Abstract
This study aimed to examine the prevalence and epidemiological characteristics of hypertension among children and adolescents aged 7–17 years in Shaanxi Province using three hypertension guidelines for children and adolescents. Data from the 2023 Shaanxi Student’s Health Surveillance Survey were used. Hypertension was defined according to three references, namely, the 2018 National Health Commission of the China (NHCC) pediatric blood pressure reference, the 2017 American Academy of Pediatrics (AAP) clinical practice guidelines, and the 2016 European Society of Hypertension guidelines (ESH). A log-binomial regression model was applied to assess the associations between hypertension and possible risk factors. A total of 220,497 students with an average age of 11.73 years were included in the analysis. The prevalence of hypertension was 11.73%, 15.75% and 10.04% according to the NHCC, AAP and ESH guidelines, respectively. All three guidelines suggest that children who were overweight or obese or who lived in rural areas had significantly greater odds of having hypertension, and central and southern Shaanxi students had significantly lower odds of having hypertension. All three guidelines show that hypertension in children and adolescents seems to be a serious health problem in Shaanxi Province as well as in Northwestern China; thus, policymakers and public health practitioners should take immediate action to address the already established modifiable risk factors.
Similar content being viewed by others
Introduction
Hypertension, also known as high blood pressure (HBP), is a major risk factor for the development of heart failure and cardiovascular disease (CVD) from childhood to adulthood and is associated with adverse cardiac and vascular changes that can in turn be associated with CVD events in adulthood1. Hypertension is also considered a major cause of poorer disability-adjusted life-years and substantially contributes to mortality and disability2. HBP is now considered a major public health problem worldwide3. The reported prevalence of hypertension in children and adolescent were widely ranged. A largely current study by Song et al. found the prevalence of hypertension from 4.32% at 6 years of age to 7.89% at 14 years of age2. In South-Asian, studies showed that the prevalence of hypertension in children and adolescents were 7 ~ 26.34%4. Data from East Asia demonstrated the pediatric hypertension prevalence was 0.1% ~3% in Japan5 and 1.9 ~ 4.4% in Korea6.The national Surveys on Chinese Students’ Constitution and Health revealed that the prevalence of elevated BP and hypertension was 13.41% and 18.25%, respectively, in 20157. Whether incorporated alone or in conjunction with medications, lifestyle modifications (weight control for obese children, physical activity, healthy diet, and enough sleep) are always indicated and serve as the first-line therapy for adolescents with elevated blood pressure or hypertension8.
In children and adolescent, BP changes normally with increasing age and body size, which means that establishing a single set of values for systolic BP (SBP) and diastolic BP (DBP) elevation is difficult. Thus, pediatric hypertension has traditionally been defined on the basis of age-specific, sex-specific, and height-specific normative values. In 2004, the US National Heart, Lung, and Blood Institute released its Fourth Report on the Diagnosis, Evaluation, and Treatment of High BP in Children and Adolescents, which recommended pediatric hypertension as a value that met or exceeded the sex-, age-, and height-specific 95th BP percentile9. In 2016 and 2017, the European Society of Hypertension (ESH)10 and American Academy of Pediatrics (AAP)8, respectively, updated their childhood hypertension management. The National Health Commission of the People’s Republic of China (NHCC), in 2018, published a reference for screening for elevated blood pressure among children and adolescents aged 7–18 years11. The definitions differences of three guidelines are shown in Table 1. In the AAP guideline, the normative values did not include data from individuals who were classified as overweight or obese due to the known associates between overweight and obesity and blood pressure. The exclusion of these data resulted in reference tables with a 1–4 mm Hg decrease in threshold cutoff points for elevated blood pressure and hypertension compared with the ESH guideline. In addition, the static cutoff points in the AAP and NHCC guidelines are lower than the ESH cutoff points12. After the publication of these guidelines, these statements caused active discussion. Their sensitivity was tested, and the percentage of reclassified children differed in some populations13. Antolini et al. reported that the AAP guidelines detected a greater incidence of hypertension than did the ESH guidelines14. Despite the large number of studies that have assessed the prevalence of hypertension in children and adolescents, to our knowledge, estimates of the prevalence of childhood hypertension have not been made using the NHCC, ESH and AAP guidelines in Shaanxi province, Northwestern China.
