Abstract
This study investigates the correlation between dietary sialic acid intake which mainly come from eggs, red meat, and dairy products and serum HbA1c levels. A survey among Xiamen’s general population, China, collected dietary data from 2,908 participants over the past year. A semi-quantitative food frequency questionnaire (FFQ) was employed. Sialic acid intake was calculated, along with measurements of biochemical indicators, including fasting blood glucose, HbA1c, blood lipids, and insulin. Sociodemographic and physical data were also collected. Logistic regression models evaluated the relationship between dietary sialic acid and HbA1c levels. The daily sialic acid intake in Xiamen’s general population was 48.55 (21.68, 65.23) mg/1000Kcal, accompanied by a 1.96% rate of high HbA1c. A significant negative correlation between dietary sialic acid and HbA1c was observed. Individuals in the highest quartile of sialic acid intake (> 65.48 mg/1000 kcal) had a lower risk of high HbA1c compared to those in the lowest quartile (< 23.63 mg/1000 kcal) [OR: 0.123 (0.022, 0.689)]. A high dietary sialic acid intake within a specific range may reduce the risk of elevated HbA1c levels, suggesting a potential preventive effect. Note that this effect is limited to specific intake ranges.
Similar content being viewed by others
Abbreviations.
Body mass index(BMI)
Diastolic blood pressure(DBP)
Fasting blood glucose(FBG)
Glycated hemoglobin(HbA1c)
High-density lipoprotein cholesterol(HDL)
Hypersensitive C-reactive protein(hs-CRP)
Insulin(INS)
Insulin resistant index(IRI)
Low- density lipoprotein cholesterol(LDL)
Sialic acids (SA)
Systolic blood pressure(SBP)
Total cholesterol(TC)
Triglycerides(TG)
Uric acid(UA)
Introduction
Diabetes, a complex and heterogeneous condition, often leads to progressive multi-organ damage1. In recent years, there has been a notable increase in the prevalence of diabetes worldwide. Currently, the global adult prevalence of diabetes exceeds 9.8% of the world’s population2. The prevalence of diabetes in the study population was approximately 10.6%3. In diabetic patients, elevated blood glucose and associated factors alter the structure, function, and lifespan of red blood cells. Non-enzymatic binding of glucose with hemoglobin forms glycosylated hemoglobin4. Glycosylated hemoglobin is categorized into three types: A1c, B, and C, with HbA1c being predominant5,6. It results from hemoglobin’s glycation in circulating red blood cells. Thus, serum HbA1c levels serve as a crucial indicator for retrospectively assessing glycemic status over the preceding 2–3 months.
The elevation of glycosylated hemoglobin not only exacerbates the burden of diabetes-related damage on the organism but may also impair functions, including compromised blood oxygen transport, association with cancer, onset of metabolic syndrome, increased risks of all-cause and cardiovascular mortality, and heightened susceptibility to chronic diseases7,8,9,10,11,12,13,14. While the correlation between elevated glycosylated hemoglobin levels and blood glucose levels is well-established, its link to red blood cell membrane stability has been underappreciated in previous research. However, sialic acid has been found to be significantly linked to the stability of red blood cell membranes15,16, highlighting its importance in this aspect.
Sialic acids (SA) occupy the terminal positions of glycoprotein and glycolipid carbohydrate chains, representing a diverse family of sugar units17,18. They are electronegative monosaccharides found in higher animals and certain microorganisms, serving as the outermost units of polysaccharide chains on the cell surface and secreted glycoproteins of all vertebrates19. Sialic acid is an essential negatively charged component of the red blood cell membrane20. It crucially maintains membrane stability, elasticity, and resilience, ensuring red blood cells’ stability in the bloodstream. This effectively prevents abnormal adhesion between red blood cells and between red blood cells and the vascular wall. Human red blood cells contain primarily N-acetylneuraminic acid (Neu5Ac) as their sialic acid component, which accounts for 74-94% of the negative charge on the cell membrane surface21. Research indicates that sialic acids, especially Neu5Ac, regulate the morphology and oxygenation capacity of intracellular hemoglobin in red blood cells, affecting their structure and distribution22. Insufficient sialic acid content can compromise the integrity of the red blood cell membrane, leading to decreased deformability and increased susceptibility to external factors. This can result in elevated levels of HbA1c.
The human body can ingest and utilize foods containing sialic acid23. A diet rich in sialic acid, such as those in edible bird’s nest, red meats, breast milk, bovine milk, and eggs24, holds promise in protecting red blood cells and preventing elevated HbA1c levels. Hence, we conducted a cross-sectional study to assess how sialic acid intake impacts HbA1c levels and whether it can mitigate elevated HbA1c levels.
