Abstract
Depressive disorder is a significant public health problem worldwide, which adversely affects children and adolescents’ health. Impaired fasting blood glucose (IFG) is more common in depressive disorder, which becomes a clinical problem that needs to be focused on. The study purposed to determine the prevalence and related factors of IFG in Chinese children and adolescents with depressive disorder and the relationship between triglyceride and high-density lipoprotein cholesterol (TG/HDL-C) ratio and IFG. This research encompassed 756 individuals aged 8 to 18 with major depressive disorders, all diagnosed under DSM-5 criteria at the Third People’s Hospital of Fuyang from January 2020 to December 2021. We detected fasting blood glucose (FBG) and lipid levels and assessed the suicidal behaviors and depressive symptoms severity of each participant. The sociodemographic and included study variables were collected and analyzed. Our study employed multiple logistic regression to discern independent factors affecting IFG in conjunction with depressive disorders among children and adolescents. The prevalence of IFG was 6.5% (49/756). IFG was positively correlated with FBG, BMI, TG, TG/HDL-C, and was negatively correlated with gender and the type of antidepressant drug taken. Binary logistic analysis showed that male (OR = 2.57, 95% CI: 1.43–4.63, P = 0.002) and higher levels of TG (OR = 1.63, 95% CI: 1.11–2.38, P = 0.013) were independently associated with IFG in children and adolescents with depressive disorder. The incidence of IFG in children and adolescents with depressive disorder was high and was positively related to the TG/HDL-C ratio. The evaluation and management of IFG in pediatric depression should extend beyond pharmacological interventions. Comprehensive strategies in both assessment and management of IFG are essential to address this condition effectively in young patients facing depressive disorders.
Similar content being viewed by others
Introduction
Major depressive disorder (MDD) is a joint group of psychiatric disorders in adolescence, which is characterized by symptoms such as low affect, decreased interest, and low energy. Global epidemiologic results show that the 1-year and total lifetime prevalence of MDD in adolescents is 8% and 19%, respectively, and the trend is increasing year by year1. The latest survey data in China show that the prevalence of depressive disorders in adolescents is about 3.0%2. Depressive disorders are often accompanied by altered dietary patterns in the population, resulting in abnormal blood glucose and lipid levels. The prevalence of impaired fasting glucose (IFG) in the general adult population was 12.7%3. A large flow-up study showed that the majority of IFG was 1.2% in children aged 5–6 years4. Another national health and nutrition survey of the adolescent population aged 12–18 years showed that the majority of IFG was 17%5. A Korean study in adolescents aged 10–19 years stated that the prevalence of IFG was 7.9%6. In addition, the majority of IFG among adolescents in the United States and Mexico was 11.4%7 and 11.2%8, respectively. European studies, such as Italy, Lithuania, and Denmark people, found that the prevalence of IFG in overweight or obese adolescents was 3.4%9, 6.9%10, and 14.1%11, respectively. One study found that the prevalence of IFG in obese Arab adolescents was around 16.5%12. Besides, Vietnamese and Iranian adolescent survey studies showed that the majority of IFG was 6.1%13 and 7%14, respectively. Evidence suggests that IFG is more common in children and adolescents, and the prevalence varies significantly among national people. It is becoming a clinical problem that needs to be focused on.
Scholarly investigations have demonstrated that elevated fasting glucose is intricately linked with the manifestation of depressive symptoms, affecting glucose metabolism in patients diagnosed with MDD, thereby disrupting overall glucose homeostasis15. Clinical observations reveal that the incidence of IFG among Chinese MDD patients fluctuates between 12.6% and 13.6%16,17. These findings bolster the hypothesis that depression significantly contributes to the onset of metabolic syndrome and its various components, namely waist circumference, hypertension, fasting blood glucose (FBG), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C)18. Further research conducted in China elucidates that disturbances in glucose metabolism in MDD patients correlate with several clinical parameters, including depression and anxiety scores, total cholesterol (TC), TG, both HDL-C and low-density lipoprotein cholesterol (LDL-C), alongside suicidal tendencies and psychotic manifestations19. In a related vein, studies indicate a strong association between FBG levels, insulin resistance, and suicidal behaviors in individuals suffering from depressive disorders20. The TG/HDL-C ratio emerges as a vital metric for assessing insulin resistance levels21. This ratio not only relates directly to anomalies in glucose metabolism but also serves as a predictive marker for the development of impaired glucose tolerance and, by extension, prediabetes and diabetes22,23,24. FBG testing, necessitating just a single blood draw, offers a convenient, reliable method for screening prediabetes and type 2 diabetes, which underscores its clinical indispensability25. The intricate interplay between FBG and clinical manifestations, lipid profiles, and metabolic syndrome markers in MDD patients is evident, making it a pivotal area of study. Moreover, investigating the prevalence of IFG and exploring the relationship between the TG/HDL-C ratio and IFG in adolescents with depressive disorders could yield valuable clinical insights, potentially guiding future therapeutic strategies.
