Abstract
Late onset multiple sclerosis (LOMS) represents between 0.6 and 12% of all MS patients. However, little is known on the incidence of LOMS in the general population. Therefore, we aimed to study the annual incidence of LOMS in a population-based cohort. The study was conducted in the province of Catania, Italy. Case ascertainment was conducted retrospectively including all patients aged ≥ 50 years at onset and with the onset between 2005 and 2020. Incidence rates (IR) have been calculated for all the study period, according to sex, age classes and for subperiods. Incidence rate ratios (IRR) have been computed to compare incidence rates. During the study period, 183 patients with LOMS were identified (113 women; 61.8%). The mean age at onset was 55.8 ± 5.4 years and the main phenotype was Relapsing Remitting MS (n = 123; 67.2%). The average annual crude IR was 2.87/100,000 person-years (95% Confidence Intervals, CI 2.31–3.13). IR increased from 2.54/100,000 in 2005–2010 to 3.32/100,000 in 2016–2020, especially in in the age group 60–69 (IRR 3.48; 95%CI 1.41–9.76; p-value 0.002). In conclusion, an increased IR over the time was observed in the age-group 60–69, possibly reflecting an increased age at onset of MS.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) represents the most common disabling neurological disease of young adults with symptom onset generally occurring between the ages of 20 to 40 years1. Although considered a disease of the young population, MS can also affect older individuals. Late Onset Multiple Sclerosis (LOMS) is defined when the onset occurs after 50 years. Patients with LOMS have different characteristics from those of MS arising at an earlier age: a higher male prevalence and an increase in primary progressive MS (PPMS) forms2,3,4. Concerning clinical characteristics, the main symptoms are more frequently motor dysfunctions, followed by sensory disturbances, there is a higher disability already at diagnosis and greater cognitive impairment2,4,5.
Across MS cohorts, the prevalence of LOMS ranges from 1.1 to 21.3%6, with estimates varying according to inclusion criteria and diagnostic criteria for MS. Incidence data is still scarce, with evidence coming either from cohort studies7 or registry-base studies8,9. A Danish register study found an incidence rate (IR) in the years 2000–2009 in the population between 50 and 64 years old of 2.72/100,000 in men and 7.47/100,000 in women, with a significant increase compared to the 1950–1959 time period9. The same increasing pattern of LOMS IR has been described in Ishafan province (Iran) between 2011 and 2016, with an IR of 10.3/100,000 and 17.4/100,000 respectively8.
Despite being one of the countries with high incidence of MS, there is no data on the incidence of LOMS in Italy.
Therefore, the aims of this study are to describe the incidence of LOMS in the province of Catania in the years 2005–2020 and to describe the clinical characteristics of incident LOMS patients.
Materials and methods
Study setting and population
The study was conducted in the province of Catania, located in the eastern part of Sicily and consisting of 58 municipalities. During the study period, the resident population in the province of Catania aged 50 years or older was considered: it ranged from 352,096 (159,922 men and 192,174 women) on January 1 2005 to 445,113 (204,077 men and 241,036 women) at January 1, 202010. During the same period, the proportion of foreign subjects to the total population, both over 50 years old, in the province ranged from 0.38% in 2005 to 1.62% in 2020.
Case ascertainment
The main sources of case ascertainment were: the neurological divisions and MS centers in Catania (University hospital Policlinico-G. Rodolico-San Marco; Garibaldi Hospital; and Cannizzaro Hospital). In addition, to ensure the completeness of case ascertainment, we also reviewed the archives of the neurological divisions of the Augusta Hospital, near the province of Catania, and the “G. Giglio” Institute Foundation in Cefalù, which is one of the reference centers for MS in Sicily.
