Abstract
We studied mortality and hospital contact in people from Thyborøn-Harboøre, an environmentally contaminated fishing community on the Danish West Coast. The population and a comparison group from other fishing communities on the Danish West Coast were identified from historical data in the Central Population Register. All persons were followed up for death and hospital contacts to March 2023. Event rates were compared with Poisson regression; adjusted rate ratios (aRR); and 95% confidence interval (CI). The old cohort included inhabitants in Thyborøn-Harboøre in 1968–1970 before pollution was controlled; 4914 persons/2485 deaths. All-cause mortality, aRR 1.06 (95% CI 1.01–1.11), and cancer mortality, aRR 1.17 (95% CI 1.05–1.30), were elevated; especially for kidney cancer aRR 1.82 (95% CI 1.07–3.12). Hospital contacts were elevated for psychiatric disorders; with an aRR of 4.07 (95% CI 1.41–11.72) for anxiety in men. As there is still considerable concern in the area about possible health consequences from stored chemicals, we included also a new cohort of newborn and immigrants to the area in 1990–2006; 2933 persons/302 deaths. All-cause mortality, aRR 1.26 (1.11–1.43) (men 1.15 and women 1.44), and cancer mortality, aRR 1.47 (95% CI 1.14–1.89) were elevated. Hospital contacts were elevated for ischemic heart disease/heart attack and indicated for autism/obsessive compulsory disorder in boys. In conclusion, mortality data confirmed incidence data of excess kidney cancer in the old cohort. The new cohort had a generally elevated mortality, possibly indicating selective immigration from other parts of Denmark. However, the new cohort is still relatively young, and the mortality pattern needs to be monitored.
Similar content being viewed by others
Introduction
The possible long-term health consequences of exposure to chemical waste are an issue of concern both for the affected individuals and for the handling of chemical waste. However, the mixed exposures from chemical waste and the long-term latency of some diseases make it very difficult to identify possible causal associations between exposures and health risks1. In the absence of ideal strategies to overcome these limitations, studies of worst case-scenarios from sites with appropriate health data have been suggested2.
After World War II, chemical production expanded in Denmark with a focus on chemicals for use in agriculture. In 1953, one of the main producers moved to a small fishing community on the Danish West Coast called Thyborøn-Harboøre. Various chemicals were produced at the factory including phenoxy herbicides for weed control, and mercury compounds for protection of grain against fungus. However, parathion, an insecticide widely used on cereals, fruit, vines, vegetables, ornamentals and cotton3, soon became the main product.
Wastewater disposal to the North Sea, dumps of both liquid and solid waste in the sandy areas, and leakages from the factory ground polluted the area. As the pollution dates back to the 1950s, 1960s, and 1970s, quantitative data are unfortunately not available. However, a thorough investigation of the pollution in the late 1980s identified more than 100 xenobiotic compounds in the wastewater4. Furthermore, in Nissum Bredning, the water surrounding the factory ground, mercury accumulated in flounders, eels, and mussels; and in 1980–1982 concentrations of 2000–2500 ppb weight were found5. According to long-term Thyborøn inhabitants, fishing for private consumption was common in this water. The investigation was followed by initiation of regulation and better control, but the old contamination remained. The area also housed two smaller fishmeal-and oil processing companies, from where leakages of fish-oil and polluted wastewater were reported6,7. Today the area is the chemically polluted area in Denmark of highest concern8.
In 2021, we found that people who lived in Thyborøn-Harboøre in 1968–1970 had a 20% higher cancer incidence than a comparison group of people who lived at the same time in other fishing communities at the Danish West Coast and without chemical factories9. The excess risk derived in particularly from cancers of the kidney and urinary bladder, where both men and women from Thyborøn-Harboøre had doubled risks. Furthermore, anecdotal cases of acutely blurred eye sights and gradual development of neurological disabilities have been reported from men working at the chemical factory in the pre-regulation period10,11.
To get a comprehensive view of possible long-term health consequences for persons who have lived in Thyborøn-Harboøre, we used available register data to investigate causes of death and hospitalization. As present inhabitants in the area are concerned about possible health consequences of leakages from the stored chemicals in the area, we included also a cohort of newcomers to the area after 1990.
