Abstract
Sertraline is one of the drugs whose transport from the blood circulation to the brain is severely limited by the blood–brain barrier and it shows low bioavailability (44%). Liposomes can be an effective carrier for this drug and increase bioavailability. In this study, the synthesis of nanometer-sized liposomes containing sertraline hydrochloride is proposed using a technique called supercritical fluid expansion into aqueous solution (ESSAS). In this technique, phospholipid precipitation rates are controlled, and homogeneous liposomes with nanometer-sized dimensions can be created. The operational parameters were optimized using the response surface methodology (pressure drop: 29.9 MPa, collection time: 13.6 min, temperature: 40 °C), which showed that the optimal values for the encapsulation efficiency, mean size, and number of liposomes were 78.4%, 89.5 nm, and 85, respectively. Also, the drug release test showed that it takes 27 h for sertraline to be completely released from the liposomal suspension.
Similar content being viewed by others
Introduction
Nanotechnology has recently gained traction in various industries, including cosmetics, pharmaceuticals, medical, food, and environmental studies. Major pharmaceutical research has focused on drug delivery systems (DDS) and nanocarrier developments. Drug delivery is the process of introducing a medicinal substance into the human body using appropriate pharmacokinetics to achieve the intended effect1,2. One of the most promising approaches to drug delivery systems is the development of nanocarriers, which significantly improve drug pharmacokinetics, reduce toxicity, and improve therapeutic efficacy and biocompatibility. Lipidic and polymeric particles, hydrogels, membranes, emulsions, microspheres, and other molecular complexes are examples of drug delivery systems that have been expanded for the treatment ofhuman ailments3.
Sertraline, a selective serotonin reuptake inhibitor (SSRI) used in psychiatry to treat major depressive disorder, is one of the drugs whose transport from systemic circulation to the brain is significantly limited by the BBB4,5. Furthermore, this medicine has a low water solubility, which causes it to accumulate after oral ingestion and interaction with the gastrointestinal fluid coating. As a result of the aforementioned causes, its absorption is slow/weak and exhibits a low bioavailability (44%). It is hoped that adding sertraline hydrochloride to lipid carriers such as liposomes may increase pharmaceutical availability in target tissues and overcome the previously highlighted limitations6. These vesicles are spherical nanoparticles composed of phospholipids and contain one or more phospholipid bilayers. Liposomes have an exterior lipid bilayer that surrounds the aqueous compartment7,8,9. As a result, hydrophilic medicines can dissolve in water confined within their inner core, whereas lipophilic substances can be trapped within lipid bilayers3,10,11. Because of these features, these nanovesicles can entrap both hydrophobic and hydrophilic active pharmaceuticals, providing various benefits such as increased drug stability, efficacy, and therapeutic index12. Furthermore, these carriers are good artificial imitations of nature, increasing the solubility and bioavailability of active medicines while maintaining low toxicity and no immunogenicity3,8,12,13,14,15,16,17. Furthermore, liposomes have been proven to have a significant advantage over other nanocarriers for delivering drugs across the blood–brain barrier (BBB). They can hide the barrier-limiting features of the pharmaceutical molecule and system, as well as regulate the drug penetration rate in specific endothelial regions of the brain, decreasing the expected zonal toxicity4,18.
Several approaches for producing nanoliposomes on a laboratory and commercial scale have been developed. Conventional preparation procedures include detergent removal, thin film hydration, emulsions, reverse phase evaporation, and solvent injection removal. These manufacturing processes have several limitations, including a lack of reproducibility, poor encapsulation efficiencies (EE), varying dimensions of manufactured liposomes, the difficulty of altering product scales, and the usage of huge volumes of organic solvents, which create toxicity in the final product. Furthermore, these approaches involve numerous steps and require downstream phases such as extrusion or sonication to produce nanoliposomes of a suitable size and homogeneity. As a result, these restrictions hinder nanoliposomes from being manufactured on an industrial scale in GMP circumstances7,8.
To reduce or eliminate the use of organic solvents and produce greener chemistry, supercritical fluid (SCF) has been investigated in the field of nanoliposome manufacturing19. Unlike traditional approaches, these technologies produce nanometric liposomes in a single step, eliminating the need for post-processing stages like extrusion or sonication. Furthermore, supercritical-assisted procedures produce liposomes with improved physicochemical qualities and reproducibility, making these approaches suitable for industrial production under GMP conditions7,20. Supercritical fluid can be used as an atomization agent, anti-solvent, or solvent21. The most known supercritical-based techniques occupied for liposome formation are the rapid expansion of supercritical solvent (RESS), supercritical reverse phase evaporation (scRPE), the expanded solution into aqueous media (DESAM), SC-CO2 gas antisolvent method (SC-CO2 GAS) supercritical Assisted liposome formation (SuperLip), and expansion of supercritical fluid (ESS)22,23,24,25,26.
