Abstract
Numerous clinical studies indicate that reproductive factors and physical performance levels are significant predictors of bone mineral density (BMD) in postmenopausal women. However, research on the relationship between these factors and body composition remains limited, and the mediating role of body composition in the impact of these factors on BMD remains unclear. This cross-sectional study aims to explore the correlation between reproductive factors, physical performance levels, BMD, and body composition in postmenopausal women, and to further investigate the mediating role of body composition in these relationships. This study enrolled 102 postmenopausal women meeting predetermined criteria from the osteoporosis outpatient clinic of Huzhou Central Hospital, China. Data were collected through surveys, assessments of physical performance function, and dual-energy X-ray absorptiometry (DXA) measurements. Correlation analysis and multiple linear regression analysis were used to determine the relationships among factors. Mediation analysis was conducted to explore the mediating role of body composition, followed by logistic regression analysis to investigate risk factors for osteoporosis. Gynoid Lean Muscle Mass (GLM) emerged as an independent predictive factor for BMD of spine, hip, and total body, and a protective factor against osteoporosis. Hand grip and 6-meter gait speed were positively correlated with BMD at these skeletal sites and GLM, also serving as protective factors against osteoporosis. Conversely, menarche age and Time taken for 5 sit-ups exhibited negative correlations with BMD and GLM, concurrently representing risk factors for osteoporosis. GLM mediated the relationship between menarche age, hand grip, and hip BMD. Prolonged reproductive periods and enhanced physical performance appear beneficial in mitigating Lean Mass loss, particularly GLM, in postmenopausal women, thereby protecting BMD and effectively preventing osteoporosis.
Similar content being viewed by others
Introduction
With the exacerbation of global population aging, the incidence of osteoporosis is steadily increasing. The global prevalence of osteoporosis is reported to be 18.3%, with a prevalence of 23.1% among women1. Osteoporosis, a systemic skeletal disorder, poses a significant threat to the health of middle-aged and elderly individuals, characterized by the loss of BMD leading to skeletal fragility. Its severe clinical consequences primarily encompass fragility fractures, particularly occurring in sites such as the spine, hip, and wrist2. Osteoporosis, especially prevalent in older postmenopausal women, increases the risk of fractures that can be associated with significant morbidity and mortality. Postmenopausal bone loss, related to estrogen deficiency, is the primary contributor to osteoporosis. Other important risk factors for postmenopausal osteoporosis include advanced age, genetics, smoking, thinness, and many diseases and drugs that impair bone health3. Hence, the identification of predictive factors for BMD changes in postmenopausal women is of paramount importance for timely osteoporosis prevention and treatment, thereby mitigating the risk of further consequential outcomes such as fractures.
Current clinical research has unveiled the associations between physiological reproductive factors, physical performance levels related to sarcopenia, and body composition with BMD in postmenopausal women4,5,6,7. The relationship between sarcopenia and osteoporosis is particularly prominent in postmenopausal women, with sarcopenia characterized by decreased muscle mass in body composition, decreased physical performance levels including hand grip, and declines in functional movements such as 5 sit-ups and 6-meter walking8. Bone and muscle are closely related endocrine tissues that synthesize and produce various cytokines9. In terms of hormonal changes, alterations in the reproductive status of women lead to fluctuations in endogenous hormone levels, particularly estrogen, thereby impacting bone, muscle, and fat synthesis metabolism, further influencing postmenopausal BMD and body composition10. However, there remains a research gap in the clinical understanding of the precise relationship between physiological reproductive factors, physical performance levels, and body composition in postmenopausal women. Additionally, the specific correlation between body composition and osteoporosis is still a subject of debate.
Therefore, this study aims to delve deeper into the mutual relationship between body composition and BMD in postmenopausal women, focusing on exploring the associations between physiological reproductive factors and physical performance manifestations with body composition and BMD, respectively. Additionally, we aim to further analyze the potential mediating role of body composition in the relationship between physiological reproductive factors, physical performance levels, and BMD in postmenopausal women.
