Abstract
Variable sleep patterns are a risk factor for disease, but the reasons some people express greater within-individual variability of sleep characteristics remains poorly understood. In our study, we leverage BSETS, a novel mobile EEG-based dataset in which 1901 nights in total were recorded from 267 extensively phenotyped participants to identify factors related to demographics, mental health, personality, chronotype and sleep characteristics which predict variability in sleep, including detailed sleep macrostructure metrics. Young age, late chronotype, and napping emerged as robust correlates of increased sleep variability. Correlations with other characteristics (such as student status, personality, mental health and co-sleeping) generally disappeared after controlling for age. We critically examine the utility of controlling the correlates of sleep variability for the means of sleep variables. Our research shows that age and sleep habits affecting the amount of sleep pressure at night are the most important factors underlying sleep variability, with a smaller role of other psychosocial variables. The avoidance of daytime naps emerges as the most promising modifiable behavior associated with increased sleep regularity.
Similar content being viewed by others
Introduction
Human sleep is a moderately to strongly individual-specific characteristic. The power spectrum of the electroencephalogram (EEG), if recorded from the same person across multiple nights, is so similar that it is referred to as the sleep EEG fingerprint1,2,3. Conversely, only about a quarter to a half of variance of sleep macrostructure metrics such as total sleep time or sleep efficiency was between-individual in multiday sleep studies4,5,6. Although typical sleep (the mean of sleep metrics across several nights) has been much more commonly studied, within-person variability in sleep has been proposed to be a distinct dimension of sleep metrics7 that may be related to both normal and pathological human variation.
Maintaining a regular sleep pattern is generally recommended by sleep societies in order to preserve health8. Longitudinal analyses have implicated sleep variability as a factor of adversely altered neurodevelopment in adolescents9, in addition to finding that increased sleep variability predicts increased mortality risk10,11. A systematic review12 as well as a large study utilizing sleep monitoring data collected from over 60,000 adults13 linked sleep irregularity to hypertension and its risk factors. Sleep variability was also linked to metabolic health measures such as adiposity and glycemic dysregulation14, as well as cardiometabolic health15,16 in reviews. A recent large study17 reported that sleep variability is a stronger predictor of mortality than mean total sleep time, highlighting the importance of sleep variability in addition to the mean values of sleep metrics.
Several systematic reviews and large-scale studies investigated the potential sources of high intra-individual variability in sleep metrics. A systematic review7 scanned the literature published up to 2014 regarding all correlates of sleep variability. From a synthesis of 53 studies, the review concluded that young age, minority status, poor physical and mental health, non-cohabitation, and poor sleep were most frequently associated with increased sleep variability. These conclusions are largely upheld in the most recent version of this continuously updated literature collection18. Similar factors were found to be associated with sleep variability in another systematic review19 focusing on children and adolescents. A large study based on eight datasets with a total of over 3000 participants20 confirmed that young age is related to increased sleep variability, but found no consistent sex effect and refined findings about minority status.
Weaknesses of the extant literature include the relatively low number of participants per study, limited mapping of psychological traits which may contribute to sleep variability (for example, personality or specific mental health problems), an unsystematic use of various variability metrics, and lack of controls for common-sense drivers of sleep variability such as age or individual mean values of sleep variables7. Furthermore, there is an almost complete lack of polysomnography-based studies (but see21), which limits the literature to investigate variations in sleep timing, but not sleep macrostructure. In the present study, we aimed to investigate the correlates of sleep regularity in a relatively large mobile EEG-based dataset, focusing on normal human variation as opposed to the relatively well-researched domains of physical health. We intended to replicate previous research7,18 regarding the relationship between sleep variability and demographics, mental health and chronotype, extend this investigation to novel traits including personality22,23, and systematically explore the effect of analytical choices (variability metrics and controls) on the results.
Methods
Participants
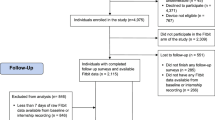
Data from the Budapest Sleep, Experiences and Traits Study (BSETS) was used. The full BSETS protocol has been published separately24. Briefly, BSETS is a multiday observational study in which healthy volunteer participants slept in their homes with a Dreem2 wearable mobile EEG headband25,26 while living their lives according to their normal routines. Participants were instructed to start recording when they intended to sleep. Each day, participants filled out an evening diary about daily experiences and a morning diary about sleep circumstances, sleep quality and dreams. On a separate occasion, they were extensively phenotyped with a web-based questionnaire. A total of 1901 nights from 267 participants were recorded in BSETS, with relatively little missing data for specific sleep or other phenotype variables (see Results). 45% of participants were male, 55% female, with a mean age of 28.9 years with and a right-skewed, bimodal age distribution in line as much of the participant pool consisted of medical students and their parents (Supplementary figure S1).
