Abstract
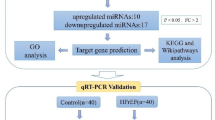
Heart failure (HF) is the leading cause of death in patients with maintenance hemodialysis (MHD). Biomarkers has an important guiding role in the early diagnosis, risk stratification, and prognostic assessment of HF. Increasing studies have indicated that long non-coding RNAs (lncRNAs) have played an indispensable role in the regulatory network of HF. This study was aiming to explore the expression profiles of lncRNAs in patients treated with MHD developing heart failure. Peripheral blood mononuclear cells were isolated from 4 hemodialysis patients with reduced ejection fraction (HFrEF) and 4 hemodialysis patients with preserved ejection fraction (HFpEF), respectively. The expression profile analysis of lncRNAs was performed by using Illumina Novaseq 6000 sequencer. Quantitative real time polymerase chain reaction (qRT-PCR) was used to verify the expression of representative differentially expressed lncRNAs. Based on lncRNA-miRNA-mRNA-KEGG network analysis, the potential role of candidate lncRNAs and their association with the severity of HF were further evaluated. In total, 1,429 differentially expressed lncRNAs were found between patients with HFrEF and patients with HFpEF, of which 613 were up-regulated and 816 were down-regulated (P < 0.05). Five candidate lncRNAs were screened out by a series of bioinformatic analyses. After being compared with miRBase, ENST00000561762, one of the 5 candidates, was considered the most likely lncRNA to be serving as a precursor for miRNA. Nine predicted target genes were found by further lncRNA-miRNA-mRNA-KEGG network analysis, and among which ITGB5 was enriched in the actin dynamics signaling pathway. In another cohort of hemodialysis patients, the expression of lncRNA ENST00000561762 was verified by qRT-PCR. Further analysis revealed that there was a strong correlation between left ventricular ejection fraction and ENST00000561762, proBNP, and 6-minute walk distance, respectively. LncRNAs expression profile was remarkably different in hemodialysis patients with HFrEF compared to those with HFpEF. Among which, lncRNA ENST00000561762 was considered as a promising biomarker for patients with HFrEF as it was predicted to be a miRNA precursor to regulate the actin dynamics signaling pathway.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is closely associated with chronic kidney disease (CKD). CVD is the leading cause of death in patients with CKD1. In China, heart failure (HF) has become the second most common CVD in CKD patients undergoing hemodialysis, which accounts for 10.2% of all CVD2. Increasing studies have confirmed that dialysis patients developing HF would result in a significantly lower survival rate as well as an extremely poor prognosis3,4. Based on ejection fraction, HF can be classified into HF with reduced ejection fraction (HFrEF, LVEF < 40%), HF with mid-range ejection fraction (HFmrEF, LVEF 40–49%) and HF with preserved ejection fraction (HFpEF, LVEF ≥ 50%). Some valuable prognostic indicators in people on dialysis such as BNP and NT-proBNP still have a limited role in the diagnosis of HF5. How effectively and quickly make an accurate diagnosis of HF in dialysis patients has always been a focus in clinical research. Therefore, elucidating the pathophysiological mechanisms of HF in maintenance hemodialysis (MHD) patients and exploring new diagnostic biomarkers and therapeutic targets is of great significance.
Long non-coding RNA (lncRNA) is a type of RNA transcript that are greater than 200 nucleotides without functional protein-coding capacity. They are usually located in the cell nucleus or cytoplasm, and playing a vital role in gene expression regulation at the transcriptional, post-transcriptional, and epigenetic levels6. A growing number of studies show that lncRNA can fold into complex structures and interact with proteins, DNA, and other RNAs, thus playing important roles in the occurrence and development of some diseases7,8,9. It has been reported in the literature that lncRNAs are involved in the regulation of heart development, heart failure, and cardiovascular aging10,11. More importantly, a large number of lncRNA have been found to affect the function of cardiomyocytes via regulating pathways including metabolism, angiogenesis and inflammatory responses12,13. These results suggested that lncRNA has great potential to become a prognostic marker for patients with HF. Recently, several lncRNAs including CRNDE, NRON and MHRT were found up-regulated in patients with HF, and were considered as novel biomarkers of HF14,15. However, up to now, research on the mechanisms of patients treated with MHD developing HF has been relatively sparse. And, there are still some differences and limitations in the lncRNA expression profile between general patients with HF and MHD patients with HF.