Materials and methods
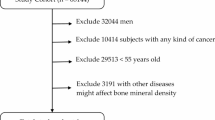
Study population
Between November 2023 and April 2024, this study was conducted among patients attending the osteoporosis outpatient clinic at Huzhou Central Hospital. Inclusion and exclusion criteria were applied as follows: postmenopausal women with a history of normal reproductive periods and no significant medical illnesses. Exclusion criteria encompassed individuals with abnormal ages of menarche or menopause due to medications, diseases, surgeries, or other unidentified reasons; those afflicted with chronic kidney or liver diseases, thyroid disorders, breast diseases, endogenous or exogenous hypercortisolism, or long-term use of steroids affecting bone metabolism, like previously using hormonal contraceptives or using hormone replacement therapy. Ultimately, 102 eligible postmenopausal women were included in the study. The research protocol obtained approval from the Research Ethics Committee of Huzhou Central Hospital (Protocol Number:202303041-01). All methods employed in this study were conducted in strict adherence to the pertinent guidelines and regulations.
Baseline data
The researchers primarily utilized survey questionnaires and scale assessments to gather patient data for the study. Data collection focused on demographic variables including age, menarche age, menopause age, parity, gravidity, as well as assessments of hand grip, time taken for five sit-to-stand repetitions, 6-meter walking speed, and SARC-CalF(it questionnaire assesses 6 components: strength, assistance in walking, rising from a chair, climbing stairs, falls and calf circumference. The standard cut-offs (≥ 11) of SARC-CalF indicate a risk for sarcopenia, while the opposite is not)11 —parameters of particular interest. The final menstrual period (FMP) is the time point of the last spontaneous menstrual cycle, confirmed by at least 12 consecutive months of amenorrhea in the absence of other physiological or pathological causes. Menopause duration refers to the age difference from menopause, calculated as the difference between her current age at the time of data collection and her menopause age. Additionally, information regarding previous history of fractures, comorbidities, medication usage, and surgical history was recorded. Measurements for enrolled patients included lumbar spine BMD (L1-L4), hip BMD (including femoral neck, Wards triangle, and greater trochanter), total body BMD, fat mass, and lean mass (where Android Lean Muscle Mass (ALM) represents the sum of lean masses of the abdomen, Gynoid Lean Muscle Mass (GLM) represents the sum of lean masses of the hip, and appendicular skeletal muscle mass (ASM) represents the sum of lean masses of the four extremities scanned), all obtained using DXA machines(GE Lunar Prodigy Advance) at Huzhou Central Hospital.
Statistic
Both statistical (Kolmogorov–Smirnov test) and graphical methods (normal probability plots) were used to examine normality for each continuous variable. Since the distributions of these variables were normal, participants ’characteristics were described using mean and standard deviation. Categorical variables were described in terms of percentages. Bivariate correlation analysis was conducted employing the Pearson correlation coefficient. Single-factor analysis of variance (ANOVA) was employed for comparing categorical variable groups, with Bonferroni correction employed as a post hoc test for between-group mean comparisons. Subsequently, variables exhibiting significant correlations underwent multiple linear regression analysis, where all baseline variables with p-values < 0.05 from univariate analysis were incorporated into both forward and backward stepwise multiple linear regression. The Bootstrap method was applied to examine whether body composition acted as a mediator between reproductive factors, physical performance with BMD. Logistic regression analysis was performed to categorize study subjects into two groups based on osteoporosis status and identify protective and risk factors for osteoporosis. The data processing and analysis were conducted using SPSS software (version 26), R (4.2.3), and Zstats v0.90 (www.medsta.cn/software), with a significance level set at p = 0.05.