Materials and methods
Study-population
From the Danish Central Population Register (CPR) it is possible to identify all persons with a permanent address in Denmark at any time from 2 April 1968 until today. For each person, dates of immigrations, emigrations, internal movements in Denmark, and death are registered. Computerized population data were not available prior to 1968. We selected two subpopulations for the study. First, people who lived in Thyborøn-Harboøre in 1968–1970 representing the early living conditions in the area. Second, people who live in Thyborøn-Harboøre in 1990–2006 but not prior to 1990. The latter population was still young but included in the analysis as newcomers after pollution control started in the late 1980s. The cohort was further divided into people who moved into the area and people born there. Newcomers after 2006 were not included because new municipality codes did not allow identification of ínhabitants from the small study areas. As in the cancer incidence study, reference cohorts from the two other fishing communities, Holmsland-Hanstholm, were identified9.
Follow-up
These populations were followed up in CPR for death and emigration until end of follow-up on 1 March 2023. Risk periods were calculated for each person starting from date of first registered address in Thyborøn-Harboøre until occurrence of the studied event, emigration, death or end of follow-up for the outcome, For the old cohort the first possible date was 2 April 1968, for the younger cohort it was 1 January 1990, and for both cohorts the last possible date was 1 March 2023, see Supplementary Table S1.
Cause of death was registered by linkage with the Cause of Death Register starting 1970 and ending 2021. The underlying cause of death was used in the analysis. The follow-up period included both deaths coded according to International Classification of Diseases (ICD)-8 and ICD-10. We used a conversion table developed by the Danish Health Authority12, Supplementary Table S2. It should be noted that cause of death was missing for people with a permanent address in Denmark, but dying outside Denmark, and for people dying before 1 January 1970 or after 31 December 2021.
To identify hospitalizations, the cohorts were linked with the National Patient Register (LPR). Registration of somatic diagnoses in LPR started in 1977, registration of psychiatric diagnoses in LPR started in 1995, and both ended by 1 February 2023, person years were accumulated accordingly. Up until 1995, only in-patient contacts were included in the National Patient Register (LPR), but from that time onwards also out-patient hospital contacts were included in LPR. A person was considered a hospitalized case for a given disease on the first date of hospitalization for this disease. The main discharge diagnosis was used. Diseases were grouped according to the list used in the Grindsted-report13, Supplementary Table S3.
Statistics
Poisson regression with control for sex, running age and calendar time was used to compare cause-specific mortality/hospitalization rates between Thyborøn-Harboøre and Holmsland-Hanstholm. For the old cohort, we checked for interactions between area and sex, area and age, and area and calendar time for the old cohort for all-cause mortality by including two-factor interactions one at a time. We also adjusted the estimate of the difference between areas by including birth cohort in the model. Results were presented as adjusted rate ratios (aRR) with 95% confidence intervals (CI). Analysis was undertaken with SAS version 9.4 on the research server in Statistics Denmark.
Ethics
The study was a retrospective cohort study. Data were retrieved from the Danish Central Population Register, the Danish Cause of Death Register, and the Danish National Patient Register. These databases are not publicly available, but the databases can be used for research projects considered beneficial for the society. The use of data and the experimental protocol were approved by Region Zealand with the registration number REG-108-2018. Region Zealand is the public authority in charge of Nykøbing Falster Hospital, where the study was undertaken. According to Danish legislation, approval by the relevant public authority serves as ethical approval of studies based entirely on register-data. No contact was made to patients, their relatives, and/or treating physicians. Informed consent was thus waived by Region Zealand. The experimental protocol followed standard guidelines for cohort studies. To ensure data safety, numbers below 5 were not reported. The study was funded by the Central Region of Denmark, 1-30-72-172-18. The funder had no impact on the design, analysis, interpretation and reporting of the findings.
Results
Old cohort
In total, 4914 people were included in the old Thyborøn-Harboøre cohort, and 9537 in the old reference cohort from Holmsland-Hanstholm. The cohorts had been followed up for 40 years (Table 1). In the Thyborøn-Harboøre cohort, in total 2485 people died, compared with 4980 persons from Holmsland-Hanstholm, resulting in a borderline statistically significantly elevated aRR of 1.06 (95% CI 1.01–1.11) (Table 2). Only the interaction between area and calendar time was statistically significant indicating that the difference in mortality between the geographical areas decreased over time. Inclusion of birth cohort in the model did not change aRRs significantly.