The purpose of this study was to create sertraline hydrochloride nanoliposomes using a unique technology called supercritical fluid solution expansion into aqueous solution (ESSAS). ESSAS is a modified version of our prior work on supercritical fluid solution (ESS) expansion21,24,27,28. Sertraline hydrochloride nanoliposomes were created utilizing the phospholipid DSPC (1,2-Distearoyl-sn-glycero-3-phosphocholine), which was initially dissolved in water and ethanol before being exposed to a high-pressure supercritical fluid. In this procedure, the pressure suddenly drops, but it remains higher than the critical pressure. As a result, phospholipids’ precipitation rate can be controlled, and homogeneous liposomes with narrow size distribution can be produced. Furthermore, whereas in other processes, the pressure is brought down to atmospheric pressure from above the critical pressure, this procedure allows for the production of massive liposomes with a depressurization rate of fewer than 10 MPa. Furthermore, supercritical CO2 which is used in this technique is a gas at normal conditions so it is easily removed from the final produc29,30. The efficiency of liposome production with this approach is dependent on various parameters, including pressure, flow rate, temperature, and duration. In cases like this, where multiple variables may influence the end result, optimizing and modeling processing variables using approaches such as the one factor at a time (OFAT) method or design of experiments (DOE) is an excellent strategy to improve process efficacy31.
DOE is a mathematical framework that measures the impact of each effective parameter on results at several levels of all other factors. Accordingly, in this technique, all the interactions between different parameters are considered, and the results obtained for the optimal points are highly accurate32,33. DOE is more beneficial than the one-factor-in-time variation approach because the DOE strategy provides more accurate results than the OFAT approach and uses fewer experiments to obtain optimal conditions34.
Response surface methodology (RSM) is one of the most widely used DOE that is applied for developing processes, designing, creating new outputs, and optimizing the process. RSM is classified into different subsets such as the central composite design (CCD), box Behnken (BB), full factorial design (FFD), doehlert matrix (DM), and placket-burman design (PBD)35,36,37. One of the RSMs, the box Behnken, is made by combining a balanced or partially balanced incomplete block design with a two-level factorial design in a particular fashion making it possible to efficiently estimate the first- and second-order coefficients of the mathematical mode38. The Box Behnken matrix with three components has a spherical, rotatable design, meaning that all of the design points (aside from the center) are distributed evenly over the sphere39. So, to investigate and optimize the factors affecting the nanoliposome’s size, encapsulation efficiency, the number of produced nanoliposomes, and vesicle stability we employed the Box-Behnken design (BB).
Experimental
Materials
Carbon dioxide (CO2) (99.99% minimum purity) was purchased from Roham Company (Tehran, Iran). Liposomes were made with cholesterol (C27H46O, 99% minimum purity) and 1,2-Distearoyl-sn-glycero-3-phosphocholine (DSPC, C44H88NO8P, 99% minimum purity) which were purchased from Sigma-Aldrich. Caledon (Georgetown, Ont., Canada) provided HPLC grade ethanol and methanol. All of the formulations were made with distilled and deionized water. Moreover, the sertraline hydrochloride standard (C17H18Cl3N, 98% minimum purity) used for encapsulation in liposomes was provided by Krka (Gradiček, Slovenia).
Preparation of nanoliposomes
Preparation of the phospholipid cargo solution
At 25 °C, 60 mg DSPC was dissolved in a 30 mL mixture of ethanol/water (30% V/V), and the desired solution was then supplemented with 9 mg cholesterol and 15 mg sertraline hydrochloride standard. After that, the solution of the active ingredients was then stirred for 90 min at 1100 rpm and afterward, 2 mL of the resulting solution was transferred to the equilibrium vessel for liposome preparation.
Nanoliposome production process
In this study, ESSAS was used to prepare the nanoliposomes. A Suprex automated Prepmaster 44 system (AP44) with a variable flow restrictor (Pittsburgh, PA) was used to prepare liposomes, and the schematic representation of the ESS apparatus for the production of liposomes is shown in Fig. 1. The device consists of two high pressure liquid vessels (equilibration and production (inner volume, 10 cm3; dimensions, 16 mm i.d. × 141 mm height; manufacturer, Suprex Co. Ltd.)) which are linked by needle valve 2. A thermocouple located inside the oven was used to monitor the temperature of the vessels, and the pressure in the high-pressure vessels was measured using a digital pressure gauge. A specific volume of cargo solution (2 ml) was transferred to the equilibration vessel and 7.5 ml of the HPLC grade water was placed in the production vessel. The temperature, collection time, and pressure drop (Pd) parameters ranges were chosen based on the earliest experimental results. In addition, for all the experiments flow rate (is the flow of supercritical CO2 during the collection time), equilibrium pressure, and equilibration time were kept constant at 2 ml/min, 40.5 MPa and 30 min, respectively. To determine the point for the highest EE, the number of the produced liposomes, and their smallest size, the parameters of temperature, collection time (the time when valves 2 and 3 are open and the supercritical fluid enters the production vessel from the equilibrium vessel), and pressure drop were investigated through Statgraphics XVII software with Box-Behnken designs.
The high-pressure pump generated dense CO2, which was delivered through a capillary tube. In the first stage, to dissolve the cargo solution in SC-CO2, valve one was opened, and dense CO2 was pumped into the equilibrium vessel. When the pressure reached 40.5 MPa, then the DSPC, cholesterol, and sertraline hydrochloride were dissolved in SC-CO2 for 30 min. When the equilibrium time was up, the contents of the equilibrium vessel were expanded into the production vessel through a nozzle with a 1/8″ inner diameter nozzle by opening valve 2. To adjust the pressure drop, valve 3 was opened, and SC-CO2 was passed via the production vessel. At this stage, by opening valves 2 and 3, a rapid pressure drop occurred, and due to the decrease in density and solubility of SC-CO2, the compounds dissolved in it were precipitated into the water in the production vessel using the nucleation phenomenon. Finally, in this process, the precipitated phospholipids and cholesterol were assembled, and spontaneously formed nanoliposomes that contained a portion of sertraline hydrochloride. Valve 3 remained open at the end of the work, while valves 1 and 2 were closed, and as a result, the production vessel reached ambient pressure. The resulting solution was then collected in a vial and stored at 4 °C for further analysis.