Results
Population characteristics
From November 2023 to May 2024, a total of 102 patients were enrolled in the study at the Huzhou Central Hospital. Table 1 displayed the demographic characteristics of the study participants, all of whom were Asian females of East Asian descent, with mean ages of 62.39, 15.03, and 49.67 years for overall age, menarche age, and menopause age, respectively. The distribution of pregnancies indicated that 11.76%, 29.41%, 32.35%, and 26.47% had been pregnant 1, 2, 3, and 4 or more times, respectively, while 53.92%, 30.39%, and 15.68% had given birth once, twice, and three or more times, respectively. The mean BMI was 22.31 kg/m2. The mean hand grip measured by the researchers was 22.42 kg, the mean 6-meter gait speed was 1.14 m/s, and the time taken for 5 sit-ups was 12.18 s. Among the participants, 56.86% scored below 11 on the SARC-CALF assessment, while 43.14% scored 11 or higher. The mean values for BMD of the spine, hip, and total body measured by DXA were 0.83, 0.77, and 0.91 g/cm2, respectively. The mean values for body composition, including lean mass (LM), android lean mass (ALM), gynoid lean mass (GLM), appendicular skeletal mass (ASM), and fat mass (FM), were 33.92, 2.38, 4.98, 14.46, and 18.66 kg, respectively.
Factors associated with BMD and body composition
Table 2 reported that age, menarche age and menopause duration exhibited a significant negative correlation with BMD of the spine (r = -0.351, p < 0.001; r = -0.490, p < 0.001; r = -0.419, p < 0.001), hip (r = -0.316, p = 0.001; r = -0.345, p = 0.003; r = -0.391, p < 0.001), and total body (r = -0.415, p < 0.001; r = -0.410, p < 0.001; r = -0.474, p < 0.001). Conversely, menopause age exhibited a positive correlation with BMD of the spine (r = 0.269, p = 0.006), hip (r = 0.283, p = 0.006), and total body (r = 0.258, p = 0.009). The hand grip and 6-meter gait speed in physical performance were found to exhibit a positive correlation with BMD of the spine (r = 0.225, p = 0.023; r = 0.261, p = 0.008), hip (r = 0.352, p < 0.001; r = 0. 257, p = 0.009), and total body (r = 0.407, p < 0.001; r = 0.354, p < 0.001), and GLM in body composition (r = 0.418, p < 0.001; r = 0.263, p = 0.008). Conversely, time taken for 5 sit-ups exhibited a negative correlation with BMD of the spine (r = -0.310, p = 0.001), hip (r = -0.287, p = 0.003), and total body (r = -0.339, p < 0.001), and GLM in body composition (r =- 0.213, p = 0.031). The analysis of body composition among LM, ALM, GLM and ASM exhibited a significant positive correlation with BMD of the spine (r = 0.415; r = 0.344; r = 0.344; r = 0.498, all p < 0.001), hip (r = 0.424; r = 0.359; r = 0.359; r = 0.461, p < 0.001), and total body (r = 0.463, p < 0.001; r = 0.411, p < 0.001; r = 0.314, p = 0.001; r = 0.519, p < 0.001). Table 3 showed that significant differences were observed among different parity groups in terms of bone mineral density BMD of the spine, hip, and total body(p = 0.006,p = 0.04 8,p = 0.025). Similarly, variations were noted in BMD and body composition across different categories of SARC-CalF scores (all p < 0.010). Table 4 illustrates the multiple linear regression models depicting the relationship between various factors and BMD. In Model 1 of the relationship between body composition and BMD, gynoid lean mass (GLM) emerged as an independent factor influencing BMD of the spine, hip, and total body (p < 0.001 for all). In Model 2, pertaining to reproductive physiological factors and BMD relationship, both menarche age and menopause age were identified as independent factors influencing BMD of the spine, hip, and total body (p < 0.001 for all, p = 0.028, 0.012, 0.030, respectively). Model 3, focusing on the relationship between physical performance and BMD, revealed hand grip and time taken for 5 sit-ups as independent factors influencing Hip BMD (p = 0.018, p = 0.048, respectively). Menarche age and hand grip emerged as independent factors influencing GLM (p = 0.040; p = 0.002) in the multiple linear regression analysis of each factor with GLM (Table 5).