Materials and methods
Human subjects
This study took place from April to August 2016 across four Xiamen City districts: Siming, Huli, Xiang’an, and Haicang. We selected 2,908 permanent residents aged 18 + using a multi-stage stratified random sampling method, considering factors like geographical location and economic status. Exclusions were made for individuals with major illnesses, severe physical disabilities, communication difficulties, or those who refused participation. Informed consent was mandatory for all participants.
Data collection
Data collection included socio-demographic information, dietary intake, anthropometric measurements, and biochemical exams. Individual socio-demographic information included personal history, medical history, family history, and other relevant factors. Dietary intake was assessed using a semi-quantitative FFQ method. Anthropometric measurements included height, weight, waist circumference, hip circumference, and blood pressure. Biochemical examinations included fasting blood glucose, HbA1c, high-sensitivity C-reactive protein, lipid profile, and other relevant factors (Medical history referred to previously diagnosed diseases). All participants underwent routine blood tests and biochemical assessments. Blood samples were collected in vacuum tubes with anticoagulants. Participants were required to fast for at least 10 h before blood collection. A 5 ml blood sample was centrifuged to separate the serum. The serum was then used to measure fasting blood glucose, glycosylated hemoglobin (HbA1c), uric acid (UA), cholesterol (TC), triglycerides (TG), low-density lipoprotein (LDL-C), high-density lipoprotein (HDL-C), high-sensitivity C-reactive protein (hs-CRP), and insulin (INS) levels. HbA1c measurements followed ion exchange chromatography per manufacturer instructions.
Indicator classification
HbA1c: HbA1c ≥ 6.5% is considered elevated, while < 6.5% is deemed normal, the American Diabetes Association has established an HbA1c of 6.5% as a diagnostic criterion25.
BMI: Body mass index (BMI) ≥ 25 indicates overweight, while < 25 suggests non-overweight, BMI is calculated by dividing a person’s weight in kilograms by their height in meters squared (kg/m2). The World Health Organization employs a BMI of 25 as the threshold for overweight26.
High-sensitivity C-reactive protein: ≥ 2 mg/L indicates inflammation, while < 2 mg/L indicates no inflammation, an elevation in high-sensitivity C-reactive protein (hs-CRP) serves as a sensitive indicator of systemic inflammation and is linked to the onset of early atherosclerotic changes, thereby predicting an increased risk of cardiovascular disease. An hs-CRP level exceeding 2 mg/L was identified as a significant risk factor for cardiovascular disease27.
Calories: Intake < 1800 Kcal is considered inadequate, while intake ≥ 1800 Kcal is deemed adequate, according to a report called the Dietary Reference Intakes for Energy, Carbohy-drate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids28. This index is also used to standardize dietary sialic acid intake.
Insulin index: An index ≥ 2.69 indicates insulin resistance, while < 2.69 is considered normal. The insulin resistance index is calculated by fasting insulin (uU/mL) x fasting blood glucose (mmol/L)/22.5, insulin resistance was defined as a suitable insulin index ≥ 2.69 for Chinese people29, insulin resistance, defined as the diminished physiological role of insulin in the body, is a prevalent pathological mechanism in the development of numerous metabolic disease processes.
Fasting blood glucose: ≥ 6.1 mmol/L is considered elevated, while < 6.1 mmol/L is deemed normal, a fasting blood glucose level ≥ 6.1 mmol/L may indicate the presence of impaired fasting blood glucose30.
Lipid profile: Total cholesterol ≥ 5.18 mmol/L is classified as elevated, while < 5.18 mmol/L is considered normal, a total cholesterol concentration ≥ 5.18 mmol/L is indicative of hyperlipidemia31.
Triglycerides: ≥ 1.7 mmol/L is considered elevated, while < 1.7 mmol/L is deemed normal, serum triglyceride levels ≥ 1.7 mmol/L are an independent risk factor of type 2 diabetes32.
Low-density lipoprotein: ≥ 3.12 mmol/L is considered elevated, while < 3.12 mmol/L is deemed normal, LDL ≥ 3.12 mmol/L is a risk factor for diabetes33.
High-density lipoprotein: < 1.55 mmol/L is considered too low, while ≥ 1.55 mmol/L is deemed normal, a level of HDL below 1.55 mmol/L is associated with an increased risk of developing cardiovascular disease34.
Income: < 3,000 yuan are typically classified as low-income, while income ≥ 3000 yuan are considered to be at the normal income level35.
Hypertension: ≥140/90 mmHg is considered hypertension, < 140/90 mmHg is normal, according to a report called Guidelines for Prevention and Treatment of Hypertension in China (3rd Edition)36.