Until recently, however, limited population-based data on the prevalence and epidemiological characteristics of hypertension in Shaanxi Province or Northwest China were available. The objective of this study was to investigate the prevalence and epidemiological characteristics of hypertension among children and adolescents aged 7–17 years in Shaanxi Province using the three hypertension guidelines for children and adolescents. We expect the results to provide the most updated information on the rate of hypertension among children and adolescents in Shaanxi Province, Northwest China.
Results
The final population included in the analyses consisted of 220,497 students aged 7–17 years, and 112,354 (50.95%) were boys. Table 2 shows the basic characteristics of this study population. The average age of our participants was 11.73 years. The average SBP and DBP of our participants were 106.39 mmHg and 66.84 mmHg, respectively. Significant differences were observed in the distributions of participant age, area, region groups, educational level, SBP, DBP, height, weight, BMI and BMI status between male and female participants (Table 2).
The prevalence of hypertension was 11.73% (95% CI: 11.59, 11.86%), 10.04% (95% CI: 9.91, 10.16%) and 15.75% (95% CI: 15.60, 15.91%) according to the NHCC, ESH and AAP guidelines, respectively. The prevalence of pediatric hypertension according to the NHCC, ESH and AAP guidelines are compared in Table 3. The prevalence of hypertension in 7–12-year-old and 13–15-year-old participants was 10.65% (95% CI 10.48, 10.82%) and 13.30% (95% CI 13.03, 13.57%), respectively, according to the NHCC guidelines and the ESH and AAP guidelines. The prevalence of hypertension in individuals aged 16–17 years was 13.03% (95% CI 12.66–13.40%) in the NHCC guidelines and 2.43% (95% CI 2.26–2.60%) in the ESH guidelines, representing a difference of more than six times. The results from subgroup analyses according to sex, area, regions and BMI status showed that the prevalence of hypertension according to the NHCC guidelines was greater than that according to the ESH guidelines and lower than that according to the AAP guidelines.
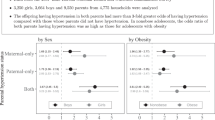
Figure 1 shows the results of the unadjusted model, where obesity showed the strongest association with developing hypertension (UPR = 2.09, 95% CI 2.03–2.14). This was followed by overweight (UPR = 2.09, 95% CI 2.03–2.14), which was associated with greater odds of having hypertension according to NHCC guidelines. A similar result was also observed for the ESH and AAP guidelines.
Table 4 describes the risk factors associated with hypertension according to the NHCC, ESH and AAP guidelines after all the possible risk factors were adjusted for in the log-binomial multivariate model. Compared with 7- to 12-year-old participants, 13- to 15-year-old participants had a greater incidence of hypertension according to the NHCC and ESH guidelines but a lower incidence of hypertension according to the AAP guidelines. Sixteen- to 17-year-old participants had a significantly lower incidence of hypertension according to the ESH guidelines but a greater incidence according to the NHCC and AAP guidelines. Moreover, girls had a significantly greater incidence of hypertension than boys did only according to the NHCC standard. However, according to the ESH and AAP guidelines, girls had a significantly lower incidence of hypertension than boys did. Students who lived in suburban areas were more likely to have hypertension than those who lived in urban areas according to all the guidelines. The prevalence of hypertension in children was lower in central and southern Shaanxi Province than in northern Shaanxi Province according to all guidelines. Furthermore, overweight and obesity increased the risk of hypertension among children according to all three guidelines.