Factors associated with the osteoporosis
According to the guidelines for the diagnosis of osteoporosis in postmenopausal women, the 102 study subjects were classified into non-osteoporosis and osteoporosis groups12. According to the 2019 Asian Sarcopenia Guidelines, the 102 study subjects were classified into sarcopenia and non-sarcopenia8. Table 6 shows characteristics of patients according to osteoporosis diagnosis. The menarche age in osteoporosis patients was found to be higher compared to non-osteoporosis patients (respectively,15.41 years (± 1.79) vs.14.26 years (± 1.33), p = 0.001). Conversely, the menopause age was lower in osteoporosis patients than non-osteoporosis patients (respectively,49.28 years (± 2.66) vs.50.44 years (± 2.56), p = 0.038). Regarding the body composition, osteoporotic patients had significantly lower LM and GLM than non-osteoporotic patients (respectively, 32.88 kg (± 4.07) vs. 35.99 kg (± 43.76), p < 0.001; 4.80 kg (± 0.59) vs. 5.34 kg (± 0.63), p < 0.001). In terms of physical performance level, patients with osteoporosis had lower hand grip, longer time taken for 5 sit-ups, and slower 6-meter gait speed than patients without osteoporosis (respectively, 21.71 kg (± 4.39) vs. 23.83 kg (± 5.33), p = 0.035);13.00s (± 3.16) vs. 10.54(± 2.32), p < 0.001;1.10 m/s (± 0.26) vs. 1.23 m/s (± 0.31), p = 0.020). Figure 1 illustrates logistic regression analysis with osteoporosis as the dependent variable. It indicates that menarche age ≥ 16 years, menopause duration>10, parity ≥ 3, prolonged time taken for 5 sit-ups, and SARC-CALF score ≥ 11 are risk factors for osteoporosis (OR = 5.32, p = 0.008; OR = 4.15, p = 0.007; OR = 1.39, p < 0.001; OR = 4.60, p = 0.002). Conversely, late menopausal age, increased hand grip, faster 6-meter gait speed, larger LM and GLM are protective factors against osteoporosis (OR = 0.84, p = 0.042; OR = 0.90, p = 0.040; OR = 0.017, p = 0.025; OR = 0.81, p < 0.001; OR = 0.23, p < 0.001). The protective and risk factors for osteoporosis are illustrated in Fig. 2.
Univariate logistic regression analyses of the Patients’ characteristics according to osteoporosis diagnosis. Note: OR (95% CI)” stands for “Odds Ratio (95% Confidence Interval). An OR of 1 implies no association between exposure and outcome. An OR greater than 1 indicates a higher odd of the outcome occurring with the exposure. An OR less than 1 indicates a lower odd of the outcome occurring with the exposure. P = p-value.
Schematic Diagram of the Mediating Role of Gynoid Lean muscle Mass and the Protective and Risk Factors for Osteoporosis. Note: The graphs A and B represented the path diagram of the mediation analysis Gynoid Lean muscle Mass on the relationship between Menarche age and Hip BMD, and Gynoid Lean muscle Mass on the relationship between Hand grip and Hip BMD. Bootstrap type: bias-corrected bootstrap method. **=p < 0.001, *=p < 0.05. Proportion mediated is calculated as the indirect effect divided by the total effect.
Mediation analysis
In Fig. 2, graphs A showed that the total effect was − 0.0247, the direct effect was − 0.0154, and the indirect effect was − 0.0093. The 95% confidence interval for the indirect effect was − 0.2371 to -0.0552, excluding 0, indicating that GLM partially mediates the relationship between menarche age and Hip BMD (proportion mediated for 37.6518%). Graphs B showed that the total effect was 0.0091, the direct effect was 0.0050, and the indirect effect was 0.0041. The 95% confidence interval for the indirect effect was 0.0783 to 0.2782, excluding 0, indicating that GLM partially mediates the relationship between hand grip and hip BMD (proportion mediated for 45.0549%).
