Abstract
Background This study was conducted to assess the clinicopathological characteristics of biopsy lesions in the lacrimal gland, in response to evolving pathological technologies and the emergence of new diseases. A retrospective review of case notes was conducted for 582 patients with biopsied lacrimal gland lesions at West China Hospital of Sichuan University in China. This study, spanning from January 1, 2010, to December 31, 2021, recorded demographics, clinical features, imaging findings, histopathological diagnoses, and recurrence rates. In a cohort of 582 patients, the mean age was 47.5 years, with 318 being female. Bilateral disease was present in 127 patients. Common signs and symptoms included a palpable mass, lid swelling, proptosis, and decreased ocular movements or diplopia. The predominant pathologies identified were inflammation, epithelial tumors, and lymphoproliferative lesions. Patients with inflammation (mean 32.8 months) experienced symptoms for a longer period compared to those with lymphoproliferative lesions (mean 22.2 months) (95% confidence interval [CI] 1.53–19.27, P = 0.022). Younger patients tended to have structural lesions (mean 42.5 years) (95%CI 4.74–21.59, P = 0.003), inflammation (mean 42.9 years) (95%CI 0.46–6.57, P<0.001), or epithelial tumors (mean 46.4 years) (95%CI 6.21–12.38, P<0.001), while older patients more frequently had lymphoproliferative lesions (mean 55.7 years). The period from 2016 to 2021 saw a higher diagnosis rate of biopsied lacrimal gland lesions than from 2010 to 2015. During this later period, there was an increase in cases of immunoglobulin G4-related ophthalmic disease (IgG4-ROD) and malignant epithelial tumors, while lymphoid hyperplasia cases declined. Adenoid cystic carcinoma showed the highest recurrence rate, with lesion extent and Ki-67 index identified as independent risk factors in our study. Inflammation, epithelial tumors, and lymphoproliferative lesions were the three primary causes of lacrimal gland lesions in our study group. Among the inflammatory conditions, IgG4-ROD was the most specific. The incidence of lacrimal gland lesions has risen, particularly for IgG4-ROD. Adenoid cystic carcinoma among the lacrimal gland lesions was prone to recurrence, with the extent of the lesion and Ki-67 index serving as independent risk factors.
Similar content being viewed by others
Introduction
The lacrimal gland are composed of various cell types including secretory gland cells, myoepithelial cells, plasma cells, B and T lymphocytes, nerve cells, and fibroblasts1. Secretion, immunity and other functions of lacrimal gland cells make it prone to a range of diseases2, leading to varied pathological types. Historically, many researchers have explored the pathological distribution of lacrimal gland lesions2,3,4,5,6,7,8,9,10, but previous studies had small sample sizes and was also a lack of clinicopathological analysis of lacrimal gland lesions in a large sample of Chinese population. Moreover, recent advancements in immunophenotyping and molecular pathology, along with the emergence of new diseases like IgG4-ROD, have significantly diversified the pathological types and altered the disease composition. Therefore, the analysis of clinicopathological features of lacrimal gland lesions in China has certain clinical significance.
The purpose of this study was to evaluate the clinicopathological features of lacrimal gland biopsy lesions in the West China Hospital of Sichuan University in China, so as to improve the diagnosis and treatment level of clinicians.
Materials and methods
Design and sample
We conducted a retrospective chart review of patients who underwent biopsies for lacrimal gland lesions at West China Hospital of Sichuan University in China, from January 1, 2010, to December 31, 2021. We excluded patients with repeated pathological diagnoses from the same individual. The follow-up period extended from the date of the initial pathological diagnosis until December 31, 2022. This study received approval from the Review Board of West China Hospital of Sichuan University and adhered to the ethical principles outlined in the Declaration of Helsinki. The cases involved in this study were published only after obtaining informed consent from the patients or their relatives.