Discussion
A large population-based cross-sectional Student’s Health Surveillance study conducted in Shaanxi Province, Northwest China, investigated the prevalence and epidemiological characteristics of hypertension among children and adolescents in 2023. We found that the prevalence of hypertension was approximately 10.04–15.75% among those aged 7–17 years according to three different guidelines. Furthermore, the rate of hypertension differed significantly with respect to baseline characteristics among the participants in the surveillance areas.
The prevalence of HBP varies widely across studies worldwide (ranging from 0.6 to 25.1%) performed at different times, in different manners, across age groups, and among populations of children and adolescent15. For instance, the prevalence of hypertension in Lithuanian adolescents aged 12–15 years is 22.2%16; in 9-13-year-old Greek school children, it is 23%17. The prevalence in Portuguese children and adolescents aged 4 to 18 years it is 12.8%18, and in 10-18-year-old Polish schoolchildren, it is 8.9%19. Data from East Asia demonstrated relatively lower prevalence, pediatric hypertension was estimated to be 0.1 ~ 10.6%4. A recent India systematic review reported a lower prevalence (7%) than the present result20. The prevalence of hypertension in Hongkong Chinese adolescent is 1.44%, which is much lower than the prevalence in Northwestern of China21. The prevalence revealed in this study is comparable to that in Korea from 1997 to 2013, but is much higher than the prevalence in Korea in recent year22. In Japan, a health check-up survey at elementary and junior high schools reported pediatric hypertension in 0-4.4% of each grade and in 0.9% of the overall population23. Therefore, blood pressure BP control in early life in China is important and meaningful.
Our findings demonstrate the variations in the estimated prevalence of hypertension in Shaanxi Province according to the NHCC, ESH and AAP guidelines, which were developed to classify prehypertension and hypertension statuses in children and adolescents. Our results indicate that the overall and subgroup (sex, area, region, and BMI status) hypertension incidence determined using the AAP guidelines was significantly greater than that determined using the NHCC and ESH guidelines24,25,26. The use of the AAP guidelines resulted in a lower incidence of hypertension in the 13–15 years age subgroup than did the use of the NHCC guidelines. Differences in the prevalence of hypertension and the ability to detect hypertension in children may be attributable to variations in the diagnostic thresholds of those three guidelines. Differences in the cut-offs of hypertension diagnostic criteria can be achieved due to differences in the reference population (e.g., year of data collection, basic characteristics) and different inclusion and exclusion criteria.
Interestingly, all of the guidelines revealed a greater prevalence of hypertension among suburban students than among urban students. Suburban children and adolescents were 1.19, 1.16 and 1.14 times more likely to have hypertension according to the NHCC, ESH and AAP guidelines, respectively, than were urban children and adolescents. This finding is consistent with previous research27,28. However, the difference in BP can be explained by children in rural areas having increases in heart rates, glycolipid levels, and breastfeeding prevalence and decreases in SES status and physical activity compared with those in urban areas29. The high incidence of childhood hypertension is alarming in rural areas, and urgent intervention is needed to determine the main risk factors. Thus, health education should include interventions to target hypertension in children in rural areas.
We also found that the incidence of hypertension varied geographically in the surveyed population. The prevalence of hypertension in central and southern Shaanxi was lower than that in northern Shaanxi. Shaanxi Province is divided into northern Shaanxi, Guanzhong, and southern Shaanxi. These regions have different natural conditions, such as soil types, topography, and climate, with different patterns of agricultural production30. For geographical and sociocultural reasons, dietary patterns are different and population specific in each area31. The diet of the people is based on whole grains and mutton in the Northern Shaanxi. In the Guanzhong region, people prefer to eat varieties of cooked wheaten food. The main food consumption is rice in southern region. Meanwhile, the lowest scores of the equilibrium pattern were in northern Shaanxi, and the scores of the snack pattern were greater in northern Shaanxi than in central and southern Shaanxi32. These factors could explain in part the regional discrepancies in the incidence of hypertension in children across Shaanxi Province. However, further studies will be required to clarify the contributions of these factors.
