Abstract
Neonatal-short peripheral intravenous catheters (n-SPCs) and neonatal-long peripheral intravenous catheters (n-LPCs) are widely used for short-term vascular access in neonates. A retrospective single-centred cohort study was conducted in the neonatal intensive care unit between 2019 and 2022 to compare the 2 types of catheters. A total of 34,464 catheter insertions were analysed (32,885 n-SPCs, 1,579 n-LPCs). n-LPCs had longer dwell time (48:27 ± 39:08 h versus 34:01 ± 33:31 h, p < 0.001). Accidental removals were lower in n-LPCs (0.3% versus 2.6%, p < 0.001). n-LPCs had higher rates of phlebitis (16.1% versus 6.6%, p < 0.001) and peripheral intravenous infiltration or extravasation (PIVIE) rate (40.0% versus 29.9%). Severe PIVIE (≥ 30% severity) was higher in n-LPCs (8.5% versus 2.8%, p < 0.001). n-LPCs offer a more stable and effective option for peripheral vascular access in neonates. Their use should be balanced with strategies to reduce the risk of phlebitis and severe PIVIE.
Similar content being viewed by others
Introduction
Vascular access is a cornerstone of neonatal intensive care for enabling effective therapy and treatment. However, obtaining, securing and maintaining reliable intravenous access in this population remains a challenge due to the fragility of neonatal veins, the need for long-term therapy, and the potential for serious complications such as infiltration, extravasation, phlebitis, and catheter-associated infections. Interpreting the evidence base around neonatal vascular access is complicated by differing definitions and variations in terminology for neonatal vascular access devices. The terms used in this study align with recent international position statements concerning the adoption of standardised terminology for neonatal vascular access devices1,2. The use of this nomenclature aims to promote clarity and consistency in discussions of neonatal vascular access, allowing for precise comparisons and interpretations across clinical and research settings1.
Neonatal-short peripheral Catheters (n-SPCs) are widely used in neonatal care for their ease of insertion and cost-effectiveness, but high failure rates and limited dwell times make them suboptimal for neonates requiring prolonged therapy or vesicant solutions3,4,5,6,7. One of the main limitations of n-SPCs is their high risk of early failure, typically due to dislodgement, occlusion, and local complications such as peripheral intravenous infiltration or extravasation (PIVIE) and phlebitis5,6,7,8,9. Studies indicate that up to 70% of n-SPCs fail before the completion of therapy, leading to repeated insertion attempts, increased pain, increased risk of infections and other morbidities3,5,7,9. As a result, there is a growing interest in alternative catheter types, such as neonatal-Long Peripheral Catheters (n-LPCs). These devices are designed to support longer dwell times and improved stability in neonatal vascular access10,11,12.
n-LPCs, also referred to as midline catheters in some literature, were introduced to neonatal care in the early nineteen-nineties to bridge the gap between n-SPCs and central venous catheters10,11,13,14,15. n-LPCs theoretically allow for dwell times of up to 14 days16. Design features incorporating longer catheter lengths enabling placement into the deeper peripheral vasculature combined with smaller catheter diameter can reduce catheter-to-vein ratios which could help to minimise mechanical irritation and improve stability17,18. These attributes are particularly beneficial for very low birth weight (VLBW) and extremely premature infants, who often have limited venous access options6,7,19,20.
Several studies have demonstrated that n-LPCs often exhibit a safety profile comparable to, or potentially better than, n-SPCs in specific neonatal populations21,22,23. For example, Colacchio et al.21 reported a 50% reduction in catheter-related complications when using n-LPCs, including a lower incidence of phlebitis and extravasation. However, these findings are primarily derived from single-site studies with small sample sizes, and the lack of robust multicentred evidence limits their generalisability.
Despite the potential advantages of n-LPCs concerns about their use in neonates persist, particularly regarding the risk of thrombosis and their unsuitability for administering hypertonic solutions21,23,24 which limits their applicability amongst neonatal patients. Additionally, the insertion of n-LPCs requires a different technique to n-SPCs and this might limit their more widespread adoption11,13,24. Given the scarcity of evidence comparing the performance of n-SPCs and n-LPCs in neonates to guide practice, this study aims to evaluate key catheter performance criteria and help fill the current knowledge gap concerning these devices.
