Abstract
The use of antibiotics by dentist surgeons faces a lack of consensus among professionals and researchers, whether in relation to prophylaxis, or at least regarding the real need for their use. Recent studies increasingly question the use of prophylactic antibiotic therapy in healthy patients. This study aimed to evaluate the knowledge of dentist surgeons working in offices across Brazil regarding antibiotic use protocols and antibiotic resistance. A questionnaire was made via Google Forms and sent by email. The results showed that most dentists prescribe antibiotics for all surgical procedures performed in their office, regardless of the complexity and the patient. Furthermore, low scientific basis was observed among some of the professionals interviewed regarding the best therapeutic choice and the role of antibiotics in the surgical procedure. The present study highlights the urgent need to improve the knowledge of these professionals in Brazil, to reduce the impact on antibiotic resistance.
Similar content being viewed by others
Introduction
Antimicrobial resistance (AMR) is one of the top global public health and development threats, being estimated that 4.95 million deaths were directly or indirectly caused by this problem1. The overuse or misuse of antimicrobial agents by health professionals is responsible for much of this problem. Is estimated that 10–13% of all antibiotics used worldwide are prescribed by dentistry2.
Dental surgeries are routinely performed by dentists in their different modalities and specialties, including easy extractions of residual roots, periodontal and endodontic surgeries, until the most complex and invasive procedures, with the participation of multidisciplinary teams of specialists, in a hospital setting. All of these procedures have in common the fact that they are invasive, involving gingival and periapical region manipulation with or without perforation of the mucosa5,6. Currently, there is no consensus among professionals and researchers regarding the best prophylactic antibiotic therapy in oral surgeries, even about the real need for its use, when related to no high degree of severity procedure5,6. Recent studies increasingly question the use of prophylactic antibiotic therapy in these cases. Some authors even suggest that there is no benefit in the expected prevention of postoperative infections. On the other hand, some professionals claim that when an intraoral surgical procedure begins, there is a breakdown of the local defenses of the mucosa and deeper tissues, even at the risk of causing it7,8. Without a consensus among professionals and an action plan on a global scale, we are migrating to a pre-antibiotic era scenario, in which simple infections can increasingly lead to high mortality rates, and the discussion among dentists in the prophylactic use of antibiotics is an important part of these actions necessary to prevent the spread of resistance9,10.
Finally, the indiscriminate use of antibiotics and antiseptics in dental practice may not be leading to the expected effect. Furthermore, it may be promoting the selection of pathogens with elevated virulence and resistance to antibiotics, which may have an impact not only on the dental procedure, but also on future systemic infections. Therefore, evaluating the impact of the use of these agents and the knowledge of dental professionals regarding this issue is extremely important for the evolution of surgical procedures in current dentistry. The aim of this study is to evaluate, by using an online Google Forms questionnaire, the therapeutic choice of dentistry in Brazil, among five different clinical cases, and evaluate their knowledge about antimicrobial resistance scenery worldwide.
Results
Descriptive analysis of participants
Table 1 describes the characteristics of the participants of this study. The questionnaire was sent to all 106,264 dentists registered on the Dental Council. Of these, 947 responded. The number of dentists who responded may be a limitation of the study, however, the high power shows the robustness of the statistical analyses. Nine hundred and forty-seven participants answered the questionnaire, being 537 (56.7%) women and 409 (43.19%) men. One participant did not identify their gender. The number of participants in the age groups from 30 to 60 years old was similar between groups and 10.45% of participants were over 61 years old.
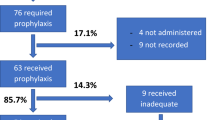
The graduation year varied from 1968 to 2023, with 708 (74.76%) graduating from private or philanthropic educational institutions, and 267 (28.19%) participants stated they had no specialization. Among the specialties, implant dentistry and oral and maxillofacial surgery were the most cited by participants (191 [20.17%] and 107 [11.3%] participants, respectively). Most participants (523 [55.23%]) had specialization as their highest degree of training and a small portion followed an academic career, with 106 (11.19%) master’s degree and 49 (5.17%) PhD. Out of the 947 participants who answered our questionnaire, 816 (86.17%) stated that they performed surgery in their office. Two hundred twenty-two participants that affirmed perform surgery in their offices have no specialization.
Antibiotic therapy protocols choices
Five clinical cases with variable levels of severity, complexity and different patient profiles were included in this study. Most participants stated that they used the longer antibiotic therapy protocol, in the clinical cases suggested, except for clinical case 3, where the number of participants who stated that they did not use antibiotic therapy was equal to those who used the longer protocol. For all clinical cases, the use of therapies with a lower dose or fewer days of treatment was chosen by less than 20% of participants. A result that called attention was the lack of standard protocols among different professionals, and professionals choosing the same antibiotic therapy protocol for all five cases, regardless of the severity or the patient (Table 2).
