Abstract
Although some studies have explored the role of meteorological factors in the development of tuberculosis (TB), the majority have been confined to single regions, leading to inconsistent findings. Consequently, we conducted a multi-city study not only to determine whether meteorological factors significantly influence the risk of developing TB but also to assess the magnitude of these effects and explore potential modifying factors. Data on daily reported TB cases and meteorological factors were collected from January 1, 2013, to December 31, 2022, across 11 cities in Zhejiang Province. A distributed lag non-linear model using a quasi-Poisson distribution was employed. Multivariate meta-regression was used to obtain overall pooled estimates and assess heterogeneity. From 2013 to 2022, 267,932 TB cases were reported in Zhejiang Province. Notably, a nonlinear relationship was observed between temperature and TB, with the relative risk (RR) peaking at 1.0 °C (RR = 1.882, 95% CI 1.173–3.020). The effect of low temperature was immediate and significant for a 13-day lag period, with the maximum effect at lag0 (RR = 1.014, 95% CI 1.008–1.021). The exposure-response curve between relative humidity (RH) and TB exhibited an M-shape, with the RR peaking at 47.7% (RR = 1.642, 95% CI 1.044–2.582). The lag effect of low RH was significant at lag 25–59, with the highest RR observed at lag 32 (RR = 1.011, 95% CI 1.001–1.022). Gross domestic product (GDP) per person, population density, and latitude demonstrated significant modification effects. Our study showed that low temperature and RH were associated with an increased risk of TB. Additionally, GDP per person, population density, and latitude may play important roles in explaining the association between RH and TB. These findings provide scientific evidence for the development of geographically specific public health policies.
Similar content being viewed by others
Introduction
Tuberculosis (TB) is a chronic infectious disease primarily caused by the inhalation of infectious aerosol particles containing Mycobacterium tuberculosis. It stands as one of the leading causes of death among infectious diseases and remains a major public health problem worldwide, particularly in low- and middle-income countries. China ranks third among the 30 countries with the highest TB burden, following India and Indonesia. Zhejiang Province, located in southeast China, has a relatively well-developed economy. Although the reported incidence of TB in Zhejiang Province fell below 40 per 100,000 population for the first time in 2022, over 22,000 cases and more than 80 deaths were reported.
Given that TB is an airborne disease, a growing body of epidemiology research over the past few decades has sought to determine the association between environmental factors and TB development. The first study in China reported an adverse effect of higher average temperatures on TB hospitalization1. Time-series analyses have since been employed to examine the effects of environmental exposures on a wide range of diseases. Existing time-series studies assessing the impact of meteorological factors on TB risk have yielded contradictory findings and have not explored potential risk modifiers in depth2,3,4. A seven-year time-series study in Beijing suggested a significant increase in excess risk of TB for every 0.1 m/s increase in wind speed over a 5-week lag period, alongside a significant decrease in excess risk for every 5 °C increase in temperature and 10% increase in relative humidity (RH) over a 10-week lag period2. In contrast, a study in Yingjisha County, Xinjiang found an increased risk of TB incidence with rising RH at a 7-day lag4. Another time-series study in Lanzhou suggested that daily reported TB cases were positively correlated with temperature and RH but negatively related to sunshine duration and wind speed3.
Research on TB and environmental epidemiology still faces limitations. Due to data availability, some existing studies are small sample studies conducted in particular counties or cities3,5,6,7. The research methodologies vary, being based on completely different analytical frameworks. Some descriptive studies directly analyze the relationship between environmental factors and health, ignoring the complexity and lagged effects of these factors8,9,10. Additionally, a subset of studies incorporates individual meteorological factors into statistical models without considering the role of other potential modifiers11,12. The application of a time-series approach based on a two-stage design for modeling multisite data was first proposed by Gasparrini et al.13. In view of these limitations, using a consistent analytical framework and expanding the study area urgently needs to provide new insights into the impact of meteorological factors on the risk of TB.
A time-series study showed that exposure to extreme temperatures can affect health for some time after its occurrence, indicating a lag effect on health14. Previous studies15,16 suggest that environmental factors and health events tend to show non-linear associations. Gasparrini et al. first proposed distributed lag non-linear models (DLNM) to describe the lag structure of non-linear exposure-response relationships and quantify the health effects17. The regression method of choice for analyzing count data is the Poisson regression18. When the outcome variable is overly dispersed, the quasi-Poisson regression method should be used instead. In this study, the number of TB cases reported per day is relatively small and dispersed, with a quasi-Poisson distribution. Therefore, quasi-Poisson regression in conjunction with the DLNM was applied to account for potential over-dispersion.