In conclusion, the prevalence of IFG in the adolescent population is high, while the prevalence of IFG in patients with depressive disorders has been less studied. In addition, there may be a link between the TG/HDL-C ratio and the occurrence of IFG, which still needs further investigation. Therefore, this study has the following research objectives: (1) to explore the prevalence of IFG in adolescent patients with depressive disorders; (2) to analyze the correlation between TG/HDL-C ratio and IFG; and (3) to explore the independent correlates of IFG in adolescent patients with depressive disorders.
Subjects and methods
Subjects
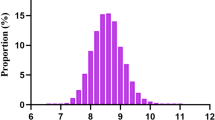
756 participants were enrolled from January 2020 to December 2021 in the Third People’s Hospital of Fuyang. Inclusion criteria: (1) Age 8–18 years; (2) meet the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) diagnostic criteria for major depressive disorders. Exclusion criteria: (1) Individuals enduring serious ailments including epilepsy, cardiac issues, tumors, or other diseases impacting brain function; (2) subjects previously diagnosed with any psychiatric conditions prior to participation; (3) participants lacking the capacity to comprehend the survey materials; (4) during pregnancy or breastfeeding. This study was conducted by the guidelines of the Declaration of Helsinki 1975 And approved by the Medical Ethics Committee of the Third People’s Hospital of Fuyang (granted number: [2018]2018-340-10). The enrolled patients and their guardians agreed to participate in the project. They signed an informed consent form after knowing the purpose of the study, the process, and the related advantages and disadvantages.
General information and biochemical indicators
Clinical data collection
Accurately measure the height and weight of the study subjects, retaining one decimal place. The formula for calculating BMI is weight (kg) / [height (m)]2. Social demographic details, including gender and age, were meticulously compiled alongside clinical electronic medical records and patient-completed questionnaires. These records encompassed comprehensive clinical information such as age at disease onset, overall disease duration, frequency of hospital admissions, and specifics regarding the current medications in terms of type and dosage for enrolled patients diagnosed with MDD. The therapeutic dose of antidepressant medication was converted to fluoxetine equivalents for each subject26.
Biochemical indexes
All patients were collected fasting peripheral venous blood (from the cephalic vein) early in the morning of the next day of admission from 6:00 to 8:00 a.m. and preserved in EDTA tubes. Fasting blood glucose (FBG), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and other hematological indexes were detected, respectively. Referring to the American Diabetes Association fasting blood glucose level, a fasting blood glucose level of 5.6–6.9 mmol/L was defined as IFG27.
Suicidal ideation and suicidal behavior
We used three easy questions to assess suicidal behavior in the last three months: 1. “Have you ever seriously considered committing suicide or killing yourself?”; 2. “Have you ever made a detailed plan to commit suicide?”; 3. “Have you ever attempted suicide in your life?” Please respond with either “yes” or “no.” Suicidal ideation is identified if only the first two criteria are satisfied. Should all three criteria be met, it qualifies as an attempted suicide.
Clinical global impression (CGI) scale
The severity of the disease using the Clinical Global Impression Severity Scale (CGI-S)28. An 8-point scale from 0 to 7 was used to assess the severity of symptoms in each study case separately.
