Abstract
Foreign body (FB) ingestion and aspiration are frequent causes of pediatric emergency room visits, with significant morbidity and mortality risks. This cross-sectional study analyzed 1,052 pediatric patients admitted for suspected FB events at a single institution between 2008 and 2015, including 886 cases of suspected ingestion and 166 cases of suspected aspiration. Cluster analysis identified three distinct clusters for both groups, with respiratory symptoms being predominant in clusters with worse outcomes. The respiratory clusters were associated with increased complication rates (13.0% for aspiration, 3.6% for ingestion) and all mortalities (three in aspiration and two in ingestion). In ingestion cases, Respiratory Cluster patients showed increased complications, prolonged hospital stays (mean 55.1 h), and accounted for all mortalities, a relationship not previously reported. Caregiver-reported certainty of event occurrence showed moderate sensitivity (72.5%) and low specificity (45.4%) for aspiration, and higher sensitivity (86.8%) with lower specificity (19.8%) for ingestion. Decision Curve Analysis revealed a net benefit in utilizing caregiver certainty for clinical decision-making. Confirmatory radiographic findings were commonly observed in ingestion cases (84.2%) than in aspiration cases (37.7%), likely due to the higher incidence of metal ingestions compared to mostly organic aspirations. Endoscopic management had high success rates (97.6%), and low mortality, highlighting its central role in FB treatment. These findings underscore the importance of assessing respiratory symptom severity within the broad clinical spectrum of FBs to identify patients at risk of worse clinical outcomes, which helps prioritize resources when necessary. Caregiver-reported information has been shown to be valuable in guiding diagnostic decisions.
Similar content being viewed by others
Introduction
The ingestion or aspiration of foreign bodies (FBs) is a frequent cause of pediatric emergency room visits and poses a substantial risk of morbidity and mortality. In the United States, 83,412 cases were reported in 2022, with 83% involving pediatric patients1. Children aged 6 years or younger are predominantly affected, accounting for 65–85% of cases2,3,4 Complications occur in 9.28% of ingestion cases prior to treatment, with an additional 2.06% arising after treatment5. Predictive factors for complications in esophageal FBs include the patient’s age, location, duration of impaction, composition, and size6. Mortality rates from FB aspiration range from 0.1 to 2.4%, with complications reported in up to 41.35% of cases, posing a significant concern in pediatric healthcare7,8,9. Furthermore, pediatric FB aspiration and ingestion cases result in considerable financial burden, with an average cost of $34,652 per admission, increasing to $116,792 in cases involving mortality10.
Regarding causality, 98% of cases are accidental and often involve common household items11. Caregivers are physically present in up to 88.4% of cases; however, this information is perceived as underutilized, with absent reporting and minimal evidence of its application in clinical workups12. Clinical symptoms are frequently nonspecific and span a wide range of organ systems, leading to high rates of misdiagnosis. For instance, initial misdiagnosis rates for aspiration cases have been reported to reach up to 35.4%13. Clustering techniques allow to identify distinct patterns, uncovering hidden associations and phenotypes in conditions with broad and overlapping symptoms14.
Previous studies on FB ingestion or aspiration have primarily focused on descriptive characterizations. This study aims to identify clinical clusters of suspected FB ingestion or aspiration based on symptoms reported at emergency room admission. It also evaluates the accuracy of caregiver-reported information during the initial interview regarding the FB incident. The analysis utilizes data collected over a six-year period from a single pediatric institution.
Methods
Data source
This cross-sectional study utilized data from an institutional registry of patients who presented to a pediatric institution with a suspected FB event between February 2008 and September 2015. Following institutional guidelines, caregivers were interviewed, and the information provided was documented in clinical records. Data for all patients in the registry was retrospectively collected from clinical records, covering the entire hospital admission until discharge or transfer to another facility.