The present study aimed to quantitatively evaluate the association between multiple meteorological factors and TB through a two-stage time-series analysis in multiple cities while exploring potential modifying factors. In pursuit of this objective, we performed a two-stage time-series analysis using data collected from 11 cities within Zhejiang Province over the period from 2013 to 2022. Our findings are expected to significantly impact clinical practices by uncovering key insights into the relationship between meteorological factors and TB in Zhejiang Province.
Materials and methods
Study area and data collection
Zhejiang Province is located between 27°02′ to 31°11′ north latitude and 118° 01′ to 123° 10′ east longitude, featuring a subtropical monsoon climate. It encompasses 11 prefecture-level cities, covering a total area of 105,500 km2. As of the end of 2022, the total resident population of Zhejiang Province was approximately 65.77 million. Zhejiang Province is an important link in the Yangtze River Delta, with its per capita disposable income of urban residents and per capita disposable income of rural residents ranking first among all provinces (autonomous regions) for many consecutive years.
The number of confirmed TB cases reported daily in each city, spanning from January 1, 2013, to December 31, 2022, was obtained from the China National Notifiable Disease Surveillance System (NDSS). Meteorological data, including daily mean temperature (°C), RH (%), sunshine hours (h), and wind speed (m/s) from 2013 to 2022, were collected from the China Meteorological Data Service Center (http://data.cma.cn/). Demographic, socioeconomic, and medical resource variables were extracted from the Statistical Yearbooks of the Zhejiang Provincial Bureau of Statistics (https://tjj.zj.gov.cn/).
Statistical analysis
All the methods were carried out in accordance with relevant institutional guidelines and regulations. In the first-stage analysis, a distributed lag non-linear model using a quasi-Poisson distribution was adopted to assess the exposure-response relationships between several meteorological factors (ambient temperature, RH, sunshine duration and wind speed) and daily reported TB cases in each of the 11 cities.
The correlation between meteorological factors and air pollutants is typically evaluated through Spearman’s correlation analysis. In this study, to avoid collinearity between these meteorological factors, variables with strong correlations (r > 0.7) were excluded from the DLNM for analysis at the same time1 (Figure S1).
Taking ambient temperature as an example, the model can be expressed as follows:
where t represents the number of days, µt refers to the count of daily reported TB cases, and Holidayt is a binary indicator adjusting for public holidays. A variable representing the day of the week (DOW) was included to control for the week effect. DOW values range from 1 to 7, with 0 or 1 representing weekdays (Monday to Friday) and weekends (Saturday to Sunday), respectively. α predicts the effect of ambient temperature and ns() refers to the natural cubic spline. The optimal model parameters were selected by comparing the fit of different models, as indicated by the sum of quasi-Akaike information criteria (QAIC) (Table S1), and assessing the robustness of various exposure-response curves. Natural cubic splines with 2 degrees of freedom (df) and 3 df were employed to model the exposure-response relationship and lag-response relationships19. It has been reported that the average incubation period for TB is four to eight weeks, with about two months between symptom onset and diagnosis20. Therefore, the maximum lag time applied in this study was 60 days. A natural cubic spline of time ranging from 6 to 9 df per year, was applied. to control for long-term trends and seasonality. The ambient temperature or RH corresponding to the minimum relative risk (RR) for TB was set as the reference value during risk estimation.
After the first-stage analysis, cumulative exposure-response estimates were pooled using multivariate meta-regression. The intercept-only model in multivariate meta-regression was utilized to calculate the overall pooled estimates and assess heterogeneity. A single meta-predictor analysis was performed to further detect potential effect modifiers by integrating demographic, socioeconomic, medical resource variables, and geographic dimensions into the model separately and comparing them to the intercept-only model. Residual heterogeneity was assessed by Cochran’s Q test and quantified using I221. The statistical significance of predictors was determined using the Wald test.
All statistical analyses were conducted using R software (version 4.2.1) with the “dlnm” and “mvmeta” packages. Geographic maps were created using the ArcGIS software (version 10.2.1). A P-value of less than 0.05 in a two-tailed test was considered statistically significant.
