Abstract
This study evaluates the efficacy of photodynamic therapy (PDT) in treating central serous chorioretinopathy (CSC) based on the number of engorged vortex vein draining macula visualized on ultra-widefield (UWF) indocyanine green angiography (ICGA). Thirty-six eyes of 36 patients with treatment-naïve CSC were included. Macula-draining vortex veins were assessed in each quadrant using UWF ICGA. The resolution of subretinal fluid (SRF), pigment epithelial detachment (PED), ellipsoid zone (EZ) disintegrity, and retinal pigment epithelium (RPE) irregularity were evaluated at 3 months after PDT. Visual and anatomical improvements were monitored for 12 months. Logistic regression analysis was performed to identify factors associated with poor visual outcomes. A higher number of macula-draining vortex vein was associated to persistent SRF (p = 0.004), PED (p = 0.001), EZ disintegrity (p = 0.011), and RPE irregularity (p = 0.001). Macula-draining vortex veins were also correlated with poor EZ restoration and limited best corrected visual acuity (BCVA) improvements. In multivariate analysis, the number of macula-draining vortex vein (B = 0.197, p = 0.047) was a risk factor for worse BCVA at 12 months. Increased macula-draining vortex vein was related with unfavorable anatomical and poor visual outcomes after PDT in CSC patients.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is a retinal disorder characterized by serous detachment of the neurosensory retina at the posterior pole and leading to visual disturbances1,2. The exact pathophysiology of CSC remains incompletely understood, but choroidal abnormalities, particularly choroidal thickening and vascular hyperpermeability, are thought to play a crucial role in its development1,3,4,5,6,7. Among these choroidal changes, vortex vein engorgement has recently emerged as a notable factor. Vortex vein engorgement, which involves the dilation of the choroidal veins, can increase hydrostatic pressure within the choroid, thereby contributing to the disruption of the outer blood-retinal barrier and subsequent fluid leakage into the subretinal space8,9,10.
Photodynamic therapy (PDT) has been widely used to treat CSC by targeting the abnormal choroidal vasculature to reduce leakage and restore retinal anatomy11,12. The efficacy of PDT can vary significantly among patients, and this variability might be influenced by pre-existing factors such as pigment epithelium detachment (PED), subretinal fluid (SRF) persistence, neovascularization, retinal pigment epithelium (RPE) atrophy, and ellipsoid zone (EZ) disruption13,14 on optical coherence tomography (OCT). Recent studies have suggested that the number of macula-draining vortex veins, as visualized on ultra-widefield (UWF) indocyanine green angiography (ICGA), indicate the severity of disease and could impact the therapeutic outcomes of PDT in patients with CSC9.
In this study, we aim to investigate the efficacy of PDT in treating CSC, focusing on the influence of macula-draining vortex vein observed on UWF ICGA. By assessing anatomical and visual outcomes following PDT, we evaluated whether the number of vortex veins draining macula correlates with treatment success. We expect this could provide insights into the visual prognoses for CSC patients after PDT.
Results
Baseline characteristics
A total of 36 patients were included in this study, The mean age of the patients was 50.56 ± 8.55 years, with 28 males and 8 females. Macula-draining vortex veins were identified on one quadrant in 12 patients, two quadrants in 13 patients, three quadrants in 7 patients, and all four quadrants in 4 patients (Table 1). Only one patient of one quadrant group was pseudophakic eye.
Demographic and ophthalmic parameters according to the macula-draining vortex veins were presented in Table 2. As the number of draining veins increased, there was a tendency for longer disease duration (p = 0.114), and more frequent shallow and irregular PED (p = 0.073) and EZ disruption (p = 0.077). There is a trend in gender distribution across groups, with the proportion of males increasing as the number of macula-draining quadrants increased (58.3% in 1 quadrant group, 84.6% in 2 quadrants group, 85.7% in 3 quadrants group, and 100% in 4 quadrants group; p = 0.336).
Comparison of treatment outcomes depending on vortex vein engorgement
The proportion of SRF resolution showed a difference between the groups (p = 0.004). All patients in the 1 or 2 quadrant groups achieved SRF absorption after 3 months, while 28.6% of the 3 quadrants group and 50% of the 4 quadrants group had persistent SRF. The proportion of persistent PED (p = 0.001), EZ disruption (p = 0.011), and RPE irregularity increased according to the number of vortex vein engorgement (Table 3).
