. reported that the posterior release didn’t produce added benefits to function17. No better functional and pain relief was found by a complete 360 release. Posterior release can improve the early and sustained flexion improvements. However, internal rotation can be increased only in the early stage. Considering the similar results of 360◦ capsular release, the patients in ACR group received limited arthroscopic release.
An anatomic cadaveric study was conducted to detect the innervation of glenohumeral joint capsule. It concluded that the posteroinferior quadrant and anteroinferior quadrant was innervated by the axillary nerve. And the anterosuperior quadrant was innervated by the subscapular nerve, while the posterosuperior quadrant was innervated by the suprascapular nerve18. And the pathologic changes in frozen shoulder are not just observed in glenohumeral joint capsule. Therefore, multisite injections of different branches could supply an optimized pain relief. In present study, the VAS improved significantly from baseline in MI group (P < 0.05), and the VAS was 0.38 ± 0.63 at latest follow-up. Previous study also confirmed the effectiveness of multisite injection, it provided better pain relief with better r functional results19.
Compared with oral corticosteroid, periarticular corticosteroid injection is a good choice to reduce local inflammation around lesion with less systemic complications. Steroid injection inhibits capsular fibrosis by reducing the synovial inflammation. The addition of local anaesthetic injection contributes to achieve pain relief20. As a well-known long-acting glucocorticoid, triamcinolone acetonide exhibits a verified efficacy in the pain relief and function of shoulder. However, the drug administration amount dosage is still chosen empirically due to no consensus on the optical dosage. Local or systemic complications (such as hyperglycemia, cartilage degeneration and cartilage degeneration) may occur after excessive doses of corticosteroids is used. The minimum dose is needed to achieving painless outcome21. 40 mg triamcinolone acetonide showed better symptomatic improvements than that of 10 mg triamcinolone acetonide in patients with capsulitis of the shoulder22. Yoon et al. designed a randomized controlled clinical trial to compare the efficacy of different corticosteroid doses. And they suggested 20 mg triamcinolone acetonide as common practice. No significance was found in the Shoulder Pain and Disability Index (SPADI) and visual analog scale (VAS) between groups treated with 40 mg and 20 mg of corticosteroid23. We also proposed 20 to 40 mg as optical dose to achieve a favorable result.
In our opinion, the rotator interval should be paid more attention to improve the external rotation of the glenohumeral joint. We routinely give local injection into the rotator interval when patients with hand-behind-the-back (HBB). Hand-behind-the-back can induce accurate pain point and help to find precise injection location. Histological findings confirmed the existence of fibrosis, fibroid degeneration, newly formed collagen disposition, and hyalinization in the rotator interval24. Arthroscope biopsy material also confirmed the existence of chronic inflammation and active fibroblastic proliferation in the area of rotator interval. The high vascularity and nerve tissue explained the reason of painful shoulder2.
The incidence rate of frozen shoulder in patients with diabetes is about 2 to 4 times more common than that in the general population25. And patients with diabetes may have more severe and complex conditions, which increases the difficulty of treatment. Patients with diabetic may experience longer duration and persistent symptom after conservative treatment. Ineffective glycemic control is associated with worse shoulder pain and function. The microangiopathies such as neuropathy, retinopathy will increase the risk of surgical treatment needs26. In this study, diabetic patients didn’t show worse outcomes, it suggested that diabetes is not a contraindication. The ROM in patients with/without diabetics had no significant difference at 6 months after operation. The similar result was also reported in previous study27.
Physiotherapy plays an important role in improving ROM and reducing adhesions in shoulder capsule. However, pain relief is a prerequisite for physiotherapy28. Corticosteroid injection combined with manipulation can restore the shoulder function satisfactorily29. The addition of lidocaine can increase immediate analgesic effect before a physiotherapy session.
Limitations
There are certain limitations in this study. Firstly, a group with physical therapy alone is lacked. Secondly, home exercise program is taught and carried out at home, but compliance was not verified individually. And the dose of exercise was not controlled. Thirdly, the number of injection sites may increase the risk of homogeneity. A well-designed comparative study with longer follow-up time is needed.
Multisite injection and arthroscopic capsular release are both effective treatments in the treatment of frozen shoulder. However, multisite injection may be recommended as a primary screening test before choosing arthroscopic capsular release. Because multisite injection is simple, safe, and lower cost-effective.
Data availability
All data generated or analyzed during this study are included in this published article and are available from the corresponding author on reasonable request.
References
Itoi, E. et al. Shoulder stiffness: Current concepts and concerns. Arthroscopy. 32(7), 1402–1414 (2016).
Hand, G. C., Athanasou, N. A., Matthews, T. & Carr, A. J. The pathology of frozen shoulder. J. Bone Joint Surg. Br. 89, 928–932 (2007).
Kim du, H., Sung, D. H., Ga, H. Y. & Choi, J. Y. Metabolic patterns of the shoulder joint on (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in adhesive capsulitis. Ann. Nucl. Med. 28(2), 136–144 (2014).
Shaffer, B., Tibone, J. E. & Kerlan, R. K. Frozen shoulder. A long-term follow-up. J. Bone Joint Surg. Am. 74(5), 738–746 (1992).
Song, A., Higgins, L. D., Newman, J. & Jain, N. B. Glenohumeral corticosteroid injections in adhesive capsulitis: A systematic search and review. Pm r. 6, 1143–1156 (2014).
Ide, J. & Takaji, K. Early and long term results of the arthroscopic treatment of shoulder stiffness. J. Bone Joint Surg. 13, 174–179 (2004).
Zuckerman, J. D., Coumo, F. & Rokito, S. Definition and classification of frozen shoulder: A consensus approach. J. Shoulder Elb. Surg. 3(S1), S72 (1994).
