Abstract
To examine the clinical effect of different conservative therapies (Glisson traction, soft and rigid cervical collar) in the treatment of children with acute atlantoaxial rotatory subluxation. One hundred and forty-four children with acute atlantoaxial rotatory subluxation treated conservatively at our hospital from June 2017 to June 2022 were retrospectively analyzed. The children were divided into three groups consisting of patients treated with Glisson traction (n = 37), patients treated with soft cervical collar (n = 55), and patients treated with rigid cervical collar (n = 52). Clinical and functional results were compared among the three groups. Success outcomes were achieved at the end of treatment in the Glisson traction group (94.59%, 35/37), soft cervical collar group (83.64%, 46/55), and rigid cervical collar group (92.31%, 48/52). There was no significant difference between the success rates among the three groups (P > 0.05). At the last follow-up, the overall scores based on our scoring scale for the Glisson traction, soft cervical collar and rigid cervical collar groups were 95.95 ± 6.11 (range: 75–100), 94.64 ± 6.30 (range: 75–100) and 95.00 ± 6.02 (range: 70–100), respectively. There was no significant difference in the overall scores among the three groups (P > 0.05). All three conservative therapies for the treatment of acute atlantoaxial rotatory subluxation can attain a good clinical outcome. Treatment using a cervical collar should be given priority as it does not require the child to be hospitalized. Rigid cervical collar provides good immobilization and can possibly lead to better clinical outcomes compared to a soft cervical collar.
Similar content being viewed by others
Introduction
Atlantoaxial rotatory subluxation (AARS) is a common cervical spine condition that typically present with painful torticollis in children1,2,3. It can occur due to trauma, infection of the pharyngeal space (Grisel syndrome), or originate from no precipitating event1,2,3,4. Due to the complex anatomy and unique biomechanical properties of the atlantoaxial joint, it can be challenging to diagnose and to treat diseases of this joint correctly and promptly4.
It is well accepted that most cases of AARS can be successfully treated by conservative therapy3,5,6. However, there have been relatively few studies in the literature on the use of conservative treatments and the evidence for conservative treatment of AARS is poor3,7. Cervical traction and cervical collars are two frequently used treatment methods, but the optimal treatment method between the use of collar or traction remains controversial. Masoudi et al. (2017) believed that traction was the primary treatment for AARS in children8. In his study, he specifically designed a simple and easy-to-use traction device for primary health care centers and underdeveloped regions. On the other hand, some surgeons believed that cervical collars may be more appropriate for AARS, especially in children with early stage AARS3,4,5,7,8. For example, Neal et al. (2015) and Spinnato et al. (2021) stated that acute cases of AARS were more commonly treated with cervical collars5,9. Powell et al. (2017) published a multi-center study in America on the treatment of AARS in children among 17 hospitals2. About one-third of the children were treated with traction, and the rest were treated with soft or rigid cervical collars and halo immobilization. The authors stated that significant institutional and surgeon variation exists in the use of collars, traction, and halo immobilization, preventing any meaningful conclusions regarding non-operative management, thus showing the lack of data and confusion on AARS treatment.
The objective of our study was to retrospectively evaluated and compare the clinical outcomes, including cure rate, curative time, and complications in AARS patients treated with traction or cervical collar. We further compared the clinical outcomes within the collar group between soft and rigid (skull-neck-thorax orthoses) collars.
Methods
Ethical approval
This study was approved by the Ethics Review Committee of Children’s Hospital Affiliated to Zhengzhou University (No. 2023-K142). Informed consent was waived by the Ethics Review Committee of Children’s Hospital Affiliated to Zhengzhou University as this was a retrospective study. The study was conducted following the ethical principles of the Declaration of Helsinki.
Participants
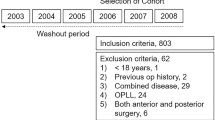
The inclusion criteria consisted of: (1) patients with Fielding classification type I and II10; (2) the presence of neck pain, torticollis, and/or limited range of motion of the cervical spine with symptoms of less than 2 weeks; (3) patient who have not received any prior treatment; (4) A cervical spine CT that indicates: Atlantodental Interval (ADI) < 5 mm and variance of bilateral lateral atlantodental space (VBLADS) > 2 mm; and (5) a follow-up period up to at least one year.