Methods
Study design and setting
A retrospective cohort study design was used. The study was conducted at the Neonatal Intensive Care Unit (NICU) of the Women’s Wellness and Research Center (WWRC) at Hamad Medical Corporation (HMC) in Doha, Qatar. WWRC is a tertiary-level academic health system (AHS) facility with an expanding NICU that reached 128 NICU level-III beds. The hospital accommodates more than 18,000, predominantly high-risk deliveries per year. The study protocol (MRC-01-23-012) was approved by the local institution review body (IRB) of the Medical Research Center (MRC) at Hamad Medical Corporation (HMC). They determined that the study was a ‘chart review’ and as the data source was anonymized; they deemed that participant consent was not feasible nor required. Participants and their parents were not involved in the design, conduct or reporting of this study.
Study population
The study population included all term and preterm neonates admitted to the NICU during the study period who required peripheral intravenous therapy using either n-SPCs or n-LPCs. While most catheters were placed within the first week of life, some neonates required IV access beyond this period due to prolonged therapy needs or difficult venous access. Exclusion criteria were neonates experiencing failure to insert an n-SPS or n-LPC, those who received intravenous therapy through other vascular access devices and routes, neonates with a pre-existing skin condition at the insertion site or data was incomplete.
Outcomes measured
The primary outcome measure was catheter dwell time, defined as the duration (in hours) that the catheter remained functional from the time of successful insertion to the time of removal. Secondary outcomes included the incidence and severity of catheter-related complications such as accidental removal, phlebitis, occlusion, PIVIE, and catheter dislodgement. Additional variables assessed included the number of attempts required for successful insertion and the site-specific complications related to catheterisation.
Data collection
Anonymised data relevant to the aims and objectives of the study was collected over four years (1st January 2019 to 31st December 2022) using electronic health records. Information retrieved included: patient demographics (e.g., gestational age, birth weight, and sex), catheter characteristics (e.g., site and side of insertion, catheter type, insertion attempts, and specific catheter dimensions such as 1 Fr and 2 Fr for n-LPCs, along with the known catheter length), clinical outcomes (e.g., catheter dwell time, complication rates, and reasons for catheter removal). All relevant clinical and procedural data, including catheter insertion details, complications, and outcomes, were systematically recorded in electronic health records as part of routine nursing and medical documentation in the NICU, ensuring accuracy despite the retrospective nature of the study.
Procedure
All vascular access procedures and data collection were managed by the neonatal vascular access team (NeoVAT). This team comprises a dedicated group of nurses and doctors and is divided into two interrelated functional groups. A nurse-led team is responsible for peripheral access, including n-SPC and n-LPCs, and a mixed professional team is responsible for managing central venous access.
During device selection and placement, the team adhered to a structured decision-making process, guided by a locally developed flow diagram and the ‘5 Rights mnemonic for Venous Access’6,25. These principles set out to ensure the Right device, in the Right vein, with the Right therapy, for the Right duration, and the Right patient. The Modified Seldinger Technique was used to insert the Premicath® n-LPC while the Seldinger Technique was used to insert the Leaderflex® n-LPC26.
Specific factors influencing venous access device choice included the anticipated duration of therapy, fluid characteristics (e.g., pH and osmolarity), and patient characteristics (such as body weight, and a history of difficult venous access). The NeoVAT team’s selection process and device management were tailored to local needs, considering product compatibility, hospital purchasing guidelines, simulation-based training attendance27, clinical consensus, and vein selection supported by near-infrared (NIR) visualisation technology. From March 2020 onwards, octyl-butyl-cyanoacrylate adhesive was incorporated into the vascular access protocol as part of catheter securement for both SPCs and LPCs12. This adhesive was applied at the insertion site immediately following catheter placement to enhance stabilization and reduce the risk of dislodgement or complications such as infiltration and phlebitis. All vascular access procedures were conducted in line with current international standards and local hospital protocols2,24.
Assessment of PIVIE severity
PIVIE severity was assessed using the Cincinnati Pediatric Intravenous Extravasation Assessment System (IEGS) (available from: https://www.cincinnatichildrens.org/service/v/vascular-access/hcp). This tool assigns a percentage score ranging from 1 to 100%, primarily based on the volume of swelling in relation to the patient’s arm length. Swelling is measured as the longest dimension, and this value is compared to the arm length to estimate the extent of the extravasation. The type of extravasated medication is also incorporated into the score, with medications categorised as high-risk (red-coded), moderate-risk (yellow-coded), or low-risk (green-coded). This scale provides a precise and objective quantification of extravasation severity, helping guide clinical decisions regarding the management and treatment of PIVIE events.
