Abstract
Raynaud’s phenomenon is a condition that causing vasospasm of the digital extremities and have a great influence on the quality of patients life. Distraction osteogenesis is accompanied with vascularization and regeneration of surrounding soft tissues. There have been no previous reports of using radial cortex transverse distraction for the treatment of RP. Since January 2019 to January 2023, 6 patients with RP accepted radial cortex transverse distraction. They were failed to conventional treatment for at least six months before the surgery. All the patients were followed-up over 1 year. The bone cortex healed without osteomyelitis or fractures. The ulcer of finger healed in one month. The pain and skin pale released after the surgery. The VAS score declined from 6 to 2 and the finger SpO2 improved. Radial cortex transverse distraction facilitated finger ulcer healing, salvage the hand and improved Raynaud symptoms. These findings suggest that radial cortex transverse distraction may be an effective procedure to treat the Raynaud’s phenomenon.
Level of Evidence II Therapeutic study.
Similar content being viewed by others
Introduction
Raynaud’s Phenomenon (RP) is an ischemic disorder resulting from vasospasm because of various etiologies. It can cause immense pain and pale of digital extremities, lead to ulceration, gangrene and amputation of digits1. The incidence rate of RP ranges from 3 to 21%, and is 10 times higher in females than in males2.
The etiology is not yet clear, but ischemia is believed to be the result of an imbalance between vasodilation and vasoconstriction factors3. Clinical manifestations are the main diagnostic basis of primary RP.
Conservative treatment options for Raynaud’s phenomenon include lifestyle modifications, such as avoiding cold environments, quitting smoking and using vibration tools, and minimizing stress and anxiety. Oral medications consisting of calcium-channel blockers, prostacyclins, nitroglycerin ointments, and some new drugs, such as phosphodiesterase inhibitors, endothelin receptor antagonists, and serotonin receptor antagonists, have been used and achieved some effects2. However, the efficacy of these drugs varies, and there is no universally effective treatment plan.
Periarterial sympathectomy is another treatment method used for refractory RP4. But the use of this method was affected by the complications caused by long incisions and the high recurrence rate5,6,7. Sympathetic blocks with ropivacaine and clonidine are valuable in preventing morbidity from Raynaud’s phenomenon8. Injection of botulinum toxin may be an effective method for the treatment of refractory RP, as suggested by small-scale studies9,10. However, there is currently not enough evidence to evaluate the efficacy of botulinum toxin A in the Raynaud’s phenomenon2,11. When traditional therapies fail, surgery becomes the next available option.
RP results in the ischemic necrosis and discoloration of digits due to disorders of vasodilation and vasoconstriction, and treatments aim to regenerate new vessels. Distraction osteogenesis has been shown to induce large new bone formation, accompanied by neovascularization and increased blood circulation of soft tissues and bone12,13,14,15. The longitudinal traction of the proximal tibia could stimulate increased tibial perfusion and bone elongation16. Transverse distraction of the tibial cortex had been clinical used for the treatment of local ischemic diseases, such as diabetic foot ulcers17,18.
There have been no previous reports of using radial cortex transverse distraction for the treatment of RP. The purpose of this study is to report the use of radial transverse distraction for the management of refractory RP disease, including techniques, contraindications, and complications.
Materials and methods
Inclusion and exclusion criteria
We retrospectively analyzed patients data from January 2019 to January 2023. The inclusion criteria followed these principles: (1) patient was diagnosed with RP by rheumatology experts, (2) finger pain and pale persisted, or ulcers and gangrene occurred after the patient received standard drug treatment for three months, (3) patient agrees to undergo the surgical treatment.
The exclusion criteria included: (1) patient who have ulcers and gangrene with infection, (2) systemic diseases that were not controlled by drug treatment, (3) inability to tolerate 2 months external fixation.
The study was approved by the Research Ethics Committee of Qilu Hospital of Shandong University. The patients were ranged from 44 to 68 years old, and they had been experiencing symptoms for 6 to 18 months. Bilateral upper limbs were involved in all 6 patients. Baseline pain scores were assessed using the Visual Analogue Scale (VAS), finger discoloration and oxygen saturation (SpO2) of all digits were recorded (Table 1). Informed consent were obtained from all patients.