Characterization of Liposomes: morphology and size distribution
Field emission scanning electron microscopy (FESEM)
Using a field emission scanning electron microscope (FESEM, MIRA3 TESCAN-XMU, and the Czech Republic), the size and morphology of the produced liposomes were evaluated. For this purpose, two tiny droplets of the nanoliposome suspension were sprayed on the aluminum bases, and then dried using air, and nanoliposomes were coated with a layer of platinum using a sputtering system (Pelco SC-7, Ted Pella Inc., Redding, CA). ImageJ software was used to analyze the images.
Size distribution, and Zeta potential of liposomes
After ESS process, Dynamic Light Scattering (mod. Zetasizer Nano S, United Kingdom) was used to determine the mean diameter (MD), standard deviation (SD), and zeta potential (ZP) of the generated nanoliposomes. This device has a 5.0 mW He–Ne laser with a 633 nm wavelength and a 173° scattering angle. Each test required 1 ml of the nanoliposome suspension, and measurements were made at room temperature in triplicates.
Storage stability study
For up to 2 months, the nanoliposome suspension made using the ESS approach was stored to investigate their storage stability. The size and morphology of the nanoliposomes were investigated for storage stability at predetermined time intervals.
Determination of encapsulation efficiency (EE)
By measuring non-encapsulated sertraline hydrochloride in the generated liposome suspension, the encapsulation efficiency of the manufactured liposomes was examined. The difference between the initial amount of sertraline hydrochloride used to create the cargo solution, and the amount of non-encapsulated sertraline hydrochloride that remained in the liposome suspension during production allowed us to calculate the amount of sertraline hydrochloride entrapped in the nanoliposomes. This was accomplished by ultracentrifugation of the liposome suspension made with the ESS method for 45 min at 7000 rpm. Following that, the supernatants were separated, and high-performance liquid chromatography (HPLC) was used to measure the amount of sertraline hydrochloride present in the supernatants.
The HPLC method for determining and measuring the sertraline hydrochloride content into supernatants was performed using a liquid chromatographer (HP Agilent 1050, Agilent, Santa Clara, California, USA) coupled with Variable Wavelength Detector and operated by HP ChemStation software. The separation was carried out with 10 μl of sample injection volume and using an Agilent HT Zorbax SB-C18 column (5 µm particle size, 4.6 mm × 250 mm; Agilent Technologies, Santa Clara, CA). Water (A) and methanol (B) were utilized as the mobile phase in the gradient elution program. During 35 min of analysis, the flow rate of the mobile phase and the wavelength of the detector were kept at 0.8 ml/min and 260 nm, respectively. The separation was performed with 10 μl of sample injection volume. The gradient program was conducted as follows: 0–10 min, 20–70% B; 10–25 min, 70% B; 25–27 min, 70–20% B; 27–35 min, 20% B. Before analyzing the supernatants, the standard curves of sertraline hydrochloride were constructed from the sertraline hydrochloride standard at concentrations ranging from 20 to 500 ppm. Then, Eq. (1) is used to evaluate the encapsulation efficiency, where CT is the initial quantity of sertraline hydrochloride and F is the quantity of free sertraline hydrochloride in the liposome suspension.
Drug release test
Dialysis experiments for drug release were carried out at 37 °C. At the center point, 4 ml of produced sertraline hydrochloride liposomes were put into a dialysis sack (MWCO 3500 Da, Sigma Aldrich, Milan, Italy), then incubated in 150 ml of distilled water bulk. In the absence of light, drug release profiles were investigated in this bulk to calculate the amount of drugs released, 1 ml aliquots of the dialysate (a distilled water bath solution containing the released sertraline) were taken at various time intervals. The dialysate solvent was then evaporated, and the residual sertraline hydrochloride was dissolved in 200 μl of ethanol to increase the drug concentration and the HPLC procedure which used to quantify the EE, was used to determine how much sertraline hydrochloride was present. Another release test was conducted using pure sertraline hydrochloride solution (12.5 mg drug in 10 ml water/ethanol 95% V/V) as a reference.
Results and discussion
The fundamental goal of creating liposomes using the ESSAS approach is to streamline the preparation and manufacturing phases while enhancing repeatability, encapsulation efficiency, homogeneity, count of created liposomes, and particle size distribution. In environmental conditions, phospholipids self-assemble when dispersed in water, and this process leads to the production of liposomes. Water/ethanol/phospholipid and sertraline in vessel 1 are saturated in the SC-CO2 during the equilibrium time. When valves 2 and 3 are opened, a pressure drop occurs and at the same time, the fluid is sprayed from the vessel 1 into the vessel 2, which causes the formation of fine water droplets. When the pressure drop occurs, the solvent power of the fluid is reduced, which causes precipitation of sertraline and phospholipid. During these steps, a part of the precipitated sertraline is trapped in water droplets. Then, Phospholipids quickly cover these droplets, and as a result, inverted lipidic micelles formed. Micelles fall in the aqueous bulk of vessel 2 and are stabilized by a second layer of phospholipids that cover around this structure, resulting in the formation of liposomes. Nanoliposome characteristics including EE, the number of liposomes produced at 1 µm scale, and liposome size are influenced by temperature, collection time, and pressure drop. Therefore, stat graphics software assessed the pressure drop, collecting time, and temperature parameters to determine the ideal value for the liposome size, EE, and the number of produced nanoliposomes. Box Behnken design, one of the experimental designs, was utilized to optimize the parameters at three different levels. With 3 center point repetitions, 15 experiments were completed, as calculated by the formula K = 2k(K−1) + C (where k is the number of parameters and C is the number of center point repetitions). The experimental condition and the obtained results are shown in Table 1.