Discussions
In this study, we observed a positive correlation between LM, ALM, GLM, ASMM in postmenopausal women and their BMD of the spine, hip, and total body. These variables were also found to exhibit protective effects against osteoporosis. Notably, GLM has emerged as an independent predictor for BMD across all three sites, with menarche age and hand grip strength being recognized as significant correlates of GLM. Conversely, fat mass (FM) displayed a positive correlation solely with BMD at the hip and total body; however, this correlation was not as robust as that observed between LM and BMD. Among reproductive factors, a later age of menarche and more parities are associated with lower BMD in the spine, hip, and total body. Menarche occurring at or after 16 years old along with three or more pregnancies were identified as risk factors for osteoporosis development. While menopausal age exhibited a positive correlation with BMD levels, parity and menopausal age did not demonstrate any significant associations with body composition. Menarche age showed a negative correlation with GLM which partially mediated the relationship between menarche age and hip BMD. Hand grip and 6-meter walking speed, indicative of physical performance level, demonstrated positive correlations with BMD of the spine, hip, and total body, as well as GLM. Conversely, time taken for five sit-to-stand repetitions exhibited a negative correlation with BMD of the spine, hip, and total body, and GLM. The better level of physical performance is associated with a lower risk of osteoporosis. Finally, GLM partially mediates the relationship between hand grip and hip BMD.
Body composition analysis serves as a valuable tool for assessing the nutritional status in health and disease. Bioelectrical impedance analysis (BIA) and dual-energy X-ray absorptiometry (DXA) are widely employed in epidemiological (predominantly BIA) and clinical (predominantly DXA) settings to evaluate body composition13. Total body DXA provides information not only about the BMD of the whole skeleton or the amount of lean tissue (identified as fat-free mass), but also about the amount and distribution of adipose tissue. Some parameters obtained from DXA measurements related to muscle and/or fat mass are used in the assessment of osteosarcopenia14. Human body composition primarily comprises three key components: bone mass, LM, and FM. Numerous clinical studies have demonstrated LM and FM as important predictors of BMD, yet controversy persists. Some studies suggest correlations exist between LM and BMD, while FM may not exhibit the same association15,16, or FM alone serves as a significant predictor of BMD17,18. Conversely, other studies indicate both LM and FM serve as important predictors of BMD6,7,19. In this study, LM exhibited a positive correlation with BMD of the lumbar spine, right hip, and total body, with GLM within LM remaining significant after inclusion in multivariable linear regression. Conversely, the predictive role of FM on BMD was inferior to LM. This may be attributed to LM serving as a surrogate for skeletal muscle mass, exerting a greater influence on bone density compared to FM, as bone mass is predominantly determined by the static mechanical loading of muscle weight and muscle contractions20. Moreover, muscle and bone share common synthetic metabolic pathways, and factors originating from muscles, such as irisin, may directly influence bone metabolism21. The protective effect of LM can be attributed to these mechanical and biochemical interactions between muscle and bone, thereby reducing the decline in BMD in postmenopausal women and more effectively preventing osteoporosis.
Previous studies have highlighted those physiological reproductive factors in postmenopausal women, such as menarche age, menopause age, and parity, are pivotal determinants of BMD. Many studies have confirmed that delayed menarche age, early menopause age, and prolonged menopausal years are associated with a significant decline in BMD, thereby correlating with the prevalence of osteoporosis4,22. Additionally, parity exhibits a significant negative correlation with BMD5. Consistent with these findings, our study revealed negative associations between age at menarche and BMD of the lumbar spine, hip, and total body, with age at menarche ≥ 16 years identified as a risk factor for osteoporosis. Conversely, menopause age exhibited a positive correlation with BMD, with BMD declining with increasing menopausal years, indicating a higher risk of developing osteoporosis with prolonged menopausal duration. Postmenopausal women with higher parity demonstrated a pronounced decrease in BMD. Delayed age at menarche and early menopause age are considered risk factors for osteoporosis in postmenopausal women, possibly due to the shorter exposure to estrogen in these women. Estrogen, a key factor in female bone formation and growth. Estrogen binds with estrogen receptor to promote the expression of osteoprotegerin (OPG), and to suppress the action of nuclear factor-κβ ligand (RANKL), thus inhibiting osteoclast formation and bone resorptive activity. It can also activate Wnt/β-catenin signaling to increase osteogenesis, and upregulate BMP signaling to promote mesenchymal stem cell differentiation from pre-osteoblasts to osteoblasts23. Besides