Abstract
This study aimed to assess differences in the enteral microbiome of relatively recent-onset amyotrophic lateral sclerosis (ALS) patients (< 6–15 months since symptom onset) compared to healthy individuals, focusing on short-chain fatty acids (SCFAs) as potential mediators of host metabolism. We included 28 volunteers (16 ALS, 12 controls) with informed consent. No significant effect of ALS on alpha diversity (measuring the variety and abundance of species within a single sample, and indicating the health and complexity of the microbiome) was observed, but ALS patients had higher abundances of Fusobacteria and Acidobacteria. ALS subtypes influenced specific species, with increased Fusobacteria and Tenericutes in spinal ALS compared to bulbar ALS. ALS patients showed increased Enterobacter, Clostridium, Veillonella, Dialister, Turicibacter, and Acidaminococcus species and decreased Prevotella, Lactobacillus, and Butyricimonas. Correlations between species varied between ALS patients and healthy individuals and among ALS subtypes. No significant differences in SCFA concentrations were found, but spinal ALS samples showed a trend towards decreased propionate content. Relationships between SCFAs and phyla colonization differed by disease status. This study suggests distinct enteral microbiome characteristics in ALS patients, though the implications are unclear. Further research is needed to determine if these differences are causative or consequential and to explore their potential as diagnostic or therapeutic targets. The study also underscores the heterogeneity of microbiome constraints in ALS and the need for more research into ALS and SCFA metabolism.
Similar content being viewed by others
Introduction
Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disease characterized by the progressive degeneration of upper and lower motor neurons1. Based on its history, it could be classified into sporadic and familial types2. Despite its historical classification as a motor neuron-centric disorder, the clinical spectrum of ALS encompasses considerable heterogeneity, manifesting in diverse phenotypes and disease trajectories among affected individuals3. This clinical diversity underscores the complex interplay of genetic, environmental, and stochastic factors contributing to ALS pathogenesis, necessitating a nuanced understanding of its underlying mechanisms4.
Recent investigations have expanded the traditional paradigm of ALS pathophysiology to include non-motor manifestations and systemic dysregulation, implicating broader physiological networks beyond the motor system5,6. Notably, emerging evidence highlights the gut microbiome as a potential modulator of ALS heterogeneity, offering insights into the multifaceted interactions between microbial communities and host physiology7,8. The gut-brain axis, a bidirectional communication pathway linking the enteric nervous system with the central nervous system, serves as a conduit for microbial metabolites, immune signals, and neural modulation, exerting profound influences on neurological health9,10.
Studies exploring the gut microbiome in ALS have revealed alterations in microbial composition and function, with notable distinctions observed among patient subgroups exhibiting divergent clinical phenotypes11,12,13. This clinical heterogeneity raises intriguing questions about the differential microbial signatures associated with distinct ALS subtypes and their implications for disease progression. Preclinical models and clinical cohorts have provided compelling evidence linking gut dysbiosis to ALS pathogenesis, highlighting the potential role of the microbiome in shaping clinical outcomes and therapeutic responses14,15. However, elucidating the mechanistic underpinnings of microbiome-host interactions in ALS heterogeneity remains a paramount challenge, necessitating integrated approaches encompassing clinical, preclinical, and translational investigations. Amongst the potential modulators of the host-microbiome relationship, short-chain fatty acids (SCFAs) play a pivotal role as critical metabolites in mediating microbiome-host interactions along the gut-brain axis, thereby exerting profound influences on neurological health16. Produced through the fermentation of dietary fibers by commensal bacteria in the gut, SCFAs, including acetate, propionate, and butyrate, serve as crucial signaling molecules that modulate various aspects of host physiology. These bioactive compounds exhibit diverse effects on immune regulation, energy metabolism, intestinal barrier integrity, and neurotransmitter synthesis, thereby influencing central nervous system function and neuroinflammatory processes17,18. Furthermore, SCFAs contribute to maintaining gut homeostasis by promoting the differentiation of regulatory T cells and enhancing mucosal barrier function, thus mitigating the risk of systemic inflammation and neurodegenerative pathology8,19,20,21Given their multifaceted roles in gut-brain communication, SCFAs represent promising targets for therapeutic interventions aimed at modulating microbiome composition and ameliorating neurological disorders such as ALS. SCFA concentrations have been measured in previous studies, showing mainly no major differences in a pilot study21and differences between ALS patients and controls not reaching statistic in another, more ample, study22.
To help the clarification of host-response relationships in ALS, in the present work, we have evaluated the potential relationship between microbiome-derived constraints, including the three significant SCFAs, in a pilot case-control study of an ALS cohort, scored by a neurologist, in the first six to fifteen months after beginning of symptoms. The results support the potential relationship between previously invoked genera (such as Enterobacter and Acidobacter) but do not reproduce other findings by ALS researchers7,11,22,23, supporting the role of individual differences in host-response relationships and the need for further studies accounting not only for bacterial abundances but also for enteral metabolomic analyses.