Medical records of all patients who had a code 340, 3410, 3418, 3419 (according to the 9th version of the International Classification of Diseases, ICD-9) anywhere in the hospital discharge diagnosis were requested. Data were collected and reviewed by qualified neurologists. Patients were considered incident cases of MS: if they satisfied the revised McDonald criteria11,12,13 for definite or possible MS; if they had clinical onset (i.e. the first appearance of a symptom of MS) between January 1 2005, and December 31 2020; if they were residents in the province of Catania and if they were older than 50 years at the time of disease onset.
In order to enrol patients with disease onset between 2005 and 2020 who satisfied the diagnostic criteria only after the study period, case ascertainment was extended until August 31 2024.
Clinical characteristics, MS phenotype and therapeutic regimen were collected at the time of diagnosis. Initial symptoms were categorized into six types: motor dysfunction; sensory disturbances; visual impairments (optic neuropathy); brainstem dysfunction; cerebellar dysfunction; others. In order to evaluate disease severity, EDSS at diagnosis was recorded. The course of disease was defined as Relapsing Remitting MS (RRMS), or Primary Progressive MS (PPMS).
Concerning the first therapeutic regimen of enrolled patients, we have classified the following therapies as moderate-efficacy disease modifying therapies (meDMT): teriflunomide, interferon beta-1a, interferon beta-1b, glatiramer acetate and dimethyl fumarate; high-efficacy DMT (HeDMT) were: fingolimod, cladribine, mitoxantrone, methotrexate, cyclophosphamide, azathioprine, immunoglobulin, daclizumab, ocrelizumab, natalizumab, rituximab, ofatumumab and siponimod.
Statistical analysis
The mean onset adjusted annual IR in the province of Catania, for individuals diagnosed with LOMS, was estimated for the entire study period and separately for the periods 2005–2010, 2011–2015, and 2016–2020 and by sex. Incidence Rate Ratios (IRR) were also computed to compare IR across time periods, considering the 2005–2010 as reference, and according to sex. The population of the province of Catania has been averaged between the resident population in 2005 and 2020 for the main analysis and, for the three sub-periods, by averaging the population at the start and at the end of each sub-period. Incidence rates for the entire study period were adjusted by the Italian standard population10 and the European standard population14. The ninety-five confidence intervals (95% CI) were calculated assuming a Poisson distribution.
Comparisons of qualitative variables were conducted using the Chi-Squared or Fisher’s test. Statistical analysis was conducted using STATA 17.0 software.
Standard protocol approvals, registrations, and patient consents
The study protocol was approved by the local Ethics Committee (Comitato Etico Catania 1 – n. 173/2022/EMPO). Informed consent was waived due to the retrospective nature of the study and clinical data were anonymised before being used for the analysis. The research has been conducted in accordance with the Declaration of Helsinki.
Results
Study sample demographic characteristics
During the study period, 183 patients with LOMS were identified (113 women, 61.8%). The mean age at onset was 55.8 ± 5.4 years (55.5 ± 5.5 years for women, 56.3 ± 5.3 years for men). The median length of time between clinical onset diagnosis was 1 year (interquartile range 0–3).
Regarding the clinical course: 123 subjects had a RRMS phenotype (67.2%), 39 PPMS (21.3%), in 21 cases (11.5%) the course was undetermined.
Data for symptoms at onset was available for 165 subjects (90.1%). The most frequent symptoms at onset were motor dysfunction (43%), followed by sensory disturbances (27.3%), visual impairment (12.1%), brainstem syndromes (9.1%), cerebellar involvement (4.2%) and other symptoms (4.2%). There were no significant differences of the frequency of symptoms onset across the three time periods (p value = 0.2).
The median EDSS at diagnosis (available for 147 cases, 80.3%) was 2.5 (interquartile range 1.5–4.5). Concerning therapy at diagnosis (available for 161 cases, 87.9%): 64 MS subjects (39.8%) received meDMT, 35 (21.7%) received HeDMT and 62 (38.5%) received no therapy.