Surgical techniques
The patients under brachial plexus block anesthesia or general anesthesia while in the supine position with upper arm tourniquet. The corticotomy window was designed on the distal 1/3 of radius. About 6 cm long curved skin incision, was made on the radial dorsal forearm. The subcutaneous soft tissue was freed and stretched and the radial periosteum was carefully exposed. A rectangular osteotomy (4 cm x 1.5 cm) was created on the radial cortex of the distal radius after drilling multiple holes along the four sides (proximal, distal, medial, and lateral) of the rectangle. The small model of external fixtor for tibial cortex transverse distraction was used to do the radius transverse distraction. After pre-drilling, two 2.5 mm half-pins were inserted into radial cortex in the osteotomized bone to do the transverse transport, another two 3.5 mm half-pins were implanted on the proximal and distal side to stabilize the external fixtor. The position of the pins and the boundary of osteotomy were confirmed through fluoroscopy. The stable distraction apparatus were assembled with modular components to do the cortex transverse distraction, about 2.0 cm space was left between the skin and external fixator.
Aftercare
Wound dressing changes daily to keep the wound clean, and pins care was administered every 2 or 3 days. Postoperative radiography was taken to confirm the position of pins and the corticotomy boundary. latent period is 3 days to rule out the complications such as local infection or skin necrosis. Radial cortex distraction was initiated at a rate of 0.25 mm every six hours. Patients were discharged from the hospital and completed radius distraction at home: 14 days of radial direction distraction followed by 14 days of return distraction, similar to the Ilizarov violin technique. Radiography was performed at 14 and 28 days after bone distraction to confirm the position of the cortex. Wound care and the protective brace were applied for patients. Early partial mobilization with active and passive exercises of the hand, wrist, and elbow was allowed. The external fixator was removed at about 6 weeks post operation, after the radial cortex bone reducted and stable.
The patients were followed up weekly during the first 8 weeks after the operation. Baseline pain score, color and temperature of hand, oxygen saturation (SpO2) of all digits and Raynaud Condition Score were recorded. Hand-holding activities were allowed. After removal the external fixator, further follow-up was conducted every month until 1 year.
The Shapiro-Wilk test was utilized to evaluate the normality of the data. The measurements that conformed to the normal distribution were expressed as mean ± standard deviation, and the two independent samples t-test was conducted. The p value less than 0.05 was considered statistically significant.
Results
The patients reported significant relief of pain after the surgery in 3 weeks, with a decrease in the baseline VAS score from 7 to 1. An increase in hand temperature and improvement in SpO2 in almost all digits were observed in all patients compared to pre-operation (see Table 2). Discoloration of the hands was resolved, the ulcers improvement was observed in all cases with the course of reduced area, granulation growth and partial healing, ulcers in two cases had completely healed by three months. All patients achieved successful finger salvage (without major amputations) and did not experience recurrence within one year. The incision healed without infection or skin necrosis. The Raynaud Condition Score of patients has significant improved at 1 year after the surgery. Complications after radial transverse distraction were few and minor. One patient experienced minor wrist dysfunction due to fixation, wrist function returned to normal after two months of exercise. No pin site infections occurred. The radial cortex achieved satisfactory union in all patients. These results were recorded by two assessors who did not participate in the operations.
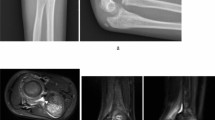
All patients reported their symptoms have improved, especially on pain symptom. There is no symptom worsen after the radial osteotomy, the pain symptom reduced during the cortex distraction and reduction. The hand temperature and finger color improved after the cortex distraction.Typical case was shown in Fig. 1.