the direct negative effects of estrogen-deficiency on bone, indirect effects of altered immune status in postmenopausal women might contribute to ongoing bone destruction, as postmenopausal women often display a chronic low-grade inflammatory phenotype with altered cytokine expression and immune cell profile24. We concurrently observed a negative correlation between menarche age and LM, particularly with GLM, whereas other physiological reproductive factors were not associated with body composition. Mediation analysis indicated that GLM partially mediated the relationship between menarche age and hip BMD. This may primarily be attributed to estrogen exerting beneficial effects on muscle synthesis, attenuating muscle damage, and enhancing post-injury repair through various mechanisms, including preventive effects on the number and function of muscle satellite cells, membrane stability post-injury, and potential antioxidant effects following injury, exercise, and/or mitochondrial stress10. Postmenopausal women with an earlier menarche age experience estrogen effects earlier, resulting in a longer duration of action in LM synthesis and protection. Although the correlation between menopause age and LM was not significant, there was an overall increasing trend, indicating that women with a later menopause age had more LM, reflecting the protective effect of estrogen on LM. The more pronounced effect of menarche age compared to menopause age on LM may be due to women with an earlier menarche age entering the pubertal growth phase earlier. During this period, rapid growth and development occur, with estrogen having a more significant effect on LM in pubescent females, particularly in the growth of GLM. This may also be one of the reasons why adult women to have a pear-shaped body structure. Therefore, the less pronounced decline in BMD in postmenopausal women with an earlier menarche age may be partially attributed to the protective effect of estrogen on GLM, which is considered one of the protective factors for BMD.
Previous studies have explored the relationship between clinical sarcopenia and osteoporosis in postmenopausal women, finding a significant association between reduced physical performance associated with sarcopenia and decreased BMD, closely linked to osteoporosis6,25,26,27,28. Our study results align with these findings. We observed a positive correlation between hand grip, 6-meter walking speed, and BMD of the spine, hip, and total body, as well as GLM, while the time taken for five sit-to-stand repetitions exhibited a negative correlation with BMD at these sites and GLM Additionally, patients with SARC-CalF scores of 11 or higher exhibited lower BMD and LM compared to those with scores below 11. Our research further underscores the association between osteoporosis and calf circumference, gait speed, and hand grip as recognized parameters for assessing musculoskeletal health28. Decreased level of physical performance and SARC-CalF ≥ 11 pose significant risk factors for osteoporosis. Additionally, through mediation analysis, we found that GLM in body composition partially mediated the relationship between hand grip and BMD. Hand grip reflects the direct force exerted on both muscles and bones through physical performance, possibly reflecting the mechanical loading of bones by muscle contraction and movement. Bones and muscles interact with each other through mechanical means (the mechanistic hypothesis), as well as through paracrine and endocrine mechanisms to maintain the internal stability of muscles and bones. At the same time, these bone- and muscle-derived cytokines, including interleukin-6, irisin, β-aminoisobutyric acid, osteocalcin, fibroblast growth factor-23, and sclerostin, regulate both local and distant tissues, and they mediate the crosstalk between bone and skeletal muscle9,29. Furthermore, this can be attributed to the shared genetic, lifestyle, and hormonal determinants of bone and muscle. Increasing physical performance appears to mitigate significant losses in LM from pre-menopause through perimenopause to post-menopause, offering a beneficial strategy to reduce the impact of ovarian aging on muscle mass10. Elevated levels of physical performance in postmenopausal women can help maintain higher LM, particularly GLM associated with female characteristics, further preventing declines in BMD. Increasing physical performance and exercise contribute to bone formation, preventing declines in BMD in postmenopausal women and alleviating osteoporosis7,27. The possible mechanisms are that exercise affects apoptosis and autophagy through the release of exercise-stimulated myohormone and the secretion of anti-inflammatory cytokines via mechanical force30. In addition, exercise may also have an impact on the epigenetic processes involved in bone metabolism. Mechanical stimulation promotes bone marrow mesenchymal stem cells (BMSCs) to osteogenic differentiation by altering the expression of non-coding RNAs31. However, the forms, methods, and effects of exercise trials aimed at improving postmenopausal women’s bone health vary. Further research is needed to determine which types of physical performance and exercise and how to conduct better physical performance and exercise to protect postmenopausal women’s BMD and prevent osteoporosis.