In this study, we detected the expression profiles of lncRNAs in peripheral blood mononuclear cells (PBMCs) of different HF types of patients with MHD by transcriptome sequencing, and characterized some markedly differentially expressed lncRNAs between patients with HFrEF and patients with HFpEF. Furthermore, we predicted the potential functions of key differentially expressed lncRNAs in regulating the function of myocardial cell through GO and KEGG analysis. Our results would help to reveal the role and mechanisms of specific lncRNA in the development of HFrEF in hemodialysis patients, and contribute to seeking new biomarkers for early diagnosis of HF in hemodialysis patients.
Materials and methods
Patient and sample
Eight participants from Ziyang Central Hospital from May 2020 to July 2023 were enrolled in this study. Inclusion criteria: Patients have received hemodialysis for more than 6 months. Exclusion criteria: Patients with some underlying diseases such as cancer, diabetes, systemic lupus erythematosus, autoimmune diseases, etc.; Patients on medications that affect immune function. According to 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure Tagged End, participants were divided into 2 groups by left ventricular ejection fraction (LVEF). Four patients with LVEF < 40% were assigned to HFrEF group, while the other four patients with LVEF ≥ 50% were assigned to HFpEF group. All participants provided written informed consent and authorized the use of their blood samples. And the study was approved by the Ethics Committee of Ziyang Central Hospital.
Fasting blood samples were taken from each participant in the morning before hemodialysis by the same nurse. In short, whole blood (10 mL) is layered on Ficoll and then centrifuged at room temperature for 20 min at 2000 rpm. PBMCs were aspirated, washed twice, suspended in PBS. After centrifugation, the cells were collected for subsequent experimentation.
RNA extraction, purification and sequencing
The project was conducted by Oebiotech Corporation (Shanghai, China). According to the manufacturer’s instructions, total RNAs were extracted with the use of mirVana miRNA Isolation kit (Ambion-1561). RNA purity and quantification were evaluated using the NanoDrop 2000 spectrophotometer (Thermo Scientific, USA). RNA integrity was assessed using the Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA). The samples with a total RNA integrity (RIN) > 7 were applied to subsequent lncRNA detection and qRT-PCR experiments. The process of RNA sequencing was accomplished by OE Biotech (Shanghai OE Biotech. Co.,Ltd. Shanghai, China). Ribo-off rRNA Depletion Kit(vazyme, Nanjing, China)was used to remove ribosomal RNA, then the libraries were constructed using VAHTS Universal V6 RNA-seq Library Prep Kit according to the manufacturer’s instructions. Concurrently, sRNA libraries were constructed using the TruSeq Small RNA Sample Prep Kit (Illumina, USA). The constructed RNA libraries were sequenced on an Illumina Novaseq 6000 platform with the generation of 150 bp paired-end reads at the final step.
Differential screening analysis and functional analysis of lncRNAs
About 853.56 M raw reads for each sample were generated. Raw reads of fastq format were firstly processed using fastp16 and the low quality reads were removed to obtain the clean reads. Then about 838.58 M clean reads for each sample were retained for subsequent analyses. The clean reads were mapped to the reference genome using HISAT217. The read counts of each gene were obtained by HTSeq-count18 and then FPKM19 of each gene was calculated. PCA analysis were performed using R (v.3.2.0) to evaluate similarities among samples.
For lncRNAs, the transcriptome from each dataset was assembled independently using the Cufflinks 2.0 program20. All transcriptomes were pooled and merged to generate a final transcriptome using Cuffmerge (Cufflinks 2.0). All transcripts that overlapped with known mRNAs, other non-coding RNA and non-lncRNA were discarded. Next, the transcripts longer than 200 bp and the number of exons > 2 were picked out, and the CPC (v.0.9-r2)21, PLEK (v.1.2)22, CNCI (v.1.0)23, Pfam (v.30)24 were used to predict transcripts with coding potential. The novel predicted lncRNAs were obtained through these processes. The characteristics (including length, type, number of exons) of lncRNA were analyzed after screening. Then the novel predicted lncRNAs and known lncRNAs (from NCBI and Ensemble database) were both used for expression calculation with FPKM4 as mRNA.
Differential expression analysis was performed using the DESeq225. Transcripts with p-value ≤ 0.05 and FC ≥ 2 were considered significant differential expression.
Furtherly, the candidate differentially expressed lncRNAs were predicted by miRanda v. 3.3a to search for the potential miRNA precursors, and those with more than 90% similarity were selected. The target gene prediction of the precursor miRNA relied on three databases of miRDB, miRTARbase, and TargetScan 7.1. Any target gene predicted by these three algorithms was recorded. To determine which of these potential target genes could be associated with HF, Disgenet (v7.0) database was further performed.
