Abstract
This study aims to explore the feasibility of applying the “Three-Low” technique (low injection rate, low iodine contrast volume, low radiation dose) in coronary CT angiography (CCTA). We prospectively collected data from 90 patients who underwent CCTA at our hospital between 2021 and 2024. The patients were randomly assigned to either the experimental group (n = 45) or the control group (n = 45). The experimental group parameters were as follows: injection rate of 3.5-4.0 ml/s, iodine contrast volume of 35–40 ml, tube voltage of 100 kVp, and tube current of 250 mA. The control group parameters were: injection rate of 4.5-5.0 ml/s, iodine contrast volume of 45–50 ml, tube voltage of 120 kVp, and tube current of 450 mA. Both groups received a high-concentration, non-ionic, water-soluble contrast agent (Iomeprol, 40 gl/100 ml). The heart rate of all patients was ≤ 70 bpm, and breath-hold scanning was performed after breathing training. The study compared the CT values of the left anterior descending artery, left circumflex artery, right coronary artery, and aorta, as well as background noise, signal-to-noise ratio (SNR), volumetric CT dose index, dose-length product, effective radiation dose, and total iodine dose between the two groups. In the control group, no cases of contrast extravasation occurred, while 6 cases of extravasation were observed in the experimental group (p = 0.026). There was no significant difference between the groups in terms of vascular image quality (mean vascular image quality score: experimental group 4.27 ± 0.62 vs. control group 4.24 ± 0.57, p > 0.05) or vascular motion artifact score (mean vascular motion artifact score: experimental group 4.20 ± 0.59 vs. control group 4.13 ± 0.55, p > 0.05). However, significant differences were found between the experimental and control groups in the CT values of the left anterior descending artery (experimental group: 571.31 ± 49.66 HU vs. control group: 449.20 ± 36.80 HU, p < 0.05), left circumflex artery (experimental group: 570.41 ± 49.98 HU vs. control group: 450.95 ± 39.27 HU, p < 0.05), right coronary artery (experimental group: 584.52 ± 53.70 HU vs. control group: 452.66 ± 40.67 HU, p < 0.05), aorta (experimental group: 624.91 ± 48.99 HU vs. control group: 465.36 ± 34.37 HU, p < 0.05), background noise (experimental group: 24.76 ± 1.97 vs. control group: 19.09 ± 1.69, p < 0.05), SNR (experimental group: 25.30 ± 1.81 vs. control group: 24.47 ± 1.75, p < 0.05), volumetric CT dose index (experimental group: 22.97 ± 1.47 mGy vs. control group: 50.53 ± 4.89 mGy, p < 0.05), dose-length product (experimental group: 363.68 ± 21.45 mGy·cm vs. control group: 782.41 ± 58.20 mGy·cm, p < 0.05), and effective radiation dose (experimental group: 5.09 ± 0.30 mSv vs. control group: 10.95 ± 0.81 mSv, p < 0.05).The results of the Fisher test indicated that the extravasation rate was significantly higher in the high injection rate group compared to the low injection rate group (P = 0.024). The “Three-Low” technique in CCTA imaging effectively reduces the incidence of contrast extravasation caused by high injection rates and decreases the radiation dose, making it a highly feasible option for clinical application and worthy of broader adoption.