Case 1 described a young patient, without comorbidities, who was submitted to a surgery of impacted lower third molar extraction, that is, without contact with the oral cavity. The patient had no previous signs of infection. Despite no comorbidity and no sign of infection, 360 (44.12%) participants stated that they used antibiotic therapy for 7 days, 150 (18.38%) used it for 3 days pre-operative and post-operatively and 110 (13.48%) use a loading dose on the day of surgery. Only 196 (24.02%) participants do not see the need to use antibiotics in this case.
The Chi-square analysis showed statistical significance regarding the therapeutic choice for Clinical Case 1 and the category of institution in which this dentist graduated. Analysis of the positive residue demonstrated that professionals trained in a public institution tend to prescribe fewer antibiotics in this case compared to professionals trained in a private institution (Fig. 1A). Furthermore, statistical significance was also observed when comparing the therapeutic choice with whether the professional had specialization. An elevated number of dentists without specialization stated that they would not prescribe antibiotics in this case, while a greater than expected number of professionals with specialization stated that they used pre- and post-surgical antibiotic therapy for 7 days (Fig. 1B). In addition, those professionals who had 5 years or less of training in the specialization were those who prescribed the most pre- and post-surgical protocol for 7 days (Fig. 1C).
Sankey diagrams to visualize the relationship between the categories of variables analyzed and therapeutic scheme choice for clinical case 1. (A) Therapy choice according to the educational institution from which the participant graduated; (B) Therapy choice among specialist and non-specialist professionals; (C) Therapy choice according to training time as a specialist. 1Data analysis was performed using the chi-square test to evaluate the association between categorical variables (p-value < 0.05). *Standardized residuals adjusted from the chi-square test, considering as significant those with values lower than -1.96 or higher than 1.96.
On the other hand, Case 2 described a patient who, despite having also undergone third molar surgery, in this case the tooth was already semi-impacted, that is, it already had contact with bacteria in the oral cavity. Furthermore, the case described symptoms that suggested an infectious process that was then confirmed as pericoronitis. In this case, the infectious process requires the use of antibiotics to treat the infection and then surgery can be performed safely. Six hundred and nine participants (74.63%) stated that they used the antibiotic for 7 days, 123 (15.07%) for 3 days and 48 (5.88%) only a loading dose on the day of surgery. Surprisingly, 36 (4.41%) participants stated that they did not use antibiotics in this case, despite clear signs of previous infection.
The Chi-square test showed statistical significance when prescribing Case 2 in relation to the level of training and time spent training as a specialist. In these parameters, a higher antibiotic prescription was observed in professionals who stated that they had a master’s degree and PhD as their highest level of training (Fig. 2A), while specialist professionals with 5 years or less of training stated that they did not use antibiotic therapy in this case (Fig. 2B).
Sankey diagrams to visualize the relationship between the categories of variables analyzed and therapeutic scheme choice for clinical case 2. (A) Therapy choice according to higher degree from participant; (B) Therapy choice according to specialist training time. 1Data analysis was performed using the chi-square test to evaluate the association between categorical variables (p-value < 0.05). *Standardized residuals adjusted from the chi-square test, considering as significant those with values lower than − 1.96 or higher than 1.96.
Case 3 described a patient without comorbidities, but who underwent a more complicated procedure, to remove multiple molars. This patient, despite not showing classic symptoms of acute infection, had marked mobility in his molars, which suggests a chronic infectious process, such as periodontitis, for example. Three hundred and six participants (37.5%) stated that they did not use antibiotics, being the only clinical case where most participants stated that they did not use antibiotics. Two hundred and eighty-four participants (34.8%) stated they used antibiotics for 7 days postoperatively, 124 (15.2%) stated they used pre and post antibiotics for 3 days and 102 (12.5%) used a dose of attack.
The Chi-square test analysis showed that the use of antibiotics was statistically significantly higher among male professionals compared to female professionals, the majority of whom stated that they did not use antibiotics in clinical case 3. The responses given by men and women regarding antibiotic prescription were significant, where women did not prescribe antibiotics for this clinical case and men prescribed antibiotics for a period of 7 days (Fig. 3A). Furthermore, the level of training of the participants was significant in the therapeutic choice for this case, where participants with an undergraduate level stated that they did not prescribe antibiotics (Fig. 3B). Corroborating this data, professionals with specialization were significant in prescribing a preoperative single-use protocol for this case (Fig. 3C).
Case 4 described a patient undergoing 2-implant surgery. No comorbidities were described by the patient and on clinical examination. Furthermore, the patient had enough bone tissue to undergo surgery, without major complications. Three hundred and sixty-one participants (44.24%) stated that they used the 7-day postoperative antibiotic therapy protocol, while 170 (20.83%) participants stated that they did not use it. Furthermore, 162 (19.85%) stated that they used pre- and post-surgical therapy for 3 days and 123 (15.07%) stated that they used a loading dose.