The strength of this study lies in the analysis of the relationship between factors influencing osteoporosis and body composition, a topic that has been rarely explored in clinical practice. Additionally, it examines the mediating role of body composition in the relationship between these factors and osteoporosis. Furthermore, the study population consisted of postmenopausal women who were non-smokers, non-drinkers, and had few medical conditions or medications known to impact bone health. However, there are limitations to our study including a relatively small sample size and that the characteristics of the study population only represent those of East Asian postmenopausal women in this region, thus limiting its universal applicability for other national and regional populations.
Conclusions
Later menarche age, earlier onset of menopause, higher parity, decreased physical performance, and decreased LM are associated with a more pronounced decline in BMD of the spine, hip, and total body in postmenopausal women, closely linked to an increased incidence of osteoporosis. Particularly, menarche age ≥ 16 years, parity ≥ 3, decreased physical performance, and reduced GLM are risk factors for osteoporosis. Postmenopausal women with these risk factors should enhance awareness of osteoporosis prevention and treatment. Furthermore, menarche age and physical performance are closely associated with GLM. Prolonged reproductive period and increased physical performance contribute to increased muscle mass, especially GLM, further aiding in the protection of BMD in postmenopausal women, thus better preventing the occurrence of osteoporosis.
Data availability
The original data presented in the study is included in the article and supplementary material. Further inquiries can be directed to the corresponding authors.
References
Salari, N. et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 16 (1), 609 (2021).
Anam, A. K. & Insogna, K. Update on osteoporosis screening and management. Med. Clin. North. Am. 105 (6), 1117–1134 (2021).
Management of osteoporosis in postmenopausal women: the 2021 position statement of the North American menopause society. Menopause 28 (9), 973–997 (2021).
He, Y. et al. Menarche age exceed 17 years and menopausal age smaller than 48 years May affect prevalence of osteoporosis for Chinese women. Arch. Osteoporos. 16 (1), 123 (2021).
Yang, Y., Wang, S. & Cong, H. Association between parity and bone mineral density in postmenopausal women. BMC Womens Health. 22 (1), 87 (2022).
He, H. et al. Relationship of sarcopenia and body composition with osteoporosis. Osteoporos. Int. 27 (2), 473–482 (2016).
Flores, L. E. et al. Examining effects of habitual physical activity and body composition on bone structure in early post-menopausal women: a pQCT analysis. Osteoporos. Int. 33 (2), 425–433 (2022).
Chen, L. K. et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21 (3), 300–307 (2020). e2.
Lu, L. & Tian, L. Postmenopausal osteoporosis coexisting with sarcopenia: the role and mechanisms of Estrogen. J. Endocrinol. 259(1) (2023).
Pellegrino, A., Tiidus, P. M. & Vandenboom, R. Mechanisms of Estrogen influence on skeletal muscle: mass, regeneration, and mitochondrial function. Sports Med. 52 (12), 2853–2869 (2022).
Lim, W. S. et al. Letter to the editor: case for validated instead of standard cut-offs for SARC-CalF. J. Nutr. Health Aging. 23 (4), 393–395 (2019).
Camacho, P. M. et al. Endocr. Pract., 26(Suppl 1): 1–46. (2020).
Marra, M. et al. Assessment of body composition in health and disease using bioelectrical impedance analysis (BIA) and dual energy X-Ray absorptiometry (DXA): A critical overview. Contrast Media Mol. Imaging. 2019, 3548284 (2019).
Gonera-Furman, A., Bolanowski, M. & Jędrzejuk, D. Osteosarcopenia-The role of Dual-Energy X-ray absorptiometry (DXA) in diagnostics. J. Clin. Med. 11(9). (2022).
Lima, D. P. et al. Osteoporosis in Parkinson’s disease and the role of lean body mass: a cross-sectional study in a Brazilian tertiary center. Front. Endocrinol. (Lausanne). 15, 1326212 (2024).
