Abstract
Cardiovascular complications in patients with autosomal dominant polycystic kidney disease (ADPKD) are frequently investigated extrarenal manifestations with contradictory outcomes. The primary goal of this study is to explore the prevalence of cardiovascular abnormalities using echocardiography and analyze their associations with clinical characteristics at different stages of chronic kidney disease (CKD) progression in ADPKD patients. We included sixty-eight patients in the study. All patients underwent transthoracic echocardiography using GE Vingmed Ultrasound (GE Norway Health Tech, Oslo, Norway). Demographic information, prior medical history, and antihypertensive medication use were recorded. To diagnose the rapid progression of CKD, creatinine levels were measured twice, with a one-year interval. Analysis revealed left ventricular hypertrophy (LVH) in over 40% of ADPKD patients, as indicated by various LVH parameters. Notably, a decline in estimated glomerular filtration rate (eGFR) after one year of observation was associated with increased left ventricular mass. Other prevalent findings included asymptomatic left ventricular diastolic dysfunction (ALVDD) in 39% of patients, left atrium (LA) enlargement in 39%, and mild valvular regurgitations in 80%. Ejection fraction, aortic root dimension, and the prevalence of mitral valve prolapse were not significantly increased. Cardiac indices did not differ substantially across the different eGFR stages. LVH, LA enlargement, ALVDD and valvular regurgitations are characteristics of cardiac phenotype in ADPKD. Cardiac indices were not different across different stages of CKD pointing towards the diagnosis of ADPKD being the main drive of their occurrence.
Similar content being viewed by others
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is the most common hereditary kidney disease, affecting over 12 million people worldwide. It is caused mostly by pathogenic variants in the polycystin 1 and polycystin 2 genes (PKD1 and PKD2)1,2. Deficiency of polycystins, products of the PKD1 and PKD2 genes, leads to kidney failure and it is estimated that approximately 10% of all patients requiring kidney replacement therapy are patients with PKD3.
Importantly, ADPKD is a systemic disease with extrarenal manifestations in many organs, including the cardiovascular system4. Polycystins occur in smooth muscle, vascular endothelium, cardiomyocytes and fibroblasts, they are associated with vascular abnormalities. The cardiac manifestations, such as left ventricular hypertrophy, early onset of hypertension, valvular complications, and pericardial effusions to name a few, result in mortality and morbidity in ADPKD patients estimated to be 1.6- to 3.2-fold higher than in the general population5,6.
It is acknowledged that LVH in ADPKD precedes chronic kidney disease (CKD) and also occurs in non-hypertensive patients7.
Cardiac abnormalities in ADPKD patients are a subject of increasing interest8,9. However, knowledge on this topic is based on observational studies involving small patient groups, resulting in unclear and sometimes contradictory findings. Expanding our understanding of the cardiovascular phenotype of ADPKD, particularly across diverse patient populations and cohorts, is crucial not only for scientific purposes but also for improving treatment strategies and addressing elevated morbidity and mortality risks.
Our study aims to investigate the prevalence of cardiovascular abnormalities using echocardiography and analyze their associations with clinical characteristics at different stages of chronic kidney disease (CKD) progression in ADPKD patients from a single reference center for adults with genetic kidney diseases.
Methods
Patients
Adults, 18 years old or older, referred to our center with a diagnosis of ADPKD between 2017 and 2021, were ordered transthoracic echocardiogram (TTE). The diagnosis of ADPKD was defined on a clinical basis according to Pei-Ravine criteria10.
Exclusion criteria were: prior diabetes, proteinuria of more than 1 g per 24 h, malignancy and history of cardiovascular event, regarded as factors interfering with echocardiographic measurements, independently of ADPKD.
