Abstract
To investigate the diagnostic value of intraoperative cytology and rapid immunocytochemistry in primary central nervous system lymphoma. 254 cases of lymphoma and 82 cases of non-lymphoma were collected from 2010 to 2023. Frozen section(FS) was using alone in 44 cases during 2010–2014, FS and intraoperative cytology(IC) were using in 251 cases during 2015 to 2022. Rapid immunocytochemical(RICC, CD20, GFAP) were using with FS + IC in 41 cases during 2021 to 2023. Method One: According to the results of archives, statistic the diagnostic accuracy of lymphoma during three time periods. Method Two: All cases were randomly renumbered, 4 neuropathologists compared the accuracy of independent histology and that of combining cytology. The archives showed the diagnostic accuracy of FS in PCNSL was 77.27%, FS + IC was 86.06%, FS + IC + RICC was 92.68%. The retrospective study demonstrated the diagnostic accuracy of FS was 79.76%, FS + IC was 87.33% and FS + IC + RICC was 92.68%. The positive predictive value, negative predictive value, sensitivity, specificity and accuracy of CD20 were 100%, 76.92%, 90.32%, 100% and 92.68%, respectively. The results of the paired χ2 test was no statistically significant difference (0.05 < P < 0.1) between FS + IC + RICC and immunohistochemical (IHC) diagnosis of paraffin sections. The integration of IC + RICC + FS diagnosis can significantly enhance the intraoperative diagnostic accuracy of PCNSL and rectify potential errors that may occurred when relying solely on FS diagnosis.
Similar content being viewed by others
Introduction
The incidence of primary central nervous system lymphoma (PCNSL) is progressively increasing over time. Timely diagnosis and treatment play a pivotal role in enhancing the survival rate of patients. The management of PCNSL primarily encompasses early administration of chemotherapy, modality-based therapy, and corresponding targeted interventions. Surgical resection fails to provide a survival advantage in individuals diagnosed with PCNSL, additionally, due to the involvement of deep brain structures and extensive lesions in PCNSL, surgical resection often poses serious complications. Hence, the primary objective of surgical biopsy is to procure precise and efficacious samples for pathological diagnosis. In order to avoid overtreatment or unnecessary complications, rapid intraoperative pathological diagnosis is a crucial link in the diagnosis and treatment of PCNSL. The “gold standard” for intraoperative diagnosis of PCNSL is still frozen section (FS). However, to obtain a more comprehensive cross-section, the utilization of FS technology may lead to excessive tissue cutting, resulting in specimen volume reduction that fails to fully depict the whole picture of the lesion. Simultaneously, brain tissue comprises abundant water and lipid components, which readily give rise to artificial illusions such as the formation of numerous ice crystals during freezing, leading to tissue and cellular deformation that poses challenges for pathological diagnosis. Previous studies have demonstrated that the intraoperative diagnostic accuracy of PCNSL using frozen histopathology alone ranges from 50 to 96%, with a potential misdiagnosis rate as high as 25%1,2. Therefore, it is imperative to employ additional techniques such as cytology to enhance the intraoperative diagnostic accuracy of PCNSL.
Intraoperative cytology (IC) is a cost-effective and simple method that requires only a small tissue sample to reveal the cellular morphology of brain tissue. It holds significant value in aiding sample evaluation and facilitating rapid intraoperative diagnosis, exhibiting an accuracy rate ranging from 84.9–95.36%3,4,5. The study suggests that incorporating IC as a diagnostic adjunct to FS yields superior outcomes in the intraoperative diagnosis of central nervous system6,7,8. With the advancement of pathology technology, intraoperative immunohistochemical staining has progressively been implemented for rapid intraoperative diagnosis, enabling direct visualization of tumor cell differentiation within 20 min (excluding molecular classifications). To date, this technology has predominantly been employed for intraoperative breast cancer diagnosis, yielding favorable outcomes9. However, the presence of ice crystals in brain tissue’s frozen section can induce cellular artifacts, thereby yielding non-specific outcomes in immunohistochemical staining and subsequently impacting diagnosis. Intraoperative rapid immunocytochemical staining (RICC) is a cell smear-based staining technique, enabling clear visualization of cellular morphology and without artifacts associated with FS, thereby facilitating definitive diagnosis of PCNSL and enhancing diagnostic accuracy within the limited intraoperative time. Hence, RICC may hold greater significance in facilitating rapid intraoperative diagnosis.