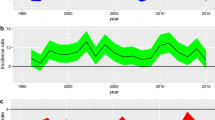
Incidence rates
During the 2005–2020 period the average population, with an age of 50 or older, in the province of Catania was 398,607 (182,001 men and 216,606 women). The IR for both sexes was 2.87/100,000 person-years (95% CI 2.47–3.31). IR was 3.26/100,000 (95% CI 2.70–3.90) for women and 2.4/100,000 (95% CI 1.88–3.02) for men, with a female to male ratio of 1.35 (95% CI 0.99–1.85; p value = 0.04). Age-specific IR reached a peak of 6.12/100,000 (95% CI 5.17–7.20) in the group aged 50–59 years (Tables 1 and 2; Fig. 1).
IR for the entire study period adjusted to the Italian population was 2.74/100,000 (95%CI 2.55–2.95), whereas when adjusted to the European population the IR was 2.79/100,000 (95%CI 2.77–2.80).
Overall, the incidence rate increased from 2.54/100,000 in 2005–2010, to 3.32/100,000 in 2016–2020. When considering the age-group 60–69, the IRs steadily increased over the time from 1.12 during 2005–2010 to 1.71 during 2011–2015 and reaching a peak of 3.12 during 2016–2020. In particular, comparing the IR of the second and third sub-periods to the first one, the IRR was 1.52 (95%CI 0.52–4.72; p value = 0.4) and 3.48 (95%CI 1.41–9.76; p value = 0.002) respectively (Table 3; Fig. 2). In this age group the IR for men increased from 0.68/100,000 (95%CI 0.11–2.25) in 2005–2010 to 2.96/100,000 (95%CI 1.44–5.43) in 2016–2020, with an IRR of 4.34 (95%CI 0.9-41.35; p value = 0.04). Whereas, in women the IR increased from 1.51/100,000 (95%CI 0.55–3.38) in 2005–2010 to 3.26/100,000 (95%CI 1.78–5.67) in 2016–2020, with an IRR of 2.16 (95%CI 0.69–7.96; p value = 0.15) (Fig. 2).
Discussion
Our study demonstrated a progressive increase in the incidence of LOMS in the province of Catania over the last 16 years, especially in the period 2016–2020. As expected, incidence of LOMS is lower compared to adult onset MS (AOMS), which in Italy varies from 4.3/100,000 (Campobasso) to 6.6/100,000 (Tuscany region) to 8.2/100,000 (province of Catania)15,16,17. This shows how MS can still be considered a typical disease of young adults; despite, the age of onset seems to be progressively increasing18. Our result differs from a Danish registry-based study, where the incidence of LOMS is 4.43/100,000 for men and 7.47/100,0009, probably due to the difference in the reference population, that included MS cases up to 64 years old, whereas in our study we have included the whole MS population older than 50 years. Nevertheless, when comparing the incidence rates of our sample in the age range 50–64, our rates were lower for both men (3.55/100,000) and women (5.33/100,000). This difference could be due to the effect of the north-south gradient, since northern countries have consistently showed higher IR, compared to Italy19. A particularly high incidence of LOMS was reported in a study carried out in Iran where the IR both sexes was 17.4/100,000, that according to the authors was due to both the increased diagnostic capabilities of MS centers and genetic predisposition of Iranian natives compared to other ethnicities8.
In our sample LOMS incidence was significantly higher in women compared to men across the 16 years study. However, when stratifying the analyses according to the age classes, this significant difference was present only for the 50–59 age class, and disappeared for the older ages. This testifies a reduction in the female-to-male gradient in the incidence of MS, with the disappearance in subjects over the age of 60, as reported in other studies2,3,8,9,20. Furthermore, comparing the three sub-periods, there is a gradual increase in incidence in the 60–69 years old subgroup, especially when comparing the 2005–2010 and 2016–2020 subperiods. Therefore, a gradual age shift is taking place from LOMS to very late onset multiple sclerosis (VLOMS), defined as MS whose onset occurs at the age of 60 years or older. Possible explanations to this gradual increase in the age at onset can be attributed either to the aging population or to the improvement in the diagnostic accuracy, although a possible role of changing environmental risk factors cannot be ruled out. Interestingly, the increased incidence was significantly higher for men compared to women in the third sub-periods compared to the first. Indeed, the introduction in 2017 of the revised MS diagnostic criteria13 might have led to the inclusion of cases that otherwise would have been diagnosed as cerebrovascular diseases, especially in aging men, where the prevalence of classical risk factors could have suggested alternative diagnoses21,22.