Eligibility criteria
This study included patients under 18 years of age who presented with suspected FB ingestion or aspiration. Suspected cases were identified based on caregiver-reported events at emergency department admission or clinical features indicative of FB ingestion or aspiration, as assessed by the attending pediatric surgeon. Cases were confirmed through imaging evidence of a FB, findings during endoscopic procedures, extraction via other techniques, or patient expulsion of the FB. Patients with incomplete clinical records or those transferred to other institutions during the index admission were excluded. The study was approved by the institutional ethics committee (approval no. CEI-53-15, dated November 18, 2015). Due to its retrospective design and the removal of all patient-identifying information, this study was classified as posing no risk according to governmental regulations on research, and the requirement for informed consent was waived by the IRB. This research was conducted in accordance with the Declaration of Helsinki.
To calculate the sample size, it was determined from a previous study that 83% of FB incidents occur in pediatric patients1. Based on a 2018 national census, the city at which this study took place had approximately 2,187,000 individuals aged 18 or younger. A minimum sample of 375 patients was required to achieve a 99% confidence level. However, since registry data was utilized, all available patients from the study period were included.
Outcomes
The primary outcome was the presenting clinical symptoms of pediatric patients with suspected FB aspiration or ingestion, categorized by the type of FB incident. The secondary outcome was the accuracy of caregivers’ initial reports at emergency room admission, assessed for their predictive value in confirming FB aspiration or ingestion.
Analysis
A descriptive analysis of sociodemographic and clinical data was performed for cases initially classified as suspected aspiration or suspected ingestion. The Shapiro-Wilk test was used to evaluate the normality of numerical variables, with skewness visually assessed through graphical methods. For variables with a parametric distribution, means and standard deviations (SD) were reported, while medians and interquartile ranges (IQR) were used for non-parametric distributions.
Numerical variables were compared using the Mann-Whitney U test or Student’s t-test, depending on the data distribution. Categorical variables were analyzed using Pearson’s chi-square test or Fisher’s exact test, based on expected frequencies.
The same analysis was conducted for patients with confirmed FB aspiration or ingestion following the diagnostic workup. A p-value of less than 0.05 was considered statistically significant.
Caregiver information accuracy assessment
To assess the accuracy of caregiver-reported information, caregiver certainty regarding FB aspiration or ingestion was compared to confirmed cases identified through diagnostic workup. Sensitivity, specificity, and their respective 95% confidence intervals were calculated. Diagnostic performance was further evaluated using the Area Under the Curve (AUC), and Positive Predictive Value (PPV) and Negative Predictive Value (NPV) were reported with 95% confidence intervals.
Decision curve analysis (DCA)
To evaluate the clinical utility of caregiver certainty in predicting FB aspiration or ingestion in pediatric patients, a DCA was performed separately for FB aspiration and FB ingestion. Net benefit is calculated by balancing true positives against false positives, adjusted for risk odds, across a range of threshold probabilities, and is visually represented through graphs.
Caregiver certainty was modeled as a binary diagnostic test and analyzed as a predictive tool. The analysis evaluated whether incorporating caregiver certainty offered a positive net benefit compared to strategies of treating all or treating none. Although this method does not establish exact probability thresholds for clinical action, it focuses on assessing the overall utility of caregiver certainty in guiding decision-making15,16.
Cluster analysis
Individual variables were initially created for each reported pain location, resulting in a total of 15 clinical symptoms, 7 pain locations for suspected aspiration cases, and 8 for suspected ingestion cases. Dimensionality reduction was performed using Multiple Correspondence Analysis (MCA), which generated factor scores for two dimensions capturing the highest variance. For suspected aspiration cases, these two dimensions explained 69.09% of the total inertia, closely approaching the commonly accepted threshold of 70%17.
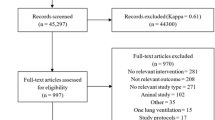
Clustering was performed using Ward’s linkage, with the Calinski-Harabasz index used to identify the optimal number of clusters. K-Means clustering was then applied to validate cluster stability and ensure consistent patient assignments18. The Kappa coefficient was used to compare patient clustering results between the two methods. In the suspected aspiration group, a Kappa coefficient of 0.8643 indicated strong agreement in patient assignments. In contrast, the initial Kappa coefficient for the suspected ingestion group showed only fair agreement.