In this study, we investigated the utility of RICC for intraoperative diagnosis of PCNSL and brain tumors using archival data and retrospective research methods. Our findings suggest that FS combining IC with RICC can significantly enhance the accuracy of intraoperative pathological diagnosis for PCNSL.
Results
Clinicopathological data
In a cohort of 254 patients with PCNSL, there were 136 male cases (53.54%) and 118 female cases (46.46%), with a median age of 61.44 years. Tumors frequently occurred in various brain regions, with the frontal lobe being the most common site (60 cases, 23.62%), followed by the basal ganglia (39 cases, 15.35%) and corpus callosum (36 cases, 14.17%). Additionally, tumors were observed in the temporal lobe (28 cases, 11.02%), cerebellum (25 cases, 9.84%), both parietal lobe and ventricles (19 cases, 7.48%), other locations such as thalamus, occipital lobe, brainstem, petrous apex etc., accounting for approximately11% collectively (Table 1).
Diagnostic results
The results of first method demonstrate that, according to the intraoperative diagnostic results from the archival records, between 2010 and 2014, out of the 44 cases with FS only, 22 cases were accurately diagnosed as PCNSL, 12 cases were accurately diagnosed as non-lymphoma cases, while confirmation could not be obtained for 9 cases, and one lymphoma case was misdiagnosed as germinoma. The diagnostic accuracy rate was 77.27%, with an uncertain diagnosis rate of 20.45% and a misdiagnosis rate of 2.27%. Between 2015 and 2022, out of the 251 cases with FS + IC only, 161 cases were accurately diagnosed as PCNSL, 55 cases were accurately diagnosed as non-lymphoma cases, while confirmation could not be obtained for 33 cases, and 1 case each of inflammatory reaction and germinoma were misdiagnosed as PCNSL. The diagnostic accuracy rate was 86.06%, with an uncertain diagnosis rate of 13.14%, and a misdiagnosis rate of 0.80%. Between 2021 and 2023, out of the 41 cases with FS + IC + RICC, 28 cases were accurately diagnosed as PCNSL, 10 cases were accurately diagnosed as non-lymphoma cases, while confirmation could not be obtained for 3 cases. The diagnostic accuracy rate was 92.68%, with an uncertain diagnosis rate of 7.32% and no instances of misdiagnosis observed.
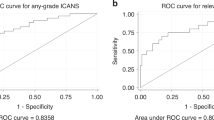
The second method demonstrates that the diagnose from retrospective studies align with those of archival records in FS + IC and FS + IC + RICC but not in FS (Fig. 1). According to the different methods employed, through a double-blind evaluation conducted by four pathologists, among the 336 cases analyzed using FS, 196 cases were accurately diagnosed as PCNSL, 72 cases were accurately diagnosed as non-lymphoma, 30 cases could not be diagnosed due to insufficient evidence, 34 cases needed to be differentiated from other malignant tumors, 1 case of glioma was misdiagnosed as lymphoma, 3 cases of PCNSL were misdiagnosed as glioma or inflammatory reaction, The diagnostic accuracy rate was 79.76%, with an uncertain diagnosis rate of 19.05% and a misdiagnosis rate of 1.20%. Among the 292 cases analyzed using FS + IC, 193 cases were accurately diagnosed as PCNSL, 62 cases were accurately diagnosed as non-lymphoma, 18 cases could not be diagnosed due to insufficient evidence, 16 cases required differentiation from other malignant tumors.1 case each of inflammatory reaction and germinoma were misdiagnosed as PCNSL, whereas 1 case of PCNSL was misdiagnosed as glioma. The diagnostic accuracy rate was 87.33%, with an uncertain diagnosis rate of 11.64% and a misdiagnosis rate of 1.03%. Among the 41 cases analyzed using FS + IC + RICC, 28 cases were accurately diagnosed as PCNSL (CD20 positive, GFAP negative), while 10 cases were accurately diagnosed as glioma or other non-lymphoma (CD20 negative, GFAP positive), 3 cases remained undiagnosed. The diagnostic accuracy rate was 92.68%, with an uncertain diagnosis rate of 7.32% and no instances of misdiagnosis (Fig. 2).