Statistical methods
Using IBM SPSS 22.0 for data analysis. We represented categorical or continuous variables as frequencies and proportions or means and standard deviations, respectively. Continuous variables were compared between groups using the Independent Samples T Test; otherwise, the Mann-Whitney U or χ2 test was used appropriately. Pearson or Spearman rank correlation analysis is used to analyze the relation between FBG, IFG, and TG/HDL-C ratios with various variables, including clinical variables and biochemical indicators. In examining the independent associated factors for IFG in the context of depressive disorders among children and adolescents, variables from sociodemographic and clinical backgrounds that demonstrate significance (p < 0.05) in univariate analyses are subsequently included in a binary logistic regression. This regression model identifies independent predictors for the presence of IFG in this specific population, with IFG coded as 0 for ‘No’ and 1 for ‘Yes’. P < 0.05 was set as a level of statistical test.
Results
Comparison of general data and biological indexes of IFG group and non-IFG group
A total of 756 patients were included, including 214 (28.3%) males and 542 (71.7%) females. The prevalence of IFG was 6.5% (49/756). The results found a statistically significant difference in gender, BMI, FBG, TG, and TG/HDL when patients with IFG were compared to those without IFG (P < 0.05). See Table 1.
Association of research variables with FBG, IFG, and TG/HDL
In the analysis presented in Table 2, we employ Pearson or Spearman rank correlation methods to examine the relationships between FBG, IFG, and TG/HDL-C ratios, and a range of variables. These variables encompass both clinical and biochemical indicators. Clinical features including age at diagnosis, age at initial hospitalization, overall duration of the illness, and the number of hospital admissions are indicative of disease progression following the diagnosis of MDD. The analysis also integrates categorical variables, which are coded numerically to facilitate the correlation assessment: gender is categorized as 1 for male and 2 for female, while educational attainment is represented by 1 for primary school, 2 for middle school, and 3 for high school. These categorical variables are systematically analyzed to determine their correlation with FBG, IFG, and TG/HDL-C ratios. Spearman’s correlation analysis yielded a positive correlation between FBG and IFG, BMI, TG, TG/HDL-C, and age, gender, age at onset, age at first hospitalization, and type of antidepressant medication taken were negatively correlated. IFG was positively correlated with FBG, BMI, TG, TG/HDL-C, and were negatively correlated with gender and the type of antidepressant drug taken. TG/HDL-C was positively correlated with BMI, FBG, and IFG. See Table 2.
Independently associated factors for IFG in patients with depressive disorder
Binary logistic analysis indicated that male (relative to female) (OR = 2.57, P = 0.002) and high TG levels (OR = 1.63, P = 0.013) were independently associated with IFG in all patients. See Table 3. In our study, the suitability of the model was evaluated using the Hosmer and Lemeshow Test. A P value of 0.190, exceeding the threshold of 0.05, suggests that the model effectively captures the information present in the data, indicating a high level of goodness of fit.
Discussion
The present study was a cross-sectional research study investigating the prevalence of IFG in adolescent patients with depressive disorders, exploring the correlation between IFG and TG/HDL-C, and analyzing the independent correlates of IFG occurrence. The results showed that the prevalence of IFG in adolescent patients with depressive disorders was 6.5% (49/756), and IFG was positively correlated with TG/HDL-C. Regression analysis indicated that male and high TG levels were independent correlates of IFG.
Research conducted across various regions of China indicates that IFG is found in approximately 0.7–17% of the adolescent population5,29,30,31,32. In comparison, studies from the Americas and Europe report a slightly lower prevalence, with figures ranging from 3.4 to 11.2% among adolescents8,9. Notably, earlier research highlights those adult patients with MDD exhibit IFG prevalence rates between 12.6% and 13.6%16,17. These findings suggest that IFG prevalence could be comparatively lower in adolescents with depressive disorders than in adults diagnosed with MDD. This investigation highlights that individuals with IFG exhibit elevated levels of FBG, BMI, TG, and the TG to HDL-C ratio. Supporting literature underscores a marked association between increased BMI and the emergence of IFG13, with studies indicating that the incidence of prediabetes, which encompasses both IFG and impaired glucose tolerance, escalates significantly alongside rising obesity rates9. Furthermore, data reveals that the prevalence of IFG is substantially greater among overweight or obese adolescents compared to their normal-weight counterparts, with reported rates of 14.1% versus 4.3%11. Additionally, a positive correlation exists between FBG levels and TG, while an inverse relationship is noted with HDL-C11,33. Concurrently, dyslipidemia is identified as an independent factor linked to elevated FBG levels, with TG, HDL-C, and LDL-C serving as individual predictive markers for IFG34. Furthermore, compared to adolescents without abnormal glucose metabolism, those with abnormal glucose metabolism had significantly higher non-HDL cholesterol levels, systolic blood pressure, central obesity, insulin sensitivity, and higher cardiometabolic risk than before35.These findings underscore the intricate interplay between lipid profiles, body weight, and glucose metabolism in the pathophysiology of prediabetes, particularly IFG, thereby providing a basis for targeted interventions in these domains.