Variables present in less than 5% of suspected ingestion cases and deemed clinically insignificant were excluded, prompting a revised clustering analysis for suspected ingestion cases. This revised analysis incorporated ten clinical symptoms and the original eight pain locations. The two dimensions explained 74.51% of the total inertia. The resulting Kappa coefficient for comparing the clustering methods was 0.7168, indicating substantial agreement.
Following patient clustering, additional bivariate analyses were performed to compare the characteristics across clusters. All statistical analyses were conducted using Stata Statistical Software: Release 18.0 (StataCorp, College Station, TX, 2023).
Results
Initially, 1,262 admissions met the inclusion criteria; however, medical records for 210 patients were unavailable, resulting in 1,052 patients included in the study. Of these, 886 (84.2%) presented with suspected ingestion, and 166 (15.8%) with suspected aspiration.
The median age of the study population was 3.7 years (IQR 2.1–6.3), with patients in the suspected ingestion group being significantly older (3.9 years [IQR 2.3–6.4] vs. 2.2 years [IQR 1.2–5.8]; p = 0.001). Preschoolers accounted for the majority of cases in both groups, with a significant predominance in suspected ingestion cases (51.5% vs. 34.9%; p = 0.001). Similarly, school-age children were most involved in suspected ingestion cases (23.3% vs. 16.3%; p = 0.047). In contrast, infants (18.7% vs. 4.9%; p = 0.001) and toddlers (23.5% vs. 15.5%; p = 0.011) were mostly seen in suspected aspiration cases. Table 1.
The proportion of patients with comorbidities showed no overall differences between groups; however, a significant increase in respiratory comorbidities was observed in the suspected aspiration group (14.5% vs. 8.0%; p = 0.008). Regarding the state of consciousness at admission, altered levels of consciousness were significantly more frequent in suspected aspiration cases (p = 0.001). Nevertheless, being alert remained the most common state in both groups, seen in 100% of suspected ingestion cases and 92.8% of suspected aspiration cases. A significant increase in confirmatory radiographic findings was observed in suspected ingestion cases (62.5% vs. 15.2%; p = 0.001), while suspected aspiration cases were associated with non-confirmatory findings, such as “suspected foreign body” (26.5% vs. 2.9%; p = 0.001) and “rules out foreign body” (58.3% vs. 34.7%; p = 0.001). Table 1.
Following workup, 70.9% of suspected ingestion cases were confirmed to have a FB, compared to a lower positivity rate of 41.6% for suspected aspiration cases (p = 0.001). Mortality was higher among suspected aspiration cases, with three deaths compared to two in the ingestion group (p = 0.031). In the ingestion group, one death resulted from a procedure-related complication during FB extraction, while the cause of the second death could not be determined. Among suspected aspiration cases, two patients died from sepsis secondary to pneumonia, and one patient succumbed to uncontrollable hemorrhage involving the trachea and right bronchi. Table 1.
Analysis of confirmed cases revealed similar age and sex distributions between groups. Regarding FB composition, organic materials (59.4% vs. 22.6%, p = 0.001) and polymers (15.9% vs. 2.7%, p = 0.001) were significantly more common in aspiration cases, whereas metallic FBs were more frequent in ingestion cases (71.8% vs. 21.7%, p = 0.001). Coins were the most commonly ingested item (55.1%, n = 346), while grains were the most frequently aspirated (20.3%, n = 14). Radiographic findings remained consistent with previous trends, showing a higher proportion of confirmatory results in ingestion cases (84.2% vs. 37.7%, p = 0.001) and a higher prevalence of non-confirmatory findings in aspiration cases (“suspected foreign body” 26.2% vs. 1.6%, p = 0.001; “rules out foreign body” 36.1% vs. 14.2%, p = 0.001). Endoscopic management was successful in 97.6% of cases, with no significant differences in failure rates between groups. Complications were significantly more common in aspiration cases, occurring in 13.0% compared to 1.8% in ingestion cases (p = 0.001). Table 2.