In double-blind retrospective diagnosis, the results of FFPE-IHC were used as reference, compared the proportion of FS, FS + IC, FS + IC + RICC in lymphoma, non-lymphoma, uncertain diagnosis and misdiagnosis. FS + IC + RICC was higher than FS and FS + IC in correct diagnosis of lymphoma and non-lymphoma, lower than FS and FS + IC in uncertain diagnosis and misdiagnosis.
The positive predictive value, negative predictive value, sensitivity, specificity and accuracy of CD20 were 100%, 76.92%, 90.32%, 100% and 92.68%, respectively. The concordance between the diagnosis of FS + IC + RICC (Table 2) and the diagnosis of FFPE-IHC was 3.26, with a paired χ2 test yielding results of 0.05 < P < 0.1. At the level of α = 0.05, the difference was not statistically significant, the results of two approaches are the identical. The concordance between the diagnosis of FS + IC (Table 3), FS (Table 4), and the diagnosis of FFPE-IHC were 37.1835 and 70.85, respectively. Both paired χ2 tests yielded results with a significance level of P < 0.005, the difference was statistically significant.
Ice crystals were commonly observed in frozen tissue sections, while cells displayed a squeezing deformation rate of 89.58%. The tumor cells in the cell smear exhibited a densely lamellar arrangement, accompanied by a diffuse distribution of lymphoid cells and a high nucleus-to-plasma ratio, both apoptosis and mitosis were observed. The cells exhibited a well-defined hierarchical arrangement and morphology, characterized by distinct nuclear and cytoplasmic structures (Fig. 3a). The RICC staining of CD20 reveals plasma membrane expression in lymphomas (Fig. 3b), while GFAP demonstrates cytoplasmic expression in gliomas (Fig. 3c). Additionally, astrocyte staining is observed in both lymphomas and gliomas (Fig. 3d).
Discussion
The current “gold standard” for diagnosing PCNSL is stereotactic biopsy10, and intraoperative frozen pathological diagnosis can provide timely evidence for clinical surgery. The limited tissue sample obtained, excessive cutting of frozen sections (FS), and cellular deformation caused by ice crystals are the primary factors contributing to the low accuracy of intraoperative diagnosis based on FS alone. In all the cases we collected, the squeezing deformation rate of cells in the frozen section was high.
Intraoperative cytology (IC) of neural tumors enables the utilization of a minute tissue sample, effectively preserving the inherent morphological characteristics and intricate cellular structures11, while minimizing sample loss and ensuring prompt and accurate diagnosis12,13. The morphological features were more discernible compared to those observed in frozen sections. However, literature has highlighted that IC is limited in providing a comprehensive histological assessment of lesions as it primarily relies on the identification of main cells and interstitial changes. Consequently, benign lesions may be misinterpreted as malignant due to the presence of individual atypical cells or mistakenly classified as benign due to high differentiation and the inclusion of some malignant cells that have not yet reached full malignancy. Moreover, the sensitivity of IC may be diminished by factors related to interpretation and sampling14. According to the results of our archival records and retrospective evaluation, the addition of IC can significantly enhance the diagnostic accuracy of PCNSL compared to the utilization of FS alone. However, there still exists a misdiagnosis rate ranging from 0.8 to 1.03% and an uncertain diagnosis rate ranging from 11.64% to 13.14%. The morphology of some cases lacks typicality, necessitating subsequent paraffin sections for differential diagnosis, with most cases necessitating differentiation from gliomas15. This is exactly the embodiment of IC defects as described in the literature above.