The formulas of the second-order polynomial models resulting from the experimental design were obtained as follows:
where Y1, Y2, and Y3 are the nanoliposomes size, count of created liposomes, and EE, and X1, X2, and X3 are the temperature (°C), the pressure drop (MPa), and a collection time (min), respectively. ANOVA analysis of experimental data was performed using stat graphics software shown in Tables S1, S2, and S3. In this table, the importance of different coefficients such as linearity, quadratic, and interaction with p-value is stated, which the expressions of the model with p < 0.05 mean significant and with p > 0.05 mean insignificant. The results of the ANOVA demonstrated good accomplishments R2 and R2 adjusted for nanoliposome size (97% and 91%), EE (98% and 95%), and the count of created nanoliposomes (95% and 86%), respectively. Additionally, the high-adjusted R-square value validates the validity of the data and the model by demonstrating a significant correlation between the estimated and measured values. In addition, the “Lack of Fit p-value” is more than 0.05, indicating that the model adequately explained the experimental data and that the Lack of Fit was not statistically significant compared to the pure error. These results show that the model developed in this work is capable of accurately predicting the experimental data.
The conclusion is further supported by Fig. S1, which displays graphs of experimental values of EE, nanoliposome size, and count of created liposomes versus predicted over the experimental range of this investigation.
It should be mentioned that the zeta potential is utilized to assess the stability of liposomes in suspension, and values greater than |30| mV signify liposome stability. In this study, the ZP was greater than − 30 mV in every instance, and the liposomes formed had good stability.
Pressure drop effect
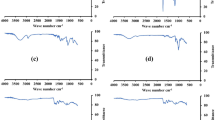
In this work, the primary pressure and flow rate were held constant at 40.5 MPa and 2 ml/min while the pressure drop was adjusted in the range of 10–30 MPa to investigate the impact of pressure drop on EE, nanoliposome count, and liposome size. The pressure drop had the greatest impact on the size, and quantity of nanoliposomes and it was a significant factor for EE, according to Pareto and main effect graphs (Fig. 2).
Figure 2b,d show that by increasing pressure drop, the size of nanoliposomes was decreased and the number of nanoliposomes increased. To explain this phenomenon, it can be stated that a higher pressure drop leads to a greater decrease in the density and solubility of SC-CO2, which in turn leads to a greater difference in the number of phospholipids that could be dissolved in it before and after the expansion stage, which resulted in a higher supersaturation. According to the nucleation theory, higher supersaturation boosted nucleation during the expansion step, which resulted in the production of smaller liposomes40,41,42. Additionally, as SC-CO2 has a lower dissolution power at a higher pressure drop, it was necessary to release more phospholipids and form more liposomes.
The encapsulation efficiency of the produced liposomes rose until the pressure drop was attained at 25 MPa and after that declined, as shown in Fig. 2f. As was indicated earlier, as the pressure drop increased, more liposomes were generated, which led to increasing the EE. However, a smaller liposome had less space to encapsulate the sertraline hydrochloride, which resulted in a reduction in EE at a very high pressure drop. Figure 3a,b (experiments 5 and 7) demonstrate the impact of pressure on the development of nanoliposomes.
Temperature effect
The impact of temperatures in the 40–70 °C range was investigated in this study. The number of liposomes generated was significantly influenced by temperature, whereas size and EE were unaffected by this parameter, as seen in the Pareto charts in Fig. 2a,c,e.
As the temperature rises, the size of liposomes does not significantly change, but their quantity does, as indicated by the main effect graphs in Fig. 3b,d. Because phospholipids became less soluble in supercritical fluid as the temperature rose, fewer liposomes were generated as a result. This was due to the fact that CO2 density decreased with increasing temperature43,44,45,46. In addition, as shown in Fig. 2f when the temperature rose, the EE of the produced liposomes increased and then decreased. Since, density, permeability, fluidity, and solubility of SC-CO2 are influenced by temperature. First, sertraline hydrochloride became more soluble in the water inside the liposomes as the temperature rose, which led to an increase in the EE. Then, the EE of nanoliposomes decreased because, as previously stated, the increase in temperature led to a decrease in the number of liposomes produced as well as to the breaking of van der Waals bonds and the interaction between phospholipids, which increased the permeability and fluidity of liposomes membrane47. Furthermore, the morphology of the liposomes produced at low temperatures was spherical, however as the temperature rose, the intermolecular force was broken, and the fluidity of the liposome membrane increased, leading to the formation of liposomes with irregular shapes. The influence of temperature on the generated nanoliposomes is depicted in Fig. 3c,d (experiments 6 and 13).
Collection time effect
Figure 2 shows that, at the 95% confidence level, the collection time had a substantial impact on size and EE. This effect was positive for EE and negative for the liposome dimension. Additionally, the collecting time had a positive impact on the number of liposomes.