Data collection
The collected data encompassed patient demographics, clinical features, imaging results, histopathological diagnoses, and recurrence rates. Only the initial occurrence of relapse in patients was analyzed. Diagnosis of Immunoglobulin G4-related ophthalmic disease (IgG4-ROD) adhered to the 2019 classification criteria set forth by the American College of Rheumatology/European League Against Rheumatism, which includes: (1) clinical or imaging evidence of involvement in typical organs such as the lacrimal gland; (2) absence of any exclusion criteria; (3) a cumulative score of at least 20 points based on pathology, serum IgG4 levels, and the number of affected organs11. Patients meeting all three criteria were classified as having IgG4-ROD in our study.
Statistical analysis
Continuous variables were presented as means ± standard deviations and analyzed using either the Student’s t-test or the Mann-Whitney U test. Categorical variables were expressed as frequencies and percentages and assessed using the Chi-squared or Fisher’s exact tests. Recurrence rates were depicted through Kaplan-Meier curves and differences between groups were evaluated using the log-rank test. A COX regression model was employed for the multivariate analysis of factors influencing outcomes. A P-value of less than 0.05 was considered to indicate statistical significance.
Results
Demographics characteristics
This study evaluated 582 patients, who had a mean age of 47.5 years (range,11 months–86 years). Of these, 318 (54.6%) were female, and the majority presented with unilateral symptoms (78.2%, n = 455). The average duration of symptoms before presentation was 29.8 ± 53.0 months. Additionally, 148 patients had a history of systemic disease, and 27 reported allergies (Table 1).
Clinical presentation
The percentage of ophthalmic signs and symptoms in patients with biopsied lacrimal gland lesions is shown in Table 2. The commonly observed signs and symptoms included a palpable mass (48.8%, n = 284), lid swelling (46.2%, n = 269), proptosis (29.4%, n = 171), and decreased ocular movements or diplopia (24.4%, n = 142) (Fig. 1a-c). Other noted symptoms were conjunctival injection, vision loss, lid hyperemia or edema, periorbital swelling or pain, ptosis, lacrimation, globe dystopia, chemosis, lagophthalmos, keratopathy, dry eye.
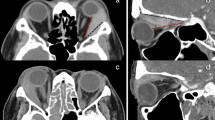
Imaging characteristics
Imaging scans were conducted on 511 patients (87.8%), revealing lacrimal gland enlargement in all cases; 127(21.8%) of these patients exhibited enlargement in both lacrimal glands. Patients with inflammatory lacrimal gland lesions typically presented with diffuse enlargement while retaining an almond-shaped gland, as seen in conditions like dacryoadenitis (Fig. 2a-c). Lymphoproliferative lesions and epithelial tumors, such as IgG4-ROD (Fig. 2d-f) and MALT lymphoma (Fig. 2g-i), were generally.
characterized by a scallop-like mass occupying the lacrimal gland. Dacryops was predominantly identified by its cystoid mass presentation.
a, d, and g: Bilateral lacrimal glands enlargement with moderate signal on MRI T1-weighted images (horizontal view). b, e, h: Bilateral lacrimal glands enlargement with slightly higher signal on MRI T2-weighted images (horizontal view). c, f, and i: B Bilateral lacrimal glands enlargement with high signal on fat-suppressed T1-weighted enhanced MRI scans (horizontal view).
MRI magnetic resonance imaging, IgG4-ROD Immunoglobulin G4-related ophthalmic disease, MALT Mucosa associated lymphoid tissue.
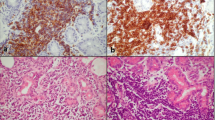
Histopathological classification
The histopathological distribution of biopsied lacrimal gland lesions is illustrated in Table 3. Inflammation (38.7%, n = 225), epithelial tumors (28.9%, n = 168), and lymphoproliferative lesions (28.4%, n = 165) emerged as the three most prevalent pathological types among our patients. Within the inflammatory category, IgG4-ROD (39.6%, n = 89) was the predominant specific cause (Fig. 3a-c). Other causes included Sjögren’s syndrome, granulomatosis with polyangiitis (GPA), amyloidosis, Kimura’s disease, and sarcoidosis.
Among the epithelial tumors, benign forms were predominantly pleomorphic adenomas (97.1%, n = 102), while the most frequent malignant epithelial tumor was adenoid cystic carcinoma (52.4%, n = 33).