The exclusion criteria consisted of: (1) patients with combined fractures or disease in the cervical region affecting the atlanto-axial joint rehabilitation; (2) cases with congenital abnormality of the cervical vertebra; (3) patients who fail to adhere to medical advice and treatment due to various reasons (adherence to the treatment protocol in this study was defined as wearing the collar or undergoing traction for > 20 h per day); (4) lack of follow-up information; and (5) Patients less than 3 years old were excluded to minimize the imaging measurement error.
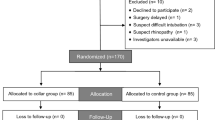
On the basis of aforementioned inclusion and exclusion criteria, data from 144 pediatric patients with acute AARS were identified through our hospital database from June 2017 to June 2022. Patients were divided into a Glisson traction group (n = 37) that received Glisson traction therapy, a soft cervical collar group (n = 55) that received soft cervical collar therapy, and a rigid cervical collar group (n = 52) that received rigid cervical collar therapy.
Treatment paradigm
-
1.
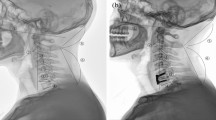
Glisson traction group (Fig. 1a): Hospitalized patients (a small number of patients received traction at home by themselves) used a neutral position cervical traction with a headrest strap, and the head of the bed was elevated by 15 degrees. The initial traction weight was 1 kg, which was increased by 0.5 kg daily or every other day, based on the patient’s adaptability. The maximum traction weight was 10–15% of the child’s body weight. Aside from eating or using the restroom, traction was maintained as much as possible. Cervical spine CT or open-mouth X-ray was reviewed every week. Traction duration was at least 2 weeks. After discharge, wearing a soft cervical collar for 1–2 weeks was recommended.
-
2.
Soft collar group (Fig. 1b): Outpatients were advised to wear a soft collar for 24 h a day outside the hospital. Clinical symptoms and radiographic images were assessed in the outpatient department every one or two weeks. The duration for wearing the collar was typically 1 to 3 weeks.
-
3.
Rigid collar group (Fig. 1c): Outpatients were advised to wear a rigid collar for 24 h a day outside the hospital. Clinical symptoms and radiographic images were assessed in the outpatient department every one or two weeks. When initially wearing the collar, the child’s neck could be properly straightened about 10–15 degrees, and the angle of the collar could be adjusted. Parents were advised that they could gradually adjust the neck brace every 3–5 days until the child’s neck returned to a neutral position. Clinical symptoms and radiographs could be re-examined in the outpatient department every week. The duration of wearing the collar was typically 1 to 4 weeks.
Data collection and outcome indicators
Data collected from the patients included age, sex, cause of disease, Fielding type, time from onset to the treatment, follow-up time, duration of treatment, complications, and treatment outcome. According to the Regulations for the Diagnosis and Therapeutic Efficacy of Traditional Chinese Medicine in the Industry Standards of Traditional Chinese Medicine of the People’s Republic of China (ISTPRC), the treatment outcome criteria were as follows11:
-
1)
Excellent: Clinical symptoms disappear and radiographs show a central position of the odontoid process. VBLADS is 0.
-
2)
Good: Clinical symptoms disappear and the radiographs show asymmetry of the odontoid process, but VBLADS < 2 mm.
-
3)
Fine: Clinical symptoms disappear or significantly alleviate and radiographs show asymmetry of the odontoid process, but the VBLADS value is greater than or equal to 2 mm.
-
4)
Poor: No obvious improvement in clinical symptoms and in radiographic images. Excellent, good, and fine were defined as a successful treatment at the end of treatment.
Outcome indicators also included (outcomes with measurements were evaluated by two orthopaedists independently and the average measurement was used for statistical analysis):
-
1.
VBLADS (Fig. 2a, b, d and e): Pre-treatment, post-treatment, and radiographs such as CT or X-ray were conducted to measure the difference (absolute value) in the distance between the midpoint of the odontoid process and the bilateral masses of the atlas vertebra.