Similar content being viewed by others
Coronary artery atherosclerotic heart disease is one of the most prevalent cardiovascular diseases in clinical practice, with an increasing incidence trend and a trend toward younger onset ages1. Coronary artery CT angiography (CCTA) is a non-invasive diagnostic tool widely employed for evaluating coronary arteries, demonstrating accuracy comparable to coronary angiography. It enables the analysis of coronary artery origin, course, and plaque progression2. However, coronary artery imaging in CT faces significant challenges due to the necessity for high temporal resolution to minimize motion artifacts caused by cardiac motion and high spatial resolution to delineate small coronary artery structures3.To meet the demands for image quality, high injection rates and multiple doses of iodine-based contrast agents are often required during examinations. Additionally, to fulfill the increasing requirements for spatial and temporal resolution, higher X-ray radiation doses are necessary to prevent the escalation of image noise. High injection rates may lead to contrast agent leakage, particularly in challenging vascular conditions, such as emergency settings and unconscious patients under intensive care unit (ICU) monitoring. Excessive intake of iodine-based contrast agents increases the risk of allergic reactions and can cause acute kidney injury and contrast-induced nephropathy. Overexposure to ionizing radiation may result in genetic mutations4,5,6. These factors are crucial considerations, emphasizing the need for appropriate iodine contrast agent doses at specific rates, maintaining a constant dose throughout the procedure, preventing contrast agent waste, and optimizing the cost associated with the rapid scan times provided by CT equipment7, serving as a patient protection measure.Therefore, reducing iodine contrast agent injection rates and doses, as well as minimizing radiation exposure, is advantageous for patients. Consequently, selecting an optimal scanning protocol in CCTA imaging remains an ongoing topic of interest8,9. This study explores the feasibility of implementing the “Three Low” technique (low injection rate, low iodine contrast agent dose, and low radiation dose) in CCTA examinations.In this study, we optimized the scanning protocol by utilizing SnapShot Assist(SSA)technology, reducing tube voltage and current, and applying prospective ECG gating to minimize radiation dose while maintaining high image quality. Additionally, we employed AI-based denoising techniques, integrating Transformer models with deep convolutional neural networks (CNN), to enhance image quality through deep learning, compensating for any potential quality reduction due to the lower radiation dose. Finally, the images acquired were analyzed and enhanced using AI-based tools to mitigate any loss of detail that might have resulted from the reduced contrast agent dosage.
Materials and methods
General information
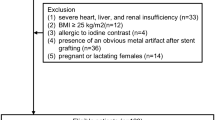
This prospective cohort study was approved by the Ethics Committee of the Second Affiliated Hospital of Xiamen Medical College, and all patients signed a written informed consent form before the examination. The study was conducted in accordance with the Declaration of Helsinki (revised 2013). Ninety subjects were selected from our hospital who underwent CCTA in 2021–2024, detailed inclusion and exclusion criteria are shown in Fig. 1.They were randomly divided into experimental group (45 subjects) and control group (45 subjects) respectively. The mean age of the experimental group was 58.16 ± 11.75 years, with an age range of 32 to 79 years and a mean body mass index (BMI) of 21.90 ± 1.25 Kg/m². The mean age of the two control groups was 56.76 ± 11.51 years, age range 32 to 74 years, and mean body mass index (BMI) 22.09 ± 0.94Kg/m². Comparing the general information of the two groups, the difference was not statistically significant (p > 0.05) and was comparable. Refer to Table 1 for details.
Methods
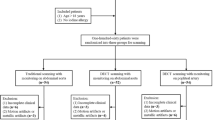
In both groups, CCTA examinations were conducted using the GE revolution GSI 64-slice spiral CT with a prospective ECG-gated scanning mode. The pitch was automatically adjusted according to the patient’s heart rate, with a rotation speed of 0.35 r/s. For the experimental group, the tube voltage was set to 100 kVp and the tube current to 250 mA, while for the control group, the tube voltage was set to 120 kVp and the tube current to 450 mA. The experimental group also employed SnapShot Assist (SSA) technology, which automatically adjusts the scan trigger point based on the patient’s real-time heart rate, optimizing coronary artery imaging. SSA technology enhances image clarity and reduces motion artifacts by automatically identifying and selecting the appropriate cardiac phase for imaging. Additionally, SSA contributes to lowering radiation exposure by ensuring the acquisition of clear images with minimal radiation through precise time triggering and optimized scan parameters.The acquired scan images were reconstructed using an iterative algorithm (ASIR) and deep learning-based AI denoising techniques, which combine Transformer models with deep convolutional neural networks (CNN). The AI denoising technique used an Efficient Self-Attention U-Net (ESAU-Net) and Multi-Scale Anatomical Contrast Network (MAC-Net). First, ESAU-Net was introduced with a channel self-attention mechanism to better capture global-local interactions and accommodate high-resolution inputs. Second, MAC-Net combined block-wise non-contrast modules to capture inherent anatomical information with pixel-wise contrast modules to maintain intrinsic anatomical consistency10 (Fig. 2).The reconstructed image slice thickness was 0.625 mm, with an inter-slice spacing of 0.625 mm. All patients underwent breath-holding training prior to the examination and were positioned supine, feet-first. The scanning range extended from the tracheal carina level to the cardiac apex. All patients received high-concentration non-ionic water-soluble iodine contrast agent (Iomeprol, 40 gl/100 ml) injected through an 18-G closed intravenous catheter in the right antecubital vein. The experimental group had an injection rate of 3.5-4.0 ml/s, with a total iodine contrast volume of 35–40 ml, tube voltage of 100 kVp, and tube current of 250 mA. The control group had an injection rate of 4.5-5.0 ml/s, with an iodine contrast volume of 45–50 ml, tube voltage of 120 kVp, and tube current of 450 mA. After contrast injection, both groups received a 40 ml saline flush at a relative rate. Scanning was initiated using contrast tracking technology, with a region of interest (ROI) placed at the ascending aortic root, and a threshold of 150 HU was set. Once the threshold was reached, the machine automatically prompted the patient to hold their breath for scanning (Figs. 3 and 4).