As it is evident in Fig. 2d, initially, with the increase in the collection time, the number of formed liposomes increased, because, during this period, more solution entered vessel 2 from vessel 1. As a result, more liposomes were produced. However, as seen in the graph, the number of liposomes remained constant after a certain time because all the solution in vessel 1 had been removed and no more solution was available to form more liposomes. According to the causes mentioned above, and due to the formation of more liposomes, the EE rose over time, which can be seen in Fig. 2f. Additionally, as seen in Fig. 2b supersaturation rose at higher times as a result of the dissolution of greater amounts of phospholipid in the SC-CO2, which led to a reduction in the size of the liposomes. The impact of collection time on the formation of nanoliposomes is shown in Fig. 3e,f (experiments 2 and 15).
Response surface analysis
The response surface diagrams of size, count, and EE of sertraline liposomes as functions of pressure drop, temperature, and collection time were created by altering the two of them while maintaining the other one, as shown in Fig. 4. The steepness of the response surfaces illustrated the influence of variables on responses. The steeper surfaces suggested that variables had a greater influence on the response. The peak value in Fig. 4d–i showed the ideal value for the EE and nanoliposome count. In contrast, the optimal value for the size of the liposomes that were formed is indicated by the valley value in Fig. 4a–c. The shape of the outline provides more evidence for the interaction of two factors.
Figure 4a illustrated how longer collection times and higher pressure drops resulted in changing liposome size at a mean temperature level of 55 °C. Additionally, Fig. 4b showed that this response would be impacted by growing pressure drop and temperature at constant collection times, resulting in the formation of smaller liposomes (61 nm). Furthermore, when temperature and collection time increase, firstly smaller liposomes are generated, and then larger liposomes were formed (Fig. 4c). Equation (2) demonstrated that the X1X2 and X1X3 interaction coefficients were negative while the X2X3 was positive. Furthermore, as seen in Fig. 4h,i, the EE of liposomes increased to a certain level with the progression of collection time and temperature as well as the pressure drop and temperature, and then it began to decline. Also, as seen in Fig. 4d,g , the number of liposomes and EE increased with increasing pressure drop and collection time. The interaction coefficients for the count of liposomes were negative for X1X3, and X1X2, as shown in Eq. (3). Moreover, according to Eqs. (4), the interactions of X1X3 have a negative influence on the EE.
Optimization condition
The predicted model was used to predict the perfect circumstances for the ESSAS method of producing sertraline liposomes. Pressure drop at 29.9 MPa, collection time at 13.6 min and temperature at 40 °C were the optimal settings for the production of nanoliposomes in order to minimize the size and maximize the EE and number of nanoliposomes. Under these conditions, the values of liposome size, count of nanoliposomes, and EE were equal to 95.1 nm, 82, and 74.4%, respectively.
The test was run at above conditions in order to evaluate the predicted model’s adaptability and optimal points with experimental test. As shown in Fig. 5a, the number of nanoliposomes produced was 85, with a mean dimension of 89.5 nm. Furthermore, Fig. 5b also shows the size distribution of liposomes produced at the optimal point. As can be seen in this figure, liposomes with a uniform size distribution were created in this experiment. Also, in this test the EE for generated nanoliposomes attained 78.4%, demonstrating the strong conformity of the predicted model with the experimental test under ideal circumstances.
In this study, the created liposomes exhibited the same or higher encapsulation efficiency than prior studies that produced sertraline liposomes (Table 2). Also, the liposomes created in this study were much smaller. Because the liposomes produced were smaller, it is expected that they will be less recognized by macrophages and will remain in the circulatory system for a longer period of time. Furthermore, unlike previous research, only safe solvents, water, and ethanol, were employed.
Storage stability study
On the liposome suspension, which is held at 4 °C in the dark, to measure the influence of time on their stability, the average diameter of liposomes containing sertraline hydrochloride as encapsulating material was investigated at various time intervals (Fig. 6a).
Over 2 months, the mean diameter of nanoliposomes created by ESSAS remained constant in comparison to the initial values. The experimental results for days 20, 40, and 60 following the storage day were 82, 81, and 90 nm, respectively, which indicated a modest change in comparison to the initial values. Therefore, these findings demonstrated that sertraline hydrochloride-encapsulated liposomes maintained at 4 °C remained stable for up to 60 days with no appreciable changes in the nanoliposomes size. This phenomenon occurred due to the uniform distribution of charge on the surface of liposomes, which made them thermodynamically stable. On the other hand, their gradual breakdown led to a modest alteration in liposome size.
Sertraline hydrochloride release test
Drug release assays were conducted at 37 °C to understand how liposomes affected the kinetics of drug release. The sertraline hydrochloride chromatogram depicted in Fig. S2 after the drug release test. In Fig. 6b a comparison between free sertraline hydrochloride, and sertraline liposomes was illustrated. According to the results, drug penetration through the dialysis membrane was not a limiting step for the fast release of free sertraline because it was released throughout a 5-h period. On the other hand, sertraline-loaded liposomes were finished their release after 27 h and approved that the usage of nanoliposomes delays the release of sertraline. Sertraline liposomes were found to have an initial burst in the drug release that was larger than 17.5% during the initial sampling period (150 min), as seen in Fig. 6b. The sertraline that was adsorbed on the liposome’s surface may have been the cause of the observed burst release. Following the first burst release, a constant drug release was detected, which could be caused by the drug that had been dissolved in the liposome’s core diffusing into the dissolving media. These findings demonstrated that liposomes significantly alter the kinetics of drug release, leading to more regular drug release.