For the clinical case 4, a statistically significant correlation was observed in the mode of prescription, according to the participant’s age, where participants aged over 46 years tend to prescribe longer antibiotic therapy protocols, while participants aged 45 years or less, were divided between prescribing within 7 days or not prescribing antibiotics (Fig. 4A). In addition, participants with less than 5 years of training in the specialization stated that they used the 7-day antibiotic therapy protocol, while specialists trained with more than 16 years stated that they used the 3-day protocol (Fig. 4B).
Sankey diagrams to visualize the relationship between the categories of variables analyzed and therapeutic scheme choice for clinical case 3. (A) Therapy choice according to gender of participants; (B) Therapy choice according to the higher degree; (C) Therapy choice among specialists and non-specialist’s participants.1Data analysis was performed using the chi-square test to evaluate the association between categorical variables (p-value < 0.05). *Standardized residuals adjusted from the chi-square test, considering as significant those with values lower than -1.96 or higher than 1.96.
Finally, Case 5 described a sinus lift procedure in the upper molar region. Although the patient has no comorbidities and no previous infectious process has been described, this procedure is more invasive and can meet bacteria from the upper respiratory system, generating a process of bacterial translocation, which is a risk factor for infection. later. Most participants (66.42%) stated that they used antibiotic therapy for 7 days as prophylaxis, 126 (15.44%) stated that they used it for 3 days and 65 (7.97%) stated that they took a loading dose on the day of surgery. Despite the procedure having a higher risk of infection, 83 (10.17%) participants stated they did not use antibiotics in these cases.
For clinical case 5, the participant’s age and gender were factors that presented statistical significance regarding the chosen protocol. It was possible to observe that younger participants (less than 25 years old to 35 years old) did not present a pattern in prescription, varying between “Do not prescribe” and “Prescribe for 3 days”. For participants over 55 years of age, the chosen protocol was 7 days of prescription (Fig. 5A). Regarding gender, women reported using the 3-day protocol more, while men reported using the 7-day protocol, once again suggesting that men prescribe more antibiotics than women (Fig. 5B).
Sankey diagrams to visualize the relationship between the categories of variables analyzed and therapeutic scheme choice for clinical case 4. (A) Therapy choice according to age of participant; (B) Therapy choice according to specialist training time. 1Data analysis was performed using the chi-square test to evaluate the association between categorical variables (p-value < 0.05). *Standardized residuals adjusted from the chi-square test, considering as significant those with values lower than − 1.96 or higher than 1.96.
Another relevant factor for therapeutic choice in case 5 was the participant’s level of education and whether he or she had a specialty (Fig. 5C and D). When the specialties were evaluated separately, oral and maxillofacial and implant dentists showed statistical significance, with the former prescribing single-dose and 3-day protocols more frequently, while implant dentists prescribing the 7-day protocol more frequently (Fig. 5E).
Sankey diagrams to visualize the relationship between the categories of variables analyzed and therapeutic scheme choice for clinical case 5. (A) Therapy choice according to age of participant; (B) Therapy choice according to gender of participant; (C) Therapy choice according to the higher degree of participants; (D) Therapy choice among specialists and non-specialists; (E) Therapy choice among implant dentistry and oral and maxillofacial specialists. 1Data analysis was performed using the chi-square test to evaluate the association between categorical variables (p-value < 0.05). *Standardized residuals adjusted from the chi-square test, considering as significant those with values lower than − 1.96 or higher than 1.96.
Additionally, when participants were asked about possible therapeutic options for the treatment of impacted third molar extraction surgery, 67 different combinations of therapeutic options were reported. Two hundred and fifty-seven participants (31.49%) stated that they used only amoxicillin, followed by 70 (8.57%) who stated that they used amoxicillin and azithromycin and 59 (7.23%) who stated that they only used the combination of amoxicillin and clavulanate.
The power analyses of this study were performed using the pwr package v1.3.0 in R for all possible chi-square test comparisons in the response form. Specifically, we utilized the function pwr.chisq.test to calculate the statistical power for each comparison. We assumed a medium effect size (w = 0.3), a sample size of 950 participants (n = 950), and a significance level of 0.05 (sig.level = 0.05). The power reached a value of 1 in all comparisons, due to the large sample size used in the analyses.
Additional data
When participants were asked about the need to use antimicrobials in surgical procedures in healthy patients without a previous infectious focus, 266 (32.6%) participants responded that it was not necessarily due to an association between the immune system’s response and the use of a sterile field. On the other hand, 239 (29.29%) participants stated that it is necessary because they consider the oral cavity a “dirty” place, due to the presence of bacteria. These participants believe that the use of antibiotics as prophylaxis reduces the number of bacteria and prevents infections (Table 3).