In the lymphoproliferative category, lymphoma (73.9%, n = 122) was the most common, with mucosa-associated lymphoid tissue (MALT) lymphoma accounting for 86.9% (n = 106) of these cases. Lymphoid hyperplasia presented as ‘reactive’ in 86.0% (n = 37) of cases and ‘atypical’ in 14.0% (n = 6).
A comparison of clinical features across different histopathological groups revealed that inflammation (58.7%, n = 132) and structural lesions (58.3%, n = 14) were more common in women. Patients with inflammatory lesions (mean 32.8 months) experienced longer symptom durations compared to those with lymphoproliferative lesions (mean 22.2 months) (95% confidence interval [CI] 1.53–19.27, P = 0.022). Those with structural lesions (mean 42.5 years) were generally younger than those with lymphoproliferative lesions (mean 55.7 years) (95%CI 4.74–21.59, P = 0.003). Furthermore, patients with inflammatory conditions (mean 42.9 years) were younger than those with epithelial tumors (mean 46.4 years) and lymphoproliferative lesions (95%CI 9.72–15.91, P = 0.024; 95%CI 0.46–6.57, P<0.001;respectively), and patients with epithelial tumors were younger than those with lymphoproliferative lesions (95%CI 6.21–12.38, P<0.001).
Regarding bilateral disease, the highest incidence was found in patients with IgG4-ROD (49.4%, n = 44), followed by those with idiopathic orbital inflammatory disease (IOID) (30.8%, n = 36) and lymphoproliferative lesions (25.5%, n = 42), indicating that IgG4-ROD more frequently involved both glands compared to IOID and lymphoproliferative lesions (hazard ratio[HR] 2.20, 95% CI 1.24–3.90, P = 0.006; HR 2.86, 95% CI 1.66–4.93, P<0.001; respectively).
lymphoplasmacytic infiltration with stromal fibrosis. b Immunoglobulin G4-positive plasma cell infiltration (right eye, IgG4 stain, ×400). c An additional immunostaining (right eye, CD138 srain,×400) identifies numerous CD138-positive plasma cells.
IgG4-ROD Immunoglobulin G4-related ophthalmic disease, HE Hematoxylin-eosin.
Changes of histopathology of biopsied lacrimal gland lesions from 2010 to 2021
Patients were subgrouped based on the year of biopsy to assess changes over time in the pathological distribution of lacrimal gland lesions (Fig. 4a). A significant increase in the number of biopsies was observed during the period from 2016 to 2021 compared to 2010–2015 (P<0.001). During the latter period, there was a rise in cases of IgG4-ROD and malignant epithelial tumors (all P<0.001), whereas the incidence of lymphoid hyperplasia decreased (P = 0.047). Other pathological distributions remained relatively stable from January 2010 to December 2021(Fig. 4b).
IOID Idiopathic orbital inflammatory disease, IgG4-ROD immunoglobulin G4-related ophthalmic disease.
Clinical outcomes of lacrimal gland lesions
The mean follow-up time was 76.8 months (range,12 months–155 months) and 11 patients were lost in our cohort. In total, 66 patients (11.6%) experienced recurrence of lacrimal gland lesions, with adenoid cystic carcinoma showing the highest recurrence rate (36.4%, n = 12). The five-year progression-free survival (PFS) rate for adenoid cystic carcinoma was 62.14% (Fig. 5a), with lesion extent and Ki-67 index identified as independent risk factors for recurrence (Table 4) (Fig. 5b-c). Recurrences occurred earlier in patients with IOID among inflammatory conditions. Among tumors, adenocarcinoma recurrences occurred significantly sooner than those in pleomorphic adenoma and MALT lymphoma, and recurrences in adenoid cystic carcinoma were earlier than in pleomorphic adenoma, as confirmed by a log-rank test (Fig. 6a-e). There were no notable changes in other recurrence categories. The shortest mean recurrence-free period was 8.4 months in patients with adenocarcinoma, while the longest was 93.8 months in those with pleomorphic adenoma.
MALT lymphoma, and adenoid cystic carcinoma.
IgG4-ROD immunoglobulin G4-related ophthalmic disease, IOID Idiopathic orbital inflammatory disease, MALT Mucosa associated lymphoid tissue.