Ethics approval
The study protocol was approved by the Institutional Review Board of the Zhejiang Provincial Center for Disease Control and Prevention (Approval No.2022-032-01). Since the aggregated data used in the study were from routine surveillance and did not involve personal information, the Institutional Review Board of Zhejiang Provincial Center for Disease Control and Prevention waived the requirement for informed consent.
Results
Descriptive statistics
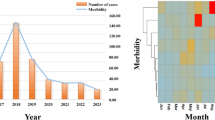
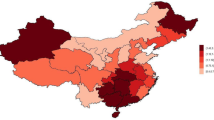
Between 2013 and 2022, a total of 267,932 cases of TB were reported across 11 cities in Zhejiang Province. As depicted in Fig. 1, the disease burden varied geographically, with the total number of TB cases ranging from 2,851 to 46,237. The central and western regions of the Zhejiang Province, such as Quzhou, Jinhua, and Lishui, had higher reported incidence rates. Of the 267,932 TB cases, 184,960 (69%) were males and 82,972 (31%) were females. In terms of age distribution, adults constituted the most prevalent group, accounting for nearly three-quarters of the reported TB cases (Table 1). The daily distribution of TB cases in Zhejiang Province showed clear cyclical and seasonal patterns, with higher incidence during the cold winter and spring seasons (Figure S2). Characteristics such as gross domestic product (GDP) per person (CNY), population density (persons/km2), resident population (10,000 persons), urbanization rate (%), licensed physicians (persons), and hospital beds (beds) are shown in Table S2.
Pooled estimates of meteorological factors and TB relationships
Figure 2 illustrates the exposure-response relationships between the four meteorological factors and TB. The overall pooled estimates revealed a nonlinear relationship between ambient temperature and TB. We found that the pooled RR of TB peaked at 1.0 °C (RR = 1.882, 95% CI 1.173–3.020), and was lowest at 29.4 °C. Similarly, a nonlinear relationship was observed between RH and TB, with the exposure-response curve showing an M-shape pattern. When RH was below 47.7%, the risk of TB progressively increased as RH rose, peaking at 47.7% (RR = 1.642, 95% CI 1.044–2.582) and reaching its the minimum RR at 73.9%. However, the exposure-response curves indicated that neither sunshine duration nor wind speed had a statistically significant effect on the risk of developing TB.
Predictor-specific summary associations at the 5th and 95th percentiles of meteorological factors
Using the point of minimum TB risk as a reference, the pooled estimates from the main model for predictor-specific summary associations at the 5th and 95th percentiles of temperature and RH are shown in Fig. 3. The estimated risk effect of low temperature was immediate and statistically significant for a 13-day lag period, peaking at lag0 (RR = 1.014, 95% CI 1.008–1.021). Conversely, high temperature was associated with a reduced risk of reported TB cases, reaching its minimum at lag 34 (RR = 0.975, 95% CI 0.966–0.984) (Fig. 3a). Regarding RH, the estimated lag effect of low RH (5th percentile, 52%) appeared to be significant at lags 25–59, with the highest RR at lag 32 (RR = 1.011, 95% CI 1.001–1.022). However, the lag relationship between high RH (95th percentile, 95%) and TB was not significant (Fig. 3b). Consistent with the exposure-response curve, the lag-response curves revealed that the effects of low and high sunshine duration and wind speed exposure on TB risk were not statistically significant (Figure S3).
Tests for heterogeneity and meta-regression
According to the random-effects meta-analysis (intercept-only), the results suggested that 32.03% and 37.88% of the variability were explained by true differences across the 11 cities (Table 2). For ambient temperature, city-level characteristics, including economic and demographic factors, medical resources, and geographic dimensions, showed no significant modification effects (All P values of Wald test > 0.05). For RH, multivariate meta-regression analyses indicated that GDP per person (P = 0.004), population density (P = 0.014), and latitude (P = 0.002) explained part of the heterogeneity, and the Cochran Q test for residual heterogeneity was insignificant (P > 0.05). Among the three meta-predictors, latitude explained the largest proportion of the heterogeneity, with the I2 statistic dropping to 23.16%.