Sialic acid intake
Sialic acid intake was calculated by assessing consumption frequency and portion sizes from the questionnaire. The intake of each type of food was computed, and then the total sialic acid intake for each participant was calculated based on the sialic acid content in each food item. Finally, the total energy intake was used to make correction37,38.
Statistical analysis
Data analysis in this study was conducted using IBM SPSS Statistics for Windows (Version 20.0, Armonk, NY: IBM Corp.) and R (version 4.1.3; R Core Team, Vienna, Austria). Participants were divided into two groups based on their HbA1c levels: elevated (≥ 6.5%) and normal (<6.5%). Descriptive statistics were used to present participant characteristics, with continuous data reported as Mean ± SD or median (P25, P75) and categorical data as frequencies or percentages. We used multivariable logistic regression to analyze the relationship between sialic acid intake and glycated hemoglobin. Models were adjusted as follows: Model 1 for age, sex, and BMI; Model 2 for biochemical indicators; Model 3 for lifestyle habits; and Model 4 is the complete model, adding disease state, total energy, and primary sialic acid source food. Sialic acid intake and its quartiles were entered into the model separately for trend tests. The hypothesis testing significance level was set at α = 0.05.
Subgroup analyses, based on factors like age, sex, BMI, income, and specific health indicators, explored the relationship between sialic acid intake and glycated hemoglobin. Additionally, Model Four explored interactions between different indicators and sialic acid, followed by sensitivity analysis to validate model stability.
Additionally, we sought to ascertain the relationship between different levels of sialic acid and the main source food of sialic acid, and conducted descriptive statistics and Pearson correlation analysis.
Result
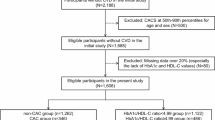
Characteristics of the study population
Of the 2,908 adults studied, 57 had glycated hemoglobin levels above 6.5%, yielding a 1.96% prevalence rate (Table 1). The study focused on a generally healthy adult population. Sialic acid intake among adults with elevated glycated hemoglobin levels averaged 28.65 (10.17, 55.53) mg/1000 kcal, compared to 48.62 (21.81, 65.28) mg/1000 kcal in those with normal levels (P < 0.001). Individuals with high HbA1c levels had lower energy and HDL-C levels, but exhibited higher BMI, blood pressure (systolic and diastolic), waist and hip circumferences, hs-CRP, insulin, total cholesterol, LDL-C, triglycerides, fasting blood glucose and insulin resistance index. All these differences reached statistical significance.
Characteristics of sialic acid intake
The survey comprised 1,138 males (39.13%) and 1,770 females (60.87%). Female participants exhibited significantly higher sialic acid intake compared to males. Sialic acid intake was highest among unmarried individuals and lowest among divorced ones. Sialic acid intake rose with education level, but declined at the graduate level and above, dipped for incomes between less than 1,000 to 8,000, and increased again for incomes over 8,000. Former smokers had significantly lower sialic acid intake than other groups. Sialic acid intake showed variation across age groups. Sialic acid intake is higher in people with lower BMI. Differences in sialic acid intake based on total cholesterol levels were not significant. However, higher low-density lipoprotein and triglycerides were associated with lower sialic acid intake. Conversely, higher high-density lipoprotein levels correlated with increased sialic acid intake. Additionally, lower sialic acid intake was observed in individuals with hypertension, insulin resistance, and elevated fasting glucose levels. Notably, the primary sources of sialic acid were eggs (55%), red meat (25%), and dairy products (12%). The detail information was showed in Table 2.
Relationship between dietary sialic acid and hba1c
We conducted multivariable logistic regression analysis to explore the relationship between dietary sialic acid and HbA1c levels. Four models were established: basic, biochemical indicator adjustment, lifestyle adjustment, and disease influence. Across all four models, dietary sialic acid’s odds ratios (ORs) were below 1 and statistically significant (P < 0.05). Dietary sialic acid intake was categorized into quartiles, and the results for the highest quartile: lowest quartile were significant (P < 0.05). Model 4 revealed progressively decreasing ORs across quartiles, with 95% CIs for high HbA1c at 0.459 (0.098, 2.156), 0.545 (0.118, 2.508), and 0.051 (0.007, 0.367), a trend mirrored crudely in the other models. Trend tests across all models demonstrated significant trends for sialic acid quartiles (P < 0.001). Concurrently, we construct trend figures for the four models, which reveal a notable decline in the probability of elevated HbA1c levels with daily intake of sialic acid. This indicates that higher sialic acid intake could potentially prevent elevated HbA1c levels. The detail information was showed in Table 3.