When participants were asked what the main reason was for maintaining antibiotics during the postoperative period, the terms that appeared most in the responses were: “Avoiding infections” (690 responses); “Protocol that I have followed for years and it has worked” (116 responses); “Patient comfort” (78 responses); “Reduce edema” (53 responses); and “Pain control” (40 responses) (Table 4).
Finally, when participants were asked about their knowledge regarding the topic “Antibiotic Resistance”, 707 (86.64%) participants responded that they had already heard about it and agreed that they are an important part of the impact on resistance; 27 (3.3%) responded that they had already heard of it, but disagreed with the topic; 23 (2.82%) stated that they have heard about it, agree, but think they can’t do anything about it; 8 (0.98%) had never heard of it and 1 participant responded that he completely disagreed with the topic of antibiotic resistance. Interestingly, the only participant who disagreed with the existence of a resistance problem responded in the previous question that the use of antibiotics is necessary to prevent infections, for patient comfort, for pain control and that is the protocol he has followed for years and has always worked. Although most participants stated that they agree that they are an important part of the impact caused using antibiotics, 92.08% of them consider it important to use antibiotics in the postoperative period as prophylaxis in healthy patients.
Discussion
The World Dental Federation, during its general assembly in 2019, discussed the best ways in which dentists can contribute to the WHO’s 2015 global action against bacterial resistance1,11, to control the indiscriminate prescription of antibiotics. Around 10% of antibiotic prescriptions are made by dentists12,13 reports that 66% of antibiotics prescribed in dentistry have no clinical indication.
The prescription of antibiotics in dentistry is indicated in very specific situations: (a) as a complement to treatments where the infection is already present; (b) to prevent the spread of infection; (c) when there is systemic involvement; (d) if the patient is clinically compromised and has a higher risk of complications13,14. Despite that, in this study, most dental professionals who responded to questionnaires use antibiotics in patients who do not comply with any of the situations mentioned above. Another major problem found in this study is that most participants are not sure why they are prescribing antibiotics and believe that these medications have analgesic capacity and provide comfort to the patient. The most alarming responses were the cases in which the dentist based himself on the simple fact that “he has been using it for years and it has always worked”, without any clinical or scientific basis.
For all clinical cases of questionnaire, variable therapeutic schemes were chosen by participants of this study, including short or long schemes. The therapeutic schemes were suggested, based on the more common protocols used in Brazil dentistry and the protocols found in the literature. Some studies suggest that shorter dosages reduce the exposure of bacteria to antibiotics, thus reducing the speed at which pathogens develop resistance, as well as having the advantage of fewer side effects as well as reducing costs. However, there are no microbiologic studies proving a safe exposure time to avoid resistance. In some cases, one day of antibiotic use is enough to select a resistant pathogen. The personalized healthcare practice will allow us to personalize prescriptions, thus improving health outcomes and delaying the development of resistance9,10,13. In addition, the choice between three- or seven-days antimicrobial prescription has no pharmacological support, since the therapy could be determined according to the label, considering the pharmacokinetic and pharmacodynamic parameters of the drugs. Some strategies are suggested by professionals to reduce the impact caused by bacterial resistance, including establishing an accurate diagnosis based on scientific evidence; if possible, choose an antibiotic drug with a restricted spectrum; use of an appropriate dose, according to the site and type of infection; always evaluate the patient 48 h after starting antibiotic therapy, to prevent the patient from using a complete antibiotic protocol without clinical response; improve knowledge about different classes of antimicrobials and possible protocols, avoiding indiscriminate use8,13,15.
In this study, five clinical cases were proposed, with different levels of severity and complexity. Unfortunately, despite great differences in complexity in both the procedure and the presence of comorbidities in patients, most dentists reported using the same antibiotic protocol for all cases.
Case 1 was designed to be an easy procedure for a patient without comorbidities. Despite this, more than 75% of professionals stated that they use antibiotic therapy, with the majority prescribing it for 7 days. Less than 25% of participants stated that the use of antibiotics was not necessary. Recent studies have shown that healthy patients undergoing extraction surgery for impacted and/or impacted lower third molars did not require a prescription for antibiotics as it is a low-severity procedure in patients without any comorbidity5,6,8.