Cancer mortality was statistically elevated in Thyborøn-Harboøre, aRR 1.17 (95% CI 1.05–1.30). Kidney cancer mortality was elevated, aRR 1.82 (95% CI 1.07–3.12), bladder cancer mortality to a lesser extent and not statistically significantly, aRR 1.25 (95% CI 0.74–2.12). Mortality was not statistically elevated for other cause of death.
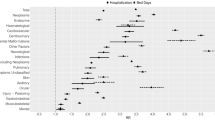
The all-cause mortality in men from Thyborøn-Harboøre was aRR 1.07 (95% CI 1.01–1.14) as compared with men in Holmsland-Hanstholm (Table 2; Fig. 1). Neither cancer mortality, nor mortality from kidney or bladder cancer were statistically elevated in men; aRR 1.14 (95% CI 0.99–1.31); 1.28 (95% CI 0.62–2.62); and 1.09 (95% CI 0.59–1.98), respectively. Mortality from cardiovascular diseases, respiratory diseases and the residual group of other diseases was modestly, but not statistically significantly, elevated in men from Thyborøn-Harboøre, aRR 1.05 (95% CI 0.95–1.17); 1.04 (95% CI 0.82–1.31); and 1.06 (0.93–1.20), respectively. In women from Thyborøn-Harboøre the all-cause mortality was aRR 1.03 (95%CI 0.96–1.11). Both cancer mortality, and mortality from kidney and bladder cancer were elevated, thought the latter not statistically significantly; the aRRs being 1.21 (95% CI 1.03–1.43); 3.01 (95% CI 1.28–7.06); and 2.23 (0.71–6.97), respectively.
In total, people living in Thyborøn-Holmsland in 1968–1970 had 4571 hospital-contact between 1977 and 1 February 2023 (Table 3) which was slightly elevated compared with the rates from Holmsland-Hanstholm; aRR 1.08 (95% CI 1.05–1.12). For hospital-contact attributed to any cancer, the aRR was 1.14 (95% CI 1.06–1.22), affecting both men and women; aRR 1.17 (95% CI 1.06–1.29) and 1.11 (95% CI 1.00–1.24), respectively. The aRR for anxiety in men was 4.07 (95% CI 1.41–11.72) based on 11 cases. For most other disease groups, the aRRs for Thyborøn-Harboøre compared with Holmsland-Hanstholm were almost identical, except a deficit risk for all neurological disorders in women, aRR 0.81 (95%CI 0.72–0.92). Inclusion of interactions in the model showed results similar to those for all-cause mortality.
New cohort
Only 302 deaths were observed in the cohort living in Thyborøn-Harboøre in 1990–2006, but compared with Hanstholm-Holmsland it nevertheless represented an elevated mortality rate, aRR 1.26 (95% CI 1.11–1.43); less in men; aRR 1.15 (95% CI 0.98–1.36), than in women; aRR 1.44 (95% CI 1.18–1.76) (Table 4). Several causes of death contributed to the elevated mortality rate; cancer aRR 1.47 (95% CI 1.14–1.89); and to a less extent cardiovascular diseases aRR 1.31 (95% CI 0.98–1.74); respiratory diseases aRR 1.26 (95% CI 0.80–1.99); external causes aRR 1.25 (95% CI 0.84–1.88); and dementia aRR 2.21 (95% CI 1.12–4.39), which based on six cases was aRR 3.47 (95% CI 1.27–9.45) in men. Women had an increased risk of cancer death; aRR 1.81 (95% CI 1.26–2.62). Of the 39 cancer deaths in women, 18 were lung cancer deaths. No person in this cohort died from kidney cancer, but five people died from bladder cancer, aRR 2.87 (95% CI 0.97–8.45).