Ilesanmi-Oyelere, B. L. et al. Lean body mass in the prediction of bone mineral density in postmenopausal women. Biores Open. Access. 7 (1), 150–158 (2018).
Fan, J. et al. Associations of fat mass and fat distribution with bone mineral density in Non-Obese postmenopausal Chinese women over 60 years old. Front. Endocrinol. (Lausanne). 13, 829867 (2022).
Mathieu, M. et al. Association between bone mineral density and fat mass independent of lean mass and physical activity in women aged 75 or older. Nutrients 13(6). (2021).
Xiang, J. et al. Lean mass and fat mass as mediators of the relationship between physical activity and bone mineral density in postmenopausal women. J. Womens Health (Larchmt). 26 (5), 461–466 (2017).
Taaffe, D. R. et al. Race and sex effects on the association between muscle strength, soft tissue, and bone mineral density in healthy elders: the health, aging, and body composition study. J. Bone Min. Res. 16 (7), 1343–1352 (2001).
Colaianni, G. et al. Irisin and bone: From preclinical studies to the evaluation of its Circulating levels in different populations of human subjects. Cells 8(5). (2019).
Yang, Y., Wang, S. & Cong, H. Association between age at menarche and bone mineral density in postmenopausal women. J. Orthop. Surg. Res. 18 (1), 51 (2023).
Cheng, C. H., Chen, L. R. & Chen, K. H. Osteoporosis due to hormone imbalance: an overview of the effects of Estrogen deficiency and glucocorticoid overuse on bone turnover. Int. J. Mol. Sci. 23(3). (2022).
Fischer, V. & Haffner-Luntzer, M. Interaction between bone and immune cells: implications for postmenopausal osteoporosis. Semin Cell. Dev. Biol. 123, 14–21 (2022).
Sjoblom, S. et al. Relationship between postmenopausal osteoporosis and the components of clinical sarcopenia. Maturitas 75 (2), 175–180 (2013).
Hamad, B., Basaran, S. & Coskun Benlidayi, I. Osteosarcopenia among postmenopausal women and handgrip strength as a practical method for predicting the risk. Aging Clin. Exp. Res. 32 (10), 1923–1930 (2020).
Watson, S. L. et al. High-Intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial. J. Bone Min. Res. 33 (2), 211–220 (2018).
Lin, Y. H. & Teng, M. M. H. Comparing self-assessment, functional, and anthropometric techniques in predicting osteoporosis. Arch. Osteoporos. 15 (1), 132 (2020).
Drey, M. et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin. Exp. Res. 28 (5), 895–899 (2016).
Zhang, L. et al. Exercise for osteoporosis: A literature review of pathology and mechanism. Front. Immunol. 13, 1005665 (2022).
Liu, C. et al. The mechanosensitive LncRNA Neat1 promotes osteoblast function through paraspeckle-dependent Smurf1 mRNA retention. Bone Res. 10 (1), 18 (2022).
Acknowledgements
We would like to thank the participants for participating in our study, as well as the professional physicians at Huzhou Central Hospital who performed the DXA measurement of body composition.
Funding
This study was funded by the Zhejiang Province Public Welfare Technology Application Research Project (Grant No. LGD21H010001), and Huzhou Municipal Science and Technology Bureau Public Welfare Application Research Project (Grant No. 2023GYB65).
Author information
Authors and Affiliations
Contributions
X.L. and Y.W. contributed to conception and design of the work. C.Q., D.Z., Y.W. contributed to acquisition of data; X.T., J.Z. and Y.Z. coordinated data collection and manuscript review. C.Q. and M.X. analyses of data. X.L. and Y.W. contributed to interpretation of results. M.X. wrote all versions of the manuscript. The final version of the manuscript was edited, reviewed, and approved by all authors, who also agreed to take responsibility for all aspects of this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, M., Qiu, C., Zhang, D. et al. Gynoid lean muscle mass as mediator between menarche age, hand grip and bone mineral density in postmenopausal women. Sci Rep 15, 15574 (2025). https://doi.org/10.1038/s41598-025-00251-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00251-8