CeRNA-miRNA-mRNA network construction
Based on the expression levels of the screened RNAs, Pearson correlation coefficients and P-values for miRNA-lncRNA, miRNA-circRNA, and miRNA- mRNA pairs were calculated for co-expression analysis. Negative correlation pairs with Pearson correlation coefficients > 0.3 were selected for further analysis. The MRE of these association pairs was predicted using the miRanda (v. 3.3a), and the predicted pairs were selected. LncRNA-miRNA-mRNA and circRNA-miRNA-mRNA networks were visualized by Cytoscape (v3.9.0) with default parameters. To identify ceRNA-mRNA pairs, the MuTaME method was used for ceRNA score calculation; the P-value of the corresponding ceRNA association was calculated using a hypergeometric distribution.
Validation of candidate lncRNAs
Briefly, a total of 74 samples (13 hemodialysis patients with HF and 61 hemodialysis patients without HF) were collected. qRT-PCR was used to verify the differential expression of selected lncRNAs. The results were calculated with the 2−∆∆Ct method26.
Statistical analysis
The data were expressed as the mean ± SD, and the statistical analyses were performed using SPSS 20.0 (IBM Corp. NY, USA) and GraphPad Prism 6.0 (GraphPad Software, USA). The unpaired Student t-test was performed to analyze the lncRNA expressions in the PBMCs between the two groups. Analysis of variance was used for comparing more than 2 groups. Pearson correlation was performed to evaluate the correlation between transcripts. P < 0.05 (two-tailed) was considered to indicate statistical significance. The q value is obtained by calibrating the p value by the Benjamini-Hochberg method and a more accurate indication of the positive and false positive levels is revealed at a given cut-off point.
Results
Clinical characteristics of the patients
The clinical characteristics of the two groups at baseline were presented in Table 1. There were no significant differences in gender, age, BMI, hypertension, and diabetes between HFrEF patients when compared to HFpEF patients. However, LVEF, Diuretic, CCB, pro-BNP, cTnT, and CYSC were statistically different between the two groups.
Expression analysis of lncRNAs in each sample
3D PCA plots were used to analyze the expression levels of lncRNAs in each sample, and the sample difference was determined by the distance between each point. As shown in Fig. 1A and B, the two groups were distributed in different areas of two-dimensional or three-dimensional space, and the same group of samples was more concentrated in spatial distribution. As shown in Venn diagram (Fig. 1C), the number of candidate lncRNA coding ability was 6503 according to the prediction results of CPC analysis, CNCI analysis, Pfam protein domain analysis and PLEK analysis. These data indicated that differentially expressed lncRNAs were discriminated between hemodialysis patients with HFrEF and hemodialysis patients with HFpEF.
Expression level of lncRNA in each sample. For each sample, lncRNAs were analyzed using 3D PCA plot (A) and correlation coefficient matrix (B). These 6503 lncRNAs are common to the results obtained from the four databases (C). Test, group of hemodialysis patients with reduced ejection fraction (HFrEF). Control, group of hemodialysis patients with preserved ejection fraction (HFpEF).
We further screened the candidate differentially expressed lncRNAs. The comparison of lncRNAs expression levels between HFrEF group and HFpEF group were shown in the form of Volcano Plot (Fig. 2A). Differential group clustering analysis also showed that the expression of lncRNAs was different between the two groups (Fig. 2B). As shown in Fig. 2C, a total of 1,429 differentially expressed lncRNAs were found between patients with HFrEF and patients with HFpEF, of which 613 were up-regulated and 816 were down-regulated. We uploaded lncRNAs expression data for 8 subjects in the Supplementary material (Supplementary Table 1). To fully investigate the function of aberrantly regulated lncRNA, GO and KEGG analysis were performed. There were 500 significantly enriched GO functions between the two groups, which mainly includes plasma membrane, muscle contraction, cell-matrix adhesion, integrin-mediated signaling pathway, cell surface, and integrin alphav-beta5 complex, and so on (Fig. 3A). Meanwhile, according to KEGG pathway analysis, we found that among the 498 pathways, pathways such as regulation of actin cytoskeleton, IL-17 signaling pathway, cGMP-PKG signaling pathway, mTOR signaling pathway, and NOD-like receptor signaling pathway emerged as significantly different between the two groups (Fig. 3B)27.