In the 1990–2006 cohort, people born in Thyborøn-Harboøre during the period contributed with only 39% of the person years and in the comparison area it was 25% (Table 1). Furthermore, these people were young and in Thyborøn-Harboøre only seven of 302 deaths occurred in people born there. Therefore, observations in the 1990–2006 cohort derived mainly from people moving there during 1990–2006. In Thyborøn-Harboøre, these immigrants had an excess mortality, aRR 1.28 (95% CI 1.13–1.46). In men, the aRR was 1.17 (95% CI 0.99–1.88), and the only statistically elevated cause of death was dementia, aRR 3.47 (95% CI 1.27–9.45) based on six cases. In women, the aRR was 1.48 (95% CI 1.21–1.81), and both death from cancer, aRR 1.82 (95% CI 1.26–2.63), and other diseases, aRR 1.50 (95% CI 1.01–2.22), were elevated.
In the 1990–2006 cohort, 2787 persons were registered with at least one hospital contact, which was similar to the rate in the comparison area, aRR 0.99 (95%CI 0.94–1.03) (Table 5). Contact regarding ischemic heart disease and heart attack were elevated; aRR 1.24 (95% CI 1.02–1.51) and 1.43 (95% CI 1.07–1.90), respectively. A remarkable difference between Thyborøn-Harboøre and the comparison area was the elevated rates for autism and obsessive compulsive disorder in boys though based on small numbers; aRR 1.85 (95% CI 0.64–5.35) and aRR 1.79 (95% CI 0.57–5.67), respectively.
Discussion
The study was initiated based on findings of a doubled incidence of kidney and bladder cancer in men and women living in Thyborøn-Harboøre at the time of heavy pollution in the area9. Kidney and bladder cancers are diseases with a good survival rate14. This means that while we had 39 and 107 incident cases of kidney and bladder cancers, respectively, we had only 25 and 22 deaths. Nevertheless, the mortality data supported the incidence data especially for women. For men, the mortality rates of the two cancers were elevated only modestly, which could possibly be explained by competing causes of death.
During the follow-up period, for every 100 men dying in Holmsland-Hanstholm, 107 men died in Thyborøn-Harboøre; and for every 100 women dying in Holmsland-Hanstholm, 103 women died in Thyborøn-Harboøre. These modestly elevated risks in overall mortality originated from a broad spectrum of diseases, but only the risk of cancer mortality reached statistical significance. The amount of hospital contact in Thyborøn-Harboøre was overall in line with that of the comparison area. Elevated risk of hospital contact was seen for cancer and psychiatric disorders; the latter in particularly for affective disorders in both men and women, and where anxiety in men reached a 4-fold elevated risk.
To assess the possible impact of pollution in Thyborøn-Harboøre on present inhabitants, we included also a cohort of inhabitants who were either born there or had moved to the area after 1990. In the cancer incidence study, the only notable finding in this younger cohort was a more than double risk of lung cancer in women. Nevertheless, when we now had a longer follow-up period, we found a clearly elevated risk of 28% for all-cause mortality; particularly in women where it amounted to 44%, and to 48% in women who had moved to the area.
Since the environmental contamination from the Love Canal landfill was identified in 197815, numerous studies of possible health consequences of residency in contaminated areas have been conducted16. It has been a challenge in most of these studies to accurately identify the exposed population. A cohort study from the Love Canal area was based on follow-up of residents interviewed in 1978–1982, but not all residents had been interviewed, and a possible selection could not be excluded15. In a recent study, the life expectancy was compared between US census tracts with and without Superfund sites. Mortality data from 2010 to 2015 were used assuming that these data reflected the population residing in the census tract long enough for the site exposure to have an impact on the life expectancy17.
The availability of long-standing population registers in the Nordic countries provides a possibility to overcome these limitations and to accurately identify individuals exposed to environmental hazards. For instance, in both Sweden18 and Finland19 all inhabitants living in areas affected by radiation fallout from the Chernobyl accident were identified from the population registers and individually followed up for later cancer occurrence. In Denmark, children born in 1940–1970 and attending schools near an asbestos-cement factory were identified from the city archive and followed up for occurrence of mesothelioma and other asbestos-related cancers20.