The Institutional Review Board (IRB) of Semmelweis University as well as the Hungarian Medical Council (under 7040-7/2021/ EÜIG “Vonások és napi események hatása az alvási EEG-re” (The effect of traits and daily activities and experiences on the sleep EEG)) approved BSETS as compliant with the latest revision of the Declaration of Helsinki. All participants gave written informed consent on a form reviewed and approved by the IRB.
Sleep and sleep variability
Subjective sleep quality was rated by participants using the Hungarian version of the Groningen Sleep Quality Scale (GSQS), administered in each morning diary. Higher scores on the GSQS indicate worse sleep quality.
Objective sleep metrics were based on mobile EEG data. Dreem2 recordings are automatically scored on a 30-second basis by an algorithm that demonstrated high validity against visual scorings26. The automatically scored hypnogram was used to extract the following 15 objective sleep macrostructure metrics: total sleep time, sleep onset latency, REM latency, clock time at sleep onset, wake after sleep onset (WASO), sleep efficiency, number of awakenings, as well as the percentage of N1, N2, SWS and REM. The variability of these sleep metrics was estimated via several methods: the individual standard deviation (iSD), the root mean square of successive differences (RMSSD) and average rolling differences (ARD), in line with published recommendations7,27. All variability metrics were calculated using the varian R package. Participants with a single observation and consequently SD = 0 (N = 3) were excluded from analyses.
In addition to within-individual variability in specific sleep metrics, we also calculated the Sleep Regularity Index (SRI28), as an omnibus measure of sleep variability. The SRI is normally calculated from actigraphy which scores an individual’s state at the same time point on successive days as “wake” or “asleep”. We adapted this method to mobile EEGs worn only during the night by (1) coding S1, S2, SWS and REM as “sleep” and (2) filling in “wake” states for all time points in-between EEG recordings. For each second of the day we calculated the following formula28:
This was then averaged across every second of the day to provide a single number per participant. The maximum value of the SRI is 100, expressing perfect regularity of sleep-wake patterns (all time points on all days are spent in the same vigilance state). Lower values indicate higher variability.
Predictors of sleep variability
In line with the strategy of published7,19 and ongoing18 systematic reviews, we organized our analysis around “themes”, conceptually related predictors with a potential relationship with sleep variability. Based on the availability of data in BSETS24 and a literature review7 we set up the following themes:
Theme 1: Demographics and cognition.
In this theme, we used the following predictors: binary-coded sex, age, binary-coded student status, self-reported grades on a national high school graduation examination, and intelligence (estimated as total scores on the ICAR16 brief open-source intelligence test29). Physical health was not assessed in detail in BSETS, but we had data on body mass index (BMI) which we included in this theme.
Theme 2: Personality.
Personality was assessed in BSETS by two questionnaires: the 44-item Big Five Inventory and the 99 item Zuckerman-Kuhlman Personality Questionnaire. The BFI uses 5-point Likert scale items to measure personality along the dimensions of Extraversion, Neuroticism, Agreeableness, Conscientiousness and Openness. The ZKPQ uses binary items to measure personality in an alternative model using the Sociability, Activity, Aggression-Hostility, Neuroticism-Anxiety and Impulsive Sensation Seeking dimensions.
Theme 3: Mental health.
BSETS used the 9-item Patient Health Questionnaire (PHQ-9) to measure symptoms of depression. In addition, the 20-item Toronto Alexithymia Scale (TAS) was used to measure alexithymia and the 28-item Dissociative Experiences Scale (DES) to measure dissociation. For both the TAS and DES, total scores were used. In addition to self-report questionnaires, participants rated positive and negative experiences during the day in each evening diary using the brief Positive and Negative Affect Scale (PANAS). An average across all days was calculated to estimate overall positive and negative emotionality during the study.
Theme 4: Chronotype and sleep.
In the final theme, we focused on sleep habits as predictors of sleep variability. Chronotype was assessed using the Hungarian version of the Munich Chronotype Questionnaire (MCTQ) as free-day midsleep corrected for oversleeping (MSFsc). Symptoms of insomnia were assessed using the Hungarian version of the Athens Insomnia Scale (AIS). In evening diaries, participants indicated the number and duration of daily naps. In the morning diaries, they indicated if they slept alone, with a partner, with a friend or other person, or with an animal (recoded as “alone” or “not alone”) and if they slept in their usual place, at home but not in their usual bed, at a friend’s or partner’s place, or in a hotel (recoded as “Slept in usual place” or “Slept in foreign place”). Individual sums of daily nap frequency, nap duration, and sleeping with another person or a foreign place were entered as four additional variables with a possible influence on sleep variability.