Discussion
The aim of this study was to assess the clinicopathological characteristics of lacrimal gland biopsy lesions at West China Hospital of Sichuan University in China. Therefore, we reviewed the database for patients who underwent biopsied lacrimal gland lesions in our hospital during the period of January 1,2010 to December 31,2021.
Our analysis revealed that our cohort included a higher number of biopsied lacrimal gland lesions than previous studies and demonstrated that: (1) approximately two-fifths of the patients presented with inflammation, while about one-third had epithelial tumors and lymphoproliferative lesions; (2) patients with inflammatory conditions experienced longer durations of symptoms, and those with structural diseases and inflammation were generally younger, with IgG4-ROD frequently involving bilateral lesions; (3) there was a significant increase in the number of lacrimal gland biopsy patients, notably those with IgG4-ROD and malignant epithelial tumors; and (4) adenoid cystic carcinoma was the most likely to recur, with lesion extent and Ki-67 levels identified as its independent risk factors.
In our study, inflammation emerged as the predominant cause of lacrimal gland lesions, aligning with findings from other studies where inflammation prevalence ranged from 27–66%2–9,12. Specifically, IgG4-ROD was the most common inflammatory cause. We observed that epithelial tumors (28.9%) were the second most prevalent etiology in our series, with a higher proportion compared to studies from Singapore (13.0%)3, Australia (11.9%)4, Korea (16.8%)5, Saudi Arabia (12.5%)7 and Western countries (22%)9. This contrasts with findings by Tao et al., who reported that epithelial tumors accounted for 83.5% of lacrimal gland space-occupying lesions in a study of 91 cases10. Moreover, pleomorphic adenoma was the most common benign epithelial tumors of the lacrimal gland3 and adenoid cystic carcinoma was the most common malignant epithelial tumor4. In addition, the proportion of lymphoproliferative lesions (28.4%) was similarly with the Korean (25.5%)5 and the Saudi Arabia (25.0%)7 studies, but its proportion was lower than that the Singaporean (37.7%)3 and the Australian (32.1%)4 studies. Furthermore, consistent with McKelvie et al., MALT lymphoma was identified as the most frequent lymphoma subtype affecting the lacrimal gland13.The difference of histopathological distribution between our study and other studies3,4,579could be attributed to different biopsy thresholds for lacrimal gland lesions, advancements in pathological techniques, regional epidemiological differences, or the emergence of new diseases like IgG4-ROD.
Our study made several key findings: patients with inflammatory conditions experienced longer symptom durations and tended to be younger, mirroring results from a prior study5. However, unlike previous research, we also noted that patients with structural diseases were typically younger. Moreover, the occurrence of bilateral disease was significantly more prevalent among patients with inflammatory conditions (37.3%) compared to those with lymphoproliferative lesions (25.5%) (HR 1.73,95% CI 1.11–2.69, P = 0.015), a finding consistent with a Korean study5. Additionally, IgG4-ROD frequently presented with bilateral involvement in our cohort. We also observed that lymphoproliferative lesions were more common in older patients and showed no gender bias.
In our analysis, there was a notable increase in the incidence of lacrimal gland lesions, particularly IgG4-ROD and malignant epithelial tumors. This trend contrasts with findings from Andrew et al., who observed a significant decline in pleomorphic adenoma over time. Immunoglobulin G4-related disease (IgG4-RD) is increasingly recognized as an immune-mediated systemic inflammatory condition that affects multiple organs, including the pancreas14, kidney15, skin16, lung17, and salivary gland18. This condition is typically marked by high serum IgG4 levels and infiltration of IgG4+ plasma cells19. Likewise, IgG4-RD also involved orbital structures20, but lacrimal gland was the most common21. Due to previously limited awareness of IgG4-ROD, earlier research often misidentified it as IOID or as lymphoproliferative disorders. In our study, IgG4-ROD was identified in 15.3% of lacrimal gland lesions, a prevalence that is lower than findings from South Korea5 but higher than those reported in Australia4 and Saudi Arabia7. These discrepancies could be attributed to differences in sample size, biopsy thresholds, or epidemiological factors.