Subgroup analysis of dietary sialic acid and hba1c
Stratified logistic regression analysis to identify variables that modify the correlation between dietary Sialic acid and HbA1c. Complete model: Adjusted SA, Gender, BMI, Age, UA, hs-CRP, TG, LDL-C, HDL-C, IRI, FBG, Income, Smoke status, Culture, Marital status, Tea-drinking habit, Alcohol consumption, hypertension, DM, CVD, RA, HUA, Total energy, Primary sialic acid source food.
We conducted stratified analyses with complete model to explore if the relationship between dietary sialic acid intake and elevated HbA1c levels was consistent across subgroups. We calculated multiplicative interactions between sialic acid intake and each covariate. Figure 1 illustrates that the association between age (≥ 55 years, < 55 years), sex (male, female), BMI (≥ 25, < 25), income (≥ 3,000 yuan, < 3,000 yuan), total cholesterol (≥ 5.18 mmol/L, < 5.18 mmol/L), insulin resistance index (≥ 2.69, < 2. 69), low-density lipoprotein (≥ 3.12 mmol/L < 3.12 mmol/L), HDL (≥ 1.55 mmol/L, < 1.55 mmol/L), triglycerides (≥ 1.7 mmol/L, < 1.7 mmol/L), and ultrasensitive C-reactive protein (≥ 2 mg/L, < 2 mg/L) were stable with ORs < 1 in all subgroups. Only the ultrasensitive C-reactive protein subgroup (≥ 2 mg/L, < 2 mg/L) had a significant interaction (P < 0.05). This indicates a more pronounced protective effect of sialic acid against elevated HbA1c in individuals with inflammation (CRP > 2 mg/L). The detail information was showed in Fig. 2.
Sensitivity analysis of logistic regression model
Sensitivity Analysis 1: Exclusion of Outliers: (a) Exclusion of extreme sialic acid intake (≥ 120 mg/1000 kcal). (b) Exclusion of extreme BMI levels (< 16 or > 30). (c) Exclusion of extreme energy intake levels (< 1000 kcal and > 4000 kcal).
Sensitivity Analysis 2: Exclusion of diabetic patients.
Sensitivity Analysis 3: Exclusion of patients with hypertension, hyperuricemia, gout, and other related conditions.
Sensitivity Analysis 4: Imputation of missing data in biochemical indicators using the median.
Sensitivity Analysis 5: Exclusion of frequent smokers.
The trends from the five sensitivity analyses align with the original model, demonstrating its stability. The detail information was showed in Table 4.
Relationships between different levels of hba1c and the main source of sialic acid
The main sources of dietary sialic acid are red meat, eggs and milk. To inform our dietary guidance, we examined the intake of major sialic acid sources in relation to HbA1c levels. Our findings revealed no significant differences in red meat intake, whereas there were notable differences in egg and milk consumption.
Furthermore, Pearson correlation analysis was conducted using all HbA1c data in conjunction with three major sialic acid source foods. The results demonstrated a significant negative correlation between HbA1c and egg and milk intake, but not with red meat intake. We also did a correlation analysis of these three foods, we found that the intake of eggs and milk is negatively correlated with that of red meat, which may be the difference between dietary patterns. The full details are presented in Table 5.
Discussion
Results and potential mechanisms
The study reported a dietary sialic acid intake of 48.55 (21.68, 65.23) mg/1000 kcal and a 1.96% rate of elevated HbA1c among the surveyed population. Logistic regression revealed a significant negative correlation between dietary sialic acid intake and elevated HbA1c levels. The protective effect of dietary sialic acid only occurs when a certain amount of sialic acid intake (> 65.48 mg/1000 Kcal). This is consistent with previously available research39. Prior research has demonstrated that dietary sialic acid can interact with the gut microbiota and exert an influence on the human body via the gut–brain axis. Moreover, sialic acid can be utilized for the proliferation of bacteria in the oral cavity or intestine, and plays a pivotal role in symbiosis and colonization. Sialidase-producing bacteria are capable of releasing sialic acid from mucosal tissue or dietary sources for utilization by themselves or other bacteria40. The regulatory effect of sialic acid on the gut microbiota of individuals with diabetes or hypertension may provide an explanation for our observed results. Moreover, an exhaustive search of the literature revealed no other pertinent population studies of dietary sialic acid.
In addition to this, dietary sialic acid supplementation can restore sialic acid levels in the body and treat certain diseases caused by sialic acid deficiency23. Exogenous sialic acid supplementation has been shown to influence glucose metabolism in pregnant women, potentially protecting against gestational diabetes, by functioning as a prebiotic to modify the gut microbiota and maintain glucose metabolism stability41. Furthermore, sialic acid-rich foods may be beneficial in alleviating liver cancer, atherosclerosis, type 2 diabetes, and colon cancer. This is primarily due to their ability to modulate the immune system, expression of inflammation, and intestinal microbiota homeostasis42. However, we propose that dietary sialic acid’s impact on glucose metabolism operates through its effects on the erythrocyte membrane.