Statistical analysis
In all analyses, we calculated Pearson correlations between all sleep variability metrics and potential predictors.
In the most basic analyses, we calculated zero-order correlations to reveal the simple observed relationship between sleep variability and other characteristics. In a second step, we controlled these correlations for age as a covariate. Published recommendations7 also call for controlling correlations for the means of sleep variables. We disagree that such controls are essential (see the Discussion and the Supplementary note) because while for skewed (gamma-distributed) sleep metrics the means and standard deviations indeed correlate, it is unclear if changes in the former are the cause of the latter and not vice versa. However, in a third model we also calculated correlations corrected for means, as recommended. Age-sleep variability correlations were only corrected for mean sleep measures (if appropriate), and correlations with the Sleep Regularity Index were not corrected for means as the SRI by itself is already a measure of variability without an interpretable mean.
In order to account for the large number of comparisons while avoiding type II errors we initially set the p-value threshold at p = 0.01, but also performed a more formal correction for multiple testing using the Benjamini-Hochberg method30 applied by theme. We report all findings which pass the laxer threshold of p = 0.01, but we focus the discussion on findings which also pass the more stringent test.
Results
Descriptive statistics
Table 1. Descriptive statistics of the variables used in the study. Self-reported phenotypes are expressed in raw points. For these and other bounded variables possible minimum and maximum values are provided in parentheses. Time variables (e.g. sleep latency, total sleep time) are expressed in minutes, except total weekly nap duration which is expressed in hours. Clock time variables (sleep onset time, chronotype) are expressed in fractional hours relative to midnight. Sleep composition and sleep efficiency are expressed in percentages. The means of binary variables sex and student status indicate the proportion of males and students, respectively, while other descriptive statistics are undefined. ‘Slept with others’ and ‘Slept in unusual place’ are averaged proportions over all day in the study and consequently have valid descriptive statistics. For sleep metrics used in variability analyses, the descriptive statistics of both the means and individual standard deviations are reported.
Demographics and cognition
Uncorrected correlations showed that higher age was associated with decreased variation in total sleep time, sleep onset time, and the percentage of N3 sleep, with a corresponding increase in the Sleep Regularity Index. In contrast, higher variability of WASO was also associated with higher age. Student status was also associated with more variable total sleep time, N3%, but less variable WASO (Supplementary figure S2). Controlling for age eliminated all correlations with student status (Fig. 1). The other correlations remained significant after controlling for multiple comparisons.
An additional correction for sleep metric means slightly changed the pattern of correlations (Supplementary figure S3). After this correction, age was still associated with less variable total sleep time and lower SRI, but also with less variability in sleep efficiency and awakenings. These associations, except for the one with sleep efficiency, remained significant after controlling for multiple comparisons.
The association between sleep variability and demographic factors. Each cell shows the correlation between the individual standard deviation of sleep variables (horizontal axis) and the means of demographic factors (vertical axis). All correlations are corrected for age (except for age itself). Only significant correlations (p < 0.01) are shown.
Personality
Impulsive Sensation Seeking was associated with more variable sleep onset times and reduced Sleep Regularity Index, Conscientiousness with lower variability in N3 sleep percentage, Sociability with reduced Sleep Regularity Index, and Openness with more variable N2 sleep percentage (Supplementary figure S4). After corrections for age only the first and the last persisted (Fig. 2). After further controls for sleep metric means (Supplementary figure S5) only the N2% variability-Openness association remained, while Openness was also associated with more variable WASO and awakenings, and Agreeableness was associated with more variable sleep efficiency. No correlations were significant after correction for multiple testing.
The association between sleep variability and personality. Each cell shows the correlation between the individual standard deviation of sleep variables (horizontal axis) and the means of personality traits (vertical axis). All correlations are corrected for age. Only significant correlations (p < 0.01) are shown.
Mental health
Dissociative symptoms were associated with more variable N3 sleep percentage and lower Sleep Regularity Index (Supplementary figure S6). Corrections for age eliminated these correlations while another one (dissociative symptoms being associated with more variable N1 sleep percentage) appeared (Fig. 3). This persisted after further controls for trait means (Supplementary figure S7). No correlation, however, was significant after correction for multiple testing.