General and abdominal obesity in children and adolescence is a serious growing health problem worldwide. Globally, the number of deaths due to high BMI has substantially increased from 2.2 million in 1990 to 4.7 million in 201733. Many studies reported that low infant BMI and high childhood BMI were associated with an increased risk of Non-Communicable Disease (NCD) related outcomes in later life34. A substantial burden of NCD deaths was attributed to high BMI in Chile35. A large analyses found that incremental increases in BMI above 25 kg/m2 were associated with a higher risk of cardiovascular, renal, hepatic and other cause-specific mortality36. In Japanese adults with normal or elevated BP, the risk of developing hypertension increased with BMI37. Because of the close association between obesity, based on BMI level, and HBP, some researchers have predicted that the prevalence of HBP in children and adolescents would increase along with the increase of BMI level38. We observed that overweight and obese children and adolescents, respectively, had a greater possibility of developing hypertension according to all of the guidelines, which is consistent with other studies showing that blood pressure or hypertension are positively correlated with BMI and obesity21,38. For example, Indian children with obesity had a significantly greater incidence of hypertension than did normal weight children20. A large study consisting of 7 cross-sectional surveys conducted in China, Korea, Poland, the USA, India, Iran, and Tunisia revealed that the relationship between BMI and HBP began in the 25th BMI percentile39. The levels of BP increased in parallel with increasing BMI among Chinese boys and girls. This is possibly because some adipocyte-derived factors are linked to blood pressure control, and aberrant production and release of those factors may contribute to a high incidence of hypertension in overweight and obese individuals40. Thus, body weight control was equally effective in decreasing BP.
Strengths of this study are the large sample size student in all 113 countries of Shaanxi province to minimize selection bias, and the use of the three current blood pressure guidelines which allows international comparisons of the prevalence of hypertension among children and adolescents between countries and regions. However, this study has some limitations. First, as a cross-sectional survey, only the prevalence of HBP can be determined, and no conclusion can be drawn on the cause of HBP in this population. Second, all causes of HBP could not be included due to the limitations of our survey methods. For example, HBP causing only undetectable BP is difficult to identify in students; hence, we suspect that our data underestimate the prevalence and burden of HBP. Nevertheless, the current study is the largest survey in northwestern China, providing the most up-to-date data on HBP and filling a gap in the knowledge of this geographical region.
Methods
Study area
Shaanxi province is located in Northwestern China, economic conditions are worse, and health services are less developed than in the eastern and coastal areas of China. It covers an area of over 200,000 square kilometers and has a population of 38.38 million. Shaanxi province has 14 districts (cities and counties) and 109 counties (cities, districts) under its jurisdiction. Shaanxi Province is divided by the Beishan Mountain and Qinling Mountain into three districe regions: northern Shaanxi, Guanzhong, and southern Shaanxi. The northern Shaanxi region is located on the Loess Plateau, north of the Beishan Mountain. The Guanzhong region is located between Beishan Mountain and Qinling Mountain. The southern Shaanxi region is located south of the Qinling Mountain. Nearly half of the population of Northwest China lives in Shaanxi Province.
Study design and data source
This study analyzed the cross-sectional survey data set of the 2023 Shaanxi Student’s Health Surveillance Survey. The survey was conducted between September and December 2023 in Shaanxi Province, Northwest China. Considering the imbalanced population distribution and economic level between urban and suburban areas in the province, a stratified multistage cluster sampling method was employed. In the urban city, we randomly selected eight schools as surveillance schools, and in the suburban county, five schools were randomly selected as the surveillance schools for there are no vocational high school and university and there are only one senior school in majority counties. In the selected school, 2 classes were randomly chosen from each grade. All students from the selected class participated in the survey (Fig. 2). All the demographics (age, sex and grade) and geographic location (urban/rural) information were collected from the registration information of surveillance school by the employees of Centre for Disease Control and Prevention. Finally, 647 schools were sampled within 113 prefectures in Shaanxi Province, and 221,004 students were included in the surveillance.