The glycation of mammalian hemoglobin is a non-enzymatic process influenced by three primary variables: the average plasma glucose concentration, the lifespan of red blood cells, and the permeability of red blood cells to glucose43. Our study revealed that the group with high fasting blood sugar had lower sialic acid intake, while the insulin-resistant and high-insulin groups had higher sialic acid intake. Research has demonstrated that mice deficient in sialic acid display increased insulin sensitivity44, which is in line with our findings. Our findings indicate that sialic acid-rich foods, including eggs and meat, have high fat and protein levels, affecting blood sugar levels. This complicating factor is challenging to eliminate and necessitates additional experimental verification. However, research suggests that desialylation of insulin receptors (IR) can lead to insulin resistance, resulting in elevated blood sugar levels. Desialylation of neuraminidase-1 promotes insulin resistance by disrupting IR signaling transduction and the binding of insulin to the L1 domain45. The relationship between sialic acid load and insulin and blood sugar is still controversial. Therefore, we speculate that the negative correlation between sialic acid and HbA1c is closely related to the stability of the red blood cell membrane. This is because sialic acid can influence the lifespan of red blood cells and their glucose permeability.
The study results indicate a negative correlation between dietary sialic acid and HbA1c. Additionally, the red blood cell membrane is associated with both sialic acid and HbA1c. Previous studies have shown an association between sialic acid on the red blood cell membrane and diabetes. Quantitative analysis of sialic acid on the red blood cell membrane is becoming an important clinical parameter for diagnosing cancer and diabetes46,47. When determining the components of red blood cell membranes in individuals with insulin-dependent diabetes, it has been observed that there is a significant increase in phospholipids and cholesterol, while there is a significant decrease in sialic acid and protein content. Insufficient expression of sialic acid is considered an indicator of diabetes. According to a study48, individuals with insulin-dependent diabetes have 38% lower expression of red blood cell membrane SA compared to healthy individuals. Additionally, the levels of LPO-RBC and SA in red blood cells can be used to predict diabetic nephropathy49. Research suggests that there is a positive correlation between serum sialic acid levels and glycosylated hemoglobin. An increase in serum sialic acid is also indicative of a decrease in membrane sialic acid50. Therefore, some studies propose that there is an increase in serum sialic acid in diabetes. These findings suggest an association between sialic acid deficiency on the red blood cell membrane and diabetes, as well as HbA1c.
Possible mechanisms: The lifespan profile of erythrocytes is inversely related to the amount of HbA1c on the erythrocyte membrane43. Erythrocyte rejuvenation is contributed by the sialic acid content of the erythrocyte membrane, which keeps overall erythrocytes in a more youthful state, while the total number of erythrocytes remains essentially unchanged51. Research has shown that 50% of total HbA1c is formed in the month prior to death, during the senescent state52, and sialic acid can slow down glycation by slowing down erythrocyte senescence very well.
HbA1c is related to the deformability of red blood cells53. Sialic acid helps to maintain the stability of red blood cells, preventing cell aggregation and hemolysis. It regulates the morphology, membrane deformability, and oxygenation capacity of intracellular hemoglobin molecules, as well as the structure and distribution of intracellular hemoglobin molecules in human red blood cells22. Moreover, it has been found that high levels of sialic acid can decrease the formation of atherosclerotic plaques, reduce blood shear forces, increase sialic acid on red blood cells, and thus protect red blood cell deformability, ultimately leading to a decrease in the formation of HbA1c20. The results of our study indicate that individuals who consume higher amounts of sialic acid have lower blood lipid levels and HbA1c levels. The findings of studies indicate that higher HbA1c levels are associated with an increased risk of atherosclerosis54, which is in line with our own findings.
According to previous research and the findings of our current investigation, it is believed that the dietary intake of sialic acid can protect the red blood cell membrane, thus preventing the glycation of hemoglobin. It is therefore recommended that an adequate intake of dietary sialic acid be ensured. The sialic acid in the population under examination was primarily derived from eggs, red meat, and milk, a finding that is consistent with the dietary patterns observed in most regions of the globe24. However, some studies have also pointed out that red meat is not good for health, so it should not be consumed in large quantities, but in moderation with non-excess eggs, which have a high content of sialic acids and do not pose much of a health burden55. Our study also shows that different levels of HbA1c are associated with eggs and milk, while the association with red meat is not significant. Additionally, there are specific sialic acid-rich foods, such as bird’s nest, which contain elevated levels of sialic acid and can be incorporated into one’s diet in moderation if accessible56.
