Abstract
Hepatitis B virus (HBV) infection is a global public health concern with a high burden in the African region. Assessing trends in HBV infection over time can provide insights into the effectiveness of prevention/treatment strategies in different settings. Herein, we investigate trends in active HBV infection and associated risk factors among blood donor candidates from Luanda, Angola. This was a retrospective study conducted with 96,654 medical records of blood donors consulted between 2018 and 2022 at the Angolan National Blood Institute. Participants were screened for hepatitis B surface antigen (HBsAg). Chi-square, Prevalence Ratio, and logistic regression were used to analyse interactions between demographic variables and were deemed significant when p < 0.05. Active HBV infection was 10% (95% CI: 9.4–10.6). Men (AOR: 1.38, p < 0.001), employed (AOR: 3.25, p < 0.001) and non-urbanised regions (AOR: 1.16, p = 0.019), were more likely to contract the HBV, while aged 30 years or older (AOR: 0.78, p < 0.001) and married (AOR: 0.66, p < 0.001), were less likely to contract the infection. From 2018 to 2022, HBV infections increased from 18.2 to 21.9%. Infections increased in under 30 years (31.3–52.5%, p < 0.001), males (91.1 to 91.8%, p = 0.149), urbanised regions (2.7 to 3.3%, p = 0.538), and unmarried (93.9 to 95.8%, p = 0.019). We revealed a highly active HBV infection over the past 5 years in the adult population of Luanda, Angola. Age, gender, occupation, place of residence and marital status have influenced the dissemination of HBV in Angola. Our findings may facilitate the planning and evaluation of the HBV control program in Angola.
Similar content being viewed by others
Introduction
Hepatitis B virus (HBV) is a liver-targeting viral infection that can lead to acute or chronic conditions. Globally, around 296 million people are living with HBV, and the burden disproportionately affects sub-Saharan Africa1. According to the World Health Organization (WHO), the burden of HBV infection is highest in the African Region, where 65 million people are chronically infected2. HBV endemicity levels based on hepatitis B surface antigen (HBsAg) prevalence were defined as low (< 2%), intermediate (2–7.99%) and high (≥ 8%)3. In Angola, the prevalence has varied from 7.5 to 25.7% indicating intermediate to high prevalence4,5,6,7,8,9. Several studies have shown that socioeconomic conditions, place of residence, level of education, accessibility to medical care, awareness and health programs, have served as a drive for the unprecedented increase of HBV infections in Africa10.
Currently, there is limited published data on HBV seroprevalence among the general population of Angola. Furthermore, the existing published data have small sample sizes, which makes it difficult to assess in detail the potential determinants or patterns of sexual behaviour that enhance HBV transmission in different regions of Angola. To the best of our knowledge, this is the first study that uses a large dataset to provide insight into the evolution of HBV cases over time as well as the putative demographic determinants related to infection in Angola. In this study, we investigated trends in HBV seroprevalence and risk factors associated with infections in the last 5 years (2018–2022) among blood donor candidates from Luanda, the capital city of Angola. The findings of this study provide insights into transmission patterns and evidence for future research on local interventions to control the dissemination of HBV in Angola.
Materials and methods
Study design and setting
This was a retrospective study conducted with the clinical record of 96,654 blood donor candidates consulted between 2018 and 2022 at the National Blood Transfusion Service in Angola, located in Luanda, the capital city of Angola. The years 2018–2022 were selected for analysis because they represent a period with more complete data on HBV seroprevalence at the National Blood Institute in Angola. During this period, significant improvements were made to data collection and reporting systems, which allowed for more accurate and comprehensive analysis. The study was carried out under the responsibility of the Angolan Health Research Center (CISA)|National Institute for Health Research (INIS). The CISA|INIS is an Angolan-specialized regional research and development institution supervised by the Angolan Ministry of Health (MoH) that promotes Health Research, whose main objective is to generate, develop and disseminate scientific, technological, and strategic knowledge about health and its determinants, for strengthening public health policies and improving the national health system in Angola. The study was conducted following Helsinki’s declaration. The study protocol received ethical approval by the National Blood Transfusion Service in Angola (nr.428/GDG/INS/2024, approved on March 7th, 2024). The need for informed consent to participate was waived by an Institutional Review Board (IRB), the clinical and pedagogical direction of the National Blood Transfusion Service in Angola, however, all data collected from medical records were anonymized to safeguard the identity of blood donors.
Data, sample collection, and laboratory procedure. A questionnaire initiated for this study was used to collect sociodemographic data such as age, gender, occupation, area of residence, marital status, and the year of blood donation. In addition, the HBV test results of all candidates, screened for the presence of anti-HBsAg (Abbott, USA) using the ARCHITECT Plus i2000SR (Abbott, USA), were collected.
Statistical analysis
The collected data was analyzed using SPSS v29 (IBM SPSS Statistics, UAS). Descriptive analyses are presented as frequencies and percentages. Quantitative data that followed a normal distribution, the mean and standard deviation (SD) were reported. Furthermore, the differences in means between groups were calculated with an independent-sample t-test or analysis of variance (ANOVA), as appropriate. To investigate interactions between qualitative variables, the Chi-square was utilized. Furthermore, after examining the frequencies and distributions of qualitative variables, we estimated prevalence ratios (PRs) and their corresponding 95% confidence intervals (CIs) using a generalised linear model (GLM) with a Poisson distribution. Additionally, an adjusted odds ratio (AOR) along with 95% confidence intervals (CIs) was calculated through multivariate logistic regression analysis. Throughout the study, two-tailed p-values were reported, and statistical significance was determined when p < 0.05.
Results
Demographic characteristics and risk factors related to active HBV infection
The demographic characterisation of the participants and the putative features related to active HBV infection using HBsAg are presented in Table 1. A total of 96,654 blood donor candidates were enrolled in the present study. The age of the candidates ranged from 18 to 65 years old, with a mean of 34.0 ± 8.69 years old. Blood donor candidates aged between 30 and 40 years old (43%, 41604/96654), male (89.7%, 86734/96654), employed in either the public or private sector (76.5%, 73961/96654), living in the non-urbanized region (96.6%, 93390/96654), and unmarried (92.8%, 89695/96654), were the most predominant. A total of 9668/96,654 (10.0%; 95% CI: 9.4 – 10.6%) of the blood donors candidates were reactive to HBsAg biomarker. The mean age of HBsAg reactive candidates was significantly lower (32.7 ± 8.08 years old) compared to non-reactive donors (34.2 ± 8.74 years old), with a difference of 1.42 years (p < 0.001). Individuals aged 18–30 years (11.4%, 3907/34253) and 30–40 years (10.1%, 4196/41604) had the highest positivity rates of HBsAg positivity. According to a generalized linear model with a Poisson distribution, they were 1.52 times (95% CI: 1.43–1.60, p < 0.001) and 1.34 times (95% CI: 1.27–1.42, p < 0.001) more likely to be infected, respectively, compared to individuals over 40 years old. Men had a higher positivity rate (10.3%, 8914/86734) and were 1.35 times (95% CI: 1.26–1.45, p < 0.001) more likely to contract the infection compared to women. Similarly, employed candidates (10