Previous literature noted that the TG/HDL-C ratio was positively correlated with the level of insulin resistance and can be used as a simple method to identify insulin resistance in an organism36,37. It has been noted that high blood glucose levels were positively correlated with a higher TG/HDL-C ratio in the organism38. And that the TG/HDL-C ratio positively predicted the onset of prediabetes and diabetes mellitus22,23,24,39. As the body’s fasting glucose rises, β-cell insulin sensitivity is significantly impaired40. For instance, glucose levels between 6.1 and 6.9 mmol/L were significantly correlated with lower glucose disposition index (GDI, i.e., the product of insulin and insulin sensitivity)41. Previous study findings elucidate that the TG/HDL-C ratio serves as a robust biomarker for identifying adolescents with elevated insulin resistance and increased cardiometabolic risk, noting distinct variances across genders21. Research conducted on New Zealand adolescents revealed that this ratio is a superior predictor of IFG42. Furthermore, FBG levels in adolescents diagnosed with MDD are markedly higher compared to their healthy counterparts, suggesting a potential link to escalated insulin resistance43. Moreover, intensified psychiatric symptoms in adolescents with depressive disorders are associated with heightened insulin resistance, thereby serving as a detrimental intermediary in the relationship between depression and insulin resistance44. The current research corroborates these findings by demonstrating a positive correlation between the TG/HDL-C ratio and both FBG and IFG levels. This alignment with prior studies conducted on the general adolescent cohort affirms the validity of the TG/HDL-C ratio as a predictive marker in adolescents experiencing depression.
Research in the field of psychoneuroendocrinology has increasingly highlighted the intricate link between metabolic irregularities and mood disorders. A pivotal study from China has revealed that disruptions in glucose metabolism among patients with MDD are closely linked to a spectrum of clinical indicators. These include severe manifestations of anxiety and depression, lipid profiles such as TC, TG, HDL-C, and LDL-C, as well as suicidal inclinations and psychotic symptoms19. Further investigation into this domain has shown a compelling association between elevated fasting blood glucose levels and the incidence of dyslipidemia in adolescents diagnosed with depressive disorders45. This correlation underscores the metabolic complexities underlying psychiatric conditions in younger populations. Meanwhile, gender-specific analysis indicates distinct metabolic profiles in relation to IFG. A comprehensive survey involving German and Swedish adolescents found that males, particularly those with advanced age and higher degrees of obesity, displayed a significantly increased risk of developing IFG46. Conversely, a separate study highlighted that older age and female gender are protective factors against IFG among adolescents14. The role of gender in the prevalence of IFG has been debated; however, current evidence suggests that it is not a significant determinant. Instead, critical factors influencing IFG include BMI, residence in rural settings, younger age13, and elevated levels of insulin, C-peptide, and glycated hemoglobin (HbA1c)11. Additionally, Clinical studies have pointed out that men and women had different TG/HDL-C ratio nodes, respectively, and metabolism-related indices were significantly worse when the TG/HDL-C ratio was > 2.5 in women or > 3.5 in men21. The current evidence might not clarify the correlation between gender and high risk of IFG because of the differences in the inclusion of study subjects in different studies, the varying criteria for IFG identification, and the various methods of testing lipid levels. However, these findings collectively emphasize the need for a holistic approach in understanding and managing metabolic dysfunctions in psychiatric conditions, particularly in diverse demographic groups. This approach could potentially enhance therapeutic strategies and improve clinical outcomes for individuals suffering from disorders such as MDD.