The differentially expressed lncRNAs between HFrEF and HFpEF groups. (A) Volcano map of differentially expressed lncRNAs. (B) Cluster heat maps of differentially expressed lncRNAs. (C) Bar chart of differentially expressed lncRNAs. Test, group of hemodialysis patients with reduced ejection fraction (HFrEF). Control, group of hemodialysis patients with preserved ejection fraction (HFpEF).
The top 5 differentially expressed lncRNAs, including ENST00000602528, ENST00000561762, ENST00000453100, ENST00000616527 and TCONS_00003951, were selected for subsequent analysis. Among them, ENST00000561762, ENST00000453100, ENST00000616527 and TCONS_00003951 were up-regulated, while ENST00000602528 was down-regulated (Table 2; Supplementary Table 2).
Prediction of miRNA precursors and its target gene
By comparing above 5 candidate lncRNAs with miRBase, two potential miRNAs were found, namely hsa-miR-766-3p and hsa-miR-3064-5p. Since hsa-miR-3064-5p is not conserved across evolution, it was excluded from subsequent analysis. Among the 5 candidate lncRNAs, it was predicted that lncRNA ENST00000561762 could target and regulate its downstream mRNA by interacting with hsa-miR-4505, meanwhile, serve as a potential miRNA precursor of ITGB5.
Next, we tried to predict the target genes of hsa-miR-766-3p and hsa-miR-4505 through online websites. Through the lncRNA-miRNA-mRNA-KEGG interaction network analysis, target genes of hsa-miR-4505 including CRAT, SELENBP1, ITGB5, R3HDM4, SMIM5, CHI3L1, GPC6, TWISTNB, and PBX1 were found to be significantly associated with the 5 candidate lncRNAs (Fig. 4A), indicating that these 9 target genes might be involved in an intact lncRNA-miRNA-mRNA network. By consulting the literature, it was found that CRAT may be responsible for the progression of chronic myocardial inflammation and heart failure28. ITGB5 has been found to be able to affect pulmonary vascular remodeling, ventricular myocyte function and vascular remodeling29. CHI3L1 was found may play a role in protecting cardiomyocytes from inflammatory damage30. Among the 9 target genes, we further focused on ITGB5 for the reason that it was enriched in the actin dynamics signaling pathway (Fig. 4B), which implied that ITGB5 might play a role in the regulation of cardiac ejection function.
Verification of the expression of lncRNA and correlation analysis
To further clarify the confidence of lncRNA expression profile, we detected the expression level of lncRNA ENST00000561762 in 74 patients using qRT-PCR. The 74 patients were divided into group I (LVEF < 40%), group II (LVEF41-50%), and group III (LVEF > 51%). As shown in Fig. 5A, level of lncRNA ENST00000561762 was statistically different between group I and group III. Additionally, relative expression levels of several common biomarkers such as ESV (Fig. 5B), LV (Fig. 5C), proBNP (Fig. 5D) as well as LA (Fig. 5E), were also detected in each group. Notably, according to correlation analysis, we found that there was a strong negative correlation between the results of LVEF with the expression level of lncRNA ENST00000561762 and proBNP, respectively (Fig. 5F and G), while a strong positive correlation between LVEF and 6MWD (Fig. 5H). The results of proBNP and 6MWD were similar to the actual clinical observation, indirectly proved the correlation between lncRNA ENST00000561762 level and the severity of HF, and also suggested the potential role of lncRNA ENST00000561762 in diagnosis of HF in MHD patients.
Correlation analysis between lncRNA ENST00000561762 and heart failure related. Clinical indexes. To further clarify the confidence of lncRNA expression profile, the expression level of lncRNA ENST00000561762 was detected in 74 patients using qRT-PCR. The 74 patients were divided into group I (LVEF < 40%), group II (LVEF41-50%), and group III (LVEF > 51%). (A) Differential expression of lncRNA ENST00000561762 among groups I, II, and III. (B–E) Differences in relative levels of ESV (B), LV (C), pro-BNP (D), and LA (E) among groups I, II, and III. (F–H) The correlation analysis between LVEF and lncRNA ENST00000561762 (F), pro-BNP and LVEF(G), as well as 6MWD and LVEF (H). *, P < 0.05, **, P < 0.01, ***, P < 0.005, ****, P < 0.001. LVEF, left ventricular ejection fraction. ESV, left ventricular systolic volume. LV, left ventricular diameter. pro-BNP, B-type natriuretic peptide. LA, left atrial diameter. 6MWD, 6-minute walk test.