Data collection
Information about demography, prior medical history and taking antihypertension drugs was recorded at the first visit to the clinic. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are referred to in the text as renin-angiotensin system inhibitors (RASi). Anthropometric data was also collected and body mass index (BMI) was calculated from weight and height. We used the Du Bois formula for the estimation of BSA. In all patients, laboratory the following laboratory tests were ordered: creatinine (mg/dL), total serum cholesterol (mg/dL), triglycerides (TG mg/dL), low-density lipoprotein (LDL) (mg/dl), high-density lipoprotein (HDL) (mg/dL) and haemoglobin (Hb) (g/dL). In a few patients, LDL and HDL results were not available due to a technical laboratory problem. Those patients were excluded from the associations’ models.
To diagnose the rapid progression of CKD, creatinine was sampled twice, in a one-year interval. All laboratory tests were performed with validated routine methods at the accredited University Clinical Laboratory. The estimated Glomerular filtration Rate (eGFR) was calculated using the creatinine-based CKD-Epi equation11.
According to calculated eGFR, participants were assigned to one of three groups: I eGFR over 60 ml/min/1,73m2, II eGFR 30-60 ml/min/1,73m2, and III eGFR up to 30 ml/ min/1,73m2.
Rapid progression of kidney failure was defined as the decline of eGFR > / 5 ml/min for a year.
Blood pressure measurement
Blood pressure was calculated by 24-h ambulatory blood pressure measurements (ABPM) Spacelabs 90,217 (Spacelabs Healthcare Company, Issaquah, USA) in the non-dominant arm. Pulse pressure was estimated as the difference between the systolic and diastolic pressure.
TTE methods
Participants were examined by the same single investigator, an experienced cardiologist specialized in echocardiography with the use of GE Vingmed Ultrasound (GE Norway Health Tech, Oslo, Norway). All images were recorded and stored for further analysis. Image quality was evaluated in the 2D parasternal views, apical views and subcostal views. LV Mass, LV Mass index and left atrium diameter (LA) were included in the analysis. The diastolic dysfunction was divided into 4 stages, I-impaired relaxation, II –pseudonormalization, III –restrictive filling (reversible), IV- restrictive filling (irreversible).
Also following valvular disorders were examined: mitral and tricuspid regurgitation, mitral valve prolapse and diastolic dysfunction. The evaluation of regurgitation was classified into mild, moderate and severe. Diagnostic criteria for mitral valve prolapse included systolic displacement of the mitral leaflets being more than 2 mm above the annular plane in the long axis view. All images were interpreted according to the European and American Society of Cardiology Echocardiography Guidelines (ASE)12. According to ASE guidelines we used an upper normal range of 200 g for men and 150 g for women for left ventricular mass (LVM), and for LVd Mass Index, 102 g/m2 for men and 88 g/m2 for women12. End-diastolic interventricular septal wall thickness (IVSD) and posterior wall thickness (LVPWd) reference range were 0.9 cm and 1.0 cm for women and men, respectively. Ejection fraction (EF) was calculated according to Teichholz formula EF = (EDV—ESV) / EDV, where EDV is end-diastolic volume and ESV is end-systolic volume; and Simpson’s Biplane Method.
The study was approved by the Bioethics Committee for Scientific Research at Medical University of Gdansk, Poland (approval No. NKBBN 429/2019). All research was performed in accordance with relevant guidelines and followed the Declaration of Helsinki. Informed consent was obtained from all participants.
Statistical methods
Statistical analyses were performed using the R Project (version 4.1.1; R Core Team, 2021) Distribution measures of the central tendency were given in terms of mean M and standard deviation (SD) for normally distributed variables and in terms of median Mdn and quartiles (Q1 – Q3) for non-normally distributed variables. The normality of distribution was tested using the Shapiro–Wilk test. The Welch t-test was used to compare the means of two normally distributed independent groups and the Mann–Whitney U test for independent groups with non-normal distributions. The calculation of the significance of the differences between the means for more than two normally distributed independent groups was conducted with Welch’s one-way ANOVA. In the case of variables that were not normally distributed, the Kruskal–Wallis test was used. To predict the effects of creatinine level, systolic pressure, diastolic pressure, RAI and beta-blocker medicine use on selected echo parameters [Left atrial end-diastolic volume index (LAEDV Index), LVD Mass, LVd Mass Index (LVDMI)] we chose a multiple linear model. Statistical significance was set at P < 0.05.