Materials and methods
Case and Control Samples Information
Stool samples were collected from ALS patients and healthy controls. Twenty-eight stool samples comprised 12 controls and 16 ALS patients (11 spinal and five bulbar). All employed samples were from cases where symptom onset was relatively recent (< 6 months from symptoms beginning in the case of bulbar patients, < 15 months in the spinal cases for slow progression, and < 12 months in the case of fast progression). All cases and controls had been antibiotic-free for over two months. Clinical data of controls and cases, as well as the sources of stool samples, are presented in Table 1, including Disease Duration (DoD), defined as the entire duration of the disease, from debut to the end. We only included cases that after follow-up confirmed the ALS diagnosis, including those with El Escorial Criteria possible or missing in the moment of sample collection. Cases with other neurological pathologies were excluded. Additionally, exclusion criteria ruled out cases with gastrointestinal diseases or those treated with drugs (such as antibiotics) that could alter nutritional balance and affect intestinal microbiota. Of note, patients with bulbar ALS exhibited disphagia under neurologist examination. The twelve healthy controls, who could be spouses or close relatives of diagnosed cases, were recruited to minimize the effects of different lifestyles and diets. Participants were from various cities or towns within the same territorial region (Barcelona urban area) and had similar living conditions and diets under dietary examination by a licensed nutritionist. The patients did not exhibit familial history of ALS and known-pathogenic mutations in the SOD1 and C9orf72 expansions were excluded by sequencing. The study followed the guidelines of Spanish legislation on this matter and the approval of the local ethics committee of Bellvitge University Hospital, with the code PR100/24.
Sample obtention and storage
The participants were instructed to froze the samples within 15 min after defecation and to store it for up to 3 days in the home freezer (-20 °C) before the neurologist visit. The sample was transported in a thermal bag to the laboratory, where it was frozen at -80 °C until DNA extraction, which was performed within three months, according guidelines by Choo et al.24.
DNA extraction and 16 S rRNA gene sequencing
Following the manufacturer’s protocol, it was performed using the QIAamp DNA Stool Mini Kit (Qiagen Cat.#51540). Stool samples ranging from 180 to 220 mg were utilized to attain the desired DNA concentration of 20–200 ng/µL.
The DNA concentration was measured on the Nanodrop at 260 nm (ND-1000 UV/Vis Spectrophotometer, Nanodrop Technologies). A metagenomic study analyzed the V3 and V4 regions of the prokaryotic 16 S ribosomal RNA gene (16 S rRNA gene) in DNA extracted from frozen human stools using the QIAamp DNA mini stool kit following manufacturer instructions. V3 and V4 regions were amplified using a limited cycle PCR, and Illumina sequencing adapters and dual index barcodes were added to the amplicon target. The 16 S rRNA gene V3 and V4 region gene-specific sequences were selected from Klindworth et al.25 as the most promising bacterial primer pair. Illumina adapter overhang nucleotide sequences were added to the gene-specific sequences. Using paired 250 bp reads and MiSeq v2 reagents, the ends of each read were overlapped to generate high-quality, full-length reads of the V3 and V4 region in a single 40 h run. The MiSeq run output is approximately 15 million reads, and assuming 96 indexed samples can generate > 100,000 reads per sample, it is commonly recognized as sufficient for metagenomic surveys. The Metagenomics Workflow performed a taxonomic classification using the Greengenes database. Next-generation sequencing with an Illumina MiSeq System was outsourced at the Servei de Genòmica i Bioinformàtica of Universitat Autònoma de Barcelona (https://www.uab.cat/ca/servei-genomica). We then obtained clusters of sequences that have identity higher than 97%, termed operational taxonomic units (OTUs)26. OTU is a term used in microbiome research to categorize bacteria based on their genetic sequence similarity, allowing to identify and quantify the different types of microorganisms present in a sample without needing to name each species individually. The abundance of these OTUs was quantified using raw counts and presented in supplemental datasets in.
https://figshare.com/articles/dataset/Supplemental_dataset/26292994.
Short-chain fatty acid analysis by high-performance liquid chromatography (HPLC)
SCFA concentrations were analyzed in fecal samples from ALS patients and healthy controls using HPLC following the protocol27. Twelve SCFAs were examined, and for its calibration, we employed a 200mmol/L concentration in a 50% methanol and 50% H2O solution. Derivatization reagents, including phosphoric acid, pyridine, potassium hydroxide, N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide, and 2-nitrophenylhydrazine, were prepared as indicated. Liquid chromatography’s mobile phase comprised acetonitrile, methanol, and MilliQ water in a 0:16:54 ratio (1 L), pH adjusted to 4.5 with 0.1 M trifluoroacetic acid. The method was optimized via derivatization to ensure standards appeared at specific retention times. Eleven glass tubes, one per standard, received 150µL of each standard and reagents, incubated at 60 °C for 20 min, then cooled. Tubes were centrifuged, and the upper ether phase was transferred to a new tube, mixed with water, centrifuged, and moved to an Eppendorf tube for evaporation. Methanol was added, mixed, and transferred for HPLC analysis, employing an Agilent 1100 LC chromatograph (Santa Clara, CA, USA) instrument with a C18 column (YMC-Pack FA 250 × 6 mm ID column YMC, Kyoto, Japan). The column temperature was set at 50 °C with a flow rate of 1.1mL/min. UV detection was employed, with the detector set at a wavelength of 400 nm. Calibration curves were made from serial standard dilutions analysed by HPLC for peak areas. R2 of the linear relationship between values was ~ 0.99. Faecal SCFAs in ALS and control samples were analysed post-dilution of the sample (0.2–0.5 g) in 5mL 70% ethanol and centrifugation at 2,500 rpm for 10 min. 150µL of diluted faecal sample in ethanol was prepared per sample for derivatization and liquid chromatography analysis. MicroM concentrations were calculated using calibration curves. We focused mainly on acetic, propionic, and butyric acids, constituting 95% of all SCFAs in a 60:20:20 ratio, respectively.