Statistical analysis
Descriptive statistics were used to summarise the baseline characteristics and distribution of patient data. Continuous variables were presented as means with standard deviations (SD) and compared using independent t-tests, while categorical variables were represented as frequencies and percentages and analysed using chi-square tests. The primary focus was on comparing the incidence of catheter-associated complications between n-SPCs and n-LPCs.
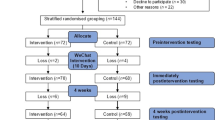
Kaplan-Meier survival analysis was employed to evaluate time-to-event outcomes, in which events were any reason for premature removal of the catheter. All analyses were performed using statistical software packages, such as SPSS 24.0 (SPSS Inc., Chicago, IL), with a p-value of < 0.05 considered statistically significant.
Ethical considerations
The study design and procedures were reviewed and approved by the Institutional Review Board (IRB) of Hamad Medical Corporation (HMC), Doha, Qatar (Protocol Number: MRC-01-23-012). All study procedures were conducted following relevant guidelines and regulations. Due to the retrospective nature of the study and the use of de-identified data, the IRB waived the requirement for informed consent. All patient data were anonymised, and strict confidentiality measures were implemented throughout the research process.
Patient and public involvement statement
Neither study participants, nor their parents were directly involved in the design, conduct or reporting of this study.
Results
A total of 34,464 catheters were reported on during the study period, with 32,885 categorised as n-SPCs and 1,579 as n-LPCs.
Participant demographics
The baseline demographic characteristics were comparable between the groups and are detailed in Table 1. The sex distribution was similar between n-SPC and n-LPC groups, with a slight male predominance in both groups (57.3% and 58.1%, respectively). The mean gestational age and birth weights were comparable across both groups. The mean current weight at catheter insertion was 2,424 ± 920 g for n-SPCs and 2,359 ± 857 g for n-LPCs. The age at catheter insertion was slightly lower in the n-LPC group (7.5 ± 15.0 days) compared to the n-SPC group (9.0 ± 19.0 days).
Catheter insertion characteristics
Table 2 shows the catheter insertion data for n-SPCs and n-LPCs. The average number of insertion attempts was similar between groups (1.33 ± 0.65 for n-SPC vs. 1.31 ± 0.64 for n-LPC, p = 0.24). The distribution of insertion sites varied significantly between the two groups (p < 0.001). The hand was the predominant insertion site for n-SPCs (86.7%), whereas n-LPCs were primarily inserted in the foot (61.2%). Other sites such as the lower arm and ankle were more frequently used for n-LPCs compared to n-SPCs (p < 0.001). The side of insertion was balanced between the groups, with both n-SPCs (52.3%) and n-LPCs (57.3%) being more frequently inserted on the left side.
General catheter removal characteristics
Table 3 details the reasons for catheter removal. In the n-SPC group, the primary reason for removal was therapy completion, accounting for 42.1%, whereas in the n-LPC group, PIVIE was the leading cause, accounting for 40.0% of removals. Accidental removal was significantly higher in the n-SPC group (2.6%) compared to the n-LPC group (0.3%, p < 0.001). Phlebitis was more common in the n-LPC group (16.1%) compared to the n-SPC group (6.6%).
Occlusion rates were comparable between groups (4.3% in n-SPC vs. 4.1% in n-LPC). Discoloration was reported in 0.6% of n-SPCs and 0.7% of n-LPCs. PIVIE occurred significantly more frequently in the n-LPC group (40.0%) compared to the n-SPC group (29.9%) (P < 0.001).
Specified catheter removal characteristics
Table 4 provides more detailed data regarding the reasons for the removal of n-LPCs, distinguishing between 2 Fr Leaderflex® and 1 Fr Premicath® catheters. In the 2 Fr Leaderflex® group, PIVIE accounted for 38.4% of removals, while in the 1 Fr Premicath® group, it accounted for 40.8%. Therapy completion was the second most common reason for removal in both groups (21.7% for 2 Fr Leaderflex® and 34.9% for 1 Fr PremiCath®). Accidental removal and discolouration were relatively uncommon in both groups, occurring in less than 1% of cases. Phlebitis was more frequent in the 2 Fr Leaderflex® group (19.9%) compared to the 1 Fr PremiCath® group (14.4%).