For statistical comparison, the 3 and 4 quadrant groups were combined into one group. The CFT and SFCT significantly decreased in all three groups (1 quadrant, 2 quadrants, and 3 or 4 quadrants group) after PDT with no significant differences between groups over 12 months. However, the visual outcome of 3 or 4 quadrant groups was significantly worse than that of the 1 quadrant group (p = 0.020) and 2 quadrants group (p = 0.012; Fig. 1).
Photoreceptor recovery rate
Photoreceptor damage defined as EZ disruption was present in 64% of patients before treatment and usually recovered within 12 months. Recovery rates were higher in the 1 and 2 quadrant groups compared to the 3 or 4 quadrant groups (Fig. 2). Final visual acuity was significantly lower in patients with EZ disruption (0.20 ± 0.30 vs. 0.06 ± 0.11 LogMAR; p = 0.05).
Factors with associated with final visual outcome
Univariate logistic regression indicated that age, initial visual acuity, and the number of quadrants with macula-draining vortex veins were significantly associated with the final visual outcome. Multivariate analysis showed that only the number of quadrants with macula-draining vortex veins remained significant (B = 0.197, p = 0.047; Table 4).
Discussion
In this study, we evaluated the impact of the number of quadrants with engorged vortex veins draining macula on the outcomes of PDT in CSC patients, using UWF ICGA. Our findings indicate that as the number of macula-draining vortex vein increased, the rate achieving dry macula decreased with more persistent PED, EZ disruption, and RPE irregularity. Despite significant reductions in CFT and SFCT across all groups, the final visual outcome was poorer in the 3 or 4 quadrant group.
Previous studies have suggested that factors such as the duration of CSC symptoms and choroidal hyperfluorescence patterns may influence PDT outcomes. Wakatsuki et al.15 reported that longer symptom duration negatively affected achieving a dry macula after PDT. Additionally, other studies have found that prolonged symptoms delay SRF absorption and negatively influence final visual acuity14,16. Studies analyzing ICGA patterns in CSC eyes showed that diffuse hyperfluorescence increased the risk of persistent SRF after PDT, leading to poorer outcomes17,18. Diffuse hyperfluorescence suggesting widespread pigment epitheliopathy appears to be associated with the chronicity of CSC. Therefore, the longer the duration of CSC, the lower the response to PDT.
Contrarily, some studies have reported that symptom duration does not correlate with treatment outcomes19. This discrepancy may arise because symptom duration is a subjective measure based on patient recall and may not be noticed until CSC becomes severe. Additionally, debates exist regarding ICGA patterns, with some studies suggesting that severe choroidal hyperfluorescence correlates with higher rates of achieving a dry macula compared to eyes with no or moderate hyperfluorescence20. This indicates that macular imaging alone may have limitations in assessing CSC severity or chronicity.
In our study, we used UWF ICGA to evaluate the treatment response of PDT based on the number of macula-draining vortex veins. This method was chosen because dilated macula-draining vortex vein may indicate chronic vascular remodeling, and ampulla dilatation represents venous outflow obstruction, potentially related to the etiology. This aligns with the concept of venous overload choroidopathy and vortex vein anastomosis defined by Spaide and Matsumoto et al.8,21 In the current study, eyes with a higher number of macula-draining vortex veins showed poorer anatomical outcomes in achieving a dry macula and more persistent PED. These results are likely due to chronic choroidal outflow obstruction, increasing intravenous hydrostatic pressure, resulting in increased choroidal capillary permeability and functional deterioration of the RPE.
While macular-draining vortex veins have been considered as chronic indicators related to CSC prognosis, it presents a paradox, as increased draining channels should theoretically contribute to reducing hydrostatic pressure. Matsumoto et al.22 reported that patients with pachychoroid neovasculopathy or polypoidal choroidal vasculopathy demonstrated more vortex vein anastomoses compared to CSC patients, showing decreased choroidal thickness. They proposed that increasing anastomoses might alleviate venous congestion. Our study, however, was confined to patients with CSC, creating a distinct cohort from their study. In addition, our previous research9, which reported the characteristics of CSC patients according to the number of macular-draining vortex veins, found that an increase in the number of macular-draining vortex veins correlated with increased choroidal thickness and choroidal hyperpermeability area. Further studies investigating choroidal vascular structures across various stages of pachychoroid disease could provide more insights into this issue.
EZ disruption was a significant factor for the prognosis of CSC patients after PDT. Studies have shown that EZ disruption at baseline13,23,24 and poor EZ recovery25,26 after treatment correlate with worse visual outcomes. In our study, higher numbers of macula-draining vortex veins were associated with greater EZ disruption and lower EZ recovery rates. This suggests that extensive vascular changes contribute to chronic disease and persistent photoreceptor damage, leading to poor visual outcomes.