The diagnostic accuracy of caregiver certainty was assessed for both FB aspiration and ingestion. For aspiration, caregiver certainty demonstrated moderate sensitivity (72.5%, 95% CI: 65.7–79.3) but low specificity (45.4%, 95% CI: 37.8–52.9), with a positive predictive value (PPV) of 48.5% (95% CI: 40.9–56.2) and a negative predictive value (NPV) of 69.8% (95% CI: 62.9–76.8). In contrast, caregiver certainty for ingestion showed higher sensitivity (86.8%, 95% CI: 84.6–89.0) but markedly lower specificity (19.8%, 95% CI: 17.2–22.4). The PPV and NPV for ingestion were 72.5% (95% CI: 69.5–75.4) and 38.1% (95% CI: 34.9–41.3), respectively. Table 3.
Two Decision Curve Analyses (DCA) were performed to assess the net benefit of caregiver certainty as a binary predictor for FB aspiration and ingestion, respectively, with the outcomes being confirmed cases of FB aspiration and ingestion. The DCA revealed that caregiver certainty was associated with a positive net benefit across a range of thresholds, compared to the strategies of treating all or treating none. However, due to the binary nature of the predictor, determining precise probability thresholds was limited. Overall, the presence or absence of caregiver certainty offers a net benefit for clinical decision-making when compared to the treat-all or treat-none approach. Figure 1A and 1B.
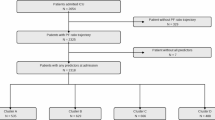
Three distinct clusters were identified among 166 cases of suspected FB aspiration. Sex and comorbidities were similar across groups, but patients in the Pain Cluster were significantly older (p = 0.001) and heavier (p = 0.001). The Respiratory Cluster, consisting of 63 patients, was characterized by higher incidences of wheezing (27.0% vs. 3.6% vs. 10.5%; p = 0.001), stridor (25.4% vs. 3.6% vs. 15.8%; p = 0.001), asphyxia (30.2% vs. 10.7% vs. 15.8%; p = 0.011), lung field hypoventilation (27.0% vs. 4.8% vs. 0%; p = 0.001), ronchi (33.3% vs. 0% vs. 5.3%; p = 0.001), airway obstruction (11.1% vs. 2.4% vs. 0%; p = 0.037), and dyspnea (66.7% vs. 0% vs. 26.3%; p = 0.001). Table 4.
The Pain Cluster, comprising 19 patients, was characterized by universal pain (100% vs. 0% vs. 3.2%; p = 0.001) and dysphagia (31.6% vs. 6.0% vs. 0%; p = 0.001) as the predominant symptoms. The Ambiguous Cluster, consisting of 84 patients, was primarily associated with choking (35.7% vs. 12.7% vs. 10.5%; p = 0.002). Table 4.
The Respiratory Cluster was associated with a longer hospital stay (median: 4 days [IQR: 1–8] vs. 1 day [IQR: 0–3] vs. 1 day [IQR: 0–3]; p = 0.001) and showed non-significant trends toward higher complication (14.3% vs. 4.8% vs. 5.3%; p = 0.105) and mortality rates (4.76% vs. 0% vs. 0%; p = 0.082). The Ambiguous Cluster had the lowest rate of confirmed FB detection after workup (29.8% vs. 47.4% vs. 55.6%; p = 0.006). Table 4.
Among 886 patients with suspected FB ingestion, three symptom clusters were identified: Upper GI Cluster, Respiratory Cluster, and Pain Cluster. Patients in the Pain Cluster were significantly older (median: 5.5 years, IQR: 3.7–7.7) and heavier (median weight: 18 kg, IQR: 14–25) compared to those in the Upper GI (median age: 3.7 years, IQR: 2.4–6.0; median weight: 15 kg, IQR: 12–18.3) and Respiratory Clusters (median age: 2.5 years, IQR: 1.4–4.2; median weight: 12 kg, IQR: 10–16) (p = 0.001 for both). The Pain Cluster also had a higher proportion of females (51.5%, p = 0.047). Table 5.