On the other hand, in Case 2 the question described a typical clinical picture of pericoronitis, which requires the therapeutic use of antibiotics to achieve adequate treatment for this infectious condition. Most participants opted to use antibiotic therapy for 7 days, which the literature supports as the most correct option. It is important to highlight that the treatment of pericoronitis does not only involve the prescription of antibiotics, but also local hygiene measures with the use of mouthwashes, in addition to being instituted as soon as possible, after the significant reduction of signs and symptoms previously present, carrying out the surgery to extract the affected tooth, only then can we have definitive treatment for this condition of pericoronitis. However, one point that caught attention were the 36 participants who stated that they did not use antibiotics in this case, despite clear signs of previous infection, exposing their patients to great risks of postoperative infections that could very well be avoided if the protocols of antibiotic therapy were implemented properly6,7,8,16,17. Probably, in this case, the professionals were not able to perform an infection diagnostic, just reading the text of the case. This study has some limitations as the fact that the questionnaire was conducted totally online, which may have caused some interpretation errors among the participants. However, it was possible to observe that some professionals may have difficulty interpreting clinical symptoms that characterize an infection, for example, showing that perhaps the training of dentists is too technical and lacks scientific knowledge about microbiology, biochemistry, pharmacology and other basic disciplines. In addition, clinical cases including other sceneries should be evaluated to better identify these fragilities.
The Case 3 described a patient without comorbidities, submitted to removal of multiple molars. This patient, despite not showing classic symptoms of acute infection, had marked mobility in his molars, which suggests a chronic infectious process, such as periodontitis, for example. This clinical case was the only one in which most participants stated that they did not use antibiotics probably because, intentionally, no clear signs of infection were described. Despite this, pronounced mobility is a characteristic that must be taken into consideration. In this case, it shows the need to update the currently established protocols, as the use of antibiotics is still recommended in all invasive dental procedures (e.g. extractions) and recent publications already show us that only patients with some degree of systemic impairment should be medicated to try to reduce the occurrence of postoperative infections5. Although both medication protocols - with or without antibiotic therapy - can be considered correct, what counts a lot in this case is the professional’s experience, the maintenance of biosafety and prior and detailed knowledge of this patient’s medical history, in order to be able to choose and give you the best treatment with the best risks/benefits in the equation of reducing postoperative infection versus increasing the risk of promoting bacterial resistance.
In Clinical Case 4, a few participants reported not using any type of antibiotic prescription for implant installation. What the current literature shows us is that in surgeries to install implants, which present sufficient bone tissue, without performing any graft, even in healthy patients, there is an indication to be performed with antibiotic therapy, but for reducing the risk of resistance installation, as an undesirable effect of antibiotic prescription, therefore a single dose is recommended in the preoperative period. On the other hand, most responses make excessive use of antibiotics18,19,20.
The fifth case is a procedure that is more invasive and frequently encounters bacteria from the upper respiratory system, due to perforations of the sinus membrane, generating a process of bacterial translocation. Sinus lift graft surgeries are anatomically located in intimate contact with the maxillary sinus membrane, which no longer becomes the oral region. There is an intervention within the respiratory tract of the patients; therefore, even in healthy patients, there is an indication for these surgical procedures to be performed with the support of antibiotic therapy, due to anatomical particularities, there is a high risk of postoperative infections19,20,21,22.
Additionally, to clinical cases, general questions demonstrated that the lack of information regarding antibiotic therapy protocols result in an impressive 67 different therapeutic choices for a single, third molar surgical procedure in a healthy patient. Moreover, the results of this study demonstrated that the overuse of antibiotics is more frequent among professionals who graduated from a private university, in comparison with public universities. We suggest that this may be explained since in Brazil, public universities are more frequently associated with scientific research, so, the knowledge of these professionals may be more associated with scientific research in comparison with professionals that studied in a private or communitarian university23. Furthermore, the professionals with some specialty tend to prescribe more antibiotics than non-specialist professionals. This result draws attention, once again, to a possible technical training of the professional, leaving scientific and academic knowledge in the background.
Another alarming fact from this present study is the fact that most participants believe that the oral cavity is a “dirty” place due to the presence of bacteria. Knowledge about the importance of human microbiota is already well established and it is no longer acceptable for health professionals to associate bacteria from the oral microbiota with dirt. These results highlight the urgent need to reduce the gap between scientific knowledge and clinical practice.
Finally, this study demonstrate that is necessary to invest in continuing education and awareness programs for these professionals, focusing in particular on the importance of a strict biosafety protocol during dental surgical procedures, which should be used as the most effective tool in preventing infections, and thus being able to promote a reduction in the number of antibiotic prescriptions in dentistry procedures considered invasive, such as tooth extraction surgeries, implant installations or grafts.