-
2.
ADI (Fig. 2c and f): Pre-treatment, post-treatment, imaging tests such as CT or X-ray were conducted. On sagittal scan, a horizontal line was drawn between the posterior arch of the atlas and the anterior edge of the dens, measuring the maximum distance between these two lines, which represents the distance between the posterior arch of the atlas and the anterior edge of the dens.
-
3.
A more commonly used cervical spondylosis scoring tables for adults consists of the cervical vertebrae Japanese Orthopaedic Association Score12. We found that this score was not very suitable for children with AARS and did not find any other suitable evaluation criteria. Based on the clinical characteristics of children with AARS, we designed a scoring scale ourselves and measured it at the last follow-up. Our scoring scale, the Zhengzhou Cervical Vertebrae Scoring Scale (ZCVSS) in Table 1, consisted of appearance (25 points), pain (30 points), range of motion (25 points), neurological symptoms (10 points) and poor habitual neck movements (15 points). Higher scores out of 100 indicated better neck function and scores were categorized into excellent (90–100), good (75–89), fair (60–74), and poor (0–59).
Statistical analysis
The Shapiro-Wilk test was used to determine the normality of the data. Non-parametric results were analyzed using the Kruskal-Wallis test by ranks. The Dunn’s test was used to conduct pairwise multiple comparisons based on rank sums upon rejection of the null hypothesis from the Kruskal-Wallis test. Categorical data was assessed using the Chi-square test upon confirming that the data satisfied the appropriate assumptions. In cases where the Chi-square assumptions were not met, bootstrapping was used with 1000 samples and a confidence level of 95%. Ordinal regression was used for a subgroup analysis to determine whether age, sex, type, treatment type, and severity of initial injury (ADI, VBLADS) had an effect on the treatment outcome (poor, fine, good, excellent). The data was analyzed in Graphpad Prism 9.0 or SPSS Statistics 22.
Results
Patient characteristics
Baseline characteristics are listed in Table 2. The Glisson traction group consisted of 22 males and 15 females with a mean age of 5.12 ± 1.66 years old (range: 3.1–10.3 years old), mean time from onset of symptom to treatment of 4.56 ± 3.17 days (range, 1–13 days). The soft cervical collar group consisted of 31 males and 24 females with a mean age of 4.95 ± 1.72 years old (range: 3–11 years old), mean time from onset of symptom to treatment of 3.91 ± 2.90 days (range: 1–13 days). The rigid cervical collar group consisted of 30 males and 22 females with a mean age of 5.32 ± 1.54 years old (range: 3.3–11 years old), mean time from onset of symptom to treatment of 3.83 ± 3.03 days (range: 1–14 days). The Glisson traction group had 32 (86.5%) and 5 (13.5%) cases of Fielding classification type I and II, respectively. The soft cervical collar group had 47 (85.5%) and 8 (14.5%) cases of Fielding classification type I and II, respectively. The rigid cervical collar group had 43 (82.7%) and 9 (17.3%) cases of Fielding classification type I and II, respectively. There were no significant differences between baseline characteristics among the three groups (P > 0.05). Ordinal regression showed no relationship between age, sex, type, treatment type, and severity of initial injury when compared to treatment outcomes. The model predicted that all cases had successful outcomes, thus yielding false positives in unsuccessful cases.
Radiological results
Radiological results are displayed in Table 3. The VBLADS at the end of treatment for the Glisson traction, soft cervical collar and rigid cervical collar group was 0.61 ± 0.81 (range: 0–2.5 mm), 0.97 ± 1.11 (range: 0–3.2 mm), 0.67 ± 0.97 (range: 0–3.6 mm), respectively. The ADI at the end of treatment for the Glisson traction, soft cervical collar and rigid cervical collar group was 2.53 ± 0.57 (range: 1.5–4.0 mm), 2.63 ± 0.40 (range: 1.7–4.3 mm), 2.68 ± 0.51 (range: 1.5–4.2 mm), respectively. One-way ANOVA showed no significant differences between the three groups (P > 0.05).