Results
Demographic and clinical characteristics of patients
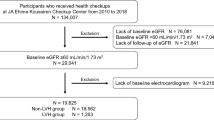
Out of 91 patients who were referred to our centre with ADPKD and underwent echocardiography, 68 patients were eligible to take part in our study. The reasons for exclusion were as follows: neoplasm (n = 1), diabetes (n = 2), prior cardiovascular events (n = 6), pregnancy (n = 1), lack of consent (n = 1), performing TEE in a different center (n = 4), and lost to follow-up (n = 8, attributed to the pandemic) (Supplemental Fig. 1). The median age of study participants was 46 (SD 13) years, most of them were women – 63% (n = 43). The mean estimated glomerular filtration rate (eGFR) in the whole group was 77 mL/min/1.73 m2. All participants were classified into one of three groups according to eGFR: I eGFR over 60 ml/m2, II eGFR 30-60 ml/m2, and III eGFR up to 30 ml/m2. Due to early referral, the majority of the patients were in the first group which consisted of 48 patients. Characteristics of the groups, stratified according to the CKD stage are displayed in Table 1.
For the whole cohort, the mean 24-h systolic blood pressure (SBP) was 134 mmHg (SD 18) and diastolic blood pressure (DBP) was 79 mmHg (SD15).
Among all participants, 46 (69%) were being treated with RAI, 17 (25%) with diuretics, 41 (60%) with beta-blockers, and 20 (29%) with a statin. Rapid progression of kidney failure was present in 9 patients (13.2%).
The data in Table 1 show significant differences between groups that after Dunn’s post-hoc test examination allowed us to conclude that, as expected, the changes in age, SPB, and PP were consistent with the decrease of eGFR. On the other hand, the percentages of sex, mean distributions of anthropometric data and lipidogram did not differ significantly between eGFR groups.
Left ventricular hypertrophy (LVH)
Left ventricular hypertrophy, defined as the LVM mass parameter (an upper normal range of 200 g for men and 150 g for women), was observed in 52% of men (n = 13) and 48.8% of women (n = 21). Mdn LVD mass in men was 129.7 g (Q1-Q3: 99.0 – 215.9) and in women 124.5 g (Q1-Q3: 99.0 – 173.3).
Mdn LVDMI was 114.8 g/m2 (Q1-Q3: 98.6 -147.7) in men and 102.0 g/m2 (Q1-Q3: 94.4 – 113.0) in women. When using the LVDMI method to determine LVH (> 102 g/m2 for men and > 88 g/m2 for women), we found LVH in 42% of men and 47% of women with ADPKD.
Mdn IVSD in men was 1.1 cm (Q1-Q3: 1.0 – 1.1) and in women was 1.0 cm (Q1-Q3: 0.9 – 1.1) and 43% of patients had IVDS > 1.0 cm.
Increased LVPWd was observed in 36.1% of men (Mdn 1.0 cm; Q1-Q3: 1.0 -1.1) and in 48.2% of women (Mdn LVPWd 0.9 cm; Q1-Q3: 0.9–1.0).
Predictors of LVH
Estimated glomerular filtration rate (eGFR) and progression of CKD
Based on the results of the Kruskal–Wallis test, we did not find significant differences in LVD Mass between eGFR groups I-III. The rapid progression of renal failure was not significantly associated with LVD Mass.
Hypertension, anti-hypertensive drugs, lipids and demographic data
LVD Mass and LVd Mass Index were independent of the magnitude of hypertension and intake of drugs with an impact on heart remodelling. Additionally, there were no significant correlations between age, BMI and cholesterol level with LVD Mass and LVD Mass index (Supplemental Table 1).