In a setting similar to the one reported on here, an investigation of mortality and health events covered Grindsted, a provincial town in Jutland, where a chemical factory started in 192413,21. Event occurrence over time in Grindsted was compared with that in comparable towns across Jutland. The analysis was adjusted for co-variates as e.g. education. In total, 39,000 people who had lived in Grindsted at some point in time were included in the analysis. The overall mortality rate was in line with that of the comparison towns, e.g. in 2011–2021 incidence rate ratio (IRR) 0.97 (95% CI 0.91–1.03). Cancer incidence was similar in the two areas, IRR 1.03 (95% CI 0.96–1.11) with some increased prostate cancer incidence among Grindsted-inhabitants in earlier years. Kidney cancer was not increased, and bladder cancer data not reported. Incidence of cardiovascular diseases was increased; IRR 1.08 (95% CI 1.03–1.14), but this excess did not derive from acute myocardial infarction, ischemic heart disease, or stroke. Occurrence of psychiatric disorders was slightly increased IRR 1.05 (95% CI 0.99–1.11). Although addressing similar problems, the methodologies were somewhat different, e.g. in definition of risk populations, and it was therefore not possible directly to compare the results of the Grindsted-report with those from the present study.
The elevated mortality in persons who moved to Thyborøn-Harboøre during the years 1990 to 2006, resembled the pattern seen in Danish citizens moving to other marginal geographic areas in Denmark during this period. In the rural-provincial area of Lolland-Falster, which includes the two southern Danish islands, people who moved in during 1998–2007 had a mortality rate ratio of 1.57 (95% CI 1.52–1.63) compared with Danes in general22. Health-related geographical relocation has thus contributed to mortality inequalities in Denmark. In the Thyborøn-Harboøre study, one may wonder why the risk estimates for cancer mortality was higher for the new than for the old cohort, especially because the opposite pattern was seen in the previous study of the cancer incidence8. However, it should be taken into account that in the cancer incidence study only cancers diagnosed after a given person had moved to Thyborøn-Harboøre were considered. In the mortality study, all cancer deaths after a given person had moved to Thyborøn-Harboøre were considered. So given the relatively long survival time for some cancer, e.g. bladder cancer, “sick” immigration could have contributed to the differences in the results.
It was a strength of the study that we had the comprehensive cohort of people living in Thyborøn-Harboøre during 1968–1970. In Denmark, the CPR allows for individual follow-up of all people who even had a permanent address in Denmark. Limitations were that causes of death were available only from 1970 onwards, hospital contact for somatic diseases only from 1977 onwards, and for psychiatric diseases from 1995. To map possible health problems for those living in Thyborøn-Harboøre after pollution came under control in the 1980s, we included a cohort of persons living in the area only in 1990–2006 and primarily consisting of people who had moved there. It was a strength that we could include a comparison cohort of people living at other fishing communities on the Danish West Coast during the same calendar years. In this way we controlled for possible differences in general living conditions, for occupational differences, and for possible dietary differences. By using individual data in the analysis, we controlled also for sex and age, and calendar time of follow-up. In our previous cancer incidence study, it was possible also to use comparison between study outcomes as an indirect control for confounding, e.g. we found excess risks for bladder and kidney cancer but not for lung cancer, indicating that tobacco smoking was not the causal agent behind the excess risks of bladder and kidney cancers. We could thus exclude a number of possible explanatory factors for the observed disease pattern, but it is not possible in an observational epidemiological study to conclusively identify causal associations. We found interaction between geographical area and calendar time, but this will not have affected our results, as calendar time was adjusted for in the calculation of risk estimates. Only the interaction between area and calendar time was statistically significant indicating that the difference in mortality between the geographical areas decreased over time. While mortality data were comprehensive, there may be some inaccuracies in registration of causes of death23. Use of hospital contacts may further be negatively affected by travel distances to hospitals24, and positively affected by limited access to private specialists, e.g. private, office-based psychiatrists. Finally, we did not have data on socioeconomic conditions, e.g. on people receiving public income support in pre-pensionable age, which might indicate presence of health-problems.
The mortality analysis confirmed the finding from the cancer incidence study of an elevated risk of kidney and bladder cancer in people living in Thyborøn-Harboøre in 1968–1970. Further investigation of possible causes is warranted. Otherwise, the Thyborøn-Harboøre inhabitants from 1968 to 1970 had a slightly elevated mortality rate and a hospital contact pattern similar to that of people living in other Danish West Coast fishing communities. One signal that deserves future monitoring was occurrence of psychiatric disorders, in particularly in men and boys.