In the Respiratory Cluster, predominant symptoms included choking (29.1%), dyspnea (48.2%), coughing (33.2%), and hemoptysis (15.9%) (p = 0.001). In contrast, the Pain Cluster was characterized by universal pain (100%) and a high prevalence of dysphagia (48.9%) (p = 0.001). The Upper GI Cluster was notable for increased vomiting (33.7%), dysphagia (35.4%), and sialorrhea (35.9%), although the latter was not statistically significant (p = 0.083). Table 5.
The length of hospital stay was longest in the Respiratory Cluster (mean: 55.1 h, SD: 144.9) compared to the Upper GI (mean: 39.7 h, SD: 99.5) and Pain Clusters (mean: 34.4 h, SD: 95.5) (p = 0.031). Confirmed FB presence was highest in the Upper GI Cluster (78.8%) and lowest in the Pain Cluster (59.6%) (p = 0.001). Patients in the Respiratory Cluster showed significant increases in complications (3.6%, p = 0.008) and mortality (0.9%, p = 0.048). Table 5.
Discussion
This study is the first to use cluster analysis to evaluate the broad spectrum of clinical symptoms observed at emergency room admission for FBs. For suspected aspiration cases, a trend toward increased complications was identified in patients within the Respiratory Cluster. A similar cluster, characterized by predominant respiratory symptoms, was also identified in suspected ingestion cases, with a significant increase in complications observed in this group. All mortalities occurred in patients within Respiratory Clusters, with three cases in suspected aspiration and two in suspected ingestion. This study is also the first to evaluate the accuracy and utility of caregiver-provided information during emergency room admission for the diagnostic workup of suspected FB ingestion and aspiration. Additionally, it is among the largest studies to concurrently analyze aspiration and ingestion cases and the first to report on pediatric FBs in the Colombian population.
The initial interview of both the patient and caregiver plays a crucial role during patient workup. Caregiver certainty demonstrated strong detection of confirmed cases, with sensitivities of 72.5% for aspiration and 86.8% for ingestion. This approach contrasts with previous predictive models for FB aspiration, which predominantly relied on witnessed choking incidents and have shown limited performance19,20. Our findings may contribute to the refinement of such models. Additionally, DCA showed that caregiver certainty was associated with a positive net benefit compared to the strategies of treating all or treating none. Despite its perceived historical underutilization, our findings support a more balanced approach, integrating caregiver insights alongside clinician intuition in clinical decision-making. Ultimately, a comprehensive assessment of these events should include multiple sources of information.
Regarding FB composition, the increased ingestion of metals and aspiration of organics aligns with findings from previous studies. The attraction to coins and other visually appealing objects during the preschool years is often linked to a developmental phase characterized by oral curiosity, a tendency to explore their environment, and the absence of molars necessary for mastication21. Although imaging studies are essential for patient workup, their effectiveness varies based on FB composition. Radiographs are particularly effective for metals, confirming the presence of a FB in 84.2% of confirmed ingestion cases in our study. However, this rate dropped to 37.7% in confirmed aspiration cases, where organic materials were the primary composition of FBs. This low positivity for aspiration aligns with findings from other studies that have reported negative radiographies in two thirds of patients22. Although CT scans offer a higher detection rate of 70–100% for FBs, their routine use in children is discouraged due to potential risks associated with radiation exposure23. A higher-than-expected proportion of patients did not receive radiographs during their evaluation; however, the reasoning behind this was not explored in the study.