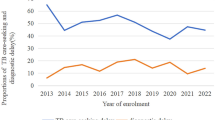
Meta-regression models were further fitted to predict associations between humidity and TB at the 25th and 75th percentiles of GDP per person, population density, and latitude. As shown in Fig. 4, higher GDP per person, population density, and latitude strongly reinforced the association between RH and TB. Zhejiang Province was divided into four regions to further validate the RH-TB association in different regions based on geographical locations. According to the region-specific curves, the pooled overall cumulative RRs in the northern and eastern regions were higher than those in the southern and western regions at an RH of 47.7%.
Discussion
Progress towards achieving the ‘End TB Strategy’ has not been sufficiently rapid, necessitating greater efforts at both national and global levels. A previous study found that incorporating meteorological factors into time-series models can improve their accuracy in predicting TB incidence22. In this study, we applied a multi-site, two-stage, time-series analysis to examine the relationship between meteorological factors and TB risk from 2013 to 2022 in Zhejiang Province. Our findings indicate that exposure to low ambient temperature and RH can acutely increase the risk of TB, while sunshine duration and wind speed do not significantly affect TB risk.
To date, an increasing number of studies have documented the important role of environmental factors in human respiratory health23,24,25,26,27. However, the precise relationship between various meteorological variables and disease risk remains unresolved. For instance, a systematic review found no significant correlation between temperature, humidity, sunshine duration, and TB risk28. Conversely, a time-series study in Lanzhou suggested that daily TB cases were positively related to maximum, minimum, and average temperatures, as well as RH, but negatively correlated with wind speed and sunshine duration3. Our results align with a time-series study conducted in Beijing (2014–2020), which showed that the lag effect of both average temperature and RH was negatively associated with the number of daily TB cases2. The inconsistencies across studies may be due to several factors. On the one hand, differences in statistical methods and models inevitably influence the conclusions drawn22. On the other hand, location-specific characteristics, such as the study area’s size and climatic conditions may modify the exposure-response relationship. For example, the Lanzhou study applied a stratification parametric model in an area with a temperate continental climate3, while our multi-city time-series study used a two-stage design for modeling multisite data and was conducted in a region with a subtropical monsoon climate.
Several studies have proposed potential biological mechanisms linking low ambient temperature to TB29,30,31,32. During the cold winter months, people, particularly older adults, and immunocompromised individuals tend to remain indoors extended long periods. This increases the risk of TB infection in crowded poorly ventilated environments once the bacteria are introduced29. Additionally, respiratory infections like influenza, which are more common in winter, can reduce immunity and potentially increase the risk of TB infection30,31. Evidence also links vitamin D levels to TB incidence32. Reduced outdoor activity and sunlight exposure during colder months may lead to decreased vitamin D synthesis, which could elevate the risk of TB29.
Previous studies have reported adverse effects of RH on respiratory health and proposed possible explanations2,33,34. One explanation is that lower RH leads to the evaporation of respiratory droplets, reducing their size and allowing them to travel further, thereby increasing the risk of transmission35. Therefore, dust, pollution particles, and pathogenic bacteria on the atmospheric surface may increase. Another possible explanation is that prolonged exposure to dry environments may reduce protective mucus production on the respiratory tract surface. Consequently, the resistance to growth of Mycobacterium tuberculosis is reduced36.
Additionally, our study indicated that GDP per person, population density, and latitude partially account for the heterogeneity in the association between RH and TB. Specifically, the moderating effects of these indicators were more pronounced at lower RH values. Among the three meta-predictors, latitude explained the largest proportion of the heterogeneity. The risk of TB in cities at higher latitudes was greater than in cities at lower latitudes, which aligns with a study conducted in Hefei, Anhui province7, where a higher TB risk was also observed in cities with greater latitudes. Upon further comparison, we noted that northern cities in Zhejiang Province, characterized by more accessible transportation and higher economic development, exhibited a correspondingly higher GDP per person and population density. A previous study investigated the spatiotemporal pattern of TB incidence found a negative correlation between GDP per person and TB incidence10. However, noting that this study analyzed the impact of meteorological and economic factors on TB risk separately, using incidence as the dependent variable, which differs from our study, is important. Additionally, Huang et al. did not find significant modifying effects of GDP per person on the association between RH and TB admissions7. Hence, further empirical investigations are warranted to better understand the role of economic and demographic factors in the lag-response relationship between RH and TB.