Conclusion
The techniques used to prepare nanoliposomes by supercritical fluid, documented in the literature, had significant drawbacks such as low EE and batch process layout. In this work, a successful ESSAS procedure was used to produce sertraline hydrochloride liposomes with DSPC as the wall material, and by utilizing RSM combined with Box-Behnken design, the operation parameters (pressure drop, temperature, and collecting time) were optimized. The findings showed that the loading content was significantly influenced by very complex process parameters. However, the model developed in this work could accurately estimate the experimental data. In addition, the results showed that the pressure drop was the most crucial parameter affecting the size and EE of the nanoliposomes. However, collecting time was the most important factor for the number of nanoliposomes. Moreover, neither the size nor the EE of nanoliposomes was significantly impacted by temperature. Additionally, it was determined that the optimal condition for the generation of nanoliposomes were 29.9 MPa of pressure drop, 40 °C of temperature, and 13.6 min of collection time. The nanoliposomes with EE = 78.4%, nanoliposome count = 85, and dimension = 89.5 nm were produced under optimal conditions. This supercritical CO2-assisted approach, in contrast to the majority of conventional procedures, is a simple one-step procedure that does not necessitate further extrusion or ultrasonication stages. Therefore, this method is an easy and convenient replacement for traditional methods to create liposomes with the best and most controllable physicochemical properties (size), while being adaptable to an industrial GMP process and avoiding the drawbacks associated with the use of organic solvents. This method will be used in the future to create liposomes that encapsulate both hydrophobic and hydrophilic active molecules. Furthermore, polymer coatings of liposomes, such as polyethylene glycol, will be investigated in order to create long-circulating and biocompatible vesicles.
Data availability
All data generated or analysed during this study are included in this published article.
References
Chamundeeswari, M., Jeslin, J. & Verma, M. L. Nanocarriers for drug delivery applications. Environ. Chem. Lett. 17, 849–865. https://doi.org/10.1007/s10311-018-00841-1 (2019).
Akiyama, R., Murakami, Y., Inoue, K., Orita, Y. & Shimoyama, Y. Fabrication of PEGylated liposome in microfluidic flow process using supercritical CO2. J. Nanopart. Res. 24, 257. https://doi.org/10.1007/s11051-022-05635-9 (2022).
Trucillo, P., Campardelli, R. & Reverchon, E. Liposomes: From bangham to supercritical fluids. Processes 8, 1022. https://doi.org/10.3390/pr8091022 (2020).
Romanelli, M. M. et al. Sertraline delivered in phosphatidylserine liposomes is effective in an experimental model of visceral leishmaniasis. Front. Cell. Infect. Microbiol. 9, 353. https://doi.org/10.3389/fcimb.2019.00353 (2019).
Harbi, I., Aljaeid, B., El-Say, K. M. & Zidan, A. S. Glycosylated sertraline-loaded liposomes for brain targeting: qbD study of formulation variabilities and brain transport. AAPS PharmSciTech 17, 1404–1420. https://doi.org/10.1208/s12249-016-0481-7 (2016).
Chauhan, T. et al. Negatively charged liposomes of sertraline hydrochloride: Formulation, characterization and pharmacokinetic studies. J. Drug Deliv. Sci. Technol. 58, 101780. https://doi.org/10.1016/j.jddst.2020.101780 (2020).
Trucillo, P., Campardelli, R., Scognamiglio, M. & Reverchon, E. Control of liposomes diameter at micrometric and nanometric level using a supercritical assisted technique. J. CO2 Util. 32, 119–127. https://doi.org/10.1016/j.jcou.2019.04.014 (2019).
Penoy, N., Grignard, B., Evrard, B. & Piel, G. A supercritical fluid technology for liposome production and comparison with the film hydration method. Int. J. Pharm. 592, 120093. https://doi.org/10.1016/j.ijpharm.2020.120093 (2021).
Nishizawa, K. et al. Preparation and characterization of cellulose ether liposomes for the inhibition of prion formation in prion-infected cells. J. Pharm. Sci. 108, 2814–2820. https://doi.org/10.1016/j.xphs.2019.03.025 (2019).
Wang, X. et al. Preparation, characterization, pharmacokinetics, and bioactivity of honokiol-in-hydroxypropyl-β-cyclodextrin-in-liposome. J. Pharm. Sci. 100, 3357–3364. https://doi.org/10.1002/jps.22534 (2011).
Bhattacharjee, A. et al. Development and optimization of besifloxacin hydrochloride loaded liposomal gel prepared by thin film hydration method using 32 full factorial design. Colloids Surf. A 585, 124071. https://doi.org/10.1016/j.colsurfa.2019.124071 (2020).
Ahmed, S. A., Salama, A. A., Gaber, M. H. & Ali, S. A. Development and characterization of soy lecithin liposome as potential drug carrier systems for doxorubicin. J. Pharm. Innov. https://doi.org/10.1007/s12247-023-09732-7 (2023).
Abdel-Rashid, R. S., Abd Allah, F. I., Hassan, A. A. & Hashim, F. M. Design, optimization, and in-vivo hypoglycaemic effect of nanosized glibenclamide for inhalation delivery. J. Liposome Res. 31(3), 291–303. https://doi.org/10.1080/08982104.2020.1806874 (2021).