Data and statistical analysis
OTUs (raw counts or percentages over total), as well as other variables (age, DoD, SCFA concentration), were analysed employing the GraphPad Prism 10 for Windows (v10.2.3(403)), the IBM SPSS suite (v27) or the MicrobiomeAnalyst V2 platform28. Briefly, in this later case, OTU abundances (in raw counts) were uploaded onto the platform, employing the GreengenesID as OTU annotation. We used total sum scaling in case of techniques requiring data scaling (e.g., correlational analyses). For phylum abundances, we tested if they followed a normal distribution employing the Kolmogorov-Smirnov test, which was the case for the most abundant phylae (> 10% abundance).
Results
Regarding the microbiome analyses, in the case of the genus, we detected a total of 628 different OTUs, with 492 showing more than two counts. Samples had an average count of 259,668 (72640 to 1162697 counts). We employed both a low count filter (4 counts in 20% samples) for excluding less abundant OTUs -resulting in 206 OTUs dismissed-and a low variance filter (10% of interquartile range) to exclude those OTUs close to being constant throughout ALS vs. control (Ctl) (or ALS subtypes) conditions and were unlikely to be associated with the conditions under study -resulting in 29 OTUs with low variance-.
Despite the sparse partial least squares discriminant analysis (Fig. 1A), suggesting the clustering of enteral microbiomes according to ALS diagnosis, the metagenome analyses did not reveal a significant effect of ALS status (nor ALS subtypes) on any measured index of alpha-diversity (Fig. 1B). At the species level, amongst 1334 species detected, ALS in the present study was associated with an increased abundance of several Enterobacter members and specific Clostridium, Veillonella, Dialister, Turicibacter, and Acidaminococcus species (Fig. 1C), with other species not reaching statistical significance (supplemental datasets are provided for further analyses). In addition, ALS patients exhibited a significantly decreased abundance of Prevotella, Lactobacillus, and Butyricimonas (Fig. 1C). In addition, when evaluating the phylum distribution, we found that ALS patients had significantly higher Fusobacteria and Acidobacteria abundances, though they were quantitatively minor (Fig. 1D). Indeed, ALS subtypes had differential abundances of specific species, such as increased Fusobacteria and Tenericutes abundances in spinal ALS compared to bulbar ALS (Fig. 1D). Indeed, reinforcing the heterogeneity of microbiome constraints in ALS, correlations between phyla were different between ALS patients and healthy individuals (Fig. 1E). For example, in controls, ALS was associated with a loss in the age-Firmicutes correlation. In addition, the abundance of Synergistetes was related to many different species in ALS patients but not in controls. Furthermore, the duration of bulbar ALS correlates significantly with the abundance of the Deferribacteres phylum. Of note, correlations between different species also differed between different ALS subtypes, with spinal ALS showing fewer inter-phylum relationships than bulbar ALS (Fig. 1F). Reinforcing the relevance of microbiome, several phylae correlated significantly with ALS-FR (Supplemental Fig. 1).
At the diagnostic stage, ALS is associated with changes in the enteral microbiome. (A) Sparse partial least squares-discriminant analyses showing differences in genus abundance between patients with ALS and healthy individuals. (B) Alpha diversity indices of the participants’ microbiome considering species abundance. (C) The abundance of the selected species is significantly affected by ALS status. (D) Phylum abundance in the studied groups showed a significantly increased Firmicutes and decreased abundance of Bacteroidetes in patients with ALS, without changes between spinal ALS and bulbar ALS subtypes. Chord diagram showing relationships (ribbons expressing significant correlations) between phylum abundances, affected by both ALS status (E) and ALS subtypes (F). In (B), Shannon Index increases as both the richness and the evenness of the community increase, providing a comprehensive measure of diversity. Also in (B) Simpson also increases with diversity, ranging from 0 to 1, where a higher value indicates greater diversity. In (C), all indicated species showed a significant difference (FDR corrected p < 0.05 after EdgeR test) between control (Ctl) and ALS patients. In (D), asterisks indicate p < 0.05 after Student’s t-test. For E and F, Spearman correlations between shown variables were calculated, and those showing significance (p < 0.05) were plotted as ribbon-connecting segments.