Discussion
Cardiovascular complication is quite common in patients with CKD, especially in patients treated with hemodialysis. More than 80% of MHD patients have varying degrees and types of cardiovascular complications, of which HF is the most common31.Biomarkers have become a key focus of clinical concern given its important guiding role in the early diagnosis, risk stratification, and prognostic assessment of HF. Recently, the regulatory function of lncRNAs has attracted widespread attention for its medical value in HF, particularly in HF with reduced ejection fraction. Increasing evidence have revealed the close relationship between lncRNAs and HF with reduced ejection fraction29. Many studies have focused on the expression profile of lncRNAs in HF with reduced ejection fraction32, nevertheless, there is still a lack of researches of lncRNAs on HF in hemodialysis patients. Moreover, these studies also rarely addressed the differential expression and function analysis of lncRNAs throughout the course of HF development.
In this study, we applied transcriptome sequencing to explore differentially expressed lncRNAs in MHD patients with HFrEF compared to those with HFrEF. We identified a number of differentially expressed lncRNAs between the two groups, such as SELENBP1 family, ITGB5 family, SMIM5 family and CHI3L1 family, etc., these results were consistent with those reported by Cairns et al.33,34,35. Although lncRNAs above mentioned have been considered as biomarkers for HF by extensively studies, the expression pattern and specific function of these lncRNAs are unknown in hemodialysis patients.
In our experimental results, according to the statistical log2FoldChange, q value and expression level, the top 5 lncRNAs were screened for literature research, and it was found that there were relevant values in promoting cell proliferation, migration, invasion and inflammatory response. Meanwhile, in the aspect of cardiac function, we found some studies on inhibiting inflammation and pyroptosis of myocardial tissue, and inhibiting the activation of Wnt/β-catenin signaling pathway36. Thus we further analyzed and identified 5 novel lncRNAs that showing a unidirectional change trend with HF progression. The exact functions of these candidate lncRNAs in the development and progression of HF are unknown. Previous study has shown that AL356055.1, also known as MACF1, is a cytoskeletal protein, plays a role in promoting osteoblast differentiation and transcription37. LncRNA LINC00570 could positively regulate the expression of URI1, FRAT1 and β-catenin, thus participate in cell proliferation, apoptosis, migration and invasion38. As for ITGB5, studies have shown that it can affect pulmonary vascular remodeling, ventricular myocyte function and vascular remodeling39. Our study focused on exploring the relationship between LncRNA ENST00000561762 and ITGB5. We discovered that lncRNA ENST00000561762 could targeted regulating the expression of downstream mRNA via interacting with hsa-miR-4505. LncRNA ENST00000561762 was able to be detected in the early stages of HF (LVEF < 40%), while it decreased with reduced LVEF, implying that the expression level of lncRNA ENST00000561762 might have a potential role in the prediction of HFrEF occurrence.
LncRNAs can act as competing endogenous RNAs (ceRNAs), thus suppress the binding of miRNAs and their downstream genes. In addition, lncRNAs can also directly serve as precursors of miRNAs40. Our data showed that lncRNA ENST00000561762 has potential to targeted regulate its downstream mRNA by interacting with hsa-miR-4505, and also serve as a potential miRNA precursor of ITGB5, which could be tested in future experiments. Moreover, based on GO and KEGG pathway analyses, we found that target genes of highly differentially expressed lncRNAs were mainly involved in pathways including regulation of actin cytoskeleton, actin dynamics signaling pathway, and so on. Among the 9 target genes of hsa-miR-4505, CRAT41,42, ITGB533,43,44, SMIM545, CHI3L146, GPC647,48 and PBX149 have been confirmed as the key target genes for cardiac function damage in hemodialysis patients. In addition, functional prediction of the target genes revealed that ITGB5 was enriched in actin dynamics signaling pathway, which was consistent with the results of functional enrichment analysis of related lncRNAs. As reported in the literature, ITGB5 was closely associated with cardiac development, coronary artery disease and age-dependent organ failure43,50. Additionally, lncRNAs NONHSAG005537 and NONHSAG017620 have been reported playing an inhibitory role in cell proliferation, migration, invasion and transformation of cardiac fibroblasts induced by TGF-β, suggesting that lncRNA may be involved in the pathogenesis of cardiac fibrosis51. In our study, expression level of lncRNA ENST00000561762 was evidenced to be negatively correlated with LVEF, implying that lncRNA ENST00000561762 might play a crucial role in diagnosis of HF in hemodialysis patients. Although our prediction has not been confirmed by experiments, the regulatory mechanism of lncRNA ENST00000561762 on ITGB5 as well as the relationship between these two indicators with LVEF% in hemodialysis patients is worthy of further investigation. There are also research findings that confirm the value of our further research. ITGB5 is an independent predictor of recurrent CHD events and cardiovascular mortality. These include heart failure and atrial fibrillation. Our study vs. provides additional biological and clinical insights52.