Comparison of representative CCTA images from adaptive iterative reconstruction ASIR and deep learning AI denoising techniques. A 48-year-old man with a body mass index of 23 BMI. red outlined area shows a zoomed-in image of CCTA detail demonstrating that deep learning-based AI denoising techniques can show coronary artery branching and calcification more clearly compared to adaptive statistical iterative reconstruction (ASIR). In addition, the overall image quality around these structures is significantly enhanced, providing more detailed and accurate diagnostic information.
Image quality
The acquired scanning images were reconstructed using the iterative algorithm ASIR and the AI noise reduction technique based on the application of Transformer and deep convolutional neural network (CNN) for deep learning of the images respectively. Then the images were transferred to the post-processing workstation AW4.7, and the images were analyzed and enhanced by the post-processing of the Artificial Intelligence Coronary Artery Software (ShuKun AI). Post-processing techniques such as multiplanar reconstruction, surface reconstruction, and volume reproduction were used to display the coronary artery trunk and its branches. Observe the image quality of the two groups and compare the image quality and quantitative parameters of the two groups. Two senior diagnostic radiologists with twenty years of cardiac diagnostic experience and one senior cardiovascular clinician with twenty-eight years of experience at our institution were selected to subjectively evaluate the image results, and the image scores were evaluated using the 5-point method.: 5 points for excellent coronary artery opacification, clear visualization with continuous vessel display without motion artifacts; 4 points for good coronary artery opacification, relatively clear visualization with minimal motion artifacts; 3 points for fair coronary artery opacification, slightly unclear visualization, suitable for diagnosis with some motion artifacts; 2 points for poor coronary artery opacification, blurry and unclear images, challenging for diagnosis with significant motion artifacts; and 1 point for very poor coronary artery opacification, unclear images unsuitable for diagnosis11.Each CCTA was completed by a senior nurse with twenty-one years of experience who assessed the patient for the presence of contrast extravasation. Two senior radiologists and two senior cardiovascular clinical physicians, not involved in the study, independently evaluated each CCTA imaging session within 48 h. CT reports were categorized into diagnostic and non-diagnostic reports. The quantitative parameters include the measurements of the CT values for the three major branches of the coronary arteries: the Left Anterior Descending (LAD), the Left Circumflex (LCX), and the Right Coronary Artery (RCA) in two groups of images. For each branch, the CT values at the proximal, mid, and distal segments were measured (Fig. 5). The average CT value of these three locations was calculated to obtain the final mean CT values for the LAD, LCX, and RCA, as well as the aortic CT value. The standard deviation (SD) of the aortic CT value was used as background noise, and the signal-to-noise ratio (SNR) was calculated as SNR = aortic CT value / SD. Additionally, iodine intake was determined by the total iodine contrast agent volume (ml) × 0.4 g iodine.
Radiation dose
Radiation dose metrics included Computed Tomography Dose Index (CTDIvol), Dose Length Product (DLP), and Effective Dose (ED). The CT machine automatically measured and recorded both DLP and CTDIvol. The effective dose (ED) was calculated as ED = DLP × k, where k = 0.014 mSv/(mGy·cm)12.
Data analysis
Statistical analysis and data processing for this study were conducted using SPSS22.0 software. Categorical data were expressed as percentages (%), and the chi-squared test (X2) was employed for analysis. Normally distributed continuous data were presented as mean ± standard deviation (X̄ ± S), and the t-test was applied. Variance is used to describe the degree of dispersion of the data; the larger the value of the variance, the more dispersed the data is.For non-normally distributed continuous data, the median and interquartile range were represented as M(P25, P75). The assessment of consistency utilized the Kappa test, where Kappa values ≤ 0.4 indicated poor consistency, 0.40 < Kappa values < 0.75 denoted moderate consistency, and Kappa values ≥ 0.75 indicated high consistency. Statistical significance was set at P < 0.0513.