Regarding choroidal thickness, our study found no significant difference of baseline SFCT between groups with different treatment responses. The role of choroidal thickness in predicting PDT treatment outcomes for CSC remains unclear. While a thicker choroid may intuitively seem beneficial for treatment response, studies have reported conflicting results27,28,29,30,31. In chronic CSC, thicker choroid was associated with unsuccessful outcomes after PDT27, while the opposite result28 was also reported. For acute CSC, one study reported that thinner choroid was linked to further treatment29, whereas another study found the contrary, with thicker choroid observed in recurrent case30. These inconsistent findings suggest uncertain relationship between choroidal thickness and treatment outcomes.
The current study has several limitations including its retrospective nature, and small sample size. Some patients dropped out voluntarily during the follow-up period due to their good visual outcome. Consequently, there may be a selection bias that increases the severity of the disease. Additionally, unmatched gender distribution could be a potential confounding factor given the known predominance of male in CSC. Future prospective studies with larger cohorts are needed to validate these findings.
In summary, our findings highlight the importance of considering macula-draining vortex vein as a predictor of PDT response. Unlike subjective symptom duration, macula-draining vortex vein is an objective indicator that offers a reliable prognostic factor, revealing choroidal outflow abnormalities that are not visible in traditional macular imaging. Identifying the engorged vortex veins draining macula can guide treatment and help predict patient outcomes more effectively in PDT for eyes with CSC.
Methods
Study population
Thirty-six patients with 36 patients with treatment-naïve CSC were retrospectively reviewed among those who visited the Eye Center of Yeungnam University Hospital from January 1, 2017, to December 31, 2019. All patients underwent PDT and were followed up for > 1 year. CSC was diagnosed as a case in which serous retinal detachment was confirmed in the macula area without any other specific findings, and when leakage was observed on fluorescein angiography (FA)17. PDT was performed in patients with symptoms that had persisted for ≥ 3 months. The exclusion criteria were as follows: patients who had previously been treated for CSC, were suspected of choroidal neovascularization, received steroid treatment, had myopia > − 6 diopters, or had undergone ophthalmic surgery within 6 months. This study was approved by the Institutional Review Board (IRB) of Yeungnam University Hospital (approval number: 20222-04-068) and was conducted in accordance with the Declaration of Helsinki. Due to the retrospective nature of the study, the IRB of Yeungnam University Hospital waived the need of obtaining informed consent.
Baseline examination
All patients underwent general ophthalmological examinations, including visual acuity, intraocular pressure, and slit-lamp biomicroscopy. Spectral domain OCT (Spectralis domain OCT; Spectralis OCT, Heidelberg Engineering, Heidelberg, Germany) was used to measure SRF, central foveal thickness (CFT), and subfoveal choroid thickness (SFCT). PED, elongation of PR outer segment, EZ disruption, and RPE irregularity were identified within 1.5 mm of the fovea.
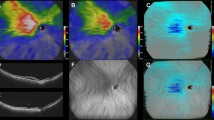
Widefield image acquisition and quantification
UWF FA and ICGA were performed using an Optos California (Optos PLC, Dunfermline, UK). Vortex veins were evaluated in four quadrants (superotemporal, superonasal, inferotemporal, inferonasal)14. Early mid-phase images were processed using ImageJ (National Institutes of Health, Bethesda, MD, USA) software to visualize medium-sized choroidal vessels. (Supplementary Fig. 1). Vortex veins were defined as engorged if they appeared brighter than these vessels, and considered as macula-draining when they elongated to the macula or optic disc. Patients were divided into four groups based on the number of quadrants with engorged vortex vein draining macula.
Photodynamic therapy
Verteporfin was injected intravenously at a dose of 6 mg/m2 for 10 min, followed by a half-fluence PDT with a diode laser (Visulas 690 S; Carl Zeiss Meditec, Inc. Dublin, California, USA) at a 689 nm light wavelength and 25 J/cm2 fluence rate for 83 s18. The targeted area included leakage points on FA, PED on OCT, and hyperfluorescence sites on ICGA.
Outcome measures
Patients were followed up at 1, 3, 6, and 12 months after PDT. Best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, fundus examination, UWF imaging, and OCT were examined. Treatment outcomes included SRF resolution, PED, EZ disruption, and RPE irregularity. The resolution of PED, EZ disruption, and RPE irregularity were also investigated. Changes in CFT, SFCT, and BCVA were measured, and EZ disruption recovery was monitored up to 12 months.