Clinical outcomes
At the end of treatment, according to the Industry Standards of Traditional Chinese Medicine of the People’s Republic of China. The Glisson traction group had 18 excellent, 15 good, 2 fair outcomes, and 2 poor outcomes, with an overall success rate of 94.59%. The soft cervical collar group had 21 excellent, 21 good, 4 fair, and 9 poor outcomes, with an overall success rate of 83.64%. The rigid cervical collar group had 23 excellent, 20 good, 5 fair, and 4 poor outcomes, with an overall success rate of 92.31%. There were no significant differences in success rate among the three groups.
In the Glisson traction group, one of the two patients who did not improve after traction was transferred to a superior hospital and received screw fixation surgery. The other patient went to a hospital of traditional Chinese medicine and underwent manual reduction. Eight of the thirteen patients with poor outcomes and two patients with fair outcomes in the soft and rigid collar groups were admitted in our hospital and received Glisson traction therapy. Among these patients, eight showed improvement. The remaining patients with poor outcomes underwent manual reduction based on traditional Chinese medicine or surgery. There was one recurrence in each of the Glisson traction and soft collar group, both of whom were immobilized with a rigid collar, upon which they later showed improvement.
At the last follow-up, our scoring scale for the Glisson traction, soft collar and rigid collar groups were 95.95 ± 6.11 (range: 75–100), 94.63 ± 6.30 (range: 75–100), 95.00 ± 6.02 (range: 70–100), respectively. There were no significant differences in the scores between the three groups (P > 0.05). Jittered box and whisker plots for VBLADS, ADI, overall score (ZCVSS) and duration of treatment are shown in Fig. 3 with 10–90 percentiles at the whiskers and 25–75 percentiles at the boxes.
Discussion
Although it has been shown that most pediatric cases of AARS can be successfully treated by conservative therapy, there is a paucity of literature and less consensus regarding the optimal management of AARS in this age group. To the best of our knowledge, this is the first study in literature that directly compares three different conservative therapies in patients with AARS.
In this study, the vast majority of patients corresponded to Fielding and Hawkins type I AARS. Similar distributions were documented in other published studies3,5,9,13. Neal et al. (2015) noted that most cases of AARS seen in children would correspond to Fielding and Hawkins type I5. The authors also rationalized that the term AARS was more suitable for cases involving Fielding and Hawkins type I and II, whereas the much more severe types III and IV can be categorized as distinct entities from AARS and considered to be major cervical spine dislocations.
A total of 144 cases of AARS children were included in this study. Conservative treatments including traction, soft cervical collar, and rigid cervical collar were applied. All three groups of patients achieved good therapeutic effects, with overall success rates of 94.59%, 83.64% and 92.31%, respectively. The success rates of Groups A and C were higher than that of Group B, however, these differences were not statistically significant. Shimazaki et al. (2020) conducted a study to investigate the ideal primary treatment for AARS, examining the efficacy of traction and cervical collars3. Their success rate (97.3%) in the use of traction was similar to the success rate (94.59%) observed in our study. The authors did not analyze the underlying reasons for their high rate of success when using traction, but we noticed some commonalities between our studies. First, all of our patients consisted of Fielding and Hawkins Type I and Type II, with the majority being Type I. Second, for both groups undergoing traction therapy, continuous traction was preferentially used instead of partial or intermittent traction on a daily basis.
Glisson traction is considered a highly successful and useful conservative therapy for AARS. However, its popularity may be in part due to a lack of researchers attempting to explain the treatment mechanism of atlantoaxial subluxation using cervical collars, leading to clinicians opting to use Glisson traction. Yet, in the clinical practice, there is a higher level of difficulty in using Glisson traction compared to a cervical collar. Glisson traction requires the child to maintain continuous traction in order to stabilize the cervical spine as much as possible. This condition can be nonideal due to various difficulties. Children who have poor compliance with traction commonly exhibit frequent left and right movements of the neck. Additionally, daily activities such as eating or using restroom often interrupts the traction treatment, which to some extent, affects its effectiveness and causes anxiety among the child’s parents. Due to the need for hospitalization during traction therapy, parents also need to take time off their work to accompany the child. Parents also often worry about traction therapy being interrupted by the child dining or using restroom, which may affect the treatment’s effectiveness, thereby causing anxiety.