Conclusion
Our study demonstrates that a significant proportion of dental professionals continue to prescribe antibiotics indiscriminately, often without a solid scientific foundation, relying instead on personal experience or outdated practices. This overuse of antibiotics, especially in situations where they are not clinically indicated, contributes to the growing issue of antibiotic resistance. Furthermore, our findings highlight a concerning gap between scientific knowledge and clinical practice, particularly among professionals who have limited access to ongoing education and research updates. It is crucial to promote evidence-based protocols for antibiotic use in dental practice, particularly for professionals working exclusively in private offices. Continuing education and awareness programs focused on the importance of proper antibiotic management, combined with strict adherence to biosafety protocols, are essential in reducing unnecessary antibiotic prescriptions. These efforts will not only improve patient care but also help mitigate the global threat of bacterial resistance.
Materials and methods
Ethical aspects and study design
This study was approved by the Ethical Committee from Universidade São Francisco (Process Number: 58541322.5.0000.5514). This study is in accordance with Brazilian General Data Protection Law (LGPD) available in Portuguese language in https://www.gov.br/defesa/pt-br/acesso-a-informacao/lei-geral-de-protecao-de-dados-pessoais-lgpd/arquivos/PortariaGMMDn5.814DiretrizparaaProteodeDadosPessoais.pdf. All subjects consent to participate in this study before being included and consent with data publication in a scientific media. All authors consent to publication of this study. The participants were not identified in this study.
Data acquisition
Data were obtained through an online application, using Google Forms, after signing the Informed Consent Form. The questionnaire was sent by the Regional Dental Council of the State of São Paulo, directly to active professional’s emails. The inclusion criteria were professionals duly registered with the dental council, over 18 years old and working in dental offices in Brazil. After collecting demographic data, participants who stated that they performed surgeries in their offices were directed to respond to clinical cases.
Data storage
Taking into consideration Circular Letter No. 2/2021/CONEP/SECNS/MS regarding guidelines for research procedures with any stage in a virtual environment, the data were stored on a Google drive, in an Excel spreadsheet, shared only between the responsible researchers, previously approved by the Ethical Committee. At no point in the questionnaire and project were the participants identified by name nor identification document number.
Demographic data
Participants were asked about their age, gender, year of graduation, higher degree, classification of graduation degree and postgraduate degree. In Brazil, the universities may be classified in public or private institutions, so, this information was obtained in the questionnaire. Participants who reported that perform surgery in their office were directed to the clinical cases stage of the form.
The questions to obtain demographic information were the following:
-
1.
How old are you?
-
a.
30 years old or less.
-
b.
31 to 40 years old.
-
c.
41 to 50 years old.
-
d.
51 to 60 years old.
-
e.
61 years old or more.
-
a.
-
2.
What is your gender?
-
a.
Female.
-
b.
Male.
-
c.
I prefer do not inform.
-
a.
-
3.
What year did you graduate from college?
This was an open question. To perform the statistical analysis, the results were evaluated classifying the participants in the follow groups, according to responses received:
-
a.
1968–1969.
-
b.
1970–1979.
-
c.
1980–1989.
-
d.
1990–1999.
-
e.
2000–2009.
-
f.
2010–2019.
-
g.
2020–2024.
-
a.
-
4.
What is your highest degree of education?
-
a.
Degree in Dentistry.
-
b.
Post-Graduate Degree (any specialization).
-
c.
Master’s degree.
-
d.
Doctorate Degree.
-
e.
Postdoctoral internship.
-
a.
-
5.
What is the classification of the university where you obtained your degree?
-
a.
Public University.
-
b.
Private University.
-
c.
Beneficent University (Private, but not-profit university. Is classified as a beneficent institution.)
-
a.
-
6.
What is the classification of the university where you obtained your post-graduate degree?
-
d.
Public University.
-
e.
Private University.
-
f.
Beneficent University (Private, but not-profit university. Is classified as a beneficent institution.)
-
d.
-
7.
Do you perform surgery in your office?
-
a.
Yes.
-
b.
Not.
-
a.
Participants who reported that perform surgery in their office were directed to the clinical cases stage of the form.
Clinical cases
Five clinical cases with different levels of severity were applied, as described below:
-
1.
Patient, female, 18 years old, denies underlying diseases and/or allergies, with an orthodontic indication for extraction of impacted/impacted lower third molars. In the anamnesis, she reported she had never had any signs and/or symptoms at the third molar region.
-
2.
Patient, male, 25 years old, denies underlying diseases and/or allergies, with an indication for extraction of lower third molars that appeared semi-impacted radiographically. In the anamnesis, he has always reported painful symptoms, with an unpleasant smell and redness in the region of the third molars. There is a diagnosis of pericoronitis in the left lower 3rd molar.
-
3.
Patient, male, 55 years old, denies underlying illnesses and/or allergies, with indication for multiple molar extractions. In the anamnesis, he did not report anything noteworthy and in the intra-oral examination, he presented lower molars with marked mobility, but without signs and/or symptoms of acute infection.
-
4.