Table 4 also shows that dwell time was significantly longer for 1 Fr PremiCath® catheters (50:03 ± 39:37 h) compared to 2 Fr Leaderflex® catheters (44:55 ± 37:50 h, p < 0.001).
PIVIE severity
Table 5 shows the severity of PIVIEs for each group. The majority of PIVIEs in both groups were graded minor, with scores < 7 (45.6% in n-SPC vs. 44.9% in n-LPC). Severe PIVIEs (≥ 30) were significantly more common in the n-LPC group (8.5%) compared to the n-SPC group (2.8%, p < 0.001). PIVIE scores between 7 and 15 were more frequently observed in the n-SPC group (25.8%) compared to the n-LPC group (17.6%). Table 6 shows the specified Distribution of PIVIE for n-LPC.
Complication analysis and catheter performance
Regression analysis revealed that the use of octyl-butyl cyanoacrylate glue significantly increased dwell time for n-SPCs by 0.30 h (18 min) on average (95% CI: 0.11–0.49; p = 0.002). However, no significant difference in dwell time was observed for n-LPC 1 Fr catheters, while glue usage was associated with a potential reduction in dwell time for n-LPC 2 Fr catheters (-1.33 h; 95% CI: -2.80 to 0.15; p = 0.078).
The Kaplan-Meier survival analysis indicated that n-LPCs had a significantly longer median dwell time compared to n-SPCs (48:27 ± 39:08 h vs. 34:01 ± 33:31 h, p < 0.001). Multivariable Cox regression analysis identified n-LPCs as having a lower risk of accidental removal (OR 0.22, 95% CI 0.14–0.35) and a reduced likelihood of occlusion (OR 0.48, 95% CI 0.34–0.69) compared to n-SPCs. However, the n-LPC group showed a higher risk of phlebitis (OR 0.67, 95% CI 0.49–0.91). Overall, considering all complications, complication rates favoured n-LPCs, suggesting that they may be a safer option for long-term vascular access. Kaplan-Meier catheter dwell rates (in hours) for patients with either a short or long peripheral catheter inserted. An ‘event’ in the curve represents every unplanned and premature removal of the catheter. Planned removal or a catheter that was removed without complications (e.g., due to ‘therapy ended’) was considered a censoring event (Fig. 1).
Discussion
This study provides a comprehensive comparison of n-SPC and n-LPC performance in a real-world neonatal setting, focusing on key clinical outcomes such as dwell time, complication rates, and PIVIE (occurrence and severity). Our findings indicate that n-LPCs offer several advantages over n-SPCs, including the potential for significantly longer dwell times and a reduced overall number of complications. These findings confirm those reported by earlier studies16,21,23 and indicate that n-LPCs could provide a stable and reliable option for neonates requiring prolonged intravenous therapy. This could reduce the need for repeated cannulation attempts and improve patient care experience and well-being. The lower rate of accidental removal in the n-LPC group further supports the use of n-LPCs, especially in clinical scenarios where maintaining vascular access is challenging. Accidental dislodgement, a common complication in neonates due to active movements and fragile veins23, can lead to repeated trauma from frequent reinsertions. When compared the 1 Fr n-LPC showed superior performance in maintaining vascular access compared to larger-size n-LPCs (e.g., 2 Fr) and n-SPCs. However, the increased incidence of phlebitis and severity of PIVIE when it occurs when using larger diameter n-LPCs reported in this study is potentially problematic and requires further consideration.
Longer dwell times and larger catheter diameters are known to be risk factors for phlebitis in all patient groups3,5,7,8,10. This situation is possibly due to an increased opportunity for infection or mechanical irritation of blood vessel walls. Future studies should seek to include data that further differentiate the types of phlebitis to better aid the evaluation of preventative strategies such as improved catheter securement and matching of catheter and vein size.