Advantages and limitations
Advantages: Most studies have considered sialic acid as a biomarker for diseases such as diabetes57,58. Our research is pioneering in establishing a link between dietary sialic acid and HbA1c, highlighting its potential as a protective factor against glycosylated hemoglobin. This discovery could facilitate lifestyle changes and the adoption of targeted diets to prevent the rise of HbA1c in certain populations. Our study includes several biochemical indicators and lifestyle habits that are essential for public health. This provides a better understanding of disease causality and insights for public health nutrition policies. The research holds greater significance for the general population due to the substantial inclusion of healthy individuals. Additionally, our questionnaire uses a FFQ that covers the past year, which is more meaningful for long-term indicators such as HbA1c.
Limitations: The cross-sectional design of the study limits it to detecting associations without establishing causality or temporal relationships. To discern such relationships, longitudinal data are required. Furthermore, it is important to note that FFQs are less accurate than 24-hour recalls and food records. As a method relying on long-term memory, FFQs may introduce recall and reporting biases59. The selection of voluntary participants may introduce bias due to their specific characteristics.
Conclusion
The global prevalence of diabetes underscores the significance of our findings. This study’s results indicate that dietary sialic acid may help prevent excessive HbA1c levels to some extent, providing a viable strategy for lowering HbA1c. These results advocate for a diet high in sialic acid and low in fat and protein to potentially mitigate elevated HbA1c levels.
Additional requirements
N/A.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to including personal medical and life information. But the datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Zucchini, S. Clinical aspects of different forms of diabetes in children and adolescents. Front. Endocrinol., 13. (2022).
Communication, I. Global Diabetes data report 2000–2045. ; (2024). https://diabetesatlas.org/data/en/world/
Communication, I. China Diabetes report 2000–2045. ; (2021). https://diabetesatlas.org/data/en/country/42/cn.html
Bunn, H. F., Gabbay, K. H. & Gallop, P. M. The glycosylation of Hemoglobin: relevance to diabetes Mellitus. Science. 200 (4337), 21–27 (1978).
Williams, A. et al. Pathophysiology of Red Blood Cell Dysfunction in Diabetes and its complications. Pathophysiology. 30 (3), 327–345 (2023).
Nitin, S. HbA1c and factors other than diabetes mellitus affecting it. Singap. Med. J.51 (8), 616–622 (2010).
Simmons, D. Increased red cell count in diabetes and pre-diabetes. Diabetes Res. Clin. Pract.90 (3), e50–e53 (2010).
Kim, J. Y. et al. Glycated hemoglobin and Cancer risk in Korean adults: results from Korean Genome and Epidemiology Study. Clin. Nutr. Res.7 (3), 170–177 (2018).
Jung, J. Y. et al. Association of fasting glucose and glycated hemoglobin with the long-term risk of incident metabolic syndrome: Korean Genome and Epidemiology Study (KoGES). Acta Diabetol.56 (5), 551–559 (2019).
de Vegt, F. et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia. 42 (8), 926–931 (1999).
Song, B. M. et al. Association between Haemoglobin A1c and all-cause and cause-specific Mortality in middle-aged and Older Koreans: A Prospective Cohort Study19 (Nutrition & Metabolism, 2022). 1.
Wu, X. L. et al. The correlation between the glycated hemoglobin (HbA1c) in non diabetics and cardiovascular risk factors. Pak. J. Pharm. Sci.29 (1), 315–319 (2016).
Wei, Q. Q. et al. Blood hemoglobin A1c levels and amyotrophic lateral sclerosis survival. Mol. Neurodegeneration, 12. (2017).
Koshi, T. et al. Elevated haemoglobin A1c but not fasting plasma glucose conveys risk of chronic kidney disease in non-diabetic individuals. Diabetes Res. Clin. Pract.146, 233–239 (2018).
Mahajan, V. S. et al. Alterations in sialic-acid O-acetylation glycoforms during murine erythrocyte development. Glycobiology. 29 (3), 222–228 (2019).
Bruno, C. & Cuppini, R. The importance of N-acetylneuraminic acid and of its interaction with ca + + in the stability of the erythrocytic membrane. Bollettino Della Soc. Italiana Di Biol. Sper.57 (21), 2144–2150 (1981).
Angata, T. & Varki, A. Chemical Diversity in the sialic acids and related α-Keto acids: an evolutionary perspective. Chem. Rev.102 (2), 439–470 (2002).
Varki, A. Glycan-based interactions involving vertebrate sialic-acid-recognizing proteins. Nature. 446 (7139), 1023–1029 (2007).