Results
Comparison of image quality between the two groups
The comparison of image quality between the two groups showed no statistically significant difference (P > 0.05). The agreement between the results of the subjective evaluation opinions of two senior diagnostic radiologists with twenty years of cardiac diagnostic experience and one senior cardiovascular clinician with twenty-eight years of experience was relatively high (Kappa = 0.80) and the agreement between the results of the vasomotor artifact score opinion was relatively high (Kappa = 0.79). Both groups’ images were deemed adequate for diagnostic purposes, as shown in Table 2.
The quantitative parameters of the two examination methods were measured and statistically analyzed by two senior radiologists, each with twenty years of experience
When measuring the CT values of the LAD, LCX, and RCA, the aortic CT value, background noise, SNR, and iodine intake in both the experimental and control groups, the inter-rater consistency between the two radiologists was moderate (Kappa = 0.71). There was a statistically significant difference between the experimental and control groups (P < 0.05) ( Table 3). The experimental group demonstrated superior performance in key parameters such as CT values, iodine intake, and image quality, exhibiting significant clinical advantages. Although background noise increased, the overall image quality remained superior to that of the control group.
Furthermore, we applied advanced deep learning reconstruction technology combining Transformers and deep convolutional neural networks (CNN) to the images in the experimental group. This technique leverages the Transformer’s efficient global feature capture capability and the CNN’s strength in local feature extraction, significantly enhancing the clarity of overall structures and surrounding tissues. It effectively reduces noise interference while preserving image details, thereby providing more accurate and detailed diagnostic information (Fig. 3).
Building upon this, we further utilized AI software to refine the reconstructed images, with a particular focus on enhancing and identifying coronary artery details. This process significantly improved the visualization of stenosis, calcification, and plaque features (Fig. 4), allowing for clearer presentation of complex coronary artery lesions. This technology is crucial for the accurate diagnosis of coronary artery diseases, reducing the risk of misdiagnosis and missed diagnoses, and providing physicians with more precise decision-making information, thereby greatly improving the accuracy and reliability of clinical diagnoses.
Comparison of radiation dose between the two groups
There were statistically significant differences in CTDIvol, DLP, and ED between the experimental group and the control group (P < 0.01). Refer to Table 4 for details.By utilizing advanced image reconstruction technology and AI recognition techniques, the experimental group successfully reduced patient radiation exposure while maintaining diagnostic accuracy. This technological advancement not only ensures the clear identification of coronary artery lesions, such as stenosis, calcification, and plaque, but also significantly reduces the long-term radiation risks associated with traditional imaging methods.Through the integration of innovative deep learning reconstruction algorithms and fixed low mA techniques, the experimental group optimized radiation dosage and improved image quality, particularly in cardiac and vascular structures where imaging precision is critical. Traditional coronary CTA scans are often associated with higher radiation doses, which poses a significant concern for patients requiring multiple scans, such as those at high risk for coronary artery disease. The new technology not only mitigates this risk but also retains the high-resolution imaging capability needed to detect small lesions, such as early-stage plaques.
The contrast extravasation between the two groups was evaluated by a senior nurse with 21 years of experience, who assessed whether contrast extravasation occurred in patients (Table 5). To assess the difference in contrast extravasation rates between the low injection rate group (experimental group) and the high injection rate group (control group), we utilized Fisher’s exact test. The results indicated that the incidence of extravasation was significantly higher in the high injection rate group compared to the low injection rate group (P = 0.026). Detailed information regarding the injection rates, contrast agent doses, the pressure exerted on the veins during injection, and the occurrence of contrast extravasation for both groups is presented (Table 6).
This finding suggests that injection rate is a key factor influencing the risk of contrast extravasation. A higher injection rate significantly increases vascular pressure, thereby raising the risk of extravasation, especially in patients with poor vascular conditions. Conversely, a lower injection rate can effectively reduce the occurrence of extravasation and is safer for patients with compromised venous status. However, in certain imaging procedures where high contrast resolution is required, a lower injection rate might affect image contrast and clarity.
Therefore, in clinical practice, injection rates should be flexibly adjusted based on the individual patient’s condition. For patients with poor vascular conditions or those requiring frequent imaging, a lower injection rate should be prioritized. Additionally, real-time monitoring of injection pressure and the use of automated injection systems can further reduce the risk of extravasation and enhance patient safety.