The use of octyl-butyl cyanoacrylate glue improved securement for n-SPCs, potentially reducing catheter movement and associated complications like phlebitis12,28,29. For n-LPC 2 Fr, the potential reduction in dwell time may be attributed to the larger catheter diameter, which could increase vein wall stress and complications, rather than the effect of glue. The 2 Fr catheter has an external diameter of 0.67 mm, and the 1 Fr catheter, has 0.33 mm. These differences might be clinically important in neonatal care where vein diameters are extremely small. The smaller 1 Fr catheter allows for a lower catheter-to-vein ratio, potentially reducing risks of phlebitis, thrombosis, and infiltration. Conversely, the larger 2 Fr catheter may increase these risks in very small veins where the catheter-to-vein ratio nears or exceeds recommended limits. Speculatively, it might be that the selection of 2 Fr n-LPCs was inappropriate for the actual blood vessel size, adversely affecting catheter-to-vein ratios. Systematic pre-insertion assessment of blood vessel diameter combined with real-time ultrasound-guided insertion would enable a better match between catheter and blood vessel diameters and potentially reduce the risk of mechanical phlebitis30,31,32.
In this study n-LPCs were associated with lower rates of extravasation and occlusion compared to n-SPCs, aligning with reports from previous studies9,14. The reduced incidence of occlusion in n-LPCs may be attributed to their longer catheter length, which minimises the risk of catheter tip malposition and venous wall contact, a common factor in occlusion in n-SPCs4. The severity of PIVIE, when it occurred was significantly higher in the n-LPC group. However, further analysis of the two sizes of n-LPCs used (1 Fr and 2 Fr) revealed that 2 Fr n-LPCs were associated with more severe PIVIE events compared to 1 Fr n-LPCs. Despite the prior research has suggested that the longer length and deeper placement of n-LPCs may reduce the risk of PIVIE10,33, our findings indicate a more complex situation. 2 Fr n-LPCs present a higher risk of severe complications. This situation might be due to many factors such as patient selection criteria or vessel selection based on supposition rather than empirical data about the suitability of larger catheters or differences in clinical infusion management.
Delays in recognising the occurrence of PIVIE with n-LPCs due to the deeper location of the catheter tip and current observational tools focusing on the superficial vessels typically used for n-SPCs might account for some of the reported differences between the two types of catheter. Incorporating real-time continuous PIVIE detection technology could be beneficial in reducing the time to detection and subsequently the severity of this complication34,35. Currently the only device (the ivWatch ®) in routine neonatal clinical has only been tested with n-SPCs34,35,36. The ivWatch® or similar technology’s potential to be used for monitoring n-LPC sites is unrealised and requires further investigation.
Limitations
This study has several limitations. The retrospective design limits the ability to establish causality. Although we controlled for known potential confounders, unmeasured variables may still have influenced the outcomes. A prospective cohort study would provide stronger evidence, allowing for more standardized data collection and real-time assessment of complications. Conducting the study in a single NICU may also limit the generalisability of the findings to other settings with different patient populations and clinical practices. Moreover, the variation over time in standardised protocols may have introduced variability in the reported complication rates. However, the inclusion of all neonates resulting in a comprehensive large data set and the use of standardised protocols (e.g., for insertion and assessing PIVIE severity) helps to mitigate these limitations.
Another limitation is the lack of systematic data collection on catheter-related bloodstream infections (CRBSIs). While mechanical complications and dwell time were the primary focus of this study, CRBSIs are an important consideration when evaluating the safety of n-LPCs. Future research should investigate infection rates associated with n-LPCs to better understand their overall risk-benefit profile in neonatal vascular access.
Overall, the results from this study support the use of n-LPCs, particularly the 1 Fr variant amongst neonatal patients. However, these results also highlight a potential trade-off in peripheral vascular access device selection between longer dwell time and increased phlebitis and severity of PIVIE that warrants further study and careful consideration in practice when selecting the optimal catheter type and vascular route for long-term peripheral vascular access in neonates.
Conclusion
n-LPCs, particularly 1 Fr may provide a safer and more reliable option for long-term peripheral vascular access amongst neonates compared to n-SPCs. However, careful consideration of device factors (e.g., size and design), therapy factors such as infusate composition and the duration of intended therapy combined with patient factors such as vein diameter and location n-LPCs need prior systematic evaluation to balance the risks and benefits of particular device choices. The varied outcomes observed with octyl-butyl cyanoacrylate glue across catheter types highlight its potential to enhance securement efficacy. This study emphasises the need for ongoing research to refine the identification of risk factors for infusion-related complications and evaluate strategies aimed at reducing their occurrence and severity.