Li, Y. et al. Preparation, characterization and evaluation of bufalin liposomes coated with citrus pectin. Coll. Surf. A 444, 54–62. https://doi.org/10.1016/j.colsurfa.2013.12.006 (2014).
Wang, S. et al. Preparation and evaluation of long-circulating deoxypodophyllotoxin-loaded liposomes using Poly(Ethylene Glycol)-distearoylphosphatidylethanolamine. J. Pharm. Innov. 11, 134–142. https://doi.org/10.1007/s12247-016-9246-9 (2016).
Solomon, D. et al. Role of in vitro release methods in liposomal formulation development: Challenges and regulatory perspective. AAPS J. 19, 1669–1681. https://doi.org/10.1208/s12248-017-0142-0 (2017).
Shukr, M. H. & Ahmed Farid, O. A. Amisulpride–CD-loaded liposomes: optimization and in vivo evaluation. AAPS PharmSciTech 19(6), 2658–2671. https://doi.org/10.1208/s12249-018-1079-z (2018).
Mohammadi, M., Karimi, M. & Raofie, F. Expansion supercritical fluid into an aqueous solution (ESSAS), a new technique for creating nano-size cyanocobalamin-loaded liposomes, and optimization of involved parameters. J. Iran. Chem. Soc. 21, 373–385. https://doi.org/10.1007/s13738-023-02930-7 (2024).
Lim, C.-B. et al. Preparation, characterization, and in vivo pharmacokinetic study of the supercritical fluid-processed liposomal amphotericin B. Pharmaceutics 11, 589. https://doi.org/10.3390/pharmaceutics11110589 (2019).
Chakravarty, P., Famili, A., Nagapudi, K. & Al-Sayah, M. A. Using supercritical fluid technology as a green alternative during the preparation of drug delivery systems. Pharmaceutics 11, 629. https://doi.org/10.3390/pharmaceutics11120629 (2019).
Salehi, H., Karimi, M. & Raofie, F. Micronization and coating of bioflavonoids extracted from Citrus sinensis L. peels to preparation of sustained release pellets using supercritical technique. JICS. 18, 3235–3248. https://doi.org/10.1007/s13738-021-02262-4 (2021).
Santo, I. E. et al. Liposomes preparation using a supercritical fluid assisted continuous process. Chem. Eng. J. 249, 153–159. https://doi.org/10.1016/j.cej.2014.03.099 (2014).
Sharifi, F. et al. Generation of liposomes using a supercritical carbon dioxide eductor vacuum system: Optimization of process variables. J. CO2 Util. 29, 163–171. https://doi.org/10.1016/j.jcou.2018.12.011 (2019).
Karimi, M., Raofie, F. & Karimi, M. Production Ganoderma lucidum extract nanoparticles by expansion of supercritical fluid solution and evaluation of the antioxidant ability. Sci. Rep. 12, 1–12. https://doi.org/10.1038/s41598-022-13727-8 (2022).
Momenkiaei, F. & Raofie, F. Preparation of Curcuma Longa L. extract nanoparticles using supercritical solution expansion. J. Pharm. Sci. 108, 1581–1589. https://doi.org/10.1016/j.xphs.2018.11.010 (2019).
Ghatnur, S. M., Sonale, R. S., Balaraman, M. & Kadimi, U. S. Engineering liposomes of leaf extract of seabuckthorn (SBT) by supercritical carbon dioxide (SCCO2)-mediated process. J. Liposome Res. 22, 215–223. https://doi.org/10.3109/08982104.2012.658576 (2012).
Salehi, H., Karimi, M., Rezaie, N. & Raofie, F. Extraction of β-Carboline alkaloids and preparation of extract nanoparticles from Peganum harmala L. capsules using supercritical fluid technique. J. Drug Deliv. Sci. Technol. 56, 101515. https://doi.org/10.1016/j.jddst.2020.101515 (2020).
Karimi, M. & Raofie, F. Preparation of Withaferin A nanoparticles extracted from Withania somnifera by the expansion of supercritical fluid solution. Phytochem. Anal. 31, 957–967. https://doi.org/10.1002/pca.2968 (2020).
Nikolai, P., Rabiyat, B., Aslan, A. & Ilmutdin, A. Supercritical CO2: Properties and technological applications-a review. J. Therm. Sci. 28, 394–430. https://doi.org/10.1007/s11630-019-1118-4 (2019).
Karimi, M. & Raofie, F. Micronization of vincristine extracted from Catharanthus roseus by expansion of supercritical fluid solution. J. Supercrit. Fluids 146, 172–179. https://doi.org/10.1016/j.supflu.2019.01.021 (2019).
Yousefi, M. et al. Supercritical fluid extraction of essential oils. TrAC, Trends Anal. Chem. 118, 182–193. https://doi.org/10.1016/j.trac.2019.05.038 (2019).
Jacyna, J., Kordalewska, M. & Markuszewski, M. J. Design of Experiments in metabolomics-related studies: An overview. J. Pharm. Biomed. Anal. 164, 598–606. https://doi.org/10.1016/j.jpba.2018.11.027 (2019).
Manmai, N., Unpaprom, Y. & Ramaraj, R. Bioethanol production from sunflower stalk: application of chemical and biological pretreatments by response surface methodology (RSM). Biomass Convers. Biorefinery 11, 1759–1773. https://doi.org/10.1007/s13399-020-00602-7 (2021).