The association between sleep variability and mental health. Each cell shows the correlation between the individual standard deviation of sleep variables (horizontal axis) and the means of mental health indicators (vertical axis). All correlations are corrected for age. Only significant correlations (p < 0.01) are shown.
Chronotype and sleep
Significant zero-order correlations were found between a large number of sleep characteristics and the variability of sleep. Late chronotype was associated with more variable sleep onset latency and reduced Sleep Regularity Index. Insomnia symptoms were associated with more variable morning GSQS self-ratings of sleep, but not of objective sleep metrics. More frequent naps during the day were associated with more variable nightly N1 sleep percentage, while longer self-reported naps were associated with higher variability of a host of sleep variables (sleep onset latency, sleep onset time, sleep efficiency, sleep composition, and reduced Sleep Regularity Index). Sleeping with another person or animal more frequently was associated with reduced variability in sleep onset times and the percentage of N3 sleep (Supplementary figure S8).
Controlling for age eliminated most associations. After this control, longer and more frequent naps were still associated with more variable sleep onset latency, WASO, sleep efficiency, and sleep composition. Insomnia symptoms and sleeping in unusual places were also associated with more variable self-rated sleep (Fig. 4). All of these correlations remained significant after corrections for multiple comparisons.
After correcting for sleep metric means, only two associations were significant: the one between chronotype and more variable sleep onset times, and the one between naps and more variable nightly sleep composition (Supplementary figure S9).
The association between sleep variability and sleep/chronotype characteristics. Each cell shows the correlation between the individual standard deviation of sleep variables (horizontal axis) and the means of sleep characteristics and chronotype (vertical axis). All correlations are corrected for age. Only significant correlations (p < 0.01) are shown.
Alternative variability metrics
The two alternative variability metrics (RMSSD and ARD) had extremely high correlations with the individual standard deviation, ranging from 0.8 (ARD, self-rated sleep) to 0.957 (RMSSD, sleep onset latency) (Supplementary table S1). All correlations with individual standard deviations which survived correction for multiple comparisons were replicated with the two alternative sleep metrics, and no new findings emerged.
Nonparametric correlations
Our initial findings were based on Pearson correlations due to the simplicity, robustness to violations of normality, and intuitive interpretability of this metric. However, due to skew in many of our variables (Supplementary figure S1, see also Supplementary note), we re-calculated all effects using Spearman rank correlations, still corrected for age (except for age correlations itself). This method replicated and generally strengthened findings.
Age effects (Fig. 1) replicated, increased in effect size and remained statistically significant, including after FDR corrections, with Spearman correlations. For example, the age-SRI Spearman correlation increased to r = 0.315.
The correlation between higher trait Impulsive Sensation Seeking and more variable sleep onset time increased slightly (r = 0.274) and was now significant even after FDR corrections.
Dissociation remained the only mental health indicator correlated with sleep variability (more variable N1% and N2%) but this effect did not survive FDR correction.
The duration and frequency of naps was still correlated (after FDR correction) with more variable N1%, N3%, and REM%, but not sleep onset latency, WASO or sleep efficiency. More variable sleep was still correlated with insomnia symptoms, but not sleeping in unusual places. Later chronotype was correlated with more variable sleep onset time, an effect not seen with Pearson correlations.
Thus, the use of nonparametric correlation confirms that age and daytime napping have the most profound effects on sleep variability, although some specific napping effects fell short of significance. Nonparametric correlations more confidently reveal relationships between personality, chronotype, and sleep variability, however, we are cautious about interpreting findings which do not replicate across methods.
Comparison with social jetlag
Social jetlag refers to the fact that most people have later sleep times on weekends than on weekdays31. As such, social jetlag is a concept strongly related to sleep variability, especially to the variability of sleep timing. In order to establish the similarity of social jetlag and self-reported or measured sleep variability, we calculated correlations between within-individual standard deviations of sleep metrics and absolute and relative social jetlag. Social jetlag was calculated as standard from self-reported habitual midsleep data in the Munich Chronotype Questionnaire (MCTQ)32,33. Alternatively, we also calculated an EEG-based estimate of social jetlag using objective measures of sleep onset and sleep termination instead of self-reports in the same formula used to calculate MCTQ-based social jetlag.