In our study, adenoid cystic carcinoma exhibited the highest frequency of recurrence, while adenocarcinoma had the shortest recurrence-free period. We identified lesion extent and Ki-67 as independent risk factors for adenoid cystic carcinoma, findings that diverge from those of previous studies22. We also found that the recurrence-free period was shorter in patients with IOID than in those with IgG4-ROD among inflammation, which was unlike to that found by a Korean study23. In our study, IOID recurrences typically occurred around 16 months post-surgery. When comparing different types of lacrimal gland tumors, adenocarcinoma recurred significantly earlier than both pleomorphic adenoma and MALT lymphoma, and adenoid cystic carcinoma recurred earlier than pleomorphic adenoma. Specifically, recurrences for adenocarcinoma and adenoid cystic carcinoma occurred approximately 8 months and 37 months after surgery, respectively. Therefore, long-term follow-up is crucial for patients with lacrimal gland lesions to monitor for any recurrence or progression of the condition.
This study has several limitations. Firstly, the retrospective design limits the ability to observe long-term outcomes and changes over time in patients’ conditions. Secondly, patients referred for biopsy might have had more severe or atypical symptoms compared to the general population with lacrimal gland issues, leading to selection bias. Additionally, being conducted at a single medical center may limit the application of the results to other regions or populations due to specific demographic or clinical practices. Consequently, our findings may not accurately represent the broader Chinese population with biopsied lacrimal gland lesions. Despite these limitations, this series, which includes 582 patients, stands as one of the largest single-center cohorts globally with biopsy-confirmed pathology of the lacrimal gland, encompassing a wide range of pathological types.
Conclusions
In conclusion, this study included one of the largest samples of biopsied lacrimal gland lesions to date. Inflammation, epithelial tumors, and lymphoproliferative disorders emerged as the three most common causes of lacrimal gland lesions in our Chinese cohort. Patients with inflammatory conditions experienced longer symptom durations. Younger patients were more likely to present with structural diseases and inflammation, and IgG4-ROD frequently involved both lacrimal glands and displayed an increasing incidence trend. Additionally, adenoid cystic carcinoma had the highest recurrence rate, with lesion extent and Ki-67 levels identified as significant independent risk factors. We prospectively investigate the genetic and molecular markers associated with different types of lacrimal gland lesions, particularly exploring the role of Ki-67 in the recurrence of adenoid cystic carcinoma.
Data availability
Data is provided with in the Related files.
References
Obata, H. Anatomy and histopathology of the human lacrimal gland. Cornea 25(S). 82–89. https://doi.org/10.1097/01.ico.0000247220.18295.d3 (2006).
von Holstein, S. L. et al. Lacrimal gland lesions in Denmark between 1974 and 2007. Acta Ophthalmol., https://doi.org/10.1111/j.1755-3768.2012.02403.x (2013).
Teo, L. et al. A survey of the histopathology of lacrimal gland lesions in a tertiary referral centre. Orbit. 32, 1–7. https://doi.org/10.3109/01676830.2012.736595 (2013).
Andrew, N. H., McNab, A. A. & Selva, D. Review of 268 lacrimal gland biopsies in an Australian cohort. Clin. Exp. Ophthalmol. 43, 5–11. https://doi.org/10.1111/ceo.12371 (2015).
Ahn, C. Kang,S.,Sa,H.S.Clinicopathologic features of biopsied lacrimal gland masses in 95 Korean patients. Graefes Arch. Clin. Exp. Ophthalmol. 257,1527–1533 .https://doi.org/10.1007/s00417-019-04327-w (2019).
Jamshidian Tehrani, M. et al. Clinical, radiological and histopathological features of patients with lacrimal gland enlargement. Arch. Iran. Med. 24, 910–915. https://doi.org/10.34172/aim.2021 (2021).
Alturkistany, W. et al. Lacrimal gland lesions biopsied in a Tertiary Eye Center in Saudi Arabia: A clinical, Radiological, Surgical, and histological review. Clin. Ophthalmol. 25, 191–200. https://doi.org/10.2147/OPTH.S331252 (2022).