Statistical analysis
SPSS (SPSS ver. 21.0 for Window, IBM Corp., Armonk, NY, USA) was used for statistical analysis. Patients were divided into four groups based on the number of quadrants with macula-draining vortex veins (quadrants 1–4). Kruskal–Wallis test and linear by linear association were conducted. For the comparison of treatment outcomes, 3 and 4 quadrants group were combined. Repeated measures ANOVA compared BCVA, CFT, and SFCT between groups. Log-rank test analyzed EZ disruption recovery, and independent t-test assessed its impact on final visual acuity. Logistic regression analysis evaluated factors associated with final visual acuity.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gass, J. D. Pathogenesis of disciform detachment of the neuroepithelium. Am. J. Ophthalmol.63(Suppl), 1–139 (1967).
Gemenetzi, M., De Salvo, G. & Lotery, A. J. Central serous chorioretinopathy: an update on pathogenesis and treatment. Eye (Lond). 24, 1743–1756. https://doi.org/10.1038/eye.2010.130 (2010).
Marmor, M. F. New hypotheses on the pathogenesis and treatment of serous retinal detachment. Graefes Arch. Clin. Exp. Ophthalmol.226, 548–552. https://doi.org/10.1007/bf02169203 (1988).
Menchini, U., Virgili, G., Lanzetta, P. & Ferrari, E. Indocyanine green angiography in central serous chorioretinopathy. ICG angiography in CSC. Int. Ophthalmol.21, 57–69. https://doi.org/10.1023/a:1005880129005 (1997).
Spaide, R. F. et al. Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina. 16, 203–213. https://doi.org/10.1097/00006982-199616030-00004 (1996).
Prünte, C. Indocyanine green angiographic findings in central serous chorioretinopathy. Int. Ophthalmol.19, 77–82. https://doi.org/10.1007/bf00133176 (1995).
Prünte, C. & Flammer, J. Choroidal capillary and venous congestion in central serous chorioretinopathy. Am. J. Ophthalmol.121, 26–34. https://doi.org/10.1016/s0002-9394(14)70531-8 (1996).
Spaide, R. F., Ledesma-Gil, G. & Gemmy Cheung, C. M. Intervortex venous anastomosis in pachychoroid-related disorders. Retina41, 997–1004. https://doi.org/10.1097/iae.0000000000003004 (2021).
Jeong, S., Kang, W., Noh, D., van Hemert, J. & Sagong, M. Choroidal vascular alterations evaluated by ultra-widefield indocyanine green angiography in central serous chorioretinopathy. Graefes Arch. Clin. Exp. Ophthalmol.260, 1887–1898. https://doi.org/10.1007/s00417-021-05461-0 (2022).
Pang, C. E., Shah, V. P., Sarraf, D. & Freund, K. B. Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am. J. Ophthalmol.158, 362–371e362. https://doi.org/10.1016/j.ajo.2014.04.021 (2014).
Chan, W. M. et al. Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br. J. Ophthalmol.87, 1453–1458. https://doi.org/10.1136/bjo.87.12.1453 (2003).
Schmidt-Erfurth, U. & Hasan, T. Mechanisms of action of photodynamic therapy with verteporfin for the treatment of age-related macular degeneration. Surv. Ophthalmol.45, 195–214. https://doi.org/10.1016/s0039-6257(00)00158-2 (2000).
Moon, J. W., Yu, H. G., Kim, T. W., Kim, H. C. & Chung, H. Prognostic factors related to photodynamic therapy for central serous chorioretinopathy. Graefes Arch. Clin. Exp. Ophthalmol.247, 1315–1323. https://doi.org/10.1007/s00417-009-1104-8 (2009).
Loo, R. H. et al. Factors associated with reduced visual acuity during long-term follow-up of patients with idiopathic central serous chorioretinopathy. Retina. 22, 19–24. https://doi.org/10.1097/00006982-200202000-00004 (2002).
Wakatsuki, Y. et al. Morphological changes and prognostic factors before and after photodynamic therapy for central serous chorioretinopathy. Pharmaceuticals (Basel). 14https://doi.org/10.3390/ph14010053 (2021).
Lai, T. Y., Wong, R. L. & Chan, W. M. Long-term outcome of half-dose verteporfin photodynamic therapy for the treatment of central serous chorioretinopathy (An American Ophthalmological Society Thesis). Trans. Am. Ophthalmol. Soc.113, T8 (2015).
Chung, C. Y., Chan, Y. Y. & Li, K. K. W. Angiographic and tomographic prognostic factors of chronic central serous chorioretinopathy treated with half-dose photodynamic therapy. Ophthalmologica240, 37–44. https://doi.org/10.1159/000484100 (2018).