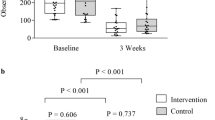
Based on these previous findings, we evaluated their concentrations in the same samples since some of the differential bacteria produce a significant amount of SCFA. We did not find significant differences in any SCFA concentration in fecal matter related to ALS status or subtypes. However, samples from the spinal ALS subtype had a tendency (p < 0.06) for decreased propionate content in comparison to healthy counterparts (Fig. 2A). In line with ALS interacting with SCFA metabolism, relationships between specific SCFA and phyla colonization show different profiles depending on disease status (Fig. 2B). Thus, we found that butyrate levels differed from the other SCFA measured. For instance, in bulbar ALS (but not in spinal ALS or control individuals), the abundance of Verrucomicrobia correlated significantly with acetic and propionic acid levels but not with butyric acid concentration. Similarly, butyrate was correlated with Chloroflexi amount in both ALS types but not in healthy individuals. When evaluating the Genus level, we found strong correlations between Eggerthella, Bifidobacterium, and Sphingomonas abundances and SCFA concentrations (Fig. 2C), with negative relationships with Oribacterium and Blautia abundances in ALS (Fig. 2C).
ALS affects relationships between SCFA content and microbiome abundance. (A) SCFA percentages are not mainly affected by ALS diagnosis and subtype. HPLC measured SCFA in fecal samples, plotting relative levels in %. (B) Heatmap showing the association between SCFA concentration and microbiome abundance at the phylum level. (C) SCFA correlates with specific Genii, with some correlations showing statistical significance in ALS patients. In (A), values shown are uncorrected Fisher’s least significant differences after ANOVA. For (B), the color of the heatmap (scale shown at the right) is related to Spearman correlation coefficients with * and ** indicating p < 0.05 and p < 0.01, respectively. (C) shows the correlation coefficient (Spearman rank) between selected genus abundances with indicated SCFA, with *,**, and *** indicating p < 0.05, p < 0.01, and p < 0.001, respectively.
Discussion
Our data provides a detailed analysis of a pilot study of ALS patients’ microbiome composition and SCFA levels within six to fifteen months of symptom onset. No significant impact of ALS or its subtypes on general (i.e., alpha) diversity was observed among the analyzed population. Alpha diversity is a measure used microbiome research to assess the variety of species within a specific sample, considering both the number of different species (richness) and their relative abundance (evenness). Higher alpha diversity typically indicates a more resilient and stable ecosystem29. However, distinct alterations at several taxonomic levels were noted, such as elevated Fusobacteria and Acidobacteria abundances in ALS. Dysbiosis can be defined as an imbalance or alteration in the composition and function of the microbiota, often associated with various diseases and influenced by factors such as diet, stress, and antibiotics29,30. Given the absence of significant differences in diversity and SCFA concentrations in our study, we cannot conclusively state that the ALS patients analyzed exhibited bona fide dysbiosis at the time of analysis. However, the observed differences in specific microbial species and some changes in the SCFA-OTUs relationship suggest potential microbiome variations in ALS, which might contribute to the clinical variability observed in these patients.
Interestingly, despite no significant differences in SCFA levels based on ALS status, we found a trend towards reduced propionate content in spinal ALS, reinforcing the need for further studies involving microbial metabolites at the early stages of this disease. The fact that we found this difference in spinal vs. bulbar cases might be derived by dysphagia, as the bulbar ALS cases exhibited some degree of this characteristic. Of note, this could impinge severe oral microbiome changes31. Indeed, dysphagia has been related to changes in fecal incontence, and therefore microbiome in stool32. Nonetheless, our results mainly agree with previous reports 22 23, mainly showing that fecal SCFA concentrations did not significantly differ between ALS patients and controls, or between patients with different clinical characteristics. Noteworthy, and reinforcing previous results demonstrating that controls and ALS patients were characterized by different correlation between SCFA and specific microbiota, with the controls including many genera negatively correlated with propionic acid, and the ALS patients including some genera positively correlated with acetic acid, involving, among other Lachnospiraceae, Veilonella, and Anaerostipes, among other22 Further analysis revealed intricate relationships between specific SCFA and microbial profiles, highlighting potential microbial markers of interest in ALS pathogenesis. These findings, advancing our understanding of microbiota-mediated mechanisms in neurodegenerative disorders, demonstrate that no single microbial profile is associated generically with ALS. Therefore, host-specific traits could be relevant in defining the exact weight of the enteral microbiome as a disease-modifying factor in ALS. These data contrast those found in a recent report33 where microbiome constraints in a longitudinal study contribute to explaining lipid metabolic derangements in ALS patients, which aligns with previous research34. By employing various bioinformatic analyses, these recent analyses revealed that acylcarnitine and fatty acid metabolism could be used to distinguish ALS patients from healthy individuals33. Our data contrast with the existence of significant changes in most abundant phyla and are similar to those described by Kim and coworkers35, where bulbar and spinal ALS clinical phenotypes differ not only in oral microbiota but also in enteral microbiota, with a potential role of Fusobacteria abundance. In our samples, Fusobacteria only contributed to less than 0.5% of the total microbiome, in contrast to these data, representing more than 5% of total OTUs. Nonetheless, similar to this paper, ALS presentation strongly affected ALS enteral microbiomes. Other relevant factors, such as differences in DoD and ALSFR could explain as well the differences between our data and other published reports. Of note, individual factors such as body-to-mass index, ALSFR, and even forced vital capacity can account as relevant in microbiome determination15,36. Globaly, some studies suggest gut microbiota composition is linked to ALS progression through dysbiosis and immune regulation12,13,36,37, while other studies find the evidence inconclusive or minimal13. In an interventional study, it was discovered that microbiome changes in a 6 month period in ALS patients36, reinforcing the highly dynamic nature of microbiome in this situation.