The inclusion criteria of this study were as follows: (1) students resident Shaanxi; (2) the basic information (age, sex, grade, county and city) collected from school is complete, (3) availability of all data required for the analysis, included height, weight, SBP and DBP. Children with CHD, chronic kidney disease, chronic liver disease or diabetes mellitus were excluded. Therefore, 507 (109 lack of basic information, 152 lack of BP data, 103 lack of height and weight, 143 excluded for chronic disease) students were excluded. According to the National Survey on Chinese Students’ Constitution reported prevalence of hypertension in children and adolescent was 18.25%7, with a power of 90%, using a two-sided alpha level of 0.05, and 15% non-response rate. Thus, after the noted exclusion, a total of 220,497 students were included in the statistical analysis, explaining the conclusion of this study fully enough.
The surveillance was approved by the Shaanxi Provincial Center for Disease Control and Prevention. All student were informed consent before surveillance. All methods were applied in accordance with relevant guidelines and regulations.
BP measurements and definitions
BP was measured using a standard mercury sphygmomanometer recommended for upper arm models that are certified according to international standard schemes that passed a comprehensive test for measurement reliability. Measurements were performed by trained health technicians after at least 5 min of rest. BP was measured three times (at 1–2 min intervals). The average of the three SBP and DBP measurements was calculated. If the values of the measurements were high or fluctuated, the students were asked to calm down, and the measurement was repeated. The instruments used for the measurements were checked and calibrated in advance.
Hypertension was defined as a BP ≥ 95th percentile based on age, sex and height percentiles according to the NHCC guidelines. The ESH guidelines recommend a similar definition of hypertension for children younger than 16 years and a BP ≥ 140/90 mmHg for those aged 16 years and older. Pediatric hypertension was defined as a BP ≥ 95th percentile for sex, age, and height or 130/80 mm Hg for children younger than 13 years and ≥ 130/80 mm Hg for those aged 13 years and older as per the AAP guidelines. In our comparison of prevalence, we considered children with elevated BP (prehypertension or high normal BP) and hypertension identified by each guideline as having “elevated BP” (Table 1).
General examinations and definitions
The height and weight were measured using standard and calibrated equipment. Weight was measured to the nearest 0.10 kg with a balance-beam scale while the subjects were wearing lightweight clothing. Height was measured to the nearest 0.1 cm using a stadiometer without shoes according to a standardized protocol. Body mass index (BMI) is a widely used measure of weight status in childhood; it was calculated as weight in kilograms divided by the square of height in meters. BMI was categorized as normal weight (< p85th), overweight (P85th to P95th) or obese (≥ P95th) according to the American Centers for Disease Control (CDC) and Prevention Growth in 200041.
Statistical analysis
Continuous variables are presented as the mean (standard deviation, SD), and categorical variables are presented as frequencies (%). Significant differences among the variables were determined by t tests for normally distributed variables and chi-square tests for categorical data. We used the normal approximation method to estimate the prevalence of hypertension with 95% confidence intervals (CIs) as defined in the NHCC, ESH and AAP guidelines stratified by demographic characteristics, and difference prevalence with SD between NHCC and ESH / AAP. Thereafter, we used a log-binomial regression model to identify the factors associated with hypertension, describing the results with prevalence ratios (PRs) and their 95% CIs and P values. We used SAS version 9.4 (SAS Institute, Cary, NC, USA) for all the statistical analyses.
Conclusion
We believe the current study, with a large sample size provides a reliable estimate of prevalence of adolescent hypertension in Shaanxi province. The hypertension among children and adolescents is more common in Shaanxi Province, Northwestern China. Of the factors studies, living in suburban, northern area of Shaanxi and being overweight or obese were all positively correlated with HBP incidence among children and adolescents in the study areas. These findings may have important public health policy implications for pediatric HBP interventions in Northwest China.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Song, P. et al. Global prevalence of hypertension in children. JAMA Pediatr. 173(12). (2019).
Daniels, S. R. Understanding the global prevalence of hypertension in children and adolescents. JAMA Pediatr. 173(12). (2019).