Discussion
Coronary artery disease (CAD) is the leading cause of death globally, resulting from the pathological dysfunction of the coronary arteries. It occurs when changes in the arterial walls lead to the accumulation of atherosclerotic plaques, causing narrowing and constriction of the vascular lumen, ultimately limiting blood flow14. For individuals with CAD, early diagnosis and treatment are essential to improve their chances of survival. In recent years, CCTA has gained widespread use in the diagnosis of coronary artery disease due to its rapid and minimally invasive nature15. However, the parameters associated with CCTA examinations, including injection rates, iodinated contrast agent volumes, and radiation doses, have consistently been a focal point of clinical concern16.In the process of conducting CCTA examinations, it is imperative to reduce the potential adverse effects on patients by ensuring image quality while lowering the injection rate of iodinated contrast agents, reducing their volume, and minimizing radiation exposure. This requires careful consideration to balance the trade-offs between image quality and patient safety9,17.
In this study, we employed the “Three-Low” technique, which involves low injection rates, low iodinated contrast agent volumes, and low radiation doses in the scan protocol. This approach offers several advantages:
-
1.
Low iodinated contrast agent injection rate to reduce the risk of contrast agent leakage.
The selection of an optimal iodine contrast agent administration protocol is crucial during CCTA, as the diagnostic capability for coronary artery diseases heavily relies on the opacification of the intricate vasculature within the coronary arteries18. The necessity for rapid intravenous injection of a large volume of iodine-based contrast agent arises; however, due to the high concentration and viscosity of the contrast agent, rapid injection over a short duration can lead to vascular damage, causing complications such as leakage19. Adverse reactions to iodine-based contrast agents are common risk factors for contrast-induced encephalopathy (CIE)20. Fortunately, most cases of contrast agent extravasation result in mild symptoms, such as redness, swelling, localized erythema, and pain. In rare instances, severe extravasation may lead to skin blistering, tissue necrosis, and, exceptionally, compartment syndrome21. Particularly in unconscious patients under intensive care unit (ICU) monitoring, high injection pressure can significantly increase the risk of vascular injury. Therefore, a cautious approach with low injection rates is recommended to minimize extravasation, thereby reducing the occurrence of adverse reactions in patients.In our pre-experimental BMI distribution range of 20-25Kg/m², iodine delivery rate (IDR) emerged as a critical factor influencing vascular attenuation during contrast agent injection. Consequently, we designed a stepwise low IDR injection protocol tailored to varying BMI, aiming to maintain low vascular pressure values monitored by a high-pressure injector throughout the contrast agent injection. This approach substantially reduces the likelihood of vascular injury. The experimental group exhibited satisfactory image quality, aligning with expectations. In comparison to the control group, the experimental group demonstrated attenuations > 400 Hounsfield Units (HU) in the aortic root and the three major branches of the coronary vasculature. This resulted in an increased number of ideal vessels, effectively achieving the objectives of the experiment.
-
2.
Utilizing deep learning combined with artificial intelligence (AI) coronary software for post-processing analysis and image enhancement.
The application of AI denoising techniques based on Transformer models and deep convolutional neural networks (CNN) in reconstructing CCTA images offers a significant advancement in imaging quality, particularly under low-dose scanning conditions. This advanced AI-driven approach not only effectively reduces noise in CCTA images but also preserves crucial anatomical details. Such preservation of detail is critical because it ensures that, even with the reduction in radiation exposure, the diagnostic accuracy remains uncompromised, maintaining the integrity of the imaging data22.Deep learning denoising algorithms, such as those based on the combination of Transformer and CNN architectures, have been shown to reduce radiation doses by up to 50% without sacrificing image quality. This is particularly important in clinical settings where minimizing patient radiation exposure is a priority. The AI software employed also plays a crucial role in identifying and enhancing coronary artery features, such as stenosis, calcifications, and plaques, which are critical for the accurate diagnosis of coronary artery disease23.The introduction of AI denoising technology has not only maintained but, in many cases, improved image quality under low-dose conditions. This reduction in radiation exposure significantly lowers long-term health risks for patients, which is a vital consideration in repeated or widespread use of CCTA. Moreover, the enhancement in image quality and diagnostic precision, coupled with the increased workflow efficiency and improved patient experience, represents a comprehensive improvement in cardiovascular imaging practices. Additionally, this technology provides robust support for analyzing complex cases, making it a valuable tool in the continued advancement of cardiovascular imaging and diagnostics24.This deeper integration of AI into CCTA imaging is not just a technical improvement but represents a broader shift towards safer, more accurate, and more efficient diagnostic practices in cardiology. By enabling clinicians to obtain high-quality diagnostic images with reduced radiation exposure, AI is poised to significantly impact patient care and outcomes, particularly in the early detection and management of coronary artery disease.