The present study has several limitations. First, time-series analyses and ecological studies, are inherently prone to ecological fallacies. Since the exposure-response associations were explored at the population level, making causal inferences may be limited. Second, other important city-specific characteristics such as greenness, local TB prevention and intervention measures and individual factors that were not covered in this study, due to data accessibility limitations, these should be considered in future research. Third, spatial autocorrelation is an issue that should be accounted for when pooling estimates from multiple cities. However, the impact of spatial autocorrelation may not significantly affected the main findings.
Despite these limitations, the strengths of this study should be acknowledged. Firstly, most time-series studies are conducted in a single city or over a short period1. In contrast, the present study was based on an extensive dataset from 11 cities in eastern China over the past 10 years, allowing for a more comprehensive assessment of the impact of meteorological factors on TB. Second, we full fully accounted for the non-linear associations and lag effects of meteorological factors using the two-stage time-series analysis, thereby improving the statistical effectiveness of the overall analysis. Third, while most previous studies collected daily records of TB hospitalizations from local hospitals7,37, we used daily rather than weekly reported TB cases derived from the NDSS, ensuring completeness and reliability. Fourth, we further assessed the region-specific association between RH and TB by comparing pooled overall cumulative RRs for TB.
In conclusion, low ambient temperature and exposure to RH have acute effects on the risk of TB in Zhejiang Province. GDP per person, population density, and latitude may partially explain the heterogeneity in the association between RH and TB. Our findings not only enhance the understanding of how meteorological variables influence the spread of TB but also provide valuable insights for developing public health intervention strategies. In the future, prospective studies that incorporate more regions and relevant environmental factors will be necessary to validate these findings and explore potential regulatory mechanisms.
Data availability
The data are available from the corresponding author upon reasonable request.
References
Tian, L. et al. Spatial patterns and effects of air pollution and meteorological factors on hospitalization for chronic lung diseases in Beijing, China. Sci. China Life Sci. 62(10), 1381–1388 (2019).
Sun, S. et al. The association between air pollutants, meteorological factors and tuberculosis cases in Beijing, China: a seven-year time series study. Environ. Res. 216(Pt 2), 114581 (2023).
Niu, Z. et al. Short-term effects of ambient air pollution and meteorological factors on tuberculosis in semi-arid area, northwest China: a case study in Lanzhou. Environ. Sci. Pollut Res. Int. 28 (48), 69190–69199 (2021).
Chang, M. et al. An investigation of the effects of meteorological factors on the incidence of tuberculosis. Sci. Rep. 14 (1), p2088 (2024).
Xu, M. et al. Temperature and humidity associated with increases in Tuberculosis notifications: a time-series study in Hong Kong. Epidemiol. Infect. 149, e8 (2020).
Nie, Y. et al. Effects and Interaction of Meteorological Factors on pulmonary tuberculosis in Urumqi, China, 2013–2019. Front. Public. Health. 10, 951578 (2022).
Huang, K. et al. Short-term effect of ambient temperature change on the risk of tuberculosis admissions: assessments of two exposure metrics. Environ. Res. 189, 109900 (2020).
Li, H., Ge, M. & Zhang, M. Spatio-temporal distribution of tuberculosis and the effects of environmental factors in China. BMC Infect. Dis. 22(1), 565 (2022).
Zhang, X. et al. Effect of meteorological factors on incidence of tuberculosis: a 15-year retrospective study based on Chinese medicine theory of five circuits and six qi. Chin. J. Integr. Med. 21 (10), 751–758 (2015).
Guo, C. et al. Spatiotemporal analysis of tuberculosis incidence and its associated factors in mainland China. Epidemiol. Infect. 145(12), 2510–2519 (2017).
Balcells, M. E. et al. Regional solar radiation is inversely correlated with incidence and severity of tuberculosis in Chile. Epidemiol. Infect. 145(9), 1815–1823 (2017).
Kirolos, A. et al. Tuberculosis case notifications in Malawi have strong seasonal and weather-related trends. Sci. Rep. 11(1), 4621 (2021).
Sera, F. & Gasparrini, A. Extended two-stage designs for environmental research. Environ. Health. 21(1), 41 (2022).
Braga, A. L., Zanobetti, A. & Schwartz, J. The time course of weather-related deaths. Epidemiology. 12 (6), 662–667 (2001).