Previous results suggest that there might be differences in the microbiota profile (alpha diversity) in ALS patients and the effects of the progression of the disease and the bacteriotherapy on the bacterial and yeast populations15,38. Indeed, we should recall the profound effect of bulbar phenotype in nutritional characteristics, though in our case at the analyzed stage no significant differences in food intake were noted. As a relevant question for future research one might pose if the weight loss that many patients experience could have an association with the microbiome or whether the influence of e.g. SCFAs on progression, which has already been shown by relatively robust data for longer fatty acids39, could have an association with the microbiome. Understanding these interactions may provide deeper insights into the clinical variability and progression of ALS, potentially leading to more effective dietary and microbiome-targeted interventions.
In our study, several recent ALS-associated OTUs, such as Acidaminococcus, Dialister, and Veillonella, could have a relevant role based on SCFA and nitrate metabolism40,41,42. Indeed, they have been previously invoked in ALS43. In our patients, Butyricimonas and Lactobacillus abundances were decreased in ALS samples, in line with previous data showing an association between Butyrcimonas abundances and neurodegeneration in independent studies44. We found significant relationships between the duration of disease in bulbar ALS, which might be viewed as a proxy for disease progression, and the abundance of the Deferribacteres phylum. These bacteria have been previously related to disease progression in AD transgenic models45. In our samples, we have also found decreased Prevotella abundance in ALS, in line with very recent results46, where patients with a more advanced stage of disease exhibit diminished Prevotella levels. Also, in line with previously reported data, our results resemble those found in36, where unclassified Acidaminococcaceae and specific Enterobacteriaceae were associated with a higher risk of ALS. Acidaminococcaceaeabundance is diminished by nutritional constraints in Parkinson’s disease (PD) patients, showing a decrease in the Mediterranean diet47. These members of the Firmicutes phylum are known to be a normal commensal of the human gut, representing ∼1% of the fecal bacterial population, and they have as a unique characteristic their ability to thrive on glutamate42. Glutamate is a relevant metabolite in the synthesis and metabolic recycling of other amino acids and, with the urea cycle in the gut, allows its use in epithelial restitution. Therefore, the overgrowth of these species could be related to excessive glutamate local concentrations (maybe related to riluzole intake) and can contribute to regional changes in intestinal permeability48. Of note, recent data suggest that, in mice, differential glutamate production by intestinal microbiota corresponds to increased appetite and that colonic glutamate administration can directly increase food intake49. Thus, hypothetically, decreased glutamate signalling could interfere with food intake, potentially contributing to heterogeneity in weight loss and metabolism found in ALS patients2.
Indeed, Enterobacteriaceae members associated with ALS in our study have been previously involved in the mapranosis process, e.g., microbiota-associated proteopathy and neuroinflammation, by contributing to amyloid-like proteins50. For instance, Enterobacteriaceae are pretty standard in the human gut and can produce functional amyloid proteins called curli50 as a result of their secretion of the amyloid CsgA, which then aggregates extracellularly to form biofilms, mediates adherence to epithelial cells, and plays a role in bacteriophage defence. This process results in the formation of curli fibers, whose exposure not only modifies host inflammatory responses inside the intestinal tract and periphery but also promotes the formation and aggregation of the amyloid protein α-synuclein, contributing to motor impairment in the context of preclinical models of PD51. Turicibacter members, on the other hand, interfere in preclinical models with local polyamine metabolism52. Two unique biological response-modifier glucans beneficially regulate gut microbiota and fecal metabolome in a non-alcoholic steatohepatitis animal model, with potential applications in human health and disease52. Indeed, the increase of Turicibacter has been invoked as beneficial in other preclinical settings related to PD53. Members of the Veillonella genus have also been associated with inflammatory changes involving microglial and Th1 cell infiltration of the central nervous system in a preclinical PD context54. Recent data show that the immunological profile in ALS is associated with the severity and advancement of the disease, with a shift towards a Th1/Th17 cell-mediated proinflammatory immune response55. Given that those changes are of peripheral origin, it may be suggested that microbiome changes such as those reported here could contribute, in a patient-specific manner, to inflammatory changes modulating disease severity56. Therefore, in line with findings from these previous analyses, we propose that the study of the potential role of microbiota and ALS should encompass the analyses of specific metabolome contents at the microbiome and host level, evidencing the non-negligible challenge for microbiome-focused interventions (either probiotics, prebiotics, and postbiotics) with immunomodulatory and neuromodulatory view in ALS management.