Parajuli, A. & Joshi, P. Factors influencing the episode duration and the anatomical and functional outcome in cases of acute central serous chorioretinopathy. BMJ Open. Ophthalmol.5, e000540. https://doi.org/10.1136/bmjophth-2020-000540 (2020).
Lai, F. H. et al. A Multicenter Study on the long-term outcomes of half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am. J. Ophthalmol.170, 91–99. https://doi.org/10.1016/j.ajo.2016.07.026 (2016).
Inoue, R., Sawa, M., Tsujikawa, M. & Gomi, F. Association between the efficacy of photodynamic therapy and indocyanine green angiography findings for central serous chorioretinopathy. Am. J. Ophthalmol.149, 441–446e441. https://doi.org/10.1016/j.ajo.2009.10.011 (2010).
Matsumoto, H. et al. Vortex vein anastomosis at the watershed in pachychoroid spectrum diseases. Ophthalmol. Retina4, 938–945. https://doi.org/10.1016/j.oret.2020.03.024 (2020).
Matsumoto, H. et al. Quantitative measures of vortex veins in the posterior pole in eyes with pachychoroid spectrum diseases. Sci. Rep.10, 19505. https://doi.org/10.1038/s41598-020-75789-w (2020).
Yu, J., Ye, X., Li, L., Chang, Q. & Jiang, C. Relationship between photoreceptor layer changes before half-dose photodynamic therapy and functional and anatomic outcomes in central serous chorioretinopathy. Eye (Lond). 35, 1002–1010. https://doi.org/10.1038/s41433-020-1018-6 (2021).
Sousa, K. et al. Outer nuclear layer as the main predictor to anatomic response to half dose photodynamic therapy in chronic central serous retinopathy. J. Ophthalmol.2019, 5859063. https://doi.org/10.1155/2019/5859063 (2019).
Park, D. G., Jeong, S., Noh, D. & Sagong, M. Optimal fluence rate of photodynamic therapy for chronic central serous chorioretinopathy. Br. J. Ophthalmol.105, 844–849. https://doi.org/10.1136/bjophthalmol-2020-316837 (2021).
Ohkuma, Y., Hayashi, T., Sakai, T., Watanabe, A. & Tsuneoka, H. One-year results of reduced fluence photodynamic therapy for central serous chorioretinopathy: the outer nuclear layer thickness is associated with visual prognosis. Graefes Arch. Clin. Exp. Ophthalmol.251, 1909–1917. https://doi.org/10.1007/s00417-013-2289-4 (2013).
van Rijssen, T. J., van Dijk, E. H. C., Dijkman, G. & Boon, C. J. F. Clinical characteristics of chronic central serous chorioretinopathy patients with insufficient response to reduced-settings photodynamic therapy. Graefes Arch. Clin. Exp. Ophthalmol.256, 1395–1402. https://doi.org/10.1007/s00417-018-4003-z (2018).
Haga, F. et al. Long-term prognostic factors of chronic central serous chorioretinopathy after half-dose photodynamic therapy: a 3-year follow-up study. PLoS One. 12, e0181479. https://doi.org/10.1371/journal.pone.0181479 (2017).
Ambiya, V. et al. Subfoveal choroidal thickness as a predictor of central serous chorioretinopathy. Eye (Lond). 30, 1623–1629. https://doi.org/10.1038/eye.2016.209 (2016).
Matet, A. et al. Risk factors for recurrences of central serous chorioretinopathy. Retina38, 1403–1414. https://doi.org/10.1097/iae.0000000000001729 (2018).
Kim, D. Y. et al. Subfoveal choroidal thickness changes in treated idiopathic central serous chorioretinopathy and their association with recurrence. Retina35, 1867–1874. https://doi.org/10.1097/iae.0000000000000557 (2015).
Acknowledgements
This work was supported by a 2022 Yeungnam University research grant.
Author information
Authors and Affiliations
Contributions
S.J. wrote the initial draf of the manuscript. S.J., W.K., and M.S. conceived the concept for this study. S.J. W.K. and M.S. were involved in critical revision of the manuscript. S.J. and M.S. performed the statistical analysis. S.J. and M.S. supervised the study. M.S. is the corresponding author for this study. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jeong, S., Kang, W. & Sagong, M. Influence of vortex vein engorgement for photodynamic therapy in central serous chorioretinopathy. Sci Rep 14, 24424 (2024). https://doi.org/10.1038/s41598-024-75506-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-75506-x