Determinants of Left ventricular mass using linear regression model
To predict the effects of one-year eGFR decline, the difference between eGFR at t2 and t1 was used as a predictor, ΔeGFR (t2-t1). Also, we analyzed SBP, DBP, RAI and beta-blocker medicine use on selected echo parameters (LVD Mass, LVd Mass Index). We estimated a multiple linear model using ordinary least squares for each response variable separately. The regression model explained a statistically significant and substantial proportion of variance (R2 = 0.39, F(5, 68) = 3.16, p = 0.002, R2adj = 0.26).
The values of the fitted coefficients of the model together with the evidence of significance are shown in Table 2.
The change in eGFR had a significant effect on LVD Mass. Specifically, an increase in creatinine concentration after one year was associated with an increase in LVD Mass.
Pericardial effusion
The measurement of pericardial fluid thickness was performed at end diastole. Remarka-bly, none of the 68 patients showed evidence of pericardial effusion, indicating that their pericardial effusion thickness remained below 3 mm.
Left atrium (LA)
Left atrial enlargement (according to the LAEDV Index, threshold 34 ml/m2) was present in 39.4% of patients. There were no significant differences in the LAEDV index across eGFR groups (I-III).
In Pearson’s correlation analysis, we did not find a correlation between LAEDV index, SBP, DBP and taking antihypertensive drugs.
Echocardiographic parameters according to eGFR
In Table 3 we summarize echocardiographic parameters according to eGFR groups.
Diastolic dysfunction
Diastolic dysfunction occurred in 33 of 68 patients (49%). All patients with impaired left ventricular relaxation were included in stage I (impaired relaxation) of 4 stages in diastolic dysfunction classification,as described in the method section.
The data in Table 4 show that patients with higher systolic pressure, BMI, and total cholesterol levels and patients taking beta-blockers were significantly more likely to have diastolic dysfunction. Similarly, diastolic dysfunction was detected significantly more often in patients with low eGFR at both time points. However, the highest association with the occurrence of diastolic dysfunction was found with increasing age of the patients.
In contrast, changes in diastolic blood pressure, use of RAI and diuretics, and increased or decreased triglyceride, HDL, and LDL levels were not significantly correlated with the occurrence of diastolic dysfunction.
Aortic root
Only one patient had Ao > 4.3 cm. Median Ao diameter in our group was 3.4 [3.2- 3.6] cm. There were no differences in Ao diameter between eGFR groups.
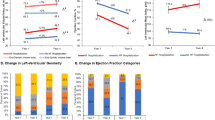
Prevalence of valvular defects
The most frequently diagnosed valvular defects were mitral and tricuspid valve regurgitation. All of these regurgitations were characterized as mild. Mitral valve prolapse (MVP) was found only in two patients (3%) (Fig. 1).
Discussion
This study aimed to assess the prevalence of structural and functional cardiac abnormalities in a group of ADPKD patients, classified according to eGFR. Alterations of the cardiovascular system in ADPKD have been known for almost 40 years13. Similarly to other phenotypic manifestations, the cardiac and vascular phenotype of ADPKD is highly diverse. Little is certain about cardiovascular involvement in ADPKD, beyond the early onset of arterial hypertension, increased incidence of LVH and valvular abnormalities.
The main outcome of our study is the high prevalence of LVH, which occurred in above 40% of study participants, independent of which LVH indicator we used (LVd Mass, LVMI, IVSD or LVPWd). Likewise, in a recent analysis of 103 patients with ADPKD, before kidney transplantation, LVH was found in 46.6%9. A similar percentage (48%) of patients with ADPKD had LVH in a study by Chapman et al.14 Finally, when LVH was defined by IVSD > 10 mm, it was present in 43% of our patients, as compared to 66% observed in the cohort described by Arjune et al.15 These numbers are alarming, given that LVH is an important risk factor for premature cardiovascular death in ADPKD4.