There is no denying that some shortcomings were present in the current study, chief among which is the small sample size. Secondly, the predicted function of lncRNA ENST00000561762 has not been fully studied in MHD patients developing HF. Thirdly, although the intersection of results from multiple databases could guarantee accuracy of our data to some extent, corresponding predicted results are far too few. Fourthly, our data was obtained from a single-center, which might not be enough to confirm the correlation between lncRNAs and HF occurrence in dialysis patients. Moreover, miRNAs that are not conserved have been excluded, which could result in the missing data in our study.
Conclusion
In summary, our study revealed the expression profile of lncRNAs in PBMCs of hemodialysis patients with different degree of HF by RNA sequencing. We identified 5 differentially expressed lncRNAs, and further established an intact lncRNA-miRNA-mRNA network, that is, lncRNA ENST00000561762 might directly act as a precursor of hsa-miR-4505 to regulate the progression of HF by targeting actin dynamics signaling pathway associated gene such as ITGB5. On one hand, our study provides a template for exploring promising disease-related biomarkers. On the other hand, our data could inform our understanding of roles of lncRNAs in HF progression, consequently helping the identification of novel biomarkers for MHD patients developing HF.
Data availability
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
References
Anker, S. D. & von Haehling, S. Inflammatory mediators in chronic heart failure: An overview. Heart 90(4), 464 – 70 (2004).
Sudoh, T., Kangawa, K., Minamino, N. & Matsuo, H. A new natriuretic peptide in porcine brain. Nature 332(6159), 78–81 (1988).
Nitsche, A. & Stadler, P. F. Evolutionary clues in lncRNAs. Wiley Interdiscip Rev. RNA, 8, 1, (2017).
Ferrè, F., Colantoni, A. & Helmer-Citterich, M. Revealing protein-lncRNA interaction. Brief. Bioinform, 17(1), 106–116 (2016).
Mark, P. B. et al. Left ventricular dysfunction with preserved ejection fraction: The most common left ventricular disorder in chronic kidney disease patients. Clin. Kidney J. 15(12), 2186–2199 (2022).
Zhu, M. et al. Lnc-mg is a long non-coding RNA that promotes myogenesis. Nat. Commun. 8, 14718 (2017).
Zampetaki, A., Albrecht, A. & Steinhofel, K. Long non-coding RNA structure and function: Is there a link? Front. Physiol. 9, 1201 (2018).
Li, L. et al. Plasma and tumor levels of Linc-pint are diagnostic and prognostic biomarkers for pancreatic cancer. Oncotarget 7(44), 71773–71781 (2016).
Vausort, M., Wagner, D. R. & Devaux, Y. Long noncoding RNAs in patients with acute myocardial infarction. Circ. Res. 115(7), 668–677 (2014).
Ma, Y. et al. Long noncoding RNA highly upregulated in liver cancer regulates the tumor necrosis factor-α-induced apoptosis in human vascular endothelial cells. DNA Cell. Biol. 35(6), 296–300 (2016).
Zhou, T., Ding, J. W., Wang, X. A. & Zheng, X. X. Long noncoding RNAs and atherosclerosis. Atherosclerosis 248, 51–61 (2016).
Sallam, T. et al. Feedback modulation of cholesterol metabolism by the lipid-responsive non-coding RNA LeXis. Nature 534(7605), 124–128 (2016).
Ellis, B. C., Graham, L. D. & Molloy, P. L. CRNDE, a long non-coding RNA responsive to insulin/IGF signaling, regulates genes involved in central metabolism. Biochim Biophys Acta 1843(2), 372–386 (2014).
Xuan, L. et al. Circulating long non-coding RNAs NRON and MHRT as novel predictive biomarkers of heart failure. J. Cell. Mol. Med. 21(9), 1803–1814 (2017).
Qi, H. et al. MSTN attenuates cardiac hypertrophy through inhibition of excessive cardiac autophagy by blocking AMPK /mTOR and miR-128/PPARγ/NF-κB. Mol. Ther. Nucleic Acids. 19, 507–522 (2020).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30(15), 2114–2120 (2014).