Finally, in the 1990s and early 2000s, the data could indicate a possibly selective immigration to Thyborøn-Harboøre of people with health problems. Among women this was illustrated by an overall 48% elevated mortality rate compared with women moving to Holmsland-Hanstholm in the same period. Geography-related redistribution of health is known from Lolland-Falster, another marginal area of Denmark22. A careful follow-up of health in the present population is needed to assess whether selection at migration or exposures in the area are responsible for the elevated mortality rate in people who had moved to Thyborøn-Harboøre in 1990 to 2006.
This study was initiated to assess possible health consequences of the historical environmental pollution in Thyborøn-Harboøre. A doubled risk of kidney and bladder cancer has been found previously, and this finding was confirmed in the present study. Compared with men from other Danish West Coast communities, the overall mortality rate for men in Thyborøn-Harboøre was slightly elevated with small contributions from a broad range of causes of death. The pattern in use of hospital contact was well in accordance with that of the comparison area. Based on small numbers, the study indicated a need for future monitoring of occurrence of psychiatric disorders. The study could further indicate selective immigration to Thyborøn-Harboøre in the 1990s and early 2000s of people with health problems.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity. Pseudonomized data are stored in Statistics Denmark and can be accessed according to EU-data protections rules. Contact to: forskerservice@dst.dk and elsebeth@sund.ku.dk.
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- aRR:
-
Adjusted rate ratio—adjusted for sex (where relevant), running age, and calendar year
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CPR:
-
Central population register
- HH:
-
Holmsland-Hanstholm
- IBD:
-
Inflammatory bowel diseases
- ICD:
-
International classification of diseases
- NR:
-
Not reported
- OCD:
-
Obsessive compulsory disorder
- TH:
-
Thyborøn-Harboøre
References
Fazzo, L. et al. Hazardous waste and health impact: a systematic review of the scientific literature. Environ. Health. 16 (1), 107. https://doi.org/10.1186/s12940-017-0311-8 (2017).
Vrijheid, M. Health effects of residence near hazardous waste landfill sites: a review of epidemiologic literature. Environ. Health Perspect. 108 (Suppl 1), 101–112. https://doi.org/10.1289/ehp.00108s1101 (2000).
https://monographs.iarc.who.int/wp-content/uploads/2018/06/mono112-08.pdf [Accessed 27 March 2023].
Ringkjøbing Amtskommune. [Total environmental approval of A/S Cheminova]. Ringkøbing: Teknisk forvaltning, Ringkjøbing Amtskommune. [In Danish] (1988).
Riisgård, H. U. Mercury pollution in the waters around Harboøre Tange and Limfjord, Denmark. Mar. Pollut. Bull. 15 (4), 129–133 (1984).
https://arkiv.dk/vis/6075286 [Accessed 25 February 2024] [in Danish].
https://arkiv.dk/vis/6622886 [Accessed 25 February 2024] [in Danish].
https://mst.dk/affald-jord/jordforurening/generationsforureningerne/ [Accessed 27 March 2023] [In Danish].
Lynge, E., Holmsgaard, H. A., Holmager, T. L. F. & Lophaven, S. Cancer incidence in Thyborøn-Harboøre, Denmark: a cohort study from an industrially contaminated site. Sci. Rep. 11 (1), 13006. https://doi.org/10.1038/s41598-021-92446-y (2021).
Jensen, E. M. [Once up on a time in Lemvig. A Family History] (Copenhagen, 2015). [In Danish].
Blæsbjerg, K. [The best Families] (Copenhagen, 2023). [In Danish].
Møller–Hansen, K. & Torre, P. [News from the Danish Health Authority: Causes of Deaths] (Sundhedsstyrelsen, 1998). [In Danish].
Wodschow, K. et al. [Disease incidence among inhabitants in Grindsted. A register-based study.] Statens Institut for Folkesundhed, SDU, (2020). https://www.sdu.dk/sif/-/media/images/sif/udgivelser/2020/rapport_grindsted_final.pdf [Accessed 27 March 2023]. [In Danish].
https://nordcan.iarc.fr/en/dataviz/survival?populations=208&years_available=1943_2021&cancers=160 [Accessed 10 March 2024].
Gensburg, L. J. et al. Mortality among former Love Canal residents. Environ. Health Perspect. 117 (2), 209–216. https://doi.org/10.1289/ehp.11350 (2009). Epub 2008 Oct 1.