In aspiration cases, the predominant symptoms of coughing, choking, and dyspnea observed in our study align with the top three symptoms identified in pooled proportions from meta-analysis24. However, our population showed lower incidences of choking (24.1% vs. 46.8%) and dyspnea (28.3% vs. 34.6%)24. Other respiratory symptoms observed in our study, such as rhonchi, wheezing, and stridor, are consistent with findings from previous research, with these symptoms reported in more than 10% of aspiration cases25,26. Regarding clustering, the Respiratory Cluster accounted for higher incidences of complications, longer hospital stays, and all mortalities within aspiration cases. Patients in this cluster had high incidences of multiple respiratory symptoms but, interestingly, low incidences of choking. This, once again, contrasts with predictive models for foreign body aspiration, which often use witnessed choking as a key predictive factor20. It is also noteworthy that this cluster had the highest percentage of confirmed FB diagnoses after workup.
In ingestion cases, clinical syndromes are characterized by high incidences of vomiting, sialorrhea, dysphagia, cough, abdominal pain, mass sensation, and hematemesis5. In our study, the three most common symptoms were pain, vomiting, and dysphagia. The Respiratory Cluster in ingestion cases exhibited higher rates of coughing (33.2%), dyspnea (48.2%), hemoptysis (15.9%), and choking (29.1%). Membership to the Respiratory Cluster was associated with higher mortality, increased complications, and prolonged length of stay. This suggests that a greater degree of respiratory symptoms at presentation may be predictive of severe disease in ingestion cases. While this finding aligns with widely accepted disease mechanisms, it has not previously been discussed in the context of FB ingestion.
Our study is limited by the disproportionately high number of ingestion cases in the pre-clustering analysis. While this distribution aligns with clinical practice, it results in unbalanced comparison groups. Regarding clustering, although various methods yielded consistent results, the single-center nature of our study limits the generalizability of our findings. Clinical presentations may vary across settings; however, the authors did not identify specific reasons for this variation at this time. The use of retrospective clinical records as a data source may introduce measurement bias, but this was addressed by cross-referencing medical records with additional sources, such as imaging software, to ensure accuracy. Finally, patient crossover between aspiration and ingestion groups from suspected to confirmed FB analysis was not recorded.
Overall, our study highlights the relationship between respiratory symptoms at emergency room admission and severe outcomes, intuitively for aspiration but also, unexpectedly, for ingestion. This is demonstrated by the fact that all mortality cases were associated with Respiratory Clusters, regardless of the type of event, as well as by the higher complication rates observed in these clusters. Assessing the severity of respiratory symptoms may help identify patients at greater risk of adverse outcomes. Our findings also uncovered the value of actively incorporating caregiver information into patient workup. While caregiver-provided information shows low performance in ruling out FBs, it proves effective in detecting cases and provides a net benefit, as observed in DCA, when treatment decisions are guided by caregiver certainty. Finally, the low incidences of mortality, complications, and endoscopic management failure reflect the effectiveness of endoscopic approaches as a cornerstone in the workup and treatment of FB cases. Further studies in diverse populations are needed to validate the relationships identified in our study.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to regulations in Colombia that restrict sharing patient information but are available from the corresponding author on reasonable request.
References
Gummin, D. D. et al. 2022 Annual report of the national poison data system from America’s Poison Centers: 40th annual report. Clin. Toxicol. 61, 717–939 (2023).
Navia-López, L. A. et al. Foreign body ingestion and associated factors in pediatric patients at a tertiary care center. Revista De Gastroenterología De México (English Edition). 87, 20–28 (2022).
Panieri, E., & Bass D. H. The management of ingested foreign bodies in children a review of 663 cases. Eur. J. Emerg. Med. 2, 83–87 (1995).
Boufersaoui, A. et al. Foreign body aspiration in children: Experience from 2624 patients. Int. J. Pediatr. Otorhinolaryngol. 77, 1683–1688 (2013).
Khorana, J. et al. Foreign body ingestion in pediatrics: Distribution, management and complications. Medicina (Kaunas); 55. Epub ahead of print 14 October 2019. https://doi.org/10.3390/medicina55100686
Sung, S. H. et al. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig. Liver Dis. 43, 632–635 (2011).
Kahraman, C. et al. Lung infections due to aspirated foreign bodies: Analysis of 84 cases. Asian Cardiovasc. Thorac. Ann. 7, 305–308 (1999).