Rahmoune., H., Bioud, B. & N. Boutrid., and Antimicrobial prophylaxis for children with vesicoureteral reflux. N. Engl. J. Med. 371 (11), 1070–1073 (2014).
Hsu, W. F. et al. A reappraisal of the prevalence of pediatric hypertension through a nationwide database in Taiwan. Sci. Rep. 11 (1), 4475 (2021).
Umemura, S. et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2019). Hypertens. Res. 42 (9), 1235–1481 (2019).
Khang, Y. H. & Lynch, J. W. Exploring determinants of secular decreases in childhood blood pressure and hypertension. Circulation 124 (4), 397–405 (2011).
Tian, C. et al. Prevalence of pre-high blood pressure and high blood pressure among non-overweight children and adolescents using international blood pressure references in developed regions in China. Ann. Hum. Biol. 44 (6), 574–577 (2017).
Flynn, J. T. et al. Urbina EM Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140 (3), e20171904 (2017).
Adolescents., N. H. B. P. E. P. W. G. H. B. P. C. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114 (2 Suppl 4th Report), 555–576 (2004).
Lurbe, E. et al. 2016 European society of hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34 (10), 1887–1920 (2016).
China, N. H.C.o.t.P.s.R.o., Reference of screening for elevated blood pressure among children and adolescents aged 7-18 years. National Health Commission of the People’s Republic of China: China, 6 (2018).
Khoury, M. & Urbina, E. M. Hypertension in adolescents: diagnosis, treatment, and implications. Lancet Child. Adolesc. Health. 5 (5), 357–366 (2021).
Di Bonito, P. et al. The American academy of pediatrics hypertension guidelines identify obese youth at high cardiovascular risk among individuals non-hypertensive by the European society of hypertension guidelines. Eur. J. Prev. Cardiol. 27 (1), 8–15 (2020).
Antolini, L. et al. Nomograms to identify elevated blood pressure values and left ventricular hypertrophy in a paediatric population. J. Hypertens. 37 (6), 1213–1222 (2019).
Furdela, V. et al. Prevalence of arterial hypertension among Ukrainian students: the comparison of European and American guidelines. Pediatr. Endocrinol. Diabetes Metab. 28 (2), 123–131 (2022).
Kuciene, R. & Dulskiene, V. Associations between body mass index, waist circumference, waist-to-height ratio, and high blood pressure among adolescents: a cross-sectional study. Sci. Rep. 9 (1), 9493 (2019).
Karatzi, K. et al. Prevalence of hypertension and hypertension phenotypes by age and gender among schoolchildren in Greece: the healthy growth study. Atherosclerosis 259, 128–133 (2017).
Maldonado, J. et al. An approach of hypertension prevalence in a sample of 5381 Portuguese children and adolescents. The AVELEIRA registry. Hypertension in children. Blood Press. 20 (3), 153–157 (2011).
Kaczmarek, M. et al. Who is at higher risk of hypertension? Socioeconomic status differences in blood pressure among Polish adolescents: a population-based ADOPOLNOR study. Eur. J. Pediatr. 174 (11), 1461–1473 (2015).
Meena, J. et al. Prevalence of hypertension among children and adolescents in India: A systematic review and Meta-Analysis. Indian J. Pediatr. 88 (11), 1107–1114 (2021).
Leung, L. C. K. et al. Prevalence and risk factors for hypertension in Hong Kong Chinese adolescents: waist circumference predicts hypertension, exercise decreases risk. Arch. Dis. Child. 96 (9), 804–809 (2011).
Xi, B. et al. Recent blood pressure trends in adolescents from China, Korea, Seychelles and the united States of America, 1997–2012. J. Hypertens. 34 (10), 1948–1958 (2016).
Kikuchi, T. Pediatric hypertension based on Japanese society of hypertension guidelines (JSH 2019) with actual school blood pressure screening data in Japan. Clin. Experimental Pediatr. 65 (6), 283–290 (2022).