The self-reported and objective estimates of social jetlag correlated only weakly (r = 0.175). Low correlations were observed between the standard deviation of sleep variables and social jetlag (Supplementary table S1), except for the variability of total sleep time (rMCTQ=0.146, rEEG=0.295), sleep onset time (rMCTQ=0.156, rEEG=0.563) and the sleep variability index (rMCTQ= − 0.262, rEEG= − 0.567). Day of the week (either used as a seven-category predictor or as binary weekday/weekend) accounted for a trivial amount of sleep metrics, with the highest value of R2 = 2.5% observed for sleep onset time (Supplementary table S1). The Sleep Regularity Index had high between-person correlations between weekdays and weekends (r = 0.673), and both weekday (r = 0.915) and weekend (r = 0.629) SRI had high correlations with the total value. In sum, weekend-weekday differences do not seem to be the main driver of the variability of most sleep metrics aside from timing.
Discussion
We used a large mobile EEG-based sample to identify biological, demographic, behavioral and psychological factors underlying sleep variability. We systematically explored the effect of controlling age and sleep metric means on the associations, as well as the use of different variability metrics.
Surprisingly, neither day of the week nor social jetlag were major drivers of sleep variability. We replicated this finding when social jetlag was calculate based on objectively measured sleep timing instead of self-reports of habitual sleep. Only low correlations between self-reported and measured social jet lag were observed. The cause for this can be twofold. On the one hand, self-reports may contain information about sleep timing which is not captured by a single week of objective tracking. Previous findings34,35,36 show that the correlation between self-reported and objectively tracked sleep timing is relatively low, but increases if the duration of the tracking period is longer. On the other hand, self-reports may simply be inaccurate, and reporting errors of different sleep characteristics (such as weekday and weekend bedtimes and rise times) add up if a derivative metric like social jetlag is calculated.
Uncorrected correlations (Supplementary figure S2–S5) between sleep variability and trait-level characteristics replicated patterns familiar from the previous literature. Younger participants and students had less regular sleep, reflected in more variable timing, duration, and composition of sleep and reduced Sleep Regularity Index. In line with previous findings37,38, we found no associations between sleep variability and cognition (school grades or intelligence) or BMI. We found no associations between affective symptoms and sleep variability, although less regular sleep was associated with dissociative symptoms. Sleep was more variable in those with a later chronotype7 and those who napped frequently, but co-sleeping with people or animals was associated with more regular sleep patterns39,40. To the best of our knowledge, ours is the largest study exploring the association between personality and sleep regularity (see22,23 for previous work). Findings were sporadic, but impulsivity and sociability had some associations with less regular sleep. Although the choice of the specific variability metric is very important in theory27, in practice we found that the individual standard deviation and two alternative variability metrics were very highly correlated in the current sample and the choice of variability metric has little influence on the results.
There are two factors, however, which may confound these results. First, age is associated with less variable sleep (Fig. 1, Supplementary figure S2, see also7,19), suggesting that it may confound the association of other age-variant human characteristics with sleep variability. A statistical control for age eliminated the apparent higher sleep variability in those who are students, have higher Sociability (BFI) and Impulsive Sensation Seeking (ZKPQ) personality scores, more dissociative symptoms, a later chronotype, and those who sleep alone more frequently, indicating that the associations were primarily driven by age and not by the psychosocial characteristics per se.
Second, the standard deviation of a person’s sleep metrics across days was strongly correlated with the means (Supplementary table S1, see also7,41 for theoretical treatises). As expected, given that sleep variability metrics are often bounded by an ideal value such as zero sleep latency or perfect sleep efficiency, bounded variables had the strongest mean-SD correlations and the sign of the correlation corresponded to the direction of skew in these variables. This suggests that variability is strongly driven by outlying values, and these outlying values also affect the mean. The correlation between means and standard deviations suggests that correlations with variability in sleep characteristics may simply reflect a correlation with mean values. For example, while participants scoring higher on the Impulsive Sensation Seeking ZKPQ personality scale have more variable sleep onset times (r = 0.25, p < 0.001), they also have later mean sleep onset times (r = 0.21, p < 0.001), mean sleep onset times and their variability are correlated (r = 0.46, p < 0.001), and controlling for means reduces the correlation between the personality trait and sleep onset variability to insignificance (r = 0.1, p = 0.11).
After further controls for the means of sleep metrics, the pattern of correlations with sleep variability changed substantially. Older age was still associated with less variable sleep after controlling for means. Of personality traits, only Openness was associated with more variable sleep (WASO, N2 sleep percentage and awakenings). Isolated correlations were seen between more variable sleep efficiency and the Agreeableness personality trait and N1 sleep percentage and dissociative symptoms. A later chronotype was only associated with increased variability in sleep timing, mirroring its well-known association with social jetlag42. More frequent napping was associated with more variable sleep composition, likely reflecting variable sleep pressure during nightly sleep43. Of these nominally significant (p < 0.01) correlations, only age effects survived a stringent control for multiple testing, a finding replicated using the two alternative sleep variability metrics as well.