-
3.
Low radiation dosage can help mitigate the harm caused by ionizing radiation to the human body.
Human beings are consistently exposed to various types of radiation, with a prevalent use of radiation in most hospitals worldwide for diagnostic imaging or cancer treatment. While these imaging technologies offer certain benefits, the potential cancer risks associated with such studies remain controversial25. Research indicates that excessive ionizing radiation can cause cellular damage and elevate the risk of cancer, with the degree of risk increasing proportionally with the dose administered26. In recent years, a series of studies have explored methods to reduce radiation doses, such as lowering tube voltage, decreasing mAs, among others, all of which have shown significant efficacy.One approach to reducing radiation dose involves lowering tube voltage. Current international guidelines recommend using 120 kVp for CCTA27. However, in this study, a scanning approach with 100 kVp was employed, resulting in a substantial reduction of approximately 50-60% in radiation dose. This significant reduction in radiation dose can markedly decrease the amount of radiation exposure to individuals undergoing the examination.
-
4.
Enhancing image quality is crucial for improving the diagnosis of medical conditions.
Studies have shown that using a low tube voltage (100 kVp) results in greater vascular enhancement, with a signal-to-noise ratio (SNR) comparable to the traditional 120 kVp protocol, while reducing radiation exposure by 50%28. Additionally, lower tube voltage enhances iodine contrast because the attenuation coefficient of iodine-based contrast agents increases at lower X-ray photon energies, meaning the contrast agent absorbs lower-energy X-rays more effectively, thus improving CCTA image quality29. In this study, we reduced the traditional 120 kVp tube voltage to 100 kVp, and the results showed that the CT values of the LAD, LCX, RCA, and aorta in the experimental group were superior to those in the control group, with higher SNR and better overall image quality. However, using low tube voltage increased background image noise, which had a relatively small impact on vascular imaging but a more significant effect on soft tissue imaging30. To address the image quality issues caused by low tube voltage, we applied AI denoising techniques based on Transformer and deep convolutional neural networks (CNN) for deep learning-based image reconstruction. This significantly improved image quality, and further post-processing analysis and image enhancement using AI coronary software enhanced diagnostic accuracy. Therefore, the 100 kVp protocol provides better overall diagnostic image quality and can be effectively used in CCTA.
This study has several limitations: (1)The study focused on individuals with normal BMI (20–25 kg/m²), and the impact of lower tube voltage techniques (such as 80 kVp) on individuals with lower BMI or higher BMI was not investigated. Further research is needed to assess whether different tube voltage settings are suitable for patients with varying BMI.(2)The sample sizes in each group were relatively small. Conducting larger-scale studies with more participants would provide stronger and more conclusive evidence regarding the effectiveness of the “Triple-Low” technique in different patient populations.(3)The study did not specifically address the impact of heart rates greater than or equal to 70 beats per minute on image quality. This is an important factor, as high heart rates can affect image quality in cardiac imaging. Future studies may explore this aspect to provide a more comprehensive understanding of the technique’s applicability.(4)This study did not compare the diagnostic performance of coronary artery stenosis with the established gold standard, invasive coronary angiography (ICA). The absence of this comparison limits our ability to fully evaluate the accuracy of coronary CT angiography (CCTA).
Addressing these limitations in future research can further validate the findings and provide more comprehensive insights into the use of the “Triple-Low” technique in CCTA.
In summary, the use of the “Triple-Low” technique in performing CCTA scans has several benefits. It increases the success rate of CCTA scans in patients with poor vascular conditions, reduces the occurrence of iodine contrast agent extravasation, minimizes the risk of allergic reactions, prevents acute kidney injury and contrast-induced nephropathy, and lowers the potential harm of ionizing radiation to the human body. Additionally, the “Triple-Low” technique enhances image quality and improves disease diagnosis. These findings support the clinical application and wider adoption of the “Triple-Low” technique in CCTA procedures.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Benjamin, E. J. et al. Heart disease and stroke statistics-2019 update: A Report From the American Heart Association. Circulation ;139(10):e56-e528. https://doi.org/10.1161/CIR.0000000000000659 (2019). Erratum in: Circulation. 141(2):e33 (2020).