Wu, Q. et al. Association between traffic-related air pollution and hospital readmissions for rheumatoid arthritis in Hefei, China: a time-series study. Environ. Pollut. 268(Pt A), p115628 (2021).
Gasparrini, A. & Armstrong, B. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med. Res. Methodol. 13, 1 (2013).
Gasparrini, A., Armstrong, B. & Kenward, M. G. Distributed lag non-linear models. Stat. Med. 29(21), 2224–2234 (2010).
Bhaskaran, K. et al. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 42(4), 1187–1195 (2013).
Zhu, S. et al. Ambient air pollutants are associated with newly diagnosed tuberculosis: a time-series study in Chengdu, China. Sci. Total Environ. 631-632, 47–55 (2018).
Li, X. X. et al. Seasonal variations in notification of active tuberculosis cases in China, 2005–2012. PLoS One. 8(7), e68102 (2013).
Gasparrini, A., Armstrong, B. & Kenward, M. G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 31 (29), 3821–3839 (2012).
Li, Z. Q. et al. Comparing the performance of time series models with or without meteorological factors in predicting incident pulmonary tuberculosis in eastern China. Infect. Dis. Poverty. 9 (1), 151 (2020).
Szyszkowicz, M. et al. Air pollution and emergency department visits for respiratory diseases: a multi-city case crossover study. Environ. Res. 163, 263–269 (2018).
Jia, H. et al. Ambient air pollution, temperature and hospital admissions due to respiratory diseases in a cold, industrial city. J. Glob Health. 12, 04085 (2022).
Tao, Y. et al. Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ. Pollut. 185, 196–201 (2014).
Zhao, Y. et al. Morbidity burden of respiratory diseases attributable to ambient temperature: a case study in a subtropical city in China. Environ. Health. 18(1), 89 (2019).
Sun, S. et al. Seasonal temperature variability and emergency hospital admissions for respiratory diseases: a population-based cohort study. Thorax. 73(10), 951–958 (2018).
Qin, T. et al. Association between averaged meteorological factors and tuberculosis risk: a systematic review and meta-analysis. Environ. Res. 212 (Pt D), 113279 (2022).
Fares, A. Seasonality of tuberculosis. J. Glob. Infect. Dis. 3(1), 46–55 (2011).
Guo, Z. et al. Epidemiological characteristics of pulmonary tuberculosis in mainland China from 2004 to 2015: a model-based analysis. BMC Public. Health. 19 (1), 219 (2019).
Wang, W. et al. Epidemiological characteristics of tuberculosis and effects of meteorological factors and air pollutants on tuberculosis in Shijiazhuang, China: a distribution lag non-linear analysis. Environ. Res. 195, 110310 (2021).
Naranbat, N. et al. Seasonality of tuberculosis in an eastern-asian country with an extreme continental climate. Eur. Respir J. 34(4), 921–925 (2009).
Li, Z. et al. Meteorological factors contribute to the risk of pulmonary tuberculosis: a multicenter study in eastern China. Sci. Total Environ. 793, 148621 (2021).
Xiao, Y. et al. The influence of meteorological factors on tuberculosis incidence in Southwest China from 2006 to 2015. Sci. Rep. 8(1), 10053 (2018).
Liu, L. et al. Evaporation and dispersion of respiratory droplets from coughing. Indoor Air. 27(1), 179–190 (2017).
Fahy, J. V. & Dickey, B. F. Airway mucus function and dysfunction. N Engl. J. Med. 363(23), 2233–2247 (2010).
Chong, K. C. et al. Independent effect of weather, air pollutants, and seasonal influenza on risk of tuberculosis hospitalization: an analysis of 22-year hospital admission data. Sci. Total Environ. 837, 155711 (2022).
Funding
This study was supported by the National Zhejiang Health Commission Major S&T Project (grant no. WKJ-ZJ-2118) and the Zhejiang Province Soft Science Research Program (2024C35082).
Author information
Authors and Affiliations
Contributions
B.C. and S.C. conceptualized the study. Q.W. conducted data analysis and edited the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, Q., Wang, W., Liu, K. et al. Effects of meteorological factors on tuberculosis and potential modifiers in Zhejiang Province, China. Sci Rep 14, 25430 (2024). https://doi.org/10.1038/s41598-024-76785-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-76785-0