As a cross-sectional survey study, this study has several limitations. First, it is challenging to clarify the causal relationship between IFG and related factors due to including study subjects at a single point in time without follow-up tracking. Second, although this study included adolescents with depressive disorders, no correlation was found between depressive symptoms and the occurrence of IFG, which may need to be confirmed by further research. Furthermore, this study is an independent investigation in a single geographic region. The sample representation is limited, and further multicenter and multitemporal follow-up studies are needed to explore the main idea of the study further.
Conclusion
The present study revealed a prevalence of IFG of 6.5% in adolescents with depressive disorders, adding partial evidence to relevant studies in this population. Correlation analysis showed that TG/HDL-C was positively correlated with FBG and IFG, although regression analysis results did not validate it. In addition, high levels of TG and gender were independent influences on IFG. In clinical practice, comprehensive strategies in both assessment and management of IFG are essential to address this condition effectively in young patients facing depressive disorders.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Shorey, S., Ng, E. D. & Wong, C. H. J. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and meta-analysis. Br. J. Clin. Psychol. 61 (2), 287–305 (2022).
Li, F. et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J. Child Psychol. Psychiatry Allied Discip. 63 (1), 34–46 (2022).
Shen, M. Y. et al. Associations between different levels of blood pressure and risk of prediabetes. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi. 43 (12), 1939–1944 (2022).
Wang, S. et al. Abnormal glucose in pre-school children and the association with obesity/physical activity: a large population-based study. Diab./Metab. Res. Rev. 37 (7), e3442 (2021).
Tester, J. M., Stiers, K. B., Garber, A. & Leung, C. W. Whole Grain Intake and Impaired Fasting Glucose in Adolescents, National Health and Nutrition Examination Survey, 2005–2014. Prev. Chronic Dis. 17, E130 (2020).
Lee, J. et al. Discrepancies between Glycosylated Hemoglobin and Fasting Plasma Glucose for Diagnosing Impaired Fasting Glucose and diabetes Mellitus in Korean Youth and Young adults. Diabetes Metabolism J. 43 (2), 174–182 (2019).
Liu, C., Wu, S. & Pan, X. Clustering of cardio-metabolic risk factors and pre-diabetes among U.S. adolescents. Sci. Rep. 11 (1), 5015 (2021).
Simental-Mendía, L. E., Rodríguez-Morán, M., Aradillas-García, C. & Guerrero-Romero, F. Hypertriglyceridemia is associated with impaired fasting glucose in normal-weight children. Pediatr. Res. 84 (3), 352–355 (2018).
Pedicelli, S. et al. Prevalence of prediabetes in children and adolescents by class of obesity. Pediatr. Obes. 17 (7), e12900 (2022).
Smetanina, N., Valickas, R., Vitkauskiene, A., Albertsson-Wikland, K. & Verkauskienė, R. Prevalence of metabolic syndrome and impaired glucose metabolism among 10- to 17-Year-old overweight and obese Lithuanian children and adolescents. Obes. Facts. 14 (3), 271–282 (2021).
Kloppenborg, J. T. et al. Impaired fasting glucose and the metabolic profile in Danish children and adolescents with normal weight, overweight, or obesity. Pediatr. Diabetes. 19 (3), 356–365 (2018).
Davidsson, L. et al. Intermediate hyperglycaemia, insulin resistance and metabolic syndrome among obese arab children (12–17 years old) in Kuwait. Prim. Care Diabetes. 15 (1), 191–193 (2021).
Phan, D. H., Do, V. V., Khuong, L. Q., Nguyen, H. T. & Minh, H. V. Prevalence of Diabetes and Prediabetes among Children Aged 11–14 Years Old in Vietnam. Journal of diabetes research 2020:7573491. (2020).
Eidkhani, V., Parizadeh, D., Hasheminia, M., Azizi, F. & Hadaegh, F. Impaired fasting glucose prevalence surge among Iranian adolescents in a decade: the Tehran lipid and glucose study. Pediatr. Diabetes. 20 (8), 1064–1071 (2019).