Fan, H. & Zhang, X. Difference in hypertension prevalence applying three childhood hypertension management guidelines in a National cohort study. J. Hum. Hypertens. 35 (11), 1038–1045 (2020).
Stabouli, S., Redon, J. & Lurbe, E. Redefining hypertension in children and adolescents: A review of the evidence considered by the European society of hypertension and American academy of pediatrics guidelines. J. Hypertens. 38 (2), 196–200 (2020).
Condren, M. et al. The impact of new guidelines on the prevalence of hypertension in children: A cross-sectional evaluation. J. Clin. Hypertens. 21 (4), 510–515 (2019).
Yang, Y. et al. Prevalence trends of hypertension and influence factors among children and adolescents aged 7–17 years in China, 2011–2015: A serial cross-sectional study. Front. Public. Health 10 (2022).
Yan, W. et al. Reevaluate secular trends of body size measurements and prevalence of hypertension among Chinese children and adolescents in past two decades. J. Hypertens. 34 (12), 2337–2343 (2016).
Liang, X. et al. Prevalence and risk factors of childhood hypertension in Urban-Rural areas of China: A Cross-Sectional study. Int. J. Hypertens. 2020, 1–18 (2020).
Wu, J. et al. Sustainable strategies for the agricultural development of Shaanxi Province based on the risk assessment of heavy metal pollution. Foods 11(10) (2022).
Hu, F. B. Dietary pattern analysis_ a new direction in nutritional epidemiology. Curr. Opin. Lipidol. 13 (1), 3–9 (2002).
Spradley, F. T. et al. Geographical variations in maternal dietary patterns during pregnancy associated with birth weight in Shaanxi Province, Northwestern China. Plos One 16(7) (2021).
Wareham, N. J. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the global burden of disease study. PLoS Med. 17(7) (2020).
Bander, A. et al. Childhood BMI and other measures of body composition as a predictor of cardiometabolic non-communicable diseases in adulthood: a systematic review. Public Health. Nutr. 26 (2), 323–350 (2022).
Riquelme, R. et al. Non-communicable diseases deaths attributable to high body mass index in Chile. Sci. Rep. 11(1) (2021).
Koethe, J. R. et al. Body mass index and the risk of incident noncommunicable diseases after starting antiretroviral therapy. HIV Med. 16 (1), 67–72 (2014).
Suzuki, Y. et al. Threshold of BMI for the development of hypertension among Japanese adults. J. Nutr. 152 (11), 2565–2571 (2022).
Dong, B. et al. Trends in blood pressure and body mass index among Chinese children and adolescents from 2005 to 2010. Am. J. Hypertens. 26 (8), 997–1004 (2013).
Wang, M. et al. Body mass index percentiles and elevated blood pressure among children and adolescents. J. Hum. Hypertens. 34 (4), 319–325 (2020).
Willig, A. L. et al. Adjusting adiposity and body weight measurements for height alters the relationship with blood pressure in children. Am. J. Hypertens. 23 (8), 904–910 (2010).
Ogden, C. L. & Flegal, K. M. Changes in terminology for childhood overweight and obesity. Natl. Health Stat. Rep. 25, 1–5 (2010).
Acknowledgements
We would like to thank all participants and investigators in this study.
Author information
Authors and Affiliations
Contributions
Author contributionsMinmin Li, Nan Yang and Ruhai Bai designed the study and selected the study methodology; Minmin Li, Xinyan Wang, Jingjun Zhao, Qianyun Wang and Tong Hui collected and organize data; Minmin Li and Ruhai Bai analyzed and interpreted the data; Minmin Li, Wei Shi and Ruhai Bai edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, M., Yang, N., Zhao, J. et al. Prevalence and risk factors for hypertension among children and adolescents in Shaanxi province, Northwestern China, according to the three hypertension guidelines. Sci Rep 15, 18963 (2025). https://doi.org/10.1038/s41598-025-01039-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01039-6