With regard to the clinical features of patients with LOMS, in our study we found that the most frequent clinical presentation is characterized by motor symptoms, followed by sensory symptoms and visual impairment; this differs from the clinical presentation in AOMS, where visual and sensory symptoms are more common3,4,23.
Considering the disease course, the relapse and remitting form was found to be the most frequent, although the percentage of the primary progressive form is higher in LOMS when compared to PPMS prevalence rates in AOMS2,3,4,20,24,25. The higher frequency of PP forms is expected, considering that PPMS usually develops at older ages. Aging affects the mechanisms of disability in MS, shifting towards chronic neurodegeneration. Particularly, key features are represented by chronic demyelination, axonal loss, gray matter atrophy, and smoldering inflammation which is characterized by low-grade, chronic inflammation within the central nervous system (CNS), including microglial activation and the presence of slowly expanding lesions26.
Nevertheless, there is a growing body of evidence that suggest to consider MS as one disease27. Indeed, evidence from pathological studies, genetic and environmental risk factors, treatment responses, and clinical observations supports the view that relapsing and progressive MS are stages of the same disease continuum rather than distinct diseases28. Both relapsing and progressive MS exhibit inflammation and demyelination, though with different intensities and distributions. Inflammation persists throughout the disease course, even in progressive stages26. On the other hand, neurodegeneration, once believed to be exclusive to progressive MS, is now recognized in RRMS as well. MRI studies have shown brain atrophy and grey matter damage early in the disease, indicating that neurodegenerative processes are active from the onset29.
With regard to therapy, half of the patients received DMT and, in particular, one third of these were meDMT. This is in agreement with the literature reporting that, compared to AOMS, there is an increased tendency of reduced prescription of DMT2,20,24. When prescribed, meDMT are preferred even in the absence of clinical trials on DMT in subjects over 50 years of age, probably because of the favourable safety profile30. Indeed, there is still paucity of information regarding efficacy of DMT in LOMS, with only one Italian registry-based study that demonstrated no differences between orally administered and injected DMT in relapsing remitting LOMS patients31.
Our results should be interpreted considering some possible limitations. Case ascertainment might have missed cases that have not been diagnosed or followed-up in the MS centers included in the study, leading to an underestimate of the IR. Nonetheless, it should be noted that several epidemiological studies on MS have been carried out in the same area over the time using the same methodology, and the main sources included patients coming from two MS referral centers also outside the province of Catania. On this ground we are quite confident on the completeness of the case finding and, above all, about the accuracy of the temporal trend. A further limit is related to the IR estimated for the group aged ≥ 70 years that is based on a very small sample, thus limiting generalization in this specific subgroup. Finally, we acknowledge that the lack of follow-up data limits the interpretation of the clinical effects of the different treatment modalities used in LOMS, and does not allow further clinical insights about disability progression and relapse rate.
Our study has several strengths. Incident cases of MS have been confirmed after reviewing the clinical documentation by a neurologist expert in MS, thus excluding cases of other inflammatory diseases of the CNS. Moreover, in order to include cases that might have had the disease onset in 2020 and being diagnosed in the following years, we have extended our observation period into 2024.
Conclusions
Our study is the first population-based study describing the IR of LOMS in a 16-years time period finding an increasing IR over the time, especially in the age-group 60–69, possibly reflecting an increased age at onset of MS. Further longitudinal studies should be conducted in order to confirm our findings.