Peng, Y. F., Zhong, S. M. & Qin, Y. H. The relationship between major depressive disorder and glucose parameters: a cross-sectional study in a Chinese population. Adv. Clin. Experimental Medicine: Official Organ. Wroclaw Med. Univ. 26 (4), 665–669 (2017).
Wang, Q. et al. Metabolic characteristics, prevalence of anxiety and its influencing factors in first-episode and drug-naïve major depressive disorder patients with impaired fasting glucose. J. Affect. Disord. 324, 341–348 (2023).
Li, Y. et al. Prevalence and influencing factors of suicide in first-episode and drug-naive young major depressive disorder patients with impaired fasting glucose: a cross-sectional study. Front. Psychiatry. 14, 1171814 (2023).
Zhang, M., Chen, J., Yin, Z., Wang, L. & Peng, L. The association between depression and metabolic syndrome and its components: a bidirectional two-sample mendelian randomization study. Translational Psychiatry. 11 (1), 633 (2021).
Xu, H. et al. Prevalence and risk factors for abnormal glucose metabolism in first-episode and drug-naïve major depressive disorder outpatients with comorbid anxiety: a cross-sectional study from a large sample of the Chinese Han population. J. Affect. Disord. 349, 400–406 (2024).
Koponen, H., Kautiainen, H., Leppänen, E., Mäntyselkä, P. & Vanhala, M. Association between suicidal behaviour and impaired glucose metabolism in depressive disorders. BMC Psychiatry. 15, 163 (2015).
Salazar, M. R. et al. Relation among the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio, insulin resistance, and associated cardio-metabolic risk factors in men and women. Am. J. Cardiol. 109 (12), 1749–1753 (2012).
Song do, K., Lee, H., Sung, Y. A. & Oh, J. Y. Triglycerides to high-density lipoprotein cholesterol ratio can predict impaired glucose tolerance in Young women with polycystic ovary syndrome. Yonsei Med. J. 57 (6), 1404–1411 (2016).
Manco, M. et al. Triglycerides-to-HDL cholesterol ratio as screening tool for impaired glucose tolerance in obese children and adolescents. Acta Diabetol. 53 (3), 493–498 (2016).
Gong, R. et al. Associations of TG/HDL Ratio with the Risk of Prediabetes and Diabetes in Chinese Adults: A Chinese Population Cohort Study Based on Open Data. International journal of endocrinology 2021:9949579. (2021).
Garonzi, C., Maguolo, A. & Maffeis, C. Pros and cons of current diagnostic tools for risk-based screening of Prediabetes and Type 2 diabetes in children and adolescents with overweight or obesity. Hormone Res. Paediatrics. 96 (4), 356–365 (2023).
Furukawa, T. A. et al. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 6 (7), 601–609 (2019).
ElSayed, N. A. et al. 2. Classification and diagnosis of diabetes: standards of Care in Diabetes-2023. Diabetes care. 46 (Suppl 1), S19–s40 (2023).
Morrens, J. et al. Use of Clinical Global impressions-Severity (CGI-S) to assess response to antidepressant treatment in patients with treatment-resistant depression. Neuropsychiatr. Dis. Treat. 18, 1127–1132 (2022).
Lu, Q. et al. Prevalence of impaired fasting glucose and analysis of risk factors in Han adolescents. J. Diabetes Complicat. 24 (5), 320–324 (2010).
Zhang, J. et al. Prevalence of diabetes and impaired fasting glucose in Uygur children of Xinjiang, China. Genet. Mol. Research: GMR. 12 (4), 5007–5012 (2013).
Yan, W. L. et al. Overweight, high blood pressure and impaired fasting glucose in Uyghur, Han, and Kazakh Chinese children and adolescents. Ethn. Health. 20 (4), 365–375 (2015).
Wang, Z. et al. Prevalence and risk factors of impaired fasting glucose and diabetes among Chinese children and adolescents: a national observational study. Br. J. Nutr. 120 (7), 813–819 (2018).
Mengzi, S. et al. The cut-off value of impaired fasting glucose should be lower: based on the associations of fasting blood glucose with blood lipids. Prim. Care Diabetes. 14 (2), 147–153 (2020).