In sum, we found age to be the only factor unambiguously associated with sleep regularity: older participants had more regular sleep schedules. This finding survived corrections for sleep metric means and stringent controls for multiple testing. Some correlations with personality and mental health were significant using the p < 0.01 threshold but did not survive a more stringent control for age and multiple testing and are possibly spurious. Sleep habits – especially napping and a late chronotype – also emerged as correlates of higher sleep variability, but their formal significance after multiple comparisons corrections depended on whether the means of sleep metrics were controlled.
We consider controlling for age to be unambiguous, as age is a clear confounder of the relationship between sleep and other characteristics. It is our view, however, that despite recommendations for it7, controlling for means may be unnecessary and may in fact mask a genuine association between sleep variability and other traits. This is especially true for sleep metrics bounded at ideal value, such as sleep onset latency or sleep efficiency, which have mean values close to ideal (e.g. in the current sample MSOL=14.99, SD = 12.61; MSE=90.92, SD = 5.51). For these variables, the room for variation is asymmetric and the variables are skewed, approximately following a gamma distribution. In such a distribution, means and standard deviations are mathematically related and there is a plausible causal route from both to the other. While a mean value more distant from the ideal increases the room for variation41, increased variability necessarily results in more bound-distant values which ultimately affect the mean. (See the Supplementary note for a simulation and Supplementary table S1 which demonstrates that bounded and skewed sleep metrics exhibit the higher correlations between means and standard deviations). Thus, we suggest that mean differences in certain sleep metrics may be the mathematical consequence, rather than the cause, of sleep variation, and statistically controlling them introduces overadjustment bias44.
In the current study, the question of controlling for means was critical in the case of napping effects on the variability of sleep onset latency, WASO and sleep efficiency. Without controlling for means, the increased variability of these sleep variables (in addition to sleep stage percentages), were associated with longer naps (Fig. 4). These effects survived corrections for multiple comparisons. However, with controls for means only the correlation with stage percentages persisted and did not survive corrections for multiple comparisons (Supplementary figure S9). We believe that this illustrates our point about the problematic nature of controlling for means. Naps during the day reduce sleep pressure, affecting the characteristics of nightly sleep45,46. More frequent napping changes the means of sleep characteristics (because some nightly sleeps are affected by the preceding nap), but also introduces variability as a nap occurs on some days but not others. Changing means in this case are not an artifact to be controlled but the consequence of the very same phenomenon that increases variability. Controlling for means effectively controls for a large part of the mechanism that caused variability.
Our study has a number of limitations. First, for the purposes of the current study BSETS is a cross-sectional study and we cannot establish the route of causation between sleep variability and other factors. Longitudinal studies are needed to clarify these. Second, the use of self-reported variables may introduce bias, typically in the downward direction as error is introduced due to the inaccuracy of self-reports. Third, although the findings cohere well with the literature, the generalizability of the findings may be affected by the demographics of the BSETS sample which predominantly consists of young, well-educated individuals. A specific demographic limitation is a positive selection for education and cognitive ability as BSETS participants were mostly drawn from the social circles of medical students. This led to restriction of range in terms of school grade and intelligence and affected our ability to detect correlations with these variables (note that the median participant had the highest possible grades from all three subjects, Table 1). Correlations with grades may have been also impacted by grade inflation as younger participants systematically had better grades (rmath=− 0.183, rliterature=-0.132, rhistory=− 0.105), and by the fact that participants older than 33 years (N = 52) may have obtained their grades in a different exam scheme which was abandoned in 2005.
In conclusion, we have shown age and sleep habits to be the most important drivers of sleep variability, with a comparatively smaller role of normal and pathological psychological characteristics. Controlling for age as an important driver of reduced sleep variability, many zero-order correlations (such as those with student status or sleeping alone) are reduced to non-significance. Conversely, we claim that statistically adjusting associations for variable means is not obviously the right choice and may introduce overcontrol bias. Our findings highlight napping habits as the most modifiable factor affecting sleep regularity.
Data availability
Raw data, code used for simulations, and a high-quality image of variable distribution fits used in the Supplementary note are available at https://osf.io/crfw3/.