Data availability
Original datasets used during the current study are available from the corresponding author upon reasonable request. Data requests should be made to Dr Mohammad A. A. Bayoumi at moh.abdelwahab@hotmail.com.
References
van Rens, M. R. et al. The NAVIGATE project: A GloVANet-WoCoVA position statement on the nomenclature for vascular access devices. J. Vasc Access., 11297298241291248. (2024).
Bayoumi, M. A. A. et al. Effect of implementing an Epicutaneo-Caval catheter team in neonatal intensive care unit. J. Vasc Access. 22 (2), 243–253 (2021).
Legemaat, M. et al. Peripheral intravenous cannulation: complication rates in the neonatal population: a multicenter observational study. J. Vasc Access. 17 (4), 360–365 (2016).
Ainsworth, S. & McGuire, W. Percutaneous central venous catheters versus peripheral cannulae for delivery of parenteral nutrition in neonates. Cochrane Database Syst. Rev. 2015 (10), CD004219 (2015).
Indarwati, F., Mathew, S., Munday, J. & Keogh, S. Incidence of peripheral intravenous catheter failure and complications in paediatric patients: systematic review and meta analysis. Int. J. Nurs. Stud. 102, 103488 (2020).
van Rens, M. et al. The ABBA project (Assess better before Access): A retrospective cohort study of neonatal intravascular device outcomes. Front. Pediatr. 10, 980725 (2022).
van Rens, M. et al. Evaluation of unmodifiable and potentially modifiable factors affecting peripheral intravenous device-related complications in neonates: a retrospective observational study. BMJ Open. 11 (9), e047788 (2021).
Franck, L. S., Hummel, D., Connell, K., Quinn, D. & Montgomery, J. The safety and efficacy of peripheral intravenous catheters in ill neonates. Neonatal Netw. 20 (5), 33–38 (2001).
Ramasethu, J. Complications of vascular catheters in the neonatal intensive care unit. Clin. Perinatol. 35 (1), 199–222 (2008). x.
Anderson, N. R. Midline catheters: the middle ground of intravenous therapy administration. J. Infus Nurs. 27 (5), 313–321 (2004).
Pettit, J. Technological advances for PICC placement and management. Adv. Neonatal Care. 7 (3), 122–131 (2007).
van Rens, M. F. et al. Octyl-butyl-cyanoacrylate glue for securement of peripheral intravenous catheters: A retrospective, observational study in the neonatal population. J. Vasc Access. 25 (4), 1229–1237 (2024).
Moran, M. A. Introducing the midline catheter as a new intravenous access device in neonates. Neonatal Intensive Care. 5 (3), 36–42 (1992).
Wyckoff, M. Midline catheter use in the premature and Full-Term infant. J. Vascular Access. Devices. 4, 26–29 (1999).
Kleidon, T. M. et al. Midline compared with peripheral intravenous catheters for therapy of 4 days or longer in pediatric patients: A randomized clinical trial. JAMA Pediatr. 177 (11), 1132–1140 (2023).
Romesberg, T. L. Evaluating the evidence for midline catheter use in the newborn intensive care unit. J. Infus Nurs. 38 (6), 420–429 (2015).
Fu, J. et al. Impact of terminal tip location of midline catheters on catheter-related complications and indwelling duration in elderly patients. Nurs. Open. 10 (4), 2349–2356 (2023).
Chenoweth, K. B., Guo, J. W. & Chan, B. The extended dwell peripheral intravenous catheter is an alternative method of NICU intravenous access. Adv. Neonatal Care. 18 (4), 295–301 (2018).
Leick-Rude, M. K. & Haney, B. Midline catheter use in the intensive care nursery. Neonatal Netw. 25 (3), 189–199 (2006).
Lesser, E., Chhabra, R., Brion, L. P. & Suresh, B. R. Use of midline catheters in low birth weight infants. J. Perinatol. 16 (3 Pt 1), 205–207 (1996).
Colacchio, K., Deng, Y., Northrup, V. & Bizzarro, M. J. Complications associated with central and non-central venous catheters in a neonatal intensive care unit. J. Perinatol. 32 (12), 941–946 (2012).