In previous studies, most researchers employed heating, microwave or AC electric fields to expedite the immunohistochemistry staining process for facilitating intraoperative diagnosis. However, the aforementioned improvements can only reduce the staining duration to 45 min and do not applicable for all types of antibodies16. Currently, RICC is extensively utilized for intraoperative diagnosis of lung16 and breast tissues9,14; however, its application in brain tissue has only been sparsely reported in recent years17,18. The RICC employed in this study is directly conjugated to the primary antibody using nano supersensitive horseradish peroxidase, thereby enabling antigen detection without the need for signal amplification by a secondary antibody. The staining duration is controlled within 20 min, allowing simultaneous execution with FS and IC staining procedures. Based on specific work practices and retrospective evaluation results, this study demonstrates that the addition of RICC does not improve the diagnosis of cases with clear morphological features in IC. However, due to the distinct contrast, RICC staining facilitates detection of cases with inadequate morphology, challenging diagnoses or very small samples, thereby compensating for limitations in IC diagnosis. 1 case of inflammatory lesion was initially misdiagnosed as PCNSL based on FS + IC, but the diagnosis was corrected after negative staining with RICC. 2 cases of PCNSL and 1 case of glioma were initially inconclusive using FS + IC, but the diagnosis was subsequently confirmed upon application of RICC staining. The findings of FS + IC + RICC are consistent with the results of FFPE-IHC, thereby, RICC plays a crucial role in enhancing the intraoperative diagnostic accuracy of PCNSL.
It should be noted that the expression pattern of RICC differs slightly from that observed in FFPE-IHC. CD20 of RICC typically exhibits positive expression in both the cell membrane and cytoplasm, while GFAP can accurately localize astrocytes. Frozen sections are susceptible to artificial artifacts during the preparation process, resulting in suboptimal section quality that often leads to shallow coloring and nonspecific staining of RICC, however, RICC staining results from cell smears show improved precision and accuracy in comparison. Moreover, due to the irreplaceable advantage of HE staining in cell morphological diagnosis, IC and RICC should not be considered as the primary choice or even a standalone intraoperative diagnostic method. Instead, they should only be used when there is insufficient histological evidence or biased diagnostic opinions from FS.
It is worth emphasizing that the diagnosis of RICC still possesses limitations. Due to the limited sample size during PCNSL biopsy, the cell smears is constrained by the selection of tissue sites and variations in smear technique among different personnel, the quantity of effective tumor cells will be influenced. In addition, after adrenocorticotropic hormone treatment, some patients with PCNSL exhibited varying degrees of necrosis, accompanied by a significant infiltration of tissue cells and non-specific inflammation; meanwhile, the presence of tumor cells was scarce or even undetectable19. In our study, 3 cases could be observed a limited presence of atypical lymphoid cells in IC staining. The diagnosis based on paraffin sections classified these cases as diffuse large B-cell lymphoma; however, CD20 of RICC were negative. The statistical analysis revealed that the negative predictive value of CD20 in the present study’s sample was only 76.92%, which could potentially be influenced by factors such as limited sample of cases. Whereas the negative predictive value for GFAP was 100%, therefore, specimens exhibiting such conditions should be comprehensively evaluated by employing GFAP, CD20 or other intraoperative immunological markers, and a meticulous diagnosis should be made in conjunction with treatment history and imaging data.
In summary, cytological smear offers the advantage of being a cost-effective, minimally invasive, and expeditious technique for intraoperative diagnostic in PCNSL. RICC staining can provide a basis for differential diagnosis within the limited time during the operation, facilitating pathologists in making more precise assessments. The integration of intraoperative cytological smear, rapid immunocytochemical, and frozen section diagnosis can significantly enhance the precision of intraoperative diagnosis for primary central nervous system lymphoma while rectifying potential errors that may arise when relying solely on frozen section diagnosis.
Materials and methods
Sample source
The samples and cases included in this study were exclusively sourced from the Department of Pathology at the First Affiliated Hospital of Fujian Medical University. This study was approved.
by the Branch for Medical Research and Clinical Technology Application, Ethics Committee of the First Affiliated Hospital of Fujian Medical University. All methods were performed in accordance with the relevant guidelines and regulations of Declaration of Helsinki and Ethical Review Methods for Biomedical Research on Human Beings. All patients signed an informed consent form before the study. A total of 336 cases of nervous system tumors, diagnosed between 2010 and July 2023, were retrospectively collected. These included 254 cases of lymphoma, 56 cases of glioma, 10 cases of metastatic carcinoma, 7 cases of inflammatory reaction, 5 cases of germinoma, and 4 cases of embryonal tumor. Among them, 44 samples collected between 2010 and 2014 exclusively contain FS, 251 samples collected from 2015 to 2022 were subjected to both FS and IC, 41 samples obtained between 2021 and 2023 encompassed FS, IC, and RICC.