References
De Gennaro, L., Ferrara, M., Vecchio, F., Curcio, G. & Bertini, M. An electroencephalographic fingerprint of human sleep. Neuroimage. 26, 114–122 (2005).
Finelli, L. A., Achermann, P. & Borbély, A. A. Individual fingerprints in human sleep EEG topography. Neuropsychopharmacology. 25, S57–62 (2001).
Eggert, T., Dorn, H. & Danker-Hopfe, H. The Fingerprint-Like Pattern of Nocturnal Brain Activity demonstrated in young individuals is also Present in Senior Adulthood. Nat. Sci. Sleep. 14, 109–120 (2022).
Yap, Y. et al. Daily relations between stress and electroencephalography-assessed sleep: a 15-Day intensive Longitudinal Design with Ecological momentary assessments. Ann. Behav. Med. https://doi.org/10.1093/abm/kaac017 (2022).
Messman, B. A. et al. Associations between daily affect and sleep vary by sleep assessment type: what can ambulatory EEG add to the picture? Sleep. Health. 7, 219–228 (2021).
Pierson-Bartel, R. & Ujma, P. P. Objective sleep quality predicts subjective sleep ratings. Sci. Rep. 14, 5943 (2024).
Bei, B., Wiley, J. F., Trinder, J. & Manber, R. Beyond the mean: a systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep. Med. Rev. 28, 108–124 (2016).
Sletten, T. L. et al. The importance of sleep regularity: a consensus statement of the National Sleep Foundation sleep timing and variability panel. Sleep. Health. 9, 801–820 (2023).
Telzer, E. H., Goldenberg, D., Fuligni, A. J., Lieberman, M. D. & Gálvan, A. Sleep variability in adolescence is associated with altered brain development. Dev. Cogn. Neurosci. 14, 16–22 (2015).
Omichi, C. et al. Irregular sleep and all-cause mortality: a large prospective cohort study. Sleep. Health. 8, 678–683 (2022).
Cribb, L. et al. Sleep regularity and mortality: a prospective analysis in the UK biobank. doi: (2023). https://doi.org/10.7554/eLife.88359.2
Makarem, N., Zuraikat, F. M., Aggarwal, B. & Jelic, S. St-Onge, M.-P. variability in sleep patterns: an emerging risk factor for hypertension. Curr. Hypertens. Rep. 22, 19 (2020).
Scott, H. et al. Sleep irregularity is associated with hypertension: findings from over 2 million nights with a large global population sample. Hypertension. 80, 1117–1126 (2023).
Zuraikat, F. M. et al. Sleep regularity and cardiometabolic heath: is variability in sleep patterns a risk factor for excess adiposity and glycemic dysregulation? Curr. Diab Rep. 20, 38 (2020).
Zhu, B. et al. Associations between sleep variability and cardiometabolic health: a systematic review. Sleep. Med. Rev. 66, 101688 (2022).
Fritz, J. et al. Cross-sectional and prospective associations between sleep regularity and metabolic health in the Hispanic Community Health Study/Study of latinos. Sleep 44, 1–11 (2021).
Windred, D. P. et al. Sleep regularity is a stronger predictor of mortality risk than sleep duration: a prospective cohort study. Sleep 47, 1–11 (2024).
Bei, B. Intraindividual Variability of Sleep: An Ongoing Systematic Review. https://sleepv.org/
Becker, S. P., Sidol, C. A., Van Dyk, T. R., Epstein, J. N. & Beebe, D. W. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: a systematic review. Sleep. Med. Rev. 34, 94–121 (2017).
Messman, B. A. et al. How much does sleep vary from night-to-night? A quantitative summary of intraindividual variability in sleep by age, gender, and racial/ethnic identity across eight-pooled datasets. J. Sleep. Res. 31, e13680 (2022).
Cheek, R. E., Shaver, J. L. & Lentz, M. J. Lifestyle practices and nocturnal sleep in midlife women with and without insomnia. Biol. Res. Nurs. 6, 46–58 (2004).
Taub, J. M. & Hawkins, D. R. Aspects of personality associated with irregular sleep habits in young adults. J. Clin. Psychol. 296–304 (1979).
Monk, T. H., Petrie, S. R., Hayes, A. J. & Kupfer, D. J. Regularity of daily life in relation to personality, age, gender, sleep quality and circadian rhythms. J. Sleep. Res. 3, 196–205 (1994).
Taji, W., Pierson, R. & Ujma, P. P. Protocol of the Budapest sleep, experiences, and traits study: an accessible resource for understanding associations between daily experiences, individual differences, and objectively measured sleep. PLoS One. 18, e0288909 (2023).