To sum up, all these data disclose a high heterogeneity of the association between ALS and microbiome changes, pointing to environmental specificities, host-microbiome particularities, as some technical issues, such as study design, statistical power (one of our main limitations in the present work), handling processing of samples, and statistical methods and interpretation of results as challenges for adequate and robust replicability of the findings. Despite the present limitations, we should remark that our data support the relevant role of microbiome-conditioned metabolomic and lipidomic changes in neurodegeneration. These approaches provide insights into the metabolic changes occurring in the gut-brain axis and their impact on neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and ALS. By studying microbial-derived metabolites, such as SCFA, lipid inflammatory mediators, and aromatic amino acids, we could suggest mechanisms of action and their role in maintaining intestinal homeostasis and regulating neuro-immunoendocrine function. Additionally, metabolomics and lipidomics allow for identifying disease pathomechanisms and the potential for therapeutic modulation of the microbiome composition through dietary and lifestyle interventions. Hopefully, these approaches will offer novel and readily available therapeutic options to prevent or delay the onset and progression of these neurodegenerative diseases.
CONCLUSIONS
Our study provides novel insights into the enteral microbiome and SCFA profiles in patients with recent-onset ALS. We found that patients with ALS had distinct microbiome characteristics compared to healthy individuals, with significantly higher abundances of Fusobacteria and Acidobacteria. Additionally, ALS subtypes had differential abundances of specific species, and correlations between phyla were different between ALS patients and healthy individuals and between different ALS subtypes. While we did not find significant differences in SCFA concentrations related to ALS status or subtypes, relationships between specific SCFA and phyla colonization showed different profiles depending on disease status. These findings suggest that the gut microbiome may play a role in the pathogenesis of ALS. However, further research is needed to determine whether these differences are a cause or a consequence of the disease. Our study also highlights the heterogeneity of microbiome constraints in ALS, emphasizing the need for personalized approaches in future studies. Overall, our results contribute to a growing body of evidence indicating that the gut microbiome may be a promising target for developing novel diagnostic and therapeutic strategies for ALS.
Data availability
The datasets generated and/or analysed during the current study are available in the Figshare repository (https://figshare.com/articles/dataset/Supplemental_dataset/26292994).
Abbreviations
- AD:
-
Alzheimer’s Disease
- ALS:
-
Amyotrophic Lateral Sclerosis
- HPLC:
-
High-Performance Liquid Chromatography
- OTU:
-
Operational Taxonomic Unit
- PD:
-
Parkinson’s Disease
- SCFA:
-
Short-Chain Fatty Acid
References
Talbott, E. O., Malek, A. M. & Lacomis, D. The epidemiology of amyotrophic lateral sclerosis. Handb. Clin. Neurol. 138, 225–238 (2016).
Tzeplaeff, L., Jürs, A. V., Wohnrade, C. & Demleitner, A. F. Unraveling the Heterogeneity of ALS-A Call to Redefine Patient Stratification for Better Outcomes in Clinical Trials. Cells 13, (2024).
Marriott, H. et al. Unsupervised machine learning identifies distinct ALS molecular subtypes in post-mortem motor cortex and blood expression data. Acta Neuropathol. Commun. 11, 208 (2023).
Dey, B., Kumar, A. & Patel, A. B. Pathomechanistic networks of motor system injury in amyotrophic lateral sclerosis. Curr. Neuropharmacol. https://doi.org/10.2174/1570159X21666230824091601 (2023).
Rusina, R., Vandenberghe, R. & Bruffaerts, R. Cognitive and behavioral manifestations in ALS: beyond motor system involvement. Diagnostics (Basel) 11, 624–35(2021).
van Es, M. A., Goedee, H. S., Westeneng, H. J., Nijboer, T. C. W. & van den Berg, L. H. Is it accurate to classify ALS as a neuromuscular disorder? Expert Rev. Neurother. 20, 895–906 (2020).
McCombe, P. A. et al. Gut microbiota in ALS: possible role in pathogenesis? Expert Rev. Neurother. 19, 785–805 (2019).
Xu, F. Z. et al. The interplay between host genetics and the gut microbiome reveals common and distinct microbiome features for complex human diseases. Microbiome. 8, 145 (2020).
Carabotti, M., Scirocco, A., Maselli, M. A. & Severi, C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28, 203–209 (2015).
Martin, C. R., Osadchiy, V., Kalani, A. & Mayer, E. A. The brain-gut-Microbiome Axis. Cell. Mol. Gastroenterol. Hepatol. 6, 133–148 (2018).
Boddy, S. L. et al. The gut microbiome: a key player in the complexity of amyotrophic lateral sclerosis (ALS). BMC Med. 19, 13 (2021).
Wright, M. L. et al. Potential role of the gut microbiome in ALS: a systematic review. Biol. Res. Nurs. 20, 513–521 (2018).