Knuuti, J. et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J;41(3):407–477. https://doi.org/10.1093/eurheartj/ehz425 (2020). Erratum in: Eur Heart J. 41(44):4242 (2020).
Yu, L. et al. Radiation dose reduction in computed tomography: Techniques and future perspective. Imaging Med. 1 (1), 65–84 (2009).
Timal, R. J. et al. Effect of no prehydration vs sodium bicarbonate Prehydration Prior to contrast-enhanced computed Tomography in the Prevention of Postcontrast Acute Kidney Injury in adults with chronic kidney disease: The Kompas Randomized Clinical Trial. JAMA Intern. Med. 180 (4), 533–541. https://doi.org/10.1001/jamainternmed.2019.7428 (2020).
Park, H. J. et al. Relationship between lower dose and Injection Speed of Iodinated Contrast Material for CT and Acute hypersensitivity reactions: An observational study. Radiology 293 (3), 565–572. https://doi.org/10.1148/radiol.2019190829 (2019).
Saleh, H. M. & Hassan, A. I. Editorial: Ionizing radiation and reproductive health. Front. Public. Health. 11, 1147934. https://doi.org/10.3389/fpubh.2023.1147934 (2023).
Faggioni, L. & Gabelloni, M. Iodine concentration and optimization in computed tomography angiography: Current issues. Invest Radiol. 51(12), 816–822. https://doi.org/10.1097/RLI.0000000000000283 (2016).
Nijssen, E. C. et al. Prophylactic hydration to protect renal function from intravascular iodinated contrast material in patients at high risk of contrast-induced nephropathy (AMACING): A prospective, randomised, phase 3, controlled, open-label, non-inferiority trial. Lancet. 389(10076), 1312–1322. https://doi.org/10.1016/S0140-6736(17)30057-0 (2017).
Rengo, M. et al. Impact of iodine concentration and iodine delivery rate on contrast enhancement in coronary CT angiography: A randomized multicenter trial (CT-CON). Eur. Radiol. 29 (11), 6109–6118. https://doi.org/10.1007/s00330-019-06196-7 (2019).
Chen, Z., Gao, Q., Zhang, Y. & Shan, H. ASCON: Anatomy-aware supervised contrastive learning framework for low-dose CT denoising. MCCAI 2023. (2023).
McGraw, S., Carlson, C., Grant, K. & Nijjar, P. S. Feasibility of ultra low-dose coronary computed tomography angiography. Indian Heart J. 70(3), 443–445. https://doi.org/10.1016/j.ihj.2017.09.004 (2018).
Scott-Moncrieff, A. et al. Real-world estimated effective radiation doses from commonly used cardiac testing and procedural modalities. Can. J. Cardiol. 27(5), 613–618. https://doi.org/10.1016/j.cjca.2011.01.011 (2011).
Yin, W. H. et al. Iterative reconstruction to preserve image quality and diagnostic accuracy at reduced radiation dose in coronary CT angiography: An intraindividual comparison. JACC Cardiovasc. Imaging. 6 (12), 1239–1249 (2013).
Sharma, B., Chang, A. & Red-Horse, K. Coronary artery development: Progenitor cells and differentiation pathways. Annu. Rev. Physiol. 79, 1–19. https://doi.org/10.1146/annurev-physiol-022516-033953 (2017).
Salavati, A. et al. Dual-source computed tomography angiography for diagnosis and assessment of coronary artery disease: Systematic review and meta-analysis. J. Cardiovasc. Comput. Tomogr. 6(2), 78–90. https://doi.org/10.1016/j.jcct.2011.10.018 (2012).
Kooiman, J. et al. Randomised trial of no hydration vs sodium bicarbonate hydration in patients with chronic kidney disease undergoing acute computed tomography-pulmonary angiography. J. Thromb. Haemost. 12(10), 1658–1666. https://doi.org/10.1111/jth.12701 (2014).
Singh, V. K. & Pollard, H. B. Ionizing radiation-induced altered microRNA expression as biomarkers for assessing acute radiation injury. Expert Rev. Mol. Diagn. 17 (10), 871–874. https://doi.org/10.1080/14737159.2017.1366316 (2017).