Sinnett, D., Bray, I., Baranyi, G., Braubach, M. & Netanyanhu, S. Systematic Review of the Health and Equity Impacts of Remediation and Redevelopment of Contaminated Sites. Int. J. Environ. Res. Public. Health. 19 (9), 5278. https://doi.org/10.3390/ijerph19095278 (2022).
Kiaghadi, A., Rifai, H. S. & Dawson, C. N. The presence of Superfund sites as a determinant of life expectancy in the United States. Nat. Commun. 12 (1), 1947. https://doi.org/10.1038/s41467-021-22249-2 (2021).
Tondel, M., Hjalmarsson, P., Hardell, L., Carlsson, G. & Axelson, O. Increase of regional total cancer incidence in north Sweden due to the Chernobyl accident? J. Epidemiol. Community Health. 58 (12), 1011–1016. https://doi.org/10.1136/jech.2003.017988 (2004).
Auvinen, A. et al. Chernobyl fallout and cancer incidence in Finland. Int. J. Cancer. 134 (9), 2253–2263. https://doi.org/10.1002/ijc.28554 (2014).
Dalsgaard, S. B., Würtz, E. T., Hansen, J., Røe, O. D. & Omland, Ø. Cancer incidence and risk of multiple cancers after environmental asbestos exposure in Childhood-A Long-Term Register-based Cohort Study. Int. J. Environ. Res. Public. Health. 19 (1), 268. https://doi.org/10.3390/ijerph19010268 (2021).
Kjærulff, T. M. et al. [Disease Incidence among Inhabitants in Grindsted – updated] (Statens Institut for Folkesundhed, SDU, 2024).
Holmager, T. L. F., Lophaven, S. N., Mortensen, L. H. & Lynge, E. Does Lolland-Falster make people sick, or do sick people move to Lolland-Falster? An example of selective migration and mortality in Denmark, 1968–2017. Soc. Sci. Med. 277, 113893. https://doi.org/10.1016/j.socscimed.2021.113893 (2021).
Mikkelsen, L. et al. Assessing the quality of cause of death data in six high-income countries: Australia, Canada, Denmark, Germany, Japan and Switzerland. Int. J. Public. Health. 65 (1), 17–28. https://doi.org/10.1007/s00038-019-01325-x (2020).
Fuglsang, N. A. et al. Geographical inequalities in the decreasing 28-day mortality following incident acute myocardial infarction: a Danish register-based cohort study, 1987–2016. BMC Cardiovasc. Disord. 22 (1), 81. https://doi.org/10.1186/s12872-022-02519-7 (2022).
Acknowledgements
We are indebted to Tom Grimsrud and Eero Pukkala for references to Nordic studies.
Funding
The study was funded by the Central Region of Denmark, 1-30-72-172-18. The funder had no impact on the design, analysis, interpretation and reporting of the findings.
Author information
Authors and Affiliations
Contributions
E.L. and S.L. designed the study. S.L. undertook the analysis. E.L. wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval, consent to participate and experimental protocol
The study was a retrospective cohort study. Data were retrieved from the Danish Central Population Register, the Danish Cause of Death Register, and the Danish National Patient Register. These databases are not publicly available, but the databases can be used for research projects considered beneficial for the society. The use of data and the experimental protocol were approved by Region Zealand with the registration number REG-108-2018. Region Zealand is the public authority in charge of Nykøbing Falster Hospital, where the study was undertaken. According to Danish legislation, approval by the relevant public authority serves as ethical approval of studies based entirely on register-data. No contact was made to patients, their relatives, and/or treating physicians. Informed consent was thus waived by Region Zealand. The experimental protocol followed standard guidelines for cohort studies. To ensure data safety, numbers below 5 were not reported. The study was funded by the Central Region of Denmark, 1-30-72-172-18. The funder had no impact on the design, analysis, interpretation and reporting of the findings.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lynge, E., Holmsgaard, H., Jensen, J.B. et al. Death and hospital contact in a cohort from Thyborøn-Harboøre an environmentally contaminated site in Denmark. Sci Rep 14, 31105 (2024). https://doi.org/10.1038/s41598-024-82307-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-82307-9