Interestingly, the occurrence of LVH in our study was independent of hypertension and antihypertensive therapy, including RAI. Hypertension was diagnosed in 60% of our patients, in agreement with previous findings of its prevalence in ADPKD, estimated at 50–70%5,16. Some studies report increased LVMI in young normotensive patients independently of BP14, while others claim its dependence on BP17. A single associate of LVMass, in our study, was eGFR decline after one year of observation. However, there was no difference between study groups divided according to eGFR measured at the time of TTE. This goes in line with the findings of the HALT–PKD study, in which there was no relationship between eGFR and LVMI measured by MRI18.
Based on our observation, LVH could be a predictor of the severity of ADPKD as it is associated with the steepness of eGFR decline after a year of observation. Our finding is further supported by the studies reporting a correlation between LVMI or IVSD and total kidney volume, another surrogate of ADPKD progression15,19. This is quite natural when taking into account the systemic nature of ADPKD and the fact that polycystins are found in all cells of the cardiovascular system. Endothelial dysfunction is an early feature of vascular damage in ADPKD patients, followed by stiffening of the large elastic arteries, increased pulse wave velocity and PP20,21,22.
Asymptomatic left ventricular diastolic dysfunction (ALVDD) is a common finding in the general population and is increasingly found with rising age. Nevertheless, the prevalence of ALVDD was unexpectedly high in our group, found in 49% of patients, especially in comparison to 27% observed in the population of adults with a mean age of 52 years23. Again, the main determinant of the ALVDD finding was age, of note our patients were significantly younger (mean age 46 years) but still the prevalence was much higher. Increased creatinine, SBP, BMI, and total cholesterol levels were associated with the diagnosis of ALVDD following a trait observed in other studies in the general population and ADPKD24,25. We also found a higher risk of ALVDD in patients taking beta-blockers and this needs further attentiveness. This finding is concerning, given the recent evidence suggesting potential negative effects of beta-blockers in heart failure with preserved ejection fraction (HFpEF)26,27. In both mentioned studies, the higher the ejection fraction, the higher the risk of hospitalization due to HF. If we treat ALVDD as a risk factor for developing HFpEF, our data are pointing in the same direction that the studies of Arnold et al. and Silverman et al.26,27 It raises the question of whether beta-blockers are a good choice for young ADPKD patients with increased HFpEF risk and a perspective of many years on treatment. A beta-adrenergic signaling pathway is changed in the heart cells of PKD2 knockout mice, which may offer a rationale for our finding28. The abovementioned findings again point to advocating early echocardiographic examination in ADPKD.
Patients with ADPKD are regarded to have also an increased risk of atrial fibrillation (AF)29. Several factors may contribute to AF, but the atrial dimension and the activation of the autonomic nervous system are the key determinants. No need to mention that both are found in ADPKD, along with overactivation of the RAAS and disrupted calcium handling29. Left atrial enlargement expressed as increased LAEDV Index was present in 39.4% of patients in our study, the same as reported in the study from the Mayo Clinic (39.3%).
The high prevalence of vascular aneurysms belongs to the phenotype of ADPKD. As Ao diameter is a predictor of the occurrence of aortic aneurysm, we expected to find this parameter increased in our patients. It was not the case. Alike the observation from the AD(H)PKD cohort15, only one man had substantially increased Ao value.
Along with Ajurne et al., we are the first to report the high prevalence of tricuspid regurgitation (TR) in patients with ADPKD (> 80%). All our patients had a mild class of TR and measurement of right ventricular systolic function (TAPSE) was within the norm across all eGFR groups. We found a similar frequency of mitral valve regurgitation (MVR) to the AD(H)PKD cohort (70% and 63%, respectively)15. It was higher than the numbers reported in cohorts from Japan, Brazil and the United States9,30,31. The development of the echocardiographic technique may explain to some extent the highest sensitivity in Germany and in our cohort, especially since our data are the most recent.