Zheng, J. et al. Gender differences in the relationship between plasma lipids and fasting plasma glucose in non-diabetic urban Chinese population: a cross-section study. Front. Med. 8 (4), 477–483 (2014).
Andes, L. J., Cheng, Y. J., Rolka, D. B., Gregg, E. W. & Imperatore, G. Prevalence of Prediabetes among adolescents and young adults in the United States, 2005–2016. JAMA Pediatr. 174 (2), e194498 (2020).
Ray, S. et al. Serum lipoprotein ratios as markers of insulin resistance: a study among non-diabetic acute coronary syndrome patients with impaired fasting glucose. Indian J. Med. Res. 141 (1), 62–67 (2015).
Brehm, A., Pfeiler, G., Pacini, G., Vierhapper, H. & Roden, M. Relationship between serum lipoprotein ratios and insulin resistance in obesity. Clin. Chem. 50 (12), 2316–2322 (2004).
Di Bonito, P. et al. One-hour post-load plasma glucose and altered glucometabolic Profile in youths with overweight or obesity. Int. J. Environ. Res. Public Health 20(11), 5961 (2023).
Di Bonito, P. et al. Impaired fasting glucose and impaired glucose tolerance in children and adolescents with overweight/obesity. J. Endocrinol. Investig. 40 (4), 409–416 (2017).
Tfayli, H., Lee, S. & Arslanian, S. Declining beta-cell function relative to insulin sensitivity with increasing fasting glucose levels in the nondiabetic range in children. Diabetes care. 33 (9), 2024–2030 (2010).
Hagman, E., Ek, A. E. & Marcus, C. Insulin function in obese children within the low and high ranges of impaired fasting glycemia. Pediatr. Diabetes. 20 (2), 160–165 (2019).
Shand, B. I., Scott, R. S., Lewis, J. G., Elder, P. A. & Frampton, C. M. Comparison of indices of insulin resistance with metabolic syndrome classifications to predict the development of impaired fasting glucose in overweight and obese subjects: a 3-year prospective study. Int. J. Obes. 33 (11), 1274–1279 (2009).
Coelho, S. G. et al. The association between depression and physiological markers of glucose homeostasis among adolescents. J. Psychosom. Res. 154, 110738 (2022).
Clark, E. L. M. et al. The role of mindfulness in associations among depression symptoms, sleep duration, and insulin resistance in adolescents. J. Behav. Med. 44 (5), 694–703 (2021).
Liu, Z. et al. The abnormalities of lipid metabolism in children and adolescents with major depressive disorder and relationship with suicidal ideation and attempted suicide. Heliyon. 10 (9), e30344 (2024).
Hagman, E. et al. Impaired fasting glucose prevalence in two nationwide cohorts of obese children and adolescents. Int. J. Obes. 38 (1), 40–45 (2014).
Acknowledgements
We are particularly thankful to the patients who agreed to participate in our study.
Funding
This study was funded by grants from the Scientific Research Project of Anhui Provincial Health Commission (No. AHWJ2021a035) and the Scientific Research Project of Fuyang Municipal Health Commission (No. FY2021-059, FY2023-069).
Author information
Authors and Affiliations
Contributions
Zhiwei Liu: Conceptualization, Formal analysis, Writing, Supervision – original draft. Liang Sun, Feng Sun, Shu Cui, Yulong Zhang, Zhaokun Zhang, Longlong Sun and Juan Wang: Investigation, Data curation. Rongchun Yang, Gaofeng Yao: Writing - review & editing. Yun Liu: Writing - review & editing, Supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures were conducted per the Declaration of Helsinki 1975 guidelines. Informed consent was obtained from participants and minor participants’ parents/legal guardians. The Medical Ethics Committee of the Third People’s Hospital of Fuyang approved this study.
Consent for publishing
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Z., Sun, L., Sun, F. et al. Prevalence and clinical correlates of impaired fasting blood glucose in children and adolescents with depressive disorder and relationship with triglyceride and high-density lipoprotein ratio. Sci Rep 14, 24112 (2024). https://doi.org/10.1038/s41598-024-76183-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-76183-6