Kim, D., Langmead, B. & Salzberg, S. L. HISAT: A fast spliced aligner with low memory requirements. Nat. Methods. 12(4), 357–360 (2015).
Roberts, A., Trapnell, C., Donaghey, J., Rinn, J. L. & Pachter, L. Improving RNA-Seq expression estimates by correcting for fragment bias. Genome Biol. 12(3), R22 (2011).
Trapnell, C. et al. Transcript assembly and quantification by RNA-Seq reveals unannotated transcripts and isoform switching during cell differentiation. Nat. Biotechnol. 28(5), 511–515 (2010).
Expert consensus on the diagnosis and treatment of young breast cancer in China. Edition. Zhonghua Yi Xue Za Zhi 103(6), 387–403 (2022).
Kong, L. et al. CPC: assess the protein-coding potential of transcripts using sequence features and support vector machine. Nucleic Acids Res. 35. Web Server issue, pp. W345-9 (2007).
Li, A., Zhang, J. & Zhou, Z. PLEK: A tool for predicting long non-coding RNAs and messenger RNAs based on an improved k-mer scheme. BMC Bioinform. 15(1), 311 (2014).
Sun, L. et al. Utilizing sequence intrinsic composition to classify protein-coding and long non-coding transcripts. Nucleic Acids Res. 41(17), e166 (2013).
Finn, R. D. et al. Pfam: the protein families database. Nucleic Acids Res. 42 (2014). Database issue, D222-30.
Anders, S., Pyl, P. T. & Huber, W. HTSeq–a Python framework to work with high-throughput sequencing data. Bioinformatics 31(2), 166–169 (2015).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2 – ∆∆CT method. Methods 25(4), 402–408 (2001).
Kanehisa, M. & Goto, S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28(1), 27–30 (2000).
Mao, H. et al. CRAT links cholesterol metabolism to innate immune responses in the heart. Nat. Metab. 5(8), 1382–1394 (2023).
Shi, A. et al. Plasma-derived extracellular vesicle analysis and deconvolution enable prediction and tracking of melanoma checkpoint blockade outcome. Sci. Adv. 6, 46 (2020).
Henry, A. et al. Therapeutic targets for heart failure identified using proteomics and mendelian randomization. Circulation 145(16), 1205–1217 (2022).
Pilmore, H. et al. Cardiovascular disease in patients with chronic kidney disease. Nephrol. (Carlton). 19(1), 3–10 (2014).
Jha, S., Thasma Loganathbabu, V. K., Kumaran, K., Krishnasamy, G. & Aruljothi, K. N. Long non-coding RNAs (lncRNAs) in heart failure: A comprehensive review. Noncoding RNA, 10, 1 (2023).
Leifheit-Nestler, M. et al. Overexpression of integrin beta 5 enhances the paracrine properties of circulating angiogenic cells via src kinase-mediated activation of STAT3. Arterioscler. Thromb. Vasc Biol. 30(7), 1398–1406 (2010).
Zhang, X. et al. Application of weighted gene co-expression network analysis to identify key modules and hub genes in oral squamous cell carcinoma tumorigenesis. Onco Targets Ther. 11, 6001–6021 (2018).
Yu, J. E. et al. Significance of chitinase-3-like protein 1 in the pathogenesis of inflammatory diseases and cancer. Exp. Mol. Med. 56(1), 1–18 (2024).
Zeng, M. et al. LncRNA MALAT1 to Enhance pyroptosis in viral myocarditis through UPF1-Mediated SIRT6 mRNA decay and Wnt-β-Catenin Signal Pathway. Cardiovasc. Toxicol. (2024).
Hu, L. et al. MACF1 promotes osteoblast differentiation by sequestering repressors in cytoplasm. Cell. Death Differ. 28(7), 2160–2178 (2021).
Piao, X., Zhou, J. & Hu, J. Role of RP11-83J16.1, a novel long non-coding RNA, in rheumatoid arthritis. Am. J. Transl Res. 12(4), 1397–1414 (2020).
Su, H. et al. CircItgb5 promotes synthetic phenotype of pulmonary artery smooth muscle cells via interacting with mir-96-5p and Uba1 in monocrotaline-induced pulmonary arterial hypertension. Respir Res. 24(1), 165 (2023).
Camacho, C. et al. BLAST+: architecture and applications. BMC Bioinform. 10, 421 (2009).