Luiz, M. T. et al. Design of experiments (DoE) to develop and to optimize nanoparticles as drug delivery systems. Eur. J. Pharm. Biopharm. 165, 127–148. https://doi.org/10.1016/j.ejpb.2021.05.011 (2021).
Onu, C. E., Nwabanne, J. T., Ohale, P. E. & Asadu, C. O. Comparative analysis of RSM, ANN and ANFIS and the mechanistic modeling in eriochrome black-T dye adsorption using modified clay. S. Afr. J. Chem. Eng. 36, 24–42. https://doi.org/10.1016/j.sajce.2020.12.003 (2021).
Witek-Krowiak, A., Chojnacka, K., Podstawczyk, D., Dawiec, A. & Pokomeda, K. Application of response surface methodology and artificial neural network methods in modelling and optimization of biosorption process. Biores. Technol. 160, 150–160. https://doi.org/10.1016/j.biortech.2014.01.021 (2014).
Guo, D. et al. Optimization, characterization and evaluation of liposomes from Malus hupehensis (Pamp.) Rehd. extracts. J. Liposome Res. 30, 366–376. https://doi.org/10.1080/08982104.2019.1651334 (2020).
Aslan, N. & Cebeci, Y. Application of Box-Behnken design and response surface methodology for modeling of some Turkish coals. Fuel 86, 90–97. https://doi.org/10.1016/j.fuel.2006.06.010 (2007).
Bezerra, M. A., Santelli, R. E., Oliveira, E. P., Villar, L. S. & Escaleira, L. A. Response surface methodology (RSM) as a tool for optimization in analytical chemistry. Talanta 76, 965–977. https://doi.org/10.1016/j.talanta.2008.05.019 (2008).
Hirunsit, P., Huang, Z., Srinophakun, T., Charoenchaitrakool, M. & Kawi, S. Particle formation of ibuprofen–supercritical CO2 system from rapid expansion of supercritical solutions (RESS): A mathematical model. Powder Technol. 154, 83–94. https://doi.org/10.1016/j.powtec.2005.03.020 (2005).
Vorobei, A. M. & Parenago, O. O. Using supercritical fluid technologies to prepare micro- and nanoparticles. Russ. J. Phys. Chem. A 95, 407–417. https://doi.org/10.1134/S0036024421030237 (2021).
Bagheri, H., Hashemipour, H., Ghalandari, V. & Ghader, S. Numerical solution of particle size distribution equation: Rapid expansion of supercritical solution (RESS) process. Particuology 57, 201–213. https://doi.org/10.1016/j.partic.2020.12.011 (2021).
Han, Y., Cheng, J., Ruan, N. & Jiao, Z. Preparation of liposomes composed of supercritical carbon dioxide-philic phospholipids using the rapid expansion of supercritical solution process. J. Drug Deliv. Sci. Technol. 64, 102568. https://doi.org/10.1016/j.jddst.2021.102568 (2021).
Fattahi, A. et al. Preparation and characterization of simvastatin nanoparticles using rapid expansion of supercritical solution (RESS) with trifluoromethane. J. Supercrit. Fluids 107, 469–478. https://doi.org/10.1016/j.supflu.2015.05.013 (2016).
Sodeifian, G., Hazaveie, S. M. & Sodeifian, F. Determination of Galantamine solubility (an anti-alzheimer drug) in supercritical carbon dioxide (CO2): Experimental correlation and thermodynamic modeling. J. Mol. Liq. 330, 115695. https://doi.org/10.1016/j.molliq.2021.115695 (2021).
Sodeifian, G. & Usefi, M. M. B. Solubility, extraction, and nanoparticles production in supercritical carbon dioxide: A mini-review. ChemBioEng Rev. 10, 133–166. https://doi.org/10.1002/cben.202200020 (2023).
Zhao, L., Temelli, F., Curtis, J. M. & Chen, L. Encapsulation of lutein in liposomes using supercritical carbon dioxide. Int. Food Res. J. 100, 168–179. https://doi.org/10.1016/j.foodres.2017.06.055 (2017).
Lei, Y. et al. Sertraline/ICG-loaded liposome for dual-modality imaging and effective chemo-photothermal combination therapy against metastatic clear cell renal cell carcinoma. Chem. Biol. Drug Des. 95, 320–331. https://doi.org/10.1111/cbdd.13652 (2020).
Chawla, R. Formulation and evaluation of negatively charged liposomes of sertraline hydrochloride for antidepressant activity. AJP. https://doi.org/10.22377/ajp.v14i2.3616 (2020).
Acknowledgements
We thank a variety of sources for supporting this work, including the Shahid Beheshti University and the Iran Ministry of Higher Education for a studentship to support (Grant No: 1398).
Funding
This work was supported by Shahid Beheshti University (Grant No.1398).
Author information
Authors and Affiliations
Contributions
M.M.: Methodology, doing experiment, writing original draft. M.K.: design, editing text, interpret the data. F.R.: Supervise the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
All authors agreed with the content and give their consent to submit the manuscript for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mohammadi, M., Karimi, M. & Raofie, F. Nano-engineering of sertraline liposomes using supercritical fluid and optimization of the involved parameters. Sci Rep 15, 15386 (2025). https://doi.org/10.1038/s41598-024-82018-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-82018-1