Luemsamran, P., Rootman, J. & White, V. A. Nassiri,N.,Heran,M.K.S.The role of biopsy in lacrimal gland inflammation: A clinicopathologic study. Orbit. 36, 411–418 (2017).
Shields, C. L. & Shields, J. A. Rathmell,J.P.Clinicopathologic review of 142 cases of lacrimal gland lesions. Ophthalmology. 96, 431–435. https://doi.org/10.1016/s0161-6420(89)32873-9 (1989).
Tao, T. et al. Clinical features and pathological analysis of lacrimal gland occupying lesions in 91 cases. Zhong Hua Yan Ke Za Zhi. 55, 842–846. https://doi.org/10.3760/cma.j.issn.0412-4081.2019.11.010 (2019).
Wallace, Z. S. et al. The 2019 American College of Rheumatology/European League Against Rheumatism classification criteria for IgG4-related disease. Ann. Rheum. Dis. 79, 77–87. (2020).
Priel, A. et al. The Epidemiological, Clinical, and Histopathological Characteristics of Lacrimal Gland Biopsies in a Tertiary Care Center in Israel. Isr. Med. Assoc. J. 20, 104–108 (2018).
McKelvie, P. A. & Wools, C. Roberts,L.,Cook,M.Intravascular large B-cell lymphoma occurring 25 years after treatment of ALK-positive anaplastic large cell lymphoma. Leuk. Lymphoma. 4, 2745–2747. https://doi.org/10.3109/10428194.2013.786071 (2013).
Hamano, H. et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl. J. Med. 344, 732–738. https://doi.org/10.1056/NEJM200103083441005 (2001).
Raissian, Y. et al. Diagnosis of IgG4-related tubulointerstitial nephritis. J. Am. Soc. Nephrol. 22, 1343–1352. https://doi.org/10.1681/ASN.20110100629 (2011).
Tokura, Y. et al. IgG4-related skin disease. Br. J. Dermatol. 71, 959–967. https://doi.org/10.1111/bjd.13296 (2014).
Liu, J. et al. Clinicopathological characteristics of IgG4-related lung disease. BMC Pulm Med. 21 (1), 413. https://doi.org/10.1186/s12890-021-01781-3 (2021).
Vasilyev, V. I. et al. IgG4-related salivary gland lesions. Ter. Arkh. 87, 92–102. https://doi.org/10.17116/terarkh201587892-102 (2015).
Deshpande, V. et al. Consensus statement on the pathology of IgG4-related disease. Mod. Pathol. 25, 1181–1192. https://doi.org/10.1038/modpathol.2012.72 (2012).
Wallace, Z. S., Deshpande, V. & Stone, J. H. Ophthalmic manifestations of IgG4-related disease: Single-center experience and literature review. Semin Arthritis Rheum. 43, 806–817. https://doi.org/10.1016/j.semarthrit.2013.11.008 (2014).
Vasilyev, V. I. et al. Diagnosis of IgG4 - related ophthalmic disease in a group of patients with various lesions of the eye and orbits. Ter. Arkh. 90, 61–71. https://doi.org/10.26442/Terarkh201890561-71 (2018).
Yang, L. D. et al. Prognostic factors for lacrimal gland adenoid cystic carcinoma: A retrospective study in Chinese patients. Int. J. Ophthalmol. 17(8):1423–1430. https://doi.org/10.18240/ijo.2024.08.06 (2024).
Min, H. K. et al. Clinical outcomes and pathological characteristics of immunoglobulin G4-related ophthalmic disease versus orbital inflammatory pseudotumor. Korean J. Intern. Med. 34, 220–226. https://doi.org/10.3904/kjim.2016.304 (2019).
Acknowledgements
The authors acknowledge all the clinicians who helped in the data collection process.
Author information
Authors and Affiliations
Contributions
Lvfu He: study design; ethics approval; data collection; analysis of data; constructing the tables; drafting and revising the manuscript.Weimin He: study design; ethics approval; drafting and revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Was waived by Ethics Committee of West China Hospital of Sichuan University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, L., He, W. Clinicopathological features of lacrimal gland biopsy lesions in 582 Chinese patients. Sci Rep 14, 26514 (2024). https://doi.org/10.1038/s41598-024-77312-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-77312-x