Methods
Technical method
Tissues (0.5–1 mm3) were cut from the samples of suspected lymphoma submitted for inspection during the operation. After slightly squeezing the tissues with two slides, the tissues were smeared in reverse direction to diffuse into a film-like structure. The cell smears were used for IC and RICC staining, respectively. All the tissue samples are required to undergo formalin fixation and paraffin embedding (FFPE) in subsequent processing, as well as the steps of HE staining and immunohistochemical(IHC) staining.
-
1)
Intraoperative cytological staining: (1) fixation with 95% ethanol for 1 min, quick rinse with running water; (2) staining with hematoxylin for 3 min; (3) differentiation with hydrochloric acid for 1 min; (4) rinse with water for 1 min; (5) staining with eosin for 30 s; (6) dehydration with alcohol, xylene transparency, and sealing with gum. (total time within 10 min)
-
2)
Rapid immunocytochemical staining: (1) fixed with 95% ethanol for 1 min, rinsed with PBS; (2) EDTA was heated to just boiling, stopped heating, cooled slowly and washed with PBS; (3) blocked with 3% H2O2 for 1 min, washed with PBS; (4) incubated with closure solution (Guizhou Mexinda medical Technology Co., Ltd, China, instant type); (5) swung off the closure solution, rapid immunocytochemical staining antibody CD20 (Meixinda, China, Rabbit mAb, clone R272, 1:2), GFAP (Mexinda, China, Rabbit mAb, clone R246, 1:10) were incubated at room temperature for 5 min, washed with PBS; (6) DAB (Mexinda, China, instant type) was stained for 1 min, washed with PBS; (7) hematoxylin staining for 1 min, washed with water; (8) alcohol dehydration, xylene transparent, and gum sealing (total time within 20 min).
Diagnostic evaluation method
-
Method 1: According to the intraoperative diagnosis recorded in the archives, based on three different periods, the intraoperative diagnostic accuracy of 44 samples with FS only, 251 samples with FS + IC only, and 41 samples with FS + IC + RICC in PCNSL cases were compared.
-
Method 2: All archival slides of 336 cases were digitally scanned and randomly renumbered for retrospective double-blind evaluation, with staining results diagnosed by four experienced neuropathologists. The evaluation process consisted of three steps: initial diagnosis of FS in 336 cases; re-diagnosis of FS + IC in 292 cases; and further re-diagnosis of FS + IC + RICC in 41 cases. Statistical comparison was conducted to assess the diagnostic accuracy among different methods for PCNSL.
The results of all methods were based on the FFPE-IHC as reference.
Statistical analysis
The results of the retrospective double-blind evaluation and the results of paraffin-embedded immunohistochemistry were subjected to statistical analysis using SPSS21.0 software, employing the χ2 test. A significance level of P < 0.05 was considered statistically significant.
Data availability
We declare that the major data supporting the results reported in this study are available within the manuscript. All data used in this study are available from the corresponding author upon reasonable request.
References
Jindal, A., Kaur, K., Mathur, K., Kumari, V. & Diwan, H. Intraoperative squash smear cytology in CNS lesions: a study of 150 Pediatric cases. J. Cytol. 34, 217–220 (2017).
Jain, S., Kaushal, M., Choudhary, A. & Bhardwaj, M. Comparative evaluation of squash smear and frozen section in the intraoperative diagnosis of central nervous system tumours. Cytopathology. 33, 107–113 (2022).
Patil, S. S., Kudrimoti, J. K., Agarwal, R. D., Jadhav, M. V. & Chuge, A. Utility of squash smear cytology in intraoperative diagnosis of central nervous system tumors. J. Cytol. 33, 205–209 (2016).
Sharma, N. et al. Comparative efficacy of imprint and squash cytology in diagnosing lesions of the central nervous system. Asian Pac. J. Cancer Prev. 12, 1693–1696 (2011).
Chand, P., Amit, S., Gupta, R. & Agarwal, A. Errors, limitations, and pitfalls in the diagnosis of central and peripheral nervous system lesions in intraoperative cytology and frozen sections. J. Cytol. 33, 93 (2016).