Nakayama, Y., Takeshita, J., Nakajima, Y. & Shime, N. Ultrasound-guided peripheral vascular catheterization in pediatric patients: a narrative review. Crit. Care. 24 (1), 592 (2020).
Dawson, D. Midline catheters in neonatal patients: evaluating A change in practice. J. Vascular Access. Devices. 7, 17–19 (2002).
Nickel, B. et al. Infusion Therapy Standards of Practice, 9th Edition. J. Infus. Nurs. 47(1S Suppl 1), S1-S285 (2024).
van Rens, M. F. P. T. et al. Evaluation of a diluted lipid emulsion solution as a lubricant for improved peripherally inserted central catheter guidewire removal in a neonatal population. BMC Pediatr. 22 (1), 71 (2022).
van Rens, M. et al. Comparing conventional and modified Seldinger techniques using a micro-insertion kit for PICC placement in neonates: a retrospective cohort study. Front. Pediatr. 12, 1395395 (2024).
Bayoumi, M. A. A. et al. Neonatal simulation program: A 5 years educational journey from Qatar. Front. Pediatr. 10, 843147 (2022).
van Rens, M. et al. Cyanoacrylate securement in neonatal PICC use: A 4-Year observational study. Adv. Neonatal Care. 22 (3), 270–279 (2022).
Pittiruti, M., Annetta, M. G. & D’Andrea, V. Point-of-care ultrasound for vascular access in neonates and children. Eur. J. Pediatr. 183 (3), 1073–1078 (2024).
Curtis, S. J. et al. Ultrasound or near-infrared vascular imaging to guide peripheral intravenous catheterization in children: a pragmatic randomized controlled trial. CMAJ 187 (8), 563–570 (2015).
Pettit, J. Assessment of the infant with a peripheral intravenous device. Adv. Neonatal Care. 3 (5), 230–240 (2003).
Ullman, A. J. et al. The Michigan appropriateness guide for intravenous catheters in pediatrics: minimagic. Pediatrics 145 (Suppl 3), S269–S84 (2020).
Clark, E. et al. Reducing risk of harm from extravasation: a 3-tiered evidence-based list of pediatric peripheral intravenous infusates. J. Infus Nurs. 36 (1), 37–45 (2013).
Doellman, D. & Rineair, S. A. The Use of Optical Detection for Continuous Monitoring of Pediatric IV Sites (Journal of the Association for Vascular Access, 2019).
van Rens, M. F. et al. Peripheral intravenous therapy infiltration/extravasation (PIVIE) risks and the potential for earlier notification of events using a novel sensor technology in a neonatal population. J. Vasc Access. 25 (6), 1801–1807 (2024).
McBride, C. A. et al. Comparing IvWatch biosensor to standard care to identify extravasation injuries in the paediatric intensive care: a protocol for a randomised controlled trial. BMJ Open 12 (2), e047765 (2022).
Acknowledgements
The authors would like to acknowledge all members of the Neonatal Vascular Access Team (NeoVAT). and Neonatal Specialized Nursing (NSN) teams, and the nursing and medical staff of the Neonatal Intensive Care Unit (NICU) at Women’s Wellness and Research Center (WWRC), for their support during the study. We would like to thank all the staff in the Medical Research Center (MRC) at Hamad Medical Corporation (HMC) for their continuous help and support during this research.
Author information
Authors and Affiliations
Contributions
MFPTvR and MAAB were the main investigators. MFPTvR, conceptualized and designed the study. ALVF coordinated and supervised data collection. MAAB verified, validated and interpreted the data. MFPTvR and KH drafted the initial manuscript and developed and revised the manuscript. MAAB, ALVF, RvdL, FP and FHJvL reviewed the manuscript for important intellectual clinical and methodological inputs. FHJvL conceptualized the statistical analyses and carried out the anonymised initial data analyses. All the authors approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The study protocol (Number: MRC-01-23-012) was approved by the Institutional Review Board (IRB) of Hamad Medical Corporation (HMC), Doha, Qatar. All study procedures were conducted following relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
van Rens, M.F.P.T., Hugill, K., van der Lee, R. et al. Short versus long peripheral intravenous catheters in neonates: a retrospective cohort study. Sci Rep 15, 15373 (2025). https://doi.org/10.1038/s41598-025-00301-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00301-1