The patient suffered RP for 4 years and accepted drug treatment. Her disease aggravated and both of her distal index fingers were amputated because of gangrene 1 year ago. Both of her middle fingers reserved discoloration and the end of finger began to gangrene. 1–3 The version of discolored digits and gangrene of middle finger. 4 The surgery was performed on the distal 1/3 radial. 5 The soft tissue was retracted and the periosteum was exposed.Corticotomy was performed by drilling multiple holes in a rectangle (4.0 cm*1.5 cm) in the cortex. two 2.5 mm pins were drilled into radial cortex in the osteotomized bone to do the transverse distraction. 6 Two 3.5 mm pins were fixed to the radial bone to stabilize the external frame. 7 The apparence of forearm after 2-week distraction. 8 The lateral x-ray of corticotomy window and external fixator 2 days after the surgery. 9 The cortex fragment transported laterally and was away from the radial shaft after 2 weeks of distraction. 10 The X-ray of radial 2 months after removal of the external fixation. 11–12 The ulcer healed and the discoloration and pain of digits disappeared.
Discussion
Distraction osteogenesis is accompanied by angiogenesis and neovascularization in surrounding soft tissues13,19,20. Transverse distraction with corticotomy, including iliac and tibial, is an new and useful surgical technique for the treatment of severe chronic limb ischemic diseases18,21. The effective of tibial cortex transverse distraction in the treatment of diabetic foot ulcers had been verified. During a two-year follow-up study, tibial cortex transverse distraction therapy resulted in a greater likelihood of healing and cure and a lower proportion of severe amputations and relapses22. After treatment with tibial cortex transverse distraction, neovascularization and increased microcirculation were observed in the diabetic foot, consistent with animal studies17,23,24. Since transverse distraction can lead to angiogenesis and neovascularization of limbs, we hypothesized that radial transverse transplantation could increase blood irrigation and improve the ischemic symptoms of RP.
RP was first described by Maurice Raynaud as a condition of transient and reversible discoloration triggered with cold exposure, and various conditions leading to ischemic outcomes1,25. RP is an general term for the blanching condition of digital vascular spasm.The skin initially blanches then followed by cyanosis because of eoxygenation of venous blood, and then rubor due to reactive hyperemia after return of flow, resulting in the classical “triphasic color change‘’26. RP includes both Primary Raynaud’s phenomenon (PRP) and Secondary Raynaud’s phenomenon (SRP). Most patients with RP have an associated underlying systemic disease and RP may predate systemic illness by up to 20 years. Low average daily temperature, anxiety, stress, and female gender maybe the predictors for RP severity and pain. The treatment of RP and digital ulceration remains unsatisfactory, so new approaches need to continue to be explored. Long-term studies are needed to investigate combination therapies and potential vascular remodeling therapies27.
In this study, we assessed the efficacy of radial cortex transverse distraction in the treatment of RP. Healed digits showed increased blood perfusion in the hand during follow-up compared to pre-operation. An increase in hand temperature and an improvement in SpO2 in almost all fingers were observed in the patients compared to pre-operation. The preoperative Temp was 29.6 ± 0.8℃, and the postoperative 6 month follow-up temperature was 33.3 ± 1.0℃, with a statistically significant difference compared with the preoperative score (p < 0.001). The preoperative RCS was 7.2 ± 0.7, and the postoperative 6 month follow-up RCS was 3.2 ± 0.5, with a statistically significant difference compared with the preoperative score(p ≤ 0.05). However, the RCS scores were subject to the influence of climatic factors, patient subjective factors, and the like. Nonetheless, they were consistent with the findings related to the improvement in pain scores as well as the manifestation of Raynaud’s phenomenon with respect to skin temperature, the RCS scores were all significantly improved from preoperative levels.
All patients achieved successful finger salvage (without pain, dislocation, or major amputations) and did not experience recurrence within one year. Complications after radial transverse distraction were few and minor. Although one patient experienced minor dysfunction due to fixation, she recovered to normal function one month later after active exercise. Radial osteotomized cortex achieved satisfactory union. These suggest that radial cortex transverse distraction is an effective method for treating severe RP.
We chose the radial bone for distraction because it is close to the hand, has enough width for distraction of the bone fragment, and is easy to expose. The site was selected on the distal dorsal radial because this area is close to neurovascular bundles and has high perfusion. Fractures in this area generally heal easily. The diaphyseal of the distal radial is larger than the other proximal regions, reducing the risk of surgical induced fracture. We selected corticotomy on the dorsal part rather than the palmar of the radial because the dorsal surface is flat and the median nerve is in the palmaris. This makes the corticotomy procedure easier and causes less soft tissue injury.