The major weakness of our study is the likely selection bias due to the enrolment of patients exclusively from a tertiary care institution. This difficulty is hard to overcome in many studies on ADPKD. Another limitation is the lack of a control group of individuals without ADPKD for comparisons. Most authors refer ADPKD to a healthy population while adjusting for age, hypertension and stage of CKD should be assured. This is almost unattainable. We decided to compare our findings to European references from echocardiography guidelines that delineate the norm and pathology. Also, we adjusted for age, BP and eGFR in our multivariate models.
In the present study, we confirm that ADPKD patients with well-preserved renal function have substantially higher LVH. Beyond hypertension, other factors—such as the rate of eGFR decline over a year—contribute to the enlargement of the left ventricle. Additionally, we identified LA enlargement, diastolic dysfunction, and valvular regurgitations as characteristic features of the cardiac phenotype in ADPKD. Interestingly, cardiac indices did not differ significantly across various stages of CKD, suggesting that the ADPKD diagnosis itself plays a central role in their occurrence. Our data provides evidence towards advocating the TTE examination early in the course of the disease. While our study primarily confirmed established findings, it also raised a few novel concerns, including a question about the benefits of prescribing beta-blockers for ADPKD patients.
Data availability
Data supporting reported results can be obtained from the Magdalena Jankowska on a valid reason upon request.
References
Torres, V. E., Harris, P. C. & Pirson, Y. Autosomal dominant polycystic kidney disease. Lancet 369(9569), 1287–1301 (2007).
Cornec-Le Gall, E., Alam, A. & Perrone, R. D. Autosomal dominant polycystic kidney disease. Lancet 393(10174), 919–935 (2019).
Zeier, M., Jones, E. & Ritz, E. Autosomal dominant polycystic kidney disease–the patient on renal replacement therapy. Nephrol Dial Transplant. 11(Suppl 6), 18–20 (1996).
Ecder, T. & Schrier, R. W. Cardiovascular abnormalities in autosomal-dominant polycystic kidney disease. Nat Rev Nephrol. 5(4), 221–228 (2009).
Chapman, A. B., Stepniakowski, K. & Rahbari-Oskoui, F. Hypertension in autosomal dominant polycystic kidney disease. Adv Chronic Kidney Dis. 17(2), 153–163 (2010).
Kuo, I. Y. & Chapman, A. B. Polycystins, ADPKD, and Cardiovascular Disease. Kidney Int Rep. 5(4), 396–406 (2020).
Schrier, R. W. Renal volume, renin-angiotensin-aldosterone system, hypertension, and left ventricular hypertrophy in patients with autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 20(9), 1888–1893 (2009).
Chebib, F. T. et al. Autosomal Dominant Polycystic Kidney Patients May Be Predisposed to Various Cardiomyopathies. Kidney Int Rep. 2(5), 913–923 (2017).
Chedid, M. et al. Cardiovascular Outcomes in Kidney Transplant Recipients With ADPKD. Kidney Int Rep. 7(9), 1991–2005 (2022).
Pei, Y. et al. Unified criteria for ultrasonographic diagnosis of ADPKD. J Am Soc Nephrol. 20(1), 205–212 (2009).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 150(9), 604–612 (2009).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 28(1), 1-39.e14 (2015).
Leier, C. V., Baker, P. B., Kilman, J. W. & Wooley, C. F. Cardiovascular abnormalities associated with adult polycystic kidney disease. Ann Intern Med. 100(5), 683–688 (1984).
Chapman, A. B. et al. Left ventricular hypertrophy in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 8(8), 1292–1297 (1997).
Arjune, S. et al. Cardiac Manifestations in Patients with Autosomal Dominant Polycystic Kidney Disease (ADPKD) A Single-Center Study. Kidney360. 4(2), 150–161 (2023).
Ecder, T. & Schrier, R. W. Hypertension in autosomal-dominant polycystic kidney disease: early occurrence and unique aspects. J Am Soc Nephrol. 12(1), 194–200 (2001).
Bardají, A. et al. Cardiac involvement in autosomal-dominant polycystic kidney disease: a hypertensive heart disease. Clin Nephrol. 56(3), 211–220 (2001).