Patient, female, 35 years old, denies underlying illnesses and/or allergies, with an indication of 2 implants in the upper premolar region. In the anamnesis, he did not report anything noteworthy and in the intra-oral examination, the imaging tests showed sufficient bone tissue, even after 1 year of extraction.
-
5.
Patient, female, 44 years old, denies underlying diseases and/or allergies, with an indication to undergo sinus lift grafts in the right upper molar region. In the anamnesis, she did not report anything worthy noticing and in the intra-oral examination, and based on imaging tests, he did not show any type of disease in the maxillary sinus.
Antibiotic therapy protocols
Four antibiotic therapy protocols were provided for participants to select in all clinical cases. Antibiotic therapy protocols were described based on the literature and commonly used protocols. The protocols are described below:
-
1.
Antibiotic medication in the preoperative period and postoperatively for 7 days.
-
2.
Antibiotic medication in the preoperative period and postoperatively for 3 days.
-
3.
Antibiotic medication only in the preoperative period.
-
4.
No antibiotic prescription.
Additional data
Additionally, participants were asked the following questions:
-
1.
Regarding the use of antibiotics in surgeries for patients without comorbidities and in the absence of infection, select the alternative that matches what you believe:
-
a.
It is necessary, as the absence of antibiotic prescription would lead to a postoperative infection.
-
b.
It is necessary to reduce the inflammatory process generated by surgery.
-
c.
It is necessary because the mouth is a “dirty” place and the use of antibiotics reduces the bacterial load present there, preventing infections.
-
d.
It is only necessary if the patient has comorbidities.
-
e.
It is not necessary, as the immune system, associated with a sterile field, provides safety for surgery.
-
a.
-
2.
What is the main reason for you to maintain antibiotics during the postoperative period (the participants could choice one or more alternatives):
-
a.
Avoid infections.
-
b.
Patient comfort.
-
c.
Decrease edema.
-
d.
Decrease in pain.
-
e.
Protocol that I have followed for a long time, and it has worked.
-
f.
I do not use antibiotics in the postoperative period.
-
a.
-
3.
Have you ever heard of antibiotic resistance?
-
a.
I have never heard/read about it.
-
b.
I’ve heard/read it, but I completely disagree.
-
c.
I’ve heard/read it, but I partially disagree.
-
d.
I’ve heard/read it, but I agree, and I don’t think I can do anything about it.
-
e.
I’ve heard/read it, and I agree that I’m an important part of reducing the impact caused by this problem.
-
a.
Data analysis
Data analysis was performed using the chi-square test to evaluate the association between categorical variables. We adopted a significance level of 5% (p-value < 0.05) as a criterion to reject the null hypothesis of independence. Furthermore, the adjusted standardized residuals of the chi-square test were examined, considering those with values lower than − 1.96 or higher than 1.96 as significant. These significant residuals indicate important deviations between the observed and expected frequencies, helping to identify specific categories that contribute to the observed association between the variables.
To complement the analysis, Sankey diagrams were used to visualize the relationship between the categories of the analyzed variables. These diagrams provide a clear graphical representation of the flows and proportions between the different categories, facilitating the understanding of the observed associations. It is important to highlight that the Sankey diagram is a visual tool and does not serve as statistical proof of association. Proof of the association between variables is based exclusively on the results of the chi-square test, as described previously.
Data availability
All data generated or analyzed during this study are included in this published article.
References
World Health Organization. Antimicrobial Resistance [Internet]. Who.int. World Health Organization: WHO. (2019). https://www.who.int/health-topics/antimicrobial-resistance
Durkin, M. J. et al. Centers for Disease Control and Prevention Epicenters. An evaluation of dental antibiotic prescribing practices in the United States. J. Am. Dent. Assoc. 148, 878–886 (2017).
Chen, P. C. et al. Dental procedures and the risk of infective endocarditis. Medicine 94, e1826 (2015).
Buonavoglia, A. et al. V. Antibiotics or no Antibiotics, that Is the Question: An Update on Efficient and Effective Use of Antibiotics in Dental Practice 550–569 (Antibiotics, 2021). n. 5.
Lang, M., Gonzalez, M. L. & Dodson, T. B. Do Antibiotics decrease the risk of inflammatory complications after third molar removal in Community practices? J. Oral Maxillofac. Surg. 75(2), 249–255 (2017).
Dallaserra, M. et al. Infectious postoperative complications in oral surgery. An observational study. J. Clin. Exp. Dent. 12(1), 65–70 (2020).
Menon, R. K., Kar Yan, L., Gopinath, D. & Botelho, M. G. Is there a need for postoperative antibiotics after third molar surgery? A 5-year retrospective study. J. Investig Clin. Dent. 10(4), e12460 (2019).
Sologova, D. et al. Antibiotics efficiency in the infection complications prevention after third molar extraction: a systematic review. Dent. J. (Basel). 10(4), 72 (2022).