Akanya, D. T., Parekh, J., Abraham, S., Uche, S. & Lancaster, G. Catheter-related right atrial thrombus requiring surgical embolectomy, Cureus 13(9), e17641 (2021).
Zhang, Y., Shi, J., Li, J. J., Zhang, L. & Li, Y. Systemic thrombolysis and anticoagulation therapy for catheter-related right atrial thrombosis caused by TIVAP: A case report and review of the literature. J. Vasc Access. 23(2), 313–317 (2022).
Cairns, J. T. et al. Loss of ELK1 has differential effects on age-dependent organ fibrosis. Int. J. Biochem. Cell. Biol. 120, 105668 (2020).
Verweij, N., Eppinga, R. N., Hagemeijer, Y. & van der Harst, P. Identification of 15 novel risk loci for coronary artery disease and genetic risk of recurrent events, atrial fibrillation and heart failure. Sci. Rep. 7 (1), 2761 (2017).
Zodro, E. et al. FUT11 as a potential biomarker of clear cell renal cell carcinoma progression based on meta-analysis of gene expression data. Tumour Biol. 35 (3), 2607–2617 (2014).
Sun, Y., Shan, X., Guo, J., Liu, X. & Ma, D. CHI3L1 promotes myocardial fibrosis via regulating lncRNA TUG1/miR-495-3p/ETS1 axis, Apoptosis, vol. 28, no. 9–10, pp. 1436–1451, (2023).
Sağlam, E. C. et al. Combined use of serum N-terminal Pro-B-type natriuretic peptide and glypican-6 in the diagnosis of heart failure. Cureus 15(9), e45766 (2023).
Melleby, A. O. et al. The heparan sulfate proteoglycan glypican-6 is upregulated in the failing heart, and regulates cardiomyocyte growth through ERK1/2 signaling. PLoS One. 11(10), e0165079 (2016).
Wu, R., Xue, P., Wan, Y., Wang, S. & Gu, M. LncRNA-uc.40 silence promotes P19 embryonic cells differentiation to cardiomyocyte via the PBX1 gene. Vitro Cell. Dev. Biol. Anim. 54 (8), 600–609 (2018).
Molck, M. C. et al. Gil-Da-Silva-Lopes, genomic imbalances in syndromic congenital heart disease. J. Pediatr. (Rio J). 93 (5), 497–507 (2017).
Han, Z. et al. Analysis of long noncoding RNAs expression profiles in the human cardiac fibroblasts with cardiac fibrosis. Biochem. Biophys. Res. Commun. 660, 73–81 (2023).
Niek, V., Ruben, E., Yanick, N. H. & Pim, H. Identification of 15 novel risk loci for coronary artery disease and genetic risk of recurrent events, atrial fibrillation and heart failure. Sci. Rep., 7,1 (2017).
Acknowledgements
We thank all the patients and the healthy volunteers who consented to provide their blood specimens.
Funding
This project was supported by Establishment of lncRNAs spectrum and risk prediction model related to heart failure in hemodialysis patients in Sichuan Chongqing region based on high-throughput gene sequencing technology (NO. 2022YFS0152). This project was supported by 2022 Chengdu Medical College-The First People’s Hospital of Ziyang Joint Scientific Research Fund Project (2022LHZY04). This project was supported by Luzhou Key Laboratory of Molecular Diagnosis of clinical Diseases will open the fund project in 2023 (FZZD2023-06).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Huaguo Wang, Xing Qi. Performed the experiments: Lin Yu, Shuai Liu, Yujiao Zhou, Wenqing Liu, Wei Liao, Qin Guo, Xuhui Song. Analyzed the data: Jifeng Li, Sheng Lin, Chuanqiang Dai, Lin Yan, Tao Li, Li Zhang, Shucheng Zhao. Contributed reagents/ materials/analysis tools: JuanTang, Jian Cai, Zejiang Liu, Ran Zhu, Q-Y Long. Wrote the paper: Huaguo Wang, Xing Qi, Lin Yu. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of ethics
This study adhered to the tenets of the Declaration of Helsinki and Malaysian Guidelines for Good Clinical Practice (GCP).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qi, X., Yu, L., Liu, S. et al. The expression profile analysis and functional prediction of lncRNAs in peripheral blood mononuclear cells in maintenance hemodialysis patients developing heart failure. Sci Rep 14, 29577 (2024). https://doi.org/10.1038/s41598-024-81080-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81080-z