Chapman, A. B. et al. The HALT polycystic kidney disease trials: design and implementation. Clin J Am Soc Nephrol. 5(1), 102–109 (2010).
Cadnapaphornchai, M. A., McFann, K., Strain, J. D., Masoumi, A. & Schrier, R. W. Increased left ventricular mass in children with autosomal dominant polycystic kidney disease and borderline hypertension. Kidney Int. 74(9), 1192–1196 (2008).
Nowak, K. L. et al. Vascular Dysfunction, Oxidative Stress, and Inflammation in Autosomal Dominant Polycystic Kidney Disease. Clin J Am Soc Nephrol. 13(10), 1493–1501 (2018).
Karava, V. et al. Early cardiovascular manifestations in children and adolescents with autosomal dominant polycystic kidney disease: a single center study. Pediatr Nephrol. 33(9), 1513–1521 (2018).
Koska-Ścigała, A., Jankowska, M., Szyndler, A., Narkiewicz, K. & Dębska-Ślizień, A. Ambulatory pulse pressure and its contributors in autosomal dominant polycystic kidney disease. Adv Clin Exp Med. 31(5), 575–578 (2022).
Kuznetsova, T. et al. Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail. 2(2), 105–112 (2009).
Kane, G. C. et al. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 306(8), 856–863 (2011).
de Almeida, E. A. et al. Diastolic function in several stages of chronic kidney disease in patients with autosomal dominant polycystic kidney disease: a tissue Doppler imaging study. Kidney Blood Press Res. 30(4), 234–239 (2007).
Arnold, S. V. et al. Beta-Blocker Use and Heart Failure Outcomes in Mildly Reduced and Preserved Ejection Fraction. JACC Heart Fail. 11(8 Pt 1), 893–900 (2023).
Silverman, D. N. et al. Association of β-Blocker Use With Heart Failure Hospitalizations and Cardiovascular Disease Mortality Among Patients With Heart Failure With a Preserved Ejection Fraction: A Secondary Analysis of the TOPCAT Trial. JAMA Netw Open. 2(12), e1916598 (2019).
DiNello, E. et al. Deletion of cardiac polycystin 2/PC2 results in increased SR calcium release and blunted adrenergic reserve. Am J Physiol Heart Circ Physiol. 319(5), H1021–H1035 (2020).
Yu, T. M. et al. New-onset Atrial Fibrillation is Associated With Polycystic Kidney Disease: A Nationwide Population-based Cohort Study. Medicine (Baltimore). 95(4), e2623 (2016).
Miyamoto, R. et al. Echocardiographic Findings and Genotypes in Autosomal Dominant Polycystic Kidney Disease. Kidney Dis (Basel). 8(3), 246–252 (2022).
Pfeferman, M. B., Rocha, D. R. D., Rodrigues, F. G., Pfeferman, E. & Heilberg, I. P. Echocardiographic Abnormalities in Autosomal Dominant Polycystic Kidney Disease (ADPKD) Patients. J Clin Med. https://doi.org/10.3390/jcm11205982 (2022).
Acknowledgements
This study was partially supported by a grant from the National Science Centre, Kraków, Poland (No. 2018/30/M/NZ5/00480).
Funding
This research was funded by a grant from the National Science Centre, Kraków, Poland (No. 2018/30/M/NZ5/00480).
Author information
Authors and Affiliations
Contributions
Conceptualization, M.J. and A. K-S.; methodology, M.J., H.J., M.D., M.H; investigation, H.J.; resources, M.J.; data curation, A.K-S.; writing—original draft preparation, A.K-S.; writing—review and editing, M.J.; visualization, A.K-S and M.J.; supervision, A.D-S.; project administration, M.J and H.J; funding acquisition, M.J.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Koska-Ścigała, A., Jankowska, H., Jankowska, M. et al. Echocardiographic characteristics of autosomal dominant polycystic kidney disease. Sci Rep 14, 29867 (2024). https://doi.org/10.1038/s41598-024-81536-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81536-2