Schauer, R. Sialic acids: fascinating sugars in higher animals and man. Zoology. 107 (1), 49–64 (2004).
McNamee, A. P., Tansley, G. D. & Simmonds, M. J. Sublethal mechanical trauma alters the electrochemical properties and increases aggregation of erythrocytes. Microvasc. Res.120, 1–7 (2018).
Cook, G. M., Heard, D. H. & Seaman, G. V. Sialic Acids Electrokinetic Charge Hum. Erythrocyte Nat., 191: 44–47. (1961).
Huang, Y. X. et al. Restoring the youth of aged red blood cells and extending their lifespan in circulation by remodelling membrane sialic acid. J. Cell. Mol. Med.20 (2), 294–301 (2016).
Okuda, T. Dietary Control of Ganglioside expression in mammalian tissues. Int. J. Mol. Sci.21 (1), 177 (2020).
Zhang, T. T., Wu, J. R. & Zhan, X. B. Dietary Sialic Acids: Distribution, Structure, and Functions (Critical Reviews in Food Science and Nutrition, 2023).
Rossi, G. & American Diabetes, A. Diagnosis and classification of diabetes mellitus. Recenti Prog. Med.101 (7–8), 274–276 (2010).
Consultation, W. H. O. Who, and Who, Obesity: Preventing and managing the global epidemic - Introduction, in Obesity: Preventing and Managing the Global Epidemic: Report of a Who Consultation. pp. 1-253. (2000).
Goff, D. C. Jr. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. Circulation. 129 (25 Suppl 2), S49–73 (2014).
Trumbo, P. et al. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J. Am. Diet. Assoc.102 (11), 1621–1630 (2002).
S.I.R.S.G., C. D. (ed) (preparatory)., Expert guidance on insulin resistance assessment methods and applications. Chin J Diabetes Mellitus., (2018).
Khan, S. H. et al. Frequency of impaired glucose tolerance and diabetes mellitus in subjects with fasting blood glucose below 6.1 mmol/L (110 mg/dL). East. Mediterr. Health J.19 (2), 175–180 (2013).
Wang, T. et al. Ratio of remnant-like particle-cholesterol to serum total triglycerides is an effective alternative to Ultracentrifugal and Electrophoretic methods in the diagnosis of familial type III hyperlipoproteinemia. Clin. Chem.45 (11), 1981–1987 (1999).
Guerrero-Romero, F. & Rodríguez-Moran, M. Hypertriglyceridemia is associated with development of metabolic glucose disorders, irrespective of glucose and insulin levels: a 15-year follow-up study. Eur. J. Intern. Med.25 (3), 265–269 (2014).
Zhang, B. et al. Epidemiological survey of chronic vascular complications of type 2 diabetic in-patients in four municipalities. Zhongguo yi xue ke xue yuan xue bao. Acta Academiae Medicinae Sinicae. 24 (5), 452–456 (2002).
Hu, Y. et al. The association between HDL-C and stroke in the middle-aged and elderly: a cross-sectional study. Brain Behav., 13(3). (2023).
Statistics, N. B. Statistical Bulletin of the People’s Republic of China on National Economic and Social Development for 2022. ; (2023). https://www.stats.gov.cn/sj/zxfb/202302/t20230228_1919011.html
LiuLISHENG. Guidelines for Prevention and Treatment of Hypertension in China (3rd Edition). (2010). https://www.chinacdc.cn/jkzt/mxfcrjbhsh/jswj/201712/P020171228507420046605.pdf
Song Yongye, L. Y., Zhang & Na Research progress on distribution of sialic acid in food. Chinese food and nutrition: pp. 1–12.
L, H. X. F. Quantitative analysis of sialic acids in Chinese conventional foods by HPLC-FLD. Open. J. Prev. Med., (2014).
Yida, Z. et al. N-Acetylneuraminic Acid Supplementation Prevents High Fat Diet-Induced Insulin Resistance in Rats through Transcriptional and Nontranscriptional Mechanisms. Biomed Research International, 2015. (2015).
Wu, J. et al. Metabolic fate of dietary sialic acid and its influence on gut and oral bacteria. Syst. Microbiol. Biomanufacturing. 2 (1), 41–49 (2022).
Wang, S. et al. Effects of oligosaccharide-sialic acid (OS) compound on maternal-newborn gut microbiome, glucose metabolism and systematic immunity in pregnancy: protocol for a randomised controlled study. BMJ Open.9 (9), e026583 (2019).
Zhang, T., Wu, J. & Zhan, X. Dietary sialic acids: distribution, structure, and functions. Crit. Rev. Food Sci. Nutr. : pp. 1–24 .