Wang, Q. et al. A real-world study of foreign body aspiration in children with 4227 cases in Western China. Sci. Rep. 14, 15251 (2024).
Ding, G. et al. Tracheobronchial foreign body aspiration in children. Medicine 99, e20480 (2020).
Shah, R. K. et al. Management of Foreign bodies obstructing the Airway in Children. Arch. Otolaryngol. Head Neck Surg. 136, 373 (2010).
Chung, S., Forte, V. & Campisi, P. A review of pediatric foreign body ingestion and management. Clin. Pediatr. Emerg. Med. 11, 225–230 (2010).
Chinski, A. et al. Foreign bodies in children: A comparison between Argentina and Europe. Int. J. Pediatr. Otorhinolaryngol. 76, S76–S79 (2012).
Zhu, Y. et al. Diagnostic errors in initial misdiagnosis of foreign body aspiration in children: A retrospective observational study in a tertiary care hospital in China. Front. Pediatr. 9. Epub ahead of print 15 October 2021. https://doi.org/10.3389/fped.2021.694211
Loftus, T. J. et al. Phenotype clustering in health care: A narrative review for clinicians. Front. Artif. Intell. 5. Epub ahead of print 12 August 2022. https://doi.org/10.3389/frai.2022.842306
Piovani, D. et al. Optimizing clinical decision making with decision curve analysis: Insights for clinical investigators. Healthcare 11, 2244 (2023).
Rousson, V. & Zumbrunn, T. Decision curve analysis revisited: Overall net benefit, relationships to ROC curve analysis, and application to case-control studies. BMC Med. Inf. Decis. Mak. 11, 45 (2011).
Higgs, N. T. Practical and innovative uses of correspondence analysis. Stat. 40, 183 (1991).
Tarekegn, A. N., Michalak, K. & Giacobini, M. Cross-validation approach to evaluate clustering algorithms: An experimental study using Multi-label datasets. SN Comput. Sci. 1, 263 (2020).
Pozailov, S. et al. Foreign body aspiration score (FOBAS)—A prospectively validated algorithm for the management and prediction of foreign body aspiration in children. Eur. J. Pediatr. Epub ahead of print 29 November 2023. https://doi.org/10.1007/s00431-023-05347-9
Lee, J. J. W. et al. Clinical prediction models for suspected Pediatric Foreign Body Aspiration. JAMA Otolaryngol. Head Neck Surg. 147, 787 (2021).
Torsello, M. et al. Foreign body aspiration in children: Our pediatric tertiary care experience. Pediatr. Surg. Int. 40, 93 (2024).
Eren, Ş. et al. Foreign body aspiration in children: Experience of 1160 cases. Ann. Trop. Paediatr. 23, 31–37 (2003).
Sugawa, C. Endoscopic management of foreign bodies in the upper gastrointestinal tract: A review. World J. Gastrointest. Endosc. 6, 475 (2014).
Foltran, F. et al. Foreign bodies in the airways: A meta-analysis of published papers. Int. J. Pediatr. Otorhinolaryngol. 76, S12–S19 (2012).
Ulas, A. B., Aydin, Y. & Eroglu, A. Foreign body aspirations in children and adults. Am. J. Surg. 224, 1168–1173 (2022).
Na’ara, S. et al. Foreign body aspiration in infants and older children: A comparative study. Ear Nose Throat J. 99, 47–51 (2020).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SA-R: Data analysis, interpretation of data, writing of manuscript. EDAG: Data acquisition, interpretation of data, writing of manuscript. SCS: Data acquisition, interpretation of data, writing of manuscript. IEG: Study design, data analysis, data interpretation. MMB: Study design, data analysis, data interpretation. FFA: Conception of study, interpretation of data. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alzate-Ricaurte, S., Alzate Gallego, E.D., Correa Salazar, S. et al. Cluster analysis of symptoms and assessment of caregiver reports in pediatric foreign bodies. Sci Rep 15, 213 (2025). https://doi.org/10.1038/s41598-024-84042-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84042-7