Data availability
Anonymized data not published within this article will be made available by request to the corresponding author from any qualified investigator.
References
Filippi, M. et al. Multiple sclerosis. Nat. Rev. Dis. Primers 4, 43 (2018).
Andersen, M. A., Buron, M. D. & Magyari, M. Late-onset MS is associated with an increased rate of reaching disability milestones. J. Neurol. 268, 3352–3360 (2021).
Bove, R. M. et al. Effect of gender on late-onset multiple sclerosis. Mult. Scler. 18, 1472–1479 (2012).
Mirmosayyeb, O. et al. Clinical characteristics and disability progression of early- and late-onset multiple sclerosis compared to adult-onset multiple sclerosis. J. Clin. Med. 9, 1326 (2020).
Butler Pagnotti, R., Hua, L. H. & Miller, J. B. Cognition and disease characteristics in adult onset versus late onset multiple sclerosis. Mult. Scler. 28, 933–941 (2022).
Naseri, A., Nasiri, E., Sahraian, M. A., Daneshvar, S. & Talebi, M. Clinical features of late-onset multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 50, 102816 (2021).
Pommerich, U. M. et al. Diet quality is not associated with late-onset multiple sclerosis risk- A Danish cohort study. Mult. Scler. Relat. Disord. 40, 101968 (2020).
Barzegar, M. et al. Prevalence and incidence of multiple sclerosis in Isfahan, Iran between 1996 and 2021: A population-based study. Mult. Scler. Relat. Disord. 84, 105479 (2024).
Koch-Henriksen, N., Thygesen, L. C., Stenager, E., Laursen, B. & Magyari, M. Incidence of MS has increased markedly over six decades in Denmark particularly with late onset and in women. Neurology 90, e1954–e1963 (2018).
Demo - Statistiche demografiche. https://demo.istat.it/.
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the ‘McDonald Criteria’. Ann. Neurol. 58, 840–846 (2005).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69, 292–302 (2011).
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17, 162–173 (2018).
European Commission & Eurostat Revision of the European Standard Population: Report of Eurostat’s Task Force: 2013 Edition (Publications Office, 2013).
Battaglia, M. A. & Bezzini, D. Estimated prevalence of multiple sclerosis in Italy in 2015. Neurol. Sci. 38, 473–479 (2017).
Bezzini, D. et al. Multiple sclerosis incidence in Tuscany from administrative data. Neurol. Sci. 39, 1881–1885 (2018).
Nicoletti, A. et al. Incidence of multiple sclerosis in the province of Catania. A geo-epidemiological study. Environ. Res. 182, (2020).
Romero-Pinel, L. et al. The age at onset of relapsing-remitting multiple sclerosis has increased over the last five decades. Mult. Scler. Relat. Disord. 68, 104103 (2022).
Lane, J., Ng, H. S., Poyser, C., Lucas, R. M. & Tremlett, H. Multiple sclerosis incidence: A systematic review of change over time by geographical region. Mult. Scler. Relat. Disord. 63, 103932 (2022).
Mouresan, E. F. et al. Clinical characteristics and long-term outcomes of late-onset multiple sclerosis: A Swedish Nationwide Study. Neurology 102, e208051 (2024).
Nociti, V., Romozzi, M. & Mirabella, M. Challenges in diagnosis and therapeutic strategies in late-onset multiple sclerosis. J. Pers. Med. 14, 400 (2024).
Sechi, E., Keegan, B. M. & Flanagan, E. P. Applying the 2017 McDonald diagnostic criteria for multiple sclerosis. Lancet Neurol. 17, 498–499 (2018).
Palathinkara, M., Razzak, A. N., Ababneh, O. E., Cairns, D. & Obeidat, A. Z. Clinical and radiologic differences between early onset, late onset, and very late onset adult multiple sclerosis. Mult. Scler. Relat. Disord. 80, 105132 (2023).