Higgins, P. J., Garlick, R. L. & Bunn, H. F. Glycosylated Hemoglobin in Human and Animal Red Cells: role of glucose permeability. Diabetes. 31 (9), 743–748 (1982).
Yamashita, T. et al. Enhanced insulin sensitivity in mice lacking ganglioside GM3. Proc. Natl. Acad. Sci.100 (6), 3445–3449 (2003).
Rao, R. M. et al. Effects of changes in glycan composition on glycoprotein dynamics: example of N-glycans on insulin receptor. Glycobiology. 31 (9), 1121–1133 (2021).
Sydow, O. Sialic acid concentration in erythrocyte membrane subfractions in patients with myotonic dystrophy and healthy controls. Clin. Chim. Acta. 172 (1), 57–63 (1988).
Kwak, B. S. et al. Quantitative analysis of sialic acid on erythrocyte membranes using a photothermal biosensor. Biosens. Bioelectron.35 (1), 484–488 (2012).
Vahalkar, G. S. & Haldankar, V. A. RBC membrane composition in insulin dependent diabetes mellitus in context of oxidative stress. Indian J. Clin. Biochem.23 (3), 223–226 (2008).
Shahvali, S. et al. The correlation between blood oxidative stress and sialic acid content in diabetic patients with nephropathy, hypertension, and hyperlipidemia. Diabetol. Int.11 (1), 19–26 (2020).
Shivananda Nayak, B. et al. Correlation of microalbumin and sialic acid with anthropometric variables in type 2 diabetic patients with and without nephropathy. Vasc Health Risk Manag. 4 (1), 243–247 (2008).
Durocher, J., Payne, R. & Conrad, M. Role of sialic acid in erythrocyte survival. Blood. 45 (1), 11–20 (1975).
Tahara, Y. On the weighted-average relationship between plasma glucose and HbA1c: response to Treviño. Diabetes Care. 29 (2), 466–467 (2006).
Keymel, S. et al. Impaired red blood cell deformability in patients with coronary artery Disease and Diabetes Mellitus. Horm. Metab. Res.43 (11), 760–765 (2011).
Santos, R. D., Shapiro, M. D. & Ballantyne, C. M. Glycated hemoglobin to detect subclinical atherosclerosis in people without Diabetes∗. J. Am. Coll. Cardiol.77 (22), 2792–2795 (2021).
Liang, M. L. et al. N-glycolylneuraminic acid in red meat and Processed meat is a Health Concern: A Review on the Formation, Health risk, and Reduction23 (Comprehensive Reviews in Food Science and Food Safety, 2024). 2.
Wu, J. R. et al. Comparison of prebiotic activity of dietary sialoglycoprotein and < i > N -acetylneuraminic acid: Sialylation is a key factor. Food Bioscience, 56. (2023).
K, P. et al. Predictive value of serum sialic acid in type-2 diabetes mellitus and its complication (nephropathy). J. Clin. Diagn. Research: JCDR. 7 (11), 2435–2437 (2013).
Mazzanti, L. et al. Sialic acid, diabetes, and aging: a study on the erythrocyte membrane. Metabolism-Clinical Experimental. 46 (1), 59–61 (1997).
Hebert, J. R. et al. Systematic errors in middle-aged women’s estimates of Energy Intake: comparing three self-report measures to total energy expenditure from doubly labeled Water. Ann. Epidemiol.12 (8), 577–586 (2002).
Acknowledgements
N/A.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. XYW, JLH, designed the study; WZ, ZCZ organized and analyzed the data; XYW, JLH, ZKX contributed materials/analysis tools; WZ, ZCZ, WQS wrote the paper. HWL, JLH supervised and revised the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
Project 2023Y1540 supported by XMU Training Program of Innovation and Enterpreneurship for Undergraduates.
Ethics approval
This is an observational study. This study was approved by the Ethics Committee of the School of Medicine, Xiamen University according to the recommendations of the World Medical Association Declaration of Helsinki Ethical Principles and the Council of International Medical Scientific Organizations, and the relevant regulations of the National Science Foundation of China. In the course of the implementation of this project, informed consent was strictly made, the use of biological samples of the sample source was informed, the personal information and medical information of the sample source will not be publicly disclosed, and every effort will be made to protect the personal medical information, disease information, life information and basis of the sample source, to the extent permitted by law. The ethical approval number: XDYX202008.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, Z., Zhang, W., Wang, X. et al. Relationship between dietary sialic acid intake and serum HbA1c: a population-based study in Xiamen, China. Sci Rep 14, 23026 (2024). https://doi.org/10.1038/s41598-024-74886-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74886-4