Brenner, D. et al. The fecal microbiome of ALS patients. Neurobiol. Aging. 61, 132–137 (2018).
Goyal, N. A. et al. Addressing heterogeneity in amyotrophic lateral sclerosis CLINICAL TRIALS. Muscle Nerve. 62, 156–166 (2020).
Mazzini, L. et al. Potential role of gut microbiota in ALS pathogenesis and possible novel therapeutic strategies. J. Clin. Gastroenterol. 52 (Suppl 1), S68–S70 (2018). Proceedings from the 9th Probiotics, Prebiotics and New Foods, Nutraceuticals and Botanicals for Nutrition&Human and Microbiota Health Meeting, held in Rome, Italy from September 10 to 12, 2017
Silva, Y. P., Bernardi, A. & Frozza, R. L. The role of short-chain fatty acids from gut microbiota in Gut-Brain communication. Front. Endocrinol. (Lausanne). 11, 25 (2020).
Caputi, V., Popov, J., Giron, M. C. & Mahony, O. A. Gut microbiota as a mediator of host Neuro-Immune interactions: implications in Neuroinflammatory disorders. Mod. Trends Psychiatry. 32, 40–57 (2021).
You, X. Y. et al. Intestinal mucosal barrier is regulated by intestinal Tract Neuro-Immune Interplay. Front. Pharmacol. 12, 659716 (2021).
Josefowicz, S. Z. et al. Extrathymically generated regulatory T cells control mucosal TH2 inflammation. Nature. 482, 395–399 (2012).
Cox, L. M. et al. The microbiota restrains neurodegenerative microglia in a model of amyotrophic lateral sclerosis. Microbiome. 10, 47 (2022).
van Wijk, F. & Cheroutre, H. Mucosal T cells in gut homeostasis and inflammation. Expert Rev. Clin. Immunol. 6, 559–566 (2010).
Niccolai, E. et al. The Gut Microbiota-Immunity Axis in ALS: A Role in Deciphering Disease Heterogeneity? Biomedicines 9, (2021).
Rowin, J., Xia, Y., Jung, B. & Sun, J. Gut inflammation and dysbiosis in human motor neuron disease. Physiol. Rep. 5, e13443–e13449 (2017).
Choo, J. M., Leong, L. E. X. & Rogers, G. B. Sample storage conditions significantly influence faecal microbiome profiles. Sci. Rep. 5, 16350 (2015).
Klindworth, A. et al. Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res. 41, e1 (2013).
Kozich, J. J., Westcott, S. L., Baxter, N. T., Highlander, S. K. & Schloss, P. D. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl. Environ. Microbiol. 79, 5112–5120 (2013).
Torii, T. et al. Measurement of short-chain fatty acids in human faeces using high-performance liquid chromatography: specimen stability. Ann. Clin. Biochem. 47, 447–452 (2010).
Chong, J., Liu, P., Zhou, G. & Xia, J. Using MicrobiomeAnalyst for comprehensive statistical, functional, and meta-analysis of microbiome data. Nat. Protoc. 15, 799–821 (2020).
Lee, J. Y., Tsolis, R. M. & Bäumler, A. J. The microbiome and gut homeostasis. Science. 377, eabp9960 (2022).
Kriss, M., Hazleton, K. Z., Nusbacher, N. M., Martin, C. G. & Lozupone, C. A. Low diversity gut microbiota dysbiosis: drivers, functional implications and recovery. Curr. Opin. Microbiol. 44, 34–40 (2018).
Duarte, J. C. M. et al. Biochemical and microbiological aspects of the oral cavity of children and young people with neurological impairment and Oropharyngeal Dysphagia. Life (Basel) 13, 1342–135 (2023).
Shimizu, A. et al. Association of poor oral health status and faecal incontinence in patients with dysphagia: a cross-sectional analysis from the Sarcopenic Dysphagia Database. J. Oral Rehabil. 50, 286–292 (2023).
Guo, K. et al. Gut microbiome correlates with plasma lipids in amyotrophic lateral sclerosis. Brain. 147, 665–679 (2024).
Sol, J. et al. Lipidomic traits of plasma and cerebrospinal fluid in amyotrophic lateral sclerosis correlate with disease progression. Brain Commun. 3, fcab143 (2021).
Kim, H. S. et al. Gut- and oral-dysbiosis differentially impact spinal- and bulbar-onset ALS, predicting ALS severity and potentially determining the location of disease onset. BMC Neurol. 22, 62 (2022).
Di Gioia, D. et al. A prospective longitudinal study on the microbiota composition in amyotrophic lateral sclerosis. BMC Med. 18, 153 (2020).
Sun, J., Huang, T., Debelius, J. W. & Fang, F. Gut microbiome and amyotrophic lateral sclerosis: a systematic review of current evidence. J. Intern. Med. 290, 758–788 (2021).
Fang, X. et al. Evaluation of the Microbial Diversity in Amyotrophic lateral sclerosis using high-throughput sequencing. Front. Microbiol. 7, 1479 (2016).