Guillemin, F. et al. Older age at multiple sclerosis onset is an independent factor of poor prognosis: A population-based cohort study. Neuroepidemiology 48, 179–187 (2017).
Moura, J. et al. Characterization of a late-onset multiple sclerosis Portuguese cohort. Mult. Scler. Relat. Disord. 70, 104506 (2023).
Frischer, J. M. et al. The relation between inflammation and neurodegeneration in multiple sclerosis brains. Brain 132, 1175–1189 (2009).
Giovannoni, G., Hawkes, C. H., Lechner-Scott, J., Levy, M. & Yeh, E. A. Multiple sclerosis is one disease. Mult. Scler. Relat. Disord. 63, 103961 (2022).
Vollmer, T. L., Nair, K. V., Williams, I. M. & Alvarez, E. Multiple sclerosis phenotypes as a continuum: The role of neurologic reserve. Neurol. Clin. Pract. 11 (4), 342–351 (2021).
Filippi, M. et al. Association between pathological and MRI findings in multiple sclerosis. Lancet Neurol. 11, 349–360 (2012).
Buscarinu, M. C. et al. Late-onset MS: Disease course and safety-efficacy of DMTS. Front. Neurol. 13, 829331 (2022).
Zanghì, A. et al. First-line therapies in late-onset multiple sclerosis: An Italian registry study. Eur. J. Neurol. 28, 4117–4123 (2021).
Acknowledgements
We thank Dr. Luigi Grimaldi (Neurology and Multiple Sclerosis Center, Fondazione Instituto “G. Giglio”, Cefalù, Italy), and Dr. Sebastiano Bucello (Multiple Sclerosis Center – Neurology Unit, ASP8, Augusta, Italy) for the contribution in case ascertainment. This article is supported by the Ministry of University and Research (MUR) as part of the FSE REACT-EU PON 2014-2020 “Research and Innovation” resources – Green/Innovation Action – DM MUR 1062/2021.
Author information
Authors and Affiliations
Contributions
CEC: conceptualization (equal); data curation; formal analysis; writing-original draft (lead); writing-review and editing.CC: data curation; resources; writing-review and editing.GS: data curation; formal analysis; writing-original draft.SLF: data curation; resources; writing-review and editing.GD: data curation; writing-review and editing.DM: data curation; resources; writing-review and editing.RM: data curation; resources; writing-review and editing.FP: data curation; resources; writing-review and editing.AN: conceptualization (lead); formal analysis; writing-review and editing (lead).
Corresponding authors
Ethics declarations
Competing interests
CEC reports no conflict of interest with respect to the research, authorship and publication of this article.CC has received grants for congress participation from Almirall, Biogen, Merck Serono, Novartis, Roche, Sanofi Genzyme, and TEVA.GS reports no conflict of interest with respect to the research, authorship and publication of this article.SLF reports no conflict of interest with respect to the research, authorship and publication of this article.GD reports no conflict of interest with respect to the research, authorship and publication of this article.DM reports no conflict of interest with respect to the research, authorship and publication of this article.RM reports no conflict of interest with respect to the research, authorship and publication of this article.FP has received honoraria for speaking activities by Almirall, Bayer, Biogen, Merck Serono, Novartis, Roche, Sanofi Genzyme, and TEVA; he also served as advisory board member the following companies: Bayer, Biogen, Merck Serono, Novartis, Roche, Sanofi Genzyme, Alexion, and TEVA; he was also funded by Pfizer and FISM for epidemiological studies; he received grants for congress participation from Almirall, Bayer, Biogen, Merck Serono, Novartis, Roche, Sanofi Genzyme, and TEVA. AN reports no conflict of interest with respect to the research, authorship and publication of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cicero, C.E., Chisari, C., Salafica, G. et al. Incidence of late onset multiple sclerosis in Italy: a population-based study. Sci Rep 14, 29649 (2024). https://doi.org/10.1038/s41598-024-81284-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81284-3