Limitations of this study. The number of patients was only 6, and this was a non-randomized trial. Second, no objective measurements for gains of radial transverse distraction. The improvement in clinical parameters points to a clear benefit of these treatments. Further research is needed to elucidate the mechanisms of this procedure.
Conclusion
In conclusion, radial cortex transverse distraction could decrease pain, increase blood perfusion, facilitate ulcer healing, and salvage limbs effectively. Additionally, radial transverse distraction has relatively few and minor complications. Radial cortex transverse distraction may be a promising procedure for treating RP compared to other surgical therapies.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
References
Choi, E., Henkin, S. & Raynaud’s phenomenon and related vasospastic disorders. Vasc. Med. (London, England) 26(1), 56–70. https://doi.org/10.1177/1358863X20983455 (2021).
Gallegos, J. E., Inglesby, D. C., Young, Z. T. & Herrera, F. A. Botulinum toxin for the treatment of intractable Raynaud phenomenon. J. Hand. Surg. 46(1), 54–59. https://doi.org/10.1016/j.jhsa.2020.07.009 (2021).
Neumeister, M. W. et al. Botox therapy for ischemic digits. Plast. Reconstr. Surg. 124(1), 191–201. https://doi.org/10.1097/PRS.0b013e3181a80576 (2009).
Flatt, A. E. Digital artery sympathectomy. J. Hand. Surg. 5(6), 550–556. https://doi.org/10.1016/s0363-5023(80)80104-3 (1980).
McCall, T. E., Petersen, D. P. & Wong, L. B. The use of digital artery sympathectomy as a salvage procedure for severe ischemia of Raynaud’s disease and phenomenon. J. Hand. Surg. 24(1), 173–177. https://doi.org/10.1053/jhsu.1999.jhsu24a0173 (1999).
Van Der Stricht, J. P. Traitement Chirurgical Du phénomène De Raynaud [Surgical treatment of Raynaud’s phenomenon]. Rev. Med. Liege 35(19), 654–655 (1980).
Merritt, W. H. Role and rationale for extended periarterial sympathectomy in the management of severe Raynaud syndrome: Techniques and results. Hand Clin. 31(1), 101–120. https://doi.org/10.1016/j.hcl.2014.09.011 (2015).
Punj, J. et al. Sympathetic blocks for Raynaud’s phenomena in pediatric rheumatological disorders. Pain Med. (Malden, Mass.) 23(7), 1211–1216. https://doi.org/10.1093/pm/pnac015 (2022).
Shwe, S., Sharma, A. A., Chahal, H. S., Doan, L. T. & Rojek, N. W. Botulinum toxin for the treatment of intractable Raynaud phenomenon. Cutis 108(3), E11–E14. https://doi.org/10.12788/cutis.0355 (2021).
Nagarajan, M. & McArthur, P. Targeted high concentration botulinum toxin a injections in patients with Raynaud’s phenomenon: A retrospective single-centre experience. Rheumatol. Int. 41(5), 943–949. https://doi.org/10.1007/s00296-020-04606-4 (2021).
Żebryk, P. & Puszczewicz, M. J. Botulinum toxin A in the treatment of Raynaud’s phenomenon: A systematic review. Arch. Med. Sci.AMS 12(4), 864–870. https://doi.org/10.5114/aoms.2015.48152 (2016).
Gubin, A. V., Borzunov, D. Y., Marchenkova, L. O., Malkova, T. A. & Smirnova, I. L. Contribution of G.A. Ilizarov to bone reconstruction: Historical achievements and state of the art. Strateg. Trauma. Limb Reconstr.. 11(3), 145–152. https://doi.org/10.1007/s11751-016-0261-7 (2016).
Ilizarov, G.A. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin. Orthop. Relat. Res. 238, 249–281 (1989).
Ilizarov, G.A. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin. Orthop. Relat. Res. 239, 263–285 (1989).