Kim, E. Y., Yeh, D. W., Choe, Y. H., Lee, W. J. & Lim, H. K. Image quality and attenuation values of multidetector CT coronary angiography using high iodine-concentration contrast material: A comparison of the use of iopromide 370 and iomeprol 400. Acta Radiol. 51 (9), 982–989 (2010).
Karády, J. et al. The effect of four-phasic versus three-phasic contrast media injection protocols on extravasation rate in coronary CT angiography: A randomized controlled trial. Eur. Radiol. 27 (11), 4538–4543 (2017).
Liu, M. R., Jiang, H., Li, X. L. & Yang, P. Case report and literature review on low-osmolar, non-ionic iodine-based contrast-induced encephalopathy. Clin. Interv Aging. 15, 2277–2289. https://doi.org/10.2147/CIA.S280931 (2020).
Alami, Z., Nasri, S., Ahid, S. & Kacem, H. H. Extravasation of contrast medium during CT examination: An observational case-control study. Pan Afr. Med. J. 20, 89. https://doi.org/10.11604/pamj.2015.20.89.3276 (2015).
Green, M., Marom, E. M., Konen, E., Kiryati, N. & Mayer, A. 3-D neural denoising for low-dose coronary CT angiography (CCTA). Comput. Med. Imaging Graph. 70, 185–191. https://doi.org/10.1016/j.compmedimag.2018.07.004 (2018).
Joshi, M. et al. Current and future applications of artificial intelligence in cardiac CT. Curr. Cardiol. Rep. 25, 109–117. https://doi.org/10.1007/s11886-022-01837-8 (2023).
Lin, A. et al. Artificial intelligence: Improving the efficiency of cardiovascular imaging. Expert Rev. Med. Devices. 17 (6), 565–577. https://doi.org/10.1080/17434440.2020.1777855 (2020).
Schultz, C. H., Fairley, R., Murphy, L. S. & Doss, M. The risk of cancer from CT scans and other sources of low-dose radiation: A critical appraisal of methodologic quality. Prehosp Disaster Med. 35(1), 3–16. https://doi.org/10.1017/S1049023X1900520X (2020).
Szalai, S. et al. Assessment of the potential impacts of the Chernobyl nuclear disaster on maternal and fetal health in Hungary. J. Matern. Fetal Neonatal Med. 35(25), 9481–9488. https://doi.org/10.1080/14767058.2022.2044471 (2022).
Ramjattan NA, Lala V, Kousa O, Makaryus AN. Coronary CT Angiography. 2023 Jan 19. In: StatPearls [Internet]. Treasure Island (FL). StatPearls Publishing (2023).
Hausleiter, J. et al. Image quality and radiation exposure with a low tube voltage protocol for coronary CT angiography results of the PROTECTION II Trial. JACC Cardiovasc Imaging. 3(11), 1113–1123. https://doi.org/10.1016/j.jcmg.2010.08.016 (2010).
Prasad, S. R., Wittram, C., Shepard, J. A., McLoud, T. & Rhea, J. Standard-dose and 50%-reduced-dose chest CT: Comparing the effect on image quality. AJR Am. J. Roentgenol. 179(2), 461–465. https://doi.org/10.2214/ajr.179.2.1790461 (2002).
Ghekiere, O. et al. Image quality in coronary CT angiography: Challenges and technical solutions. Br. J. Radiol. 90(1072), 20160567. https://doi.org/10.1259/bjr.20160567 (2017).
Acknowledgements
Not Applicable.
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
Shaochuan Wang:Writing - Original Draft,Zhengwen Sun:Writing - Review and editing,Yihong Zeng:Formal analysis,Yan Wang:Project administration, Xinyu Xu:Data Curation,Xueqin Liu:Investigation,Yonggui Yang:Supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The relevant data and images in the manuscript have obtained the informed consent of the patient or legal guardian. The study was approved by the Institutional Review Board of The Second Affiliated Hospital of Xiamen Medical College. All methods were carried out in accordance with guidelines and regulations of the Declaration of Helsinki. Written informed consent was obtained from patients prior to CT imaging.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, S., Sun, Z., Zeng, Y. et al. Feasibility study of ‘Triple-Low’ technique for coronary artery computed tomography angiography (CCTA). Sci Rep 14, 32110 (2024). https://doi.org/10.1038/s41598-024-83884-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-83884-5