Several studies have supported the use of cervical collars as a safe and effective means of treating AARS3,14,15. Beier et al. (2012) reported 21 out of 22 patients with acute AARS who achieved good reduction using conservative treatment with a collar14. Shimazaki’s study found that 88 patients had wore cervical collars as an initial treatment and demonstrated that the success rate was 68.2%3. Despite the relatively low success rate, the remaining 28 patients who had poor outcomes with a cervical collar were then transitioned to Glisson traction and 27 of these patients showed improvement. The authors thus believed that cervical collar fixation while monitoring the patient’s progress can be considered as an initial treatment for AARS, especially for patients with Fielding classification type I at an early stage after onset.
However, the choice between a soft or rigid cervical collar still remains unclear. To our knowledge, only one previous study attempted to evaluate the efficacy of different cervical immobilization devices. Ciaran et al. (2021) observed 33 AARS cases with an average delay time of 2 months after the onset of symptoms, where 19 of their patients were treated with a rigid collar and 14 patients were treated with halo-body orthosis7. Although no statistically significant differences were found, the authors believed that immobilization with a rigid collar after manipulation under anaesthesia was a reasonable treatment option.
In our study, the success rates in using soft or rigid cervical collars were 83.64% and 92.31%, respectively. Rigid cervical collars appear to have a higher success rate than soft collars, however, there was no statistically significant difference in the success rates between the two types of cervical collars. One possible reason for this circumstance may be due to a small sample size. Additionally, based on our experience using these two collars, we noticed some differences between the use of soft and rigid collars. The material of the soft collar is relatively soft, and its coverage area is just around the neck. Its main function when worn is to support the head, which has a limited effect on immobilizing the neck. Children tend to be more active when they are not in pain. Thus, after wearing the collar for a few days and experiencing reduced pain, the children tended to start moving their necks. This activity may affect the effectiveness of the collar, leading to a decreased success rate. In contrast, a rigid collar provides firm immobilization and restricts the movement of the child’s neck, which might be helpful for the gradual reduction of AARS. In addition, we have also made some exploration on the wearing time of the collars. In our department, hospitalization and traction treatment were generally recommended for children who did not show improvement after wearing the soft collar for two weeks. Whereas for children wearing the rigid collar, it was often advised to continue wearing it, even up to more than a month.
Our study has several limitations. First, it was a retrospective, cohort study. Second, when the patient was initially diagnosed, we used CT scans whereas for post-treatment and follow-up examinations, we usually used open-mouth X-rays. Due to radiation concerns, most parents were unwilling to undergo CT scans at the end of treatment. The inconsistency between these two imaging techniques may have an impact on our imaging results. Future works that use consistent imaging methods, preferably CT scans, may be more accurate for measuring baseline and post-treatment outcomes. Third, we set the imaging criteria for the diagnosis of AARS as VBLADS > 2 mm, whereas some studies have set this threshold to be VBLADS > 1 mm or VBLADS > 2.2mm16,17. Similar to the controversies surrounding the nomenclature, pathogenesis and treatment of AARS4,5,9, there is still no gold standard for the diagnostic imaging criteria. Multiple studies have shown that there are variations in the Lateral Atlanto-Dental Space (LADS) among normal populations18,19,20,21,22, with some researchers suggesting a prevalence of up to 56%22. Moreover, from an anatomical perspective, the structure of the atlas and axis resembles a bearing with an elliptical housing for a circular shaft. When the head deviates to one side, physiological asymmetry of LADS can exist, further increasing the uncertainty of imaging diagnostic criteria. Considering that the atlantoaxial joint is the most flexible joint of the body, pediatric cervical vertebra and its surrounding ligaments are still developing and need to support a relatively larger and heavier head compared to the body. Under these circumstances, we probably should not be overly concerned with what the exact value of VBLADS is considered normal or abnormal in imaging. The diagnosis of AARS should be decided by combining the patient’s medical history and physical examination along with medical imaging that shows unequal VBLADS. From this perspective, we agree with Pang and Li’s (2004) viewpoint that any departure from the normal rotational relationship of the atlantoaxial complex is defined as AARS23.