Mathon, B., Amelot, A., Mokhtari, K. & Bielle, F. Increasing the diagnostic yield of stereotactic brain biopsy using intraoperative histological smear. Clin. Neurol. Neurosurg. 186, 105544 (2019).
Maity, P. et al. Utility of intraoperative squash cytology in diagnosis of paediatric central nervous system lesions. Diagn. Cytopathol. 47, 428–433 (2019).
Sugita, Y. et al. Intraoperative rapid diagnosis of primary central nervous system lymphomas: advantages and pitfalls. Neuropathology. 34, 438–445 (2014).
Nguyen, L., Khazai, L., Hakam, A., Centeno, B. A. & Rosa, M. Diagnostic value of intraoperative rapid cytokeratin immunostain in the cytological evaluation of sentinel lymph nodes in patients with invasive lobular carcinoma. Diagn. Cytopathol. 47, 482–487 (2019).
Hasner, M. C. et al. Diagnostics and treatment delay in primary central nervous system lymphoma: what the neurosurgeon should know. Acta Neurochir. (Wien). 166, 261 (2024).
Lacruz, C. R. et al. Intraoperative consultation on pediatric central nervous system tumors by squash cytology. Cancer Cytopathol. 123, 331–346 (2015).
Abad-Licham, M. et al. Intraoperative cytology when cryostat is not available. A 7-year experience in a Peruvian cancer center. Diagn. Cytopathol. 51, E45–E53 (2023).
Jaiswal, Y. P. & Gadkari, R. U. Evaluation of role of intraoperative cytology technique in diagnosis and management of cancer. J. Cytol. 37, 126–130 (2020).
Lee, I. K. et al. Intraoperative examination of sentinel lymph nodes by immunohistochemical staining in patients with breast cancer. Eur. J. Surg. Oncol. 32, 405–409 (2006).
Yadav, M. et al. An audit of diagnostic disparity between Intraoperative Frozen Section Diagnosis and final histopathological diagnosis of Central Nervous System lesions at a Tertiary Care Center. J. Lab. Physicians. 17;14, 384–393 (2022).
Abdo, M. et al. Comparative evaluation of PD-L1 expression in cytology imprints, circulating tumour cells and tumour tissue in non-small cell lung cancer patients. Mol. Oncol. 17, 737–746 (2023).
Uzuka, T. et al. Indication of intraoperative immunohistochemistry for accurate pathological diagnosis of brain tumors. Brain Tumor Pathol. 28, 239–246 (2011).
Tanino, M. et al. Rapid immunohistochemistry based on alternating current electric field for intraoperative diagnosis of brain tumors. Brain Tumor Pathol. 32, 12–19 (2015).
Meng, Y. H. & Zhang, J. Z. Updates on patholog and clinical management of primary central nervous system lymphoma. Zhonghua Bing Li Xue Za Zhi. 8;47, 396–400 (2018).
Acknowledgements
1. This work was sponsored by Startup Fund for Scientific Research of Fujian Medical University (No. 2021QH1070).
2. This work was sponsored by Scientific Research Project of National Key Clinical Specialty Construction Project (Grant No.2022YBL-JB-08).
Funding
No specific funding was disclosed.
Author information
Authors and Affiliations
Contributions
L.H.: cases collection, technical operation and improvement, data analysis, writing–original draft and editing. J.T., L.Z. and X.S.: Retrospective diagnosis, data analysis. Ch.H. and X.L.: Figure acquisition, digital operation. Q.W. and S.Z.: Cases collection, technical support. Y.Ch. and Sh.Zh.: Reagent acquisition. X. W.: Conceptualization, retrospective diagnosis, data analysis, writing–review. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hu, L., Tang, J., Su, X. et al. The utilization of cytology for intraoperative diagnosis of primary central nervous system lymphoma. Sci Rep 14, 26527 (2024). https://doi.org/10.1038/s41598-024-78187-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78187-8
Keywords
This article is cited by
-
Clinical utility of repeat brain biopsy in recurrent or refractory primary CNS lymphoma – a diagnostic dilemma
Journal of Neuro-Oncology (2026)
-
Accuracy of intra-operative brain tumor squash cytology compared to large excision biopsy: a comparative study at the University Teaching Hospital of Kigali (CHUK), Rwanda
Journal of Neuro-Oncology (2026)