Ozbaydar, M. U., Tonbul, M., Altun, M. & Yalaman, O. Donuk omuz hastaliğinin tedavisinde artroskopik selektif kapsül gevşetmesi [Arthroscopic selective capsular release in the treatment of frozen shoulder]. Acta Orthop. Traumatol. Turc. 39(2), 104–113 (2005).
Griggs, S. M., Ahn, A. & Green, A. Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J. Bone Joint Surg. Am. 82, 1398–1407 (2000).
Dawson, J., Rogers, K., Fitzpatrick, R. & Carr, A. The Oxford Shoulder score revisited. Arch. Orthop. Trauma. Surg. 129(1), 119–123 (2009).
Beaton, D. E., Wright, J. G., Katz, J. N. & the Upper Extremity Collaborative Group. Development of the QuickDASH: Comparison of three item-reduction approaches. J. Bone Joint Surg. Am. 87(5), 1038–1046 (2005).
Stubbs, D. F. Visual analogue scale. Br. J. Clin. Pharmacol. 7(1), 124 (1979).
Hagiwara, Y. et al. Effects of Arthroscopic Coracohumeral Ligament Release on Range of Motion for patients with Frozen Shoulder. Open. Orthop. J. 12, 373–379 (2018).
Hagiwara, Y. et al. Clinical outcomes of arthroscopic pan-capsular release with or without entire coracohumeral ligament release for patients with frozen shoulder. JSES Int. 4(4), 826–832 (2020).
Kanbe, K. Clinical outcome of arthroscopic capsular release for frozen shoulder: Essential technical points in 255 patients. J. Orthop. Surg. Res. 13(1), 56 (2018).
Jerosch, J., Nasef, N. M., Peters, O. & Mansour, A. M. Mid-term results following arthroscopic capsular release in patients with primary and secondary adhesive shoulder capsulitis. Knee Surg. Sports Traumatol. Arthrosc. 21, 1195–1202 (2013).
Sivasubramanian, H. et al. Arthroscopic capsular release to treat idiopathic frozen shoulder: How much release is needed? Orthop. Traumatol. Surg. Res. 107(1), 102766 (2021).
Tran, J., Peng, P. W. H. & Agur, A. M. R. Anatomical study of the innervation of glenohumeral and acromioclavicular joint capsules: Implications for image-guided intervention. Reg. Anesth. Pain Med. 44, 452–458 (2019).
Koraman, E., Turkmen, I., Uygur, E. & Poyanlı, O. A Multisite Injection is more effective than a single glenohumeral injection of corticosteroid in the treatment of primary frozen shoulder: A Randomized Controlled Trial. Arthroscopy. 37(7), 2031–2040 (2021).
Kitridis, D., Tsikopoulos, K., Bisbinas, I., Papaioannidou, P. & Givissis, P. Efficacy of pharmacological therapies for adhesive capsulitis of the shoulder: A systematic review and network meta-analysis. Am. J. Sports Med. 47, 3552–3560 (2019).
Jacobs, J. W. How to perform local soft-tissue glucocorticoid injections. Best Pract. Res. Clin. Rheumatol. 23, 193–219 (2009).
Yoon, S. H., Lee, H. Y., Lee, H. J. & Kwack, K. S. Optimal dose of intra-articular corticosteroids for adhesive capsulitis: A randomized, triple-blind, placebo-controlled trial. Am. J. Sports Med. 41, 1133–1139 (2013).
Sun, Y., Liu, S., Chen, S. & Chen, J. The Effect of Corticosteroid Injection into Rotator interval for early frozen shoulder: A Randomized Controlled Trial. Am. J. Sports Med. 46(3), 663–670 (2018).
Thomas, S. J. et al. Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J. Shoulder Elb. Surg. 16, 748–751 (2007).
Cho, C. H., Jin, H. J. & Kim, D. H. Comparison of clinical outcomes between idiopathic frozen shoulder and diabetic frozen shoulder after a single ultrasound-guided intra-articular corticosteroid injection. Diagnostics (Basel). 10(6), 370 (2020).
Whelton, C. & Peach, C. A. Review of diabetic frozen shoulder. Eur. J. Orthop. Surg. Traumatol. 28, 363–371 (2018).
Yanlei, G. L., Keong, M. W. & TijauwTjoen, D. L. Do diabetic patients have different outcomes after arthroscopic capsular release for frozen shoulder? J. Orthop. 16(3), 211–215 (2019).
Zhang, K., de Sa, D., Kanakamedala, A., Sheean, A. J. & Vyas, D. Management of concomitant preoperative rotator cuff pathology and adhesive capsulitis: A systematic review of indications, treatment approaches, and outcomes. Arthroscopy. 35, 979–993 (2019).
Jacobs, L. G., Smith, M. G., Khan, S. A., Smith, K. & Joshi, M. Manipulation or intraarticular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. J. Shoulder Elb. Surg. 18, 348–353 (2009).
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
X.J. and Z.Y. conceived the idea of the study and participated in the design of the study. l.M., X.Z. and S.J analysis the data and write the final manuscript. Z.M., Q.K., and L.K. performed acquisition of data. W.Q. and P.X. performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study was reviewed and approved by the Ethics Review Committee of Changzhou hospital affiliated to Nanjing University of Chinese Medicine. The written informed consent was obtained before study.
Consent for publication
N/R.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, M., Xu, Z., Shi, J. et al. A retrospective comparative study on the effectiveness of multisite injection versus arthroscopic capsular release for idiopathic frozen shoulder. Sci Rep 14, 24303 (2024). https://doi.org/10.1038/s41598-024-74582-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74582-3