Bjornevik, K. et al. Association of polyunsaturated fatty acids and clinical progression in patients with ALS: post hoc analysis of the EMPOWER trial. Neurology. 101, e690–e698 (2023).
Jumas-Bilak, E. et al. Acidaminococcus intestini sp. nov., isolated from human clinical samples. Int. J. Syst. Evol. Microbiol. 57, 2314–2319 (2007).
Wicaksono, D. P., Washio, J., Abiko, Y., Domon, H. & Takahashi, N. Nitrite Production from Nitrate and its link with Lactate metabolism in oral Veillonella spp. Appl. Environ. Microbiol. 86 (20), e01255–20 (2020).
Rogosa, M. Acidaminococcus gen. n., Acidaminococcus fermentans sp. n., anaerobic gram-negative diplococci using amino acids as the sole energy source for growth. J. Bacteriol. 98, 756–766 (1969).
Zhang, L., Zhuang, Z., Zhang, G., Huang, T. & Fan, D. Assessment of bidirectional relationships between 98 genera of the human gut microbiota and amyotrophic lateral sclerosis: a 2-sample mendelian randomization study. BMC Neurol. 22, 8 (2022).
Fan, K. C. et al. Altered gut microbiota in older adults with mild cognitive impairment: a case-control study. Front. Aging Neurosci. 15, 1162057 (2023).
Chen, C. et al. Gut dysbiosis contributes to amyloid pathology, associated with C/EBPβ/AEP signaling activation in Alzheimer’s disease mouse model. Sci. Adv. 6, eaba0466 (2020).
Hertzberg, V. S. et al. Gut microbiome differences between amyotrophic lateral sclerosis patients and spouse controls. Amyotroph. Lateral Scler. Frontotemporal Degener. 23, 91–99 (2022).
Solch, R. J. et al. Mediterranean diet adherence, gut microbiota, and Alzheimer’s or Parkinson’s disease risk: a systematic review. J. Neurol. Sci. 434, 120166 (2022).
Abe, M. et al. Results of the 2018 Japan Society for blood purification in critical care survey: current status and outcomes. Ren. Replace. Ther. 8, 58 (2022).
Tan, S. et al. Interaction between the gut microbiota and colonic enteroendocrine cells regulates host metabolism. Nat. Metab. 6, 1076–1091 (2024).
Friedland, R. P. & Chapman, M. R. The role of microbial amyloid in neurodegeneration. PLoS Pathog. 13, e1006654 (2017).
Sampson, T. R. et al. A gut bacterial amyloid promotes α-synuclein aggregation and motor impairment in mice. eLife 9, (2020).
Preethy, S. et al. Two unique biological response-modifier glucans beneficially regulating gut microbiota and faecal metabolome in a non-alcoholic steatohepatitis animal model, with potential applications in human health and disease. BMJ Open. Gastroenterol. 9, e000985–000995 (2022).
Radisavljevic, N. et al. Microbiota-mediated effects of Parkinson’s disease medications on parkinsonian non-motor symptoms in male transgenic mice. mSphere. 9, e0037923 (2024).
Bai, X. B. et al. Oral pathogens exacerbate Parkinson’s disease by promoting Th1 cell infiltration in mice. Microbiome. 11, 254 (2023).
Jin, M., Günther, R., Akgün, K., Hermann, A. & Ziemssen, T. Peripheral proinflammatory Th1/Th17 immune cell shift is linked to disease severity in amyotrophic lateral sclerosis. Sci. Rep. 10, 5941 (2020).
Beers, D. R. & Appel, S. H. Immune dysregulation in amyotrophic lateral sclerosis: mechanisms and emerging therapies. Lancet Neurol. 18, 211–220 (2019).
Acknowledgements
We acknowledge patient’s and controls for their contribution.
Funding
This work is supported by grants from Instituto de Salud Carlos III (PI20/000155, and PI23/00176), Generalitat de Catalunya (2021 SGR 00990), from Miquel Valls Foundation (Jack Van den Hoek donation), FUNDELA, and RedELA funds.
Author information
Authors and Affiliations
Contributions
LF, JCES and VA analyzed the samples both for SCFA and microbiome. MP and RD obtained the clinical samples and staged the patients. RP, JB and VA drafted the general project and interpreted the patient data. MPO and VA prepared the manuscript, got funds for the analyses and performed statistical tests. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study followed the guidelines of Spanish legislation and the approval of the local ethics committee of Bellvitge University Hospital. All patients and controls gave informed consent.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fontdevila, L., Povedano, M., Domínguez, R. et al. Examining the complex Interplay between gut microbiota abundance and short-chain fatty acid production in amyotrophic lateral sclerosis patients shortly after onset of disease. Sci Rep 14, 23497 (2024). https://doi.org/10.1038/s41598-024-75083-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-75083-z
Keywords
This article is cited by
-
Butyric acid and valeric acid attenuate stress-induced ferroptosis and depressive-like behaviors by suppressing hippocampal neuroinflammation
Journal of Translational Medicine (2025)