In conclusion, Glisson traction and cervical collars are both suitable conservative therapies for the treatment of children with acute AARS. Successful treatment of AARS was achieved using Glisson traction (94.59%, 35/37), soft cervical collars (83.64%, 46/55), and rigid cervical collars (92.31%, 48/52). Our scoring scale at the last follow-up, also yielded excellent mean results for the use of Glisson traction (95.95 ± 6.11), soft cervical collars (94.64 ± 6.30) and rigid cervical collars (95.00 ± 6.02). We recommend the use of cervical collars as an initial treatment option since it does not require the child to be hospitalized. Rigid (skull-neck-thorax orthoses) cervical collars could be a more preferential for immobilization and can possibly lead to better clinical results given that it had a 9% higher success rate compared to soft collars, albeit the different was not statistically significant. Future works should consist of prospective randomized controlled trials with a larger sample size that analyzes the difference between cervical collars and traction for the treatment of AARS.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Jeszenszky, D., Fekete, T., Kleinstuck, F., Haschtmann, D. & Loibl, M. Transoral closed reduction of fixed atlanto-axial rotatory-subluxation (AARS) in Childhood and Adolescence. Clin. Spine Surg. 31, E252–E256. https://doi.org/10.1097/BSD.0000000000000563 (2018).
Powell, E. C. et al. Atlantoaxial Rotatory Subluxation in Children. Pediatr. Emerg. Care 33, 86–91. https://doi.org/10.1097/PEC.0000000000001023 (2017).
Shimazaki, T. et al. Primary treatment of atlantoaxial rotatory fixation in children: a multicenter, retrospective series of 125 cases. J. Neurosurg. Spine 34, 498–505. https://doi.org/10.3171/2020.7.SPINE20183 (2020).
Yeung, C. Y. & Feng, C. K. Halter Traction for the treatment of atlantoaxial rotatory fixation. J. Bone Joint Surg. Am. 104, 229–238. https://doi.org/10.2106/JBJS.21.00831 (2022).
Neal, K. M. & Mohamed, A. S. Atlantoaxial rotatory subluxation in children. J. Am. Acad. Orthop. Surg. 23, 382–392. https://doi.org/10.5435/JAAOS-D-14-00115 (2015).
Xu, P. et al. Successful closed reduction of atlantoaxial rotatory fixation in Children-A Retrospective Study of 30 patients. Global Spine J. 12, 1655–1660. https://doi.org/10.1177/2192568220984427 (2022).
Hill, C. S., Borg, A., Tahir, M. Z. & Thompson, D. N. P. Atlantoaxial rotatory fixation in childhood: a staged management strategy incorporating manipulation under anaesthesia. Childs Nerv. Syst. 37, 167–175. https://doi.org/10.1007/s00381-020-04727-y (2021).
Masoudi, M. S., Derakhshan, N., Ghaffarpasand, F. & Sadeghpour, T. Management of Pediatric Atlantoaxial Rotatory Subluxation with a simple handmade cervical traction device: doing more with less. World Neurosurg. 106, 355–358. https://doi.org/10.1016/j.wneu.2017.06.177 (2017).
Spinnato, P. et al. Atlantoaxial rotatory subluxation/fixation and Grisel’s syndrome in children: clinical and radiological prognostic factors. Eur. J. Pediatr. 180, 441–447. https://doi.org/10.1007/s00431-020-03836-9 (2021).
Fielding, J. W. & Hawkins, R. J. Atlanto-axial rotatory fixation. (fixed rotatory subluxation of the atlanto-axial joint). J. Bone Joint Surg. Am. 59, 37–44 (1977).