Ilizarov, G. A. Clinical application of the tension-stress effect for limb lengthening. Clin. Orthop. Relat. Res. 250, 8–26 (1990).
Aronson, J. Temporal and spatial increases in blood flow during distraction osteogenesis. Clin. Orthop. Relat. Res. 301, 124–131 (1994).
Chen, Y. et al. Proximal tibial cortex transverse distraction facilitating healing and limb salvage in severe and recalcitrant diabetic foot ulcers. Clin. Orthop. Relat. Res. 478(4), 836–851. https://doi.org/10.1097/CORR.0000000000001075 (2020).
Fan, Z. Q., Yu, Z. H., Zheng, J. Z., Yu, B. F. & Liu, D. W. Tibial cortex transverse distraction in treating diabetic foot ulcers: What are we concerned about? J. Int. Med. Res. 48 (9), 300060520954697. https://doi.org/10.1177/0300060520954697 (2020).
Matsuyama, J. et al. Osteogenesis and angiogenesis in regenerating bone during transverse distraction: Quantitative evaluation using a canine model. Clin. Orthop. Relat. Res. 433, 243–250. https://doi.org/10.1097/01.blo.0000150562.24256.a4 (2005).
Ohashi, S., Ohnishi, I., Kageyama, T., Imai, K. & Nakamura, K. Distraction osteogenesis promotes angiogenesis in the surrounding muscles. Clin. Orthop. Relat. Res. 454, 223–229. https://doi.org/10.1097/01.blo.0000238795.82466.74 (2007).
Liu, Y. et al. Anterior superior iliac spine distraction for severe and recalcitrant diabetic foot ulcers. Injury 54(2), 778–783. https://doi.org/10.1016/j.injury.2022.11.070 (2023).
Li, Y. X. et al. Tibial cortex transverse distraction followed by open correction with internal fixation for management of foot and ankle deformity with ulcers. Orthop. Surg. 13(7), 2081–2092. https://doi.org/10.1111/os.13148 (2021).
Thaller, P. H., Fürmetz, J., Böcker, W. & Ehrnthaller, C. Transverse kallusdistraktion: Neue Chancen für den Extremitätenerhalt? [Transverse distraction osteogenesis: New chances for limb salvage?]. Der Unfallchirurg. 125(4), 282–287. https://doi.org/10.1007/s00113-022-01156-1 (2022).
Grüneboom, A. et al. A network of trans-cortical capillaries as mainstay for blood circulation in long bones. Nat. Metab. 1(2), 236–250. https://doi.org/10.1038/s42255-018-0016-5 (2019).
Herrick, A. L. & Wigley, F. M. Raynaud’s phenomenon. Best Pract. Res. Clin. Rheumatol. 34(1), 101474. https://doi.org/10.1016/j.berh.2019.101474 (2020).
Belch, J. et al. ESVM guidelines - the diagnosis and management of Raynaud’s phenomenon. VASA Z. fur Gefasskrankheiten. 46(6), 413–423. https://doi.org/10.1024/0301-1526/a000661 (2017).
Herrick, A. L. Raynaud’s phenomenon and digital ulcers: Advances in evaluation and management. Curr. Opin. Rheumatol. 33(6), 453–462. https://doi.org/10.1097/BOR.0000000000000826 (2021).
Funding
This research was supportted by the Natural Science foundation of Shandong Province, ZR2023MH368.
Author information
Authors and Affiliations
Contributions
Zhihu Ma, Li Qiao and Lei Zhu wrote the main manuscript text, Yidong Cui, Ruowen Zhu, Xingsheng Zhang prepared figure and tables. Qingjia Xu, Yantao Pei, Gang Wang followed up the patients. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Qilu Hospital of Shandong University. All procedures performed in this study involving human participants followed the relevant guidelines and regulations of the Declaration of Helsinki.
Informed consent
All patients in our study were anonymous. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, Z., Qiao, L., Cui, Y. et al. Radial cortex transverse distraction help to treat the Raynaud’s phenomenon. Sci Rep 14, 29984 (2024). https://doi.org/10.1038/s41598-024-81612-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81612-7