Dreem, I. Dreem Whitepaper. (2017).
Arnal, P. J. et al. The Dreem Headband compared to polysomnography for electroencephalographic signal acquisition and sleep staging. Sleep 43, 1–13 (2020).
Wiley, J. F., Bei, B., Trinder, J. & Manber, R. Variability as a predictor: a bayesian variability model for small samples and few repeated measures. arXiv. https://doi.org/10.48550/arxiv.1411.2961 (2014).
Phillips, A. J. K. et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci. Rep. 7, 3216 (2017).
Dworak, E. M., Revelle, W., Doebler, P. & Condon, D. M. Using the international cognitive ability resource as an open source tool to explore individual differences in cognitive ability. Pers. Individ Dif. 109906 https://doi.org/10.1016/j.paid.2020.109906 (2020).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. Roy. Stat. Soc.: Ser. B (Methodol.). 57, 289–300 (1995).
Wittmann, M., Dinich, J., Merrow, M. & Roenneberg, T. Social Jetlag: misalignment of biological and social time. Chronobiol Int. 23, 497–509 (2006).
Haraszti, R. Á., Ella, K., Gyöngyösi, N., Roenneberg, T. & Káldi, K. Social Jetlag negatively correlates with academic performance in undergraduates. Chronobiol Int. 31, 603–612 (2014).
Roenneberg, T., Wirz-Justice, A. & Merrow, M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms. 18, 80–90 (2003).
Schneider, J., Fárková, E. & Bakštein, E. Human chronotype: comparison of questionnaires and wrist-worn actigraphy. Chronobiol Int. 39, 205–220 (2022).
Thun, E. et al. An Actigraphic Validation Study of Seven Morningness-Eveningness Inventories. Eur. Psychol. 17, 222–230 (2012).
Paciello, L. M. et al. Validity of chronotype questionnaires in adolescents: correlations with actigraphy. J. Sleep. Res. 31, e13576 (2022).
McCrae, C. S., Vatthauer, K. E., Dzierzewski, J. M. & Marsiske, M. Habitual sleep, reasoning, and Processing Speed in older adults with Sleep complaints. Cognit Ther. Res. 36, 156–164 (2012).
Kuula, L. et al. Naturally occurring circadian rhythm and sleep duration are related to executive functions in early adulthood. J. Sleep. Res. 27, 113–119 (2018).
Minors, D., Atkinson, G., Bent, N., Rabbitt, P. & Waterhouse, J. The effects of age upon some aspects of lifestyle and implications for studies on circadian rhythmicity. Age Ageing. 27, 67–72 (1998).
Goldman, S. E. et al. Association between nighttime sleep and napping in older adults. Sleep. 31, 733–740 (2008).
Baird, B. M., Le, K. & Lucas, R. E. On the nature of intraindividual personality variability: reliability, validity, and associations with well-being. J. Pers. Soc. Psychol. 90, 512–527 (2006).
Ujma, P. P., Horváth, C. G. & Bódizs, R. Daily rhythms, light exposure and social jetlag correlate with demographic characteristics and health in a nationally representative survey. Sci. Rep. 13, 12287 (2023).
Borbély, A. & Tobler, I. The two-process model: origin of its concepts and their implications. Clin. Translational Neurosci. 8, 5 (2023).
Schisterman, E. F., Cole, S. R. & Platt, R. W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 20, 488–495 (2009).
Werth, E., Dijk, D. J., Achermann, P. & Borbély, A. A. Dynamics of the sleep EEG after an early evening nap: experimental data and simulations. Am. J. Physiol. 271, R501–R510 (1996).
Campbell, I. G. & Feinberg, I. Homeostatic sleep response to naps is similar in normal elderly and young adults. Neurobiol. Aging. 26, 135–144 (2005).
Acknowledgements
This paper was supported by the János Bolyai Research Scholarship of the Hungarian Academy of Sciences. This research was supported by the National Research, Development and Innovation Office – NKFIH (grant number: 138935), as well as by the Ministry of Culture and Innovation in Hungary (TKP2021-EGA-25, TKP2021-NKTA-47).
Author information
Authors and Affiliations
Contributions
PPU: conceptualization, methodology, formal analysis, writing—original draft. BR: conceptualization, writing—Original draft. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ujma, P.P., Bódizs, R. Correlates of sleep variability in a mobile EEG-based volunteer study. Sci Rep 14, 26012 (2024). https://doi.org/10.1038/s41598-024-76117-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-76117-2