Regulations for the Diagnosis and Therapeutic Efficacy of Traditional Chinese Medicine. Diseases and Syndromes (Industry Standards of Traditional Chinese Medicine of the People’s Republic of China). 48 (State Administration of Traditional Chinese Medicine in China, 2012).
Tetreault, L. et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur. Spine J. 26, 78–84. https://doi.org/10.1007/s00586-016-4660-8 (2017).
Pang, D. & Li, V. Atlantoaxial rotatory fixation: part 2–new diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging. Neurosurgery57, 941–953. https://doi.org/10.1227/01.neu.0000181309.13211.3a (2005) (discussion 941–953).
Beier, A. D. et al. Rotatory subluxation: experience from the hospital for Sick Children. J. Neurosurg. Pediatr. 9, 144–148. https://doi.org/10.3171/2011.11.PEDS11147 (2012).
Landi, A., Pietrantonio, A., Marotta, N., Mancarella, C. & Delfini, R. Atlantoaxial rotatory dislocation (AARD) in pediatric age: MRI study on conservative treatment with Philadelphia collar–experience of nine consecutive cases. Eur. Spine J. 21(Suppl 1), S94-99. https://doi.org/10.1007/s00586-012-2216-0 (2012).
Lu, T., Wei, N., Zhou, Y. & Xu, H. B. [Traumatic Atlantoaxail Rotatory Subluxation in Children]. J. Appl. Clin. Pediatr. 27, 226-227 (2012).
Zhang, X. B. et al. Clinical significance of imaging findings for atlantoaxial rotatory subluxation in children. Turk. J. Med. Sci. 48, 332–338. https://doi.org/10.3906/sag-1707-137 (2018).
Tian, M. M., Lin, M., Qian, Q. & Jiang, H. W. [MSCT imaging research on atlanto-axial joint in rotary functional position]. Zhongguo Gu Shang 28, 915–919 (2015).
Harty, J. A., Lenehan, B. & O’Rourke, S. K. Odontoid lateral mass asymmetry: do we over-investigate?. Emerg. Med. J. 22, 625–627. https://doi.org/10.1136/emj.2003.014100 (2005).
Hicazi, A., Acaroglu, E., Alanay, A., Yazici, M. & Surat, A. Atlantoaxial rotatory fixation-subluxation revisited: a computed tomographic analysis of acute torticollis in pediatric patients. Spine (Phila Pa. 1976) 27, 2771–2775. https://doi.org/10.1097/01.BRS.0000035723.17327.49 (2002).
Monckeberg, J. E. et al. CT scan study of atlantoaxial rotatory mobility in asymptomatic adult subjects: a basis for better understanding C1-C2 rotatory fixation and subluxation. Spine (Phila Pa. 1976) 34, 1292–1295. https://doi.org/10.1097/BRS.0b013e3181a4e4e9 (2009).
Jia, L. [Is there a subluxation in the atlantoaxial joint and its related issues]. Chin. J. Surg. 44, 1369-1375 (2006).
Pang, D. & Li, V. Atlantoaxial rotatory fixation: part 1–Biomechanics of normal rotation at the atlantoaxial joint in children. Neurosurgery 55, 614–625. https://doi.org/10.1227/01.neu.0000134386.31806.a6 (2004) (discussion 625 – 616).
Author information
Authors and Affiliations
Contributions
B.W. and W.C. contributed to writing—original draft; B.W., Z.L. and F.L. contributed to data curation; all authors contributed to formal analysis; B.W., Z.J. and Q.Z. contributed to resources; K.S. and Z.L. contributed to conceptualization; all authors contributed to writing—review and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Review Committee of Children’s Hospital Affiliated to Zhengzhou University (No. 2023-K142). Consent to participate was waived by the Ethics Review Committee of Children’s Hospital Affiliated to Zhengzhou University as this was a retrospective study and no personal data was used in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, B., Cheng, W., Li, Z. et al. Comparison of Glisson traction, soft or rigid cervical collars for the treatment of acute atlantoaxial rotatory subluxation in children: a retrospective study. Sci Rep 14, 25927 (2024). https://doi.org/10.1038/s41598-024-77267-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-77267-z