López-Lozano, J. M. et al. THRESHOLDS study group. A nonlinear time-series analysis approach to identify thresholds in associations between population antibiotic use and rates of resistance. Nat. Microbiol. 4 (7), 1160–1172 (2019).
Milic, T., Raidoo, P. & Gebauer, D. Antibiotic prophylaxis in oral and maxillofacial surgery: a systematic review. Br. J. Oral Maxillofac. Surg. 59(6), 633–642 (2020).
Antibiotic Resistance in Dentistry | FDI [Internet]. preprod.fdiworlddental.org. https://preprod.fdiworlddental.org/antibiotic-resistance-dentistry
Cervino, G. et al. Antibiotic prophylaxis on third molar extraction: systematic review of recent data. Antibiotics 8(53), 1–14 (2019).
Sukumar, S., Martin, F. E., Hughes, T. E. & Adler, C. J. Think before you prescribe: how dentistry contributes to antibiotic resistance. Aust Dent. J. 65(1), 21–29 (2020).
Sukegawa, S. et al. What are the risk factors for postoperative infections of third molar extraction surgery: A retrospective clinical study? Med. Oral Patol. Oral Cir. Bucal. 24(1), e123–e129 (2019).
Wilson, W. R. et al. Heart Health in the Young; Council on Cardiovascular and Stroke nursing; and the Council on Quality of Care and Outcomes Research. Prevention of Viridans Group Streptococcal Infective endocarditis: A Scientific Statement from the American Heart Association. Circulation 143(20), e963–e978 (2021).
Stein, K. et al. The use and misuse of antibiotics in dentistry: A scoping review. J. Am. Dent. Assoc. 149(10), 869–884e5 (2018).
Khouly, I., Braun, R. S. & Chambrone, L. Antibiotic prophylaxis may not be indicated for prevention of dental implant infections in healthy patients. A systematic review and meta-analysis. Clin. Oral Investig. 23 (4), 1525–1553 (2019).
Khalil, D., Hultin, M., Rashid, M. U. & Lund, B. Oral microflora and selection of resistance after a single dose of Amoxicillin. Clin. Microbiol. Infect. 22 (11), 949 (2016).
Canullo, L. et al. The use of antibiotics in implant therapy: A systematic review and meta-analysis with.
Roca-Millan, E. et al. Systemic antibiotic prophylaxis to reduce early implant failure: A systematic review and meta-analysis. Antibiot. (Basel). 10(6), 698 (2021).
Testori, T., Weinstein, T., Taschieri, S. & Wallace, S. S. Risk factors in lateral window sinus elevation surgery. Periodontol 2000. 81(1), 91–123 (2019).
Caiazzo, A., Canullo, L. & Pesce, P. Consensus report by the Italian Academy of Osseointegration on the use of antibiotics and antiseptic agents in implant surgery. Int. J. Oral Maxillofac. ImplantsInt J. Oral Maxillofac. Implants. 3635(130), 103–105 (2020).
e-MEC. National Registry of Higher Education Courses and Institutions. Available in: (2024). https://emec.mec.gov.br/emec/nova. Accessed in October, 21, 2024.
Acknowledgements
We would like to thank Universidade São Francisco; National Council for Scientific and Technological Development (CNPq), Ministry of Science and Technology, Brazil; and The São Paulo State Research Foundation (FAPESP); for supporting our researchers. We also would like to thank the Regional Dental Council of the State of São Paulo for disseminating the Google forms link among the dentistry in Brazil.
Funding
This study was supported by Universidade São Francisco.
Author information
Authors and Affiliations
Contributions
CAN and KLR contributed with study design, data analysis, and writing of the manuscript, CHA contributed to writing and revision of the manuscript, NCR and NGLS contributed for data analysis, ACGF and LMC contributed with data analysis, writing and revision of the manuscript, and RG contributed with study design, data analysis, writing and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethical Committee from Universidade São Francisco (Process Number: 58541322.5.0000.5514). This study is in accordance with Brazilian General Data Protection Law (LGPD) available in Portuguese language in https://www.gov.br/defesa/pt-br/acesso-a-informacao/lei-geral-de-protecao-de-dados-pessoais-lgpd/arquivos/PortariaGMMDn5.814DiretrizparaaProteodeDadosPessoais.pdf. All subjects consent to participate in this study before being included and consent with data publication in a scientific media.
Consent for publication
All authors consent to publication of this study. The participants were not identified in this study. All participants consent to publish these results in a scientific journal.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
das Neves, C.A., Russi, K.L., Alves, C.H. et al. Overprescription of antibiotics in Brazilian dental clinics: an evaluation of current practices. Sci Rep 14, 29796 (2024). https://doi.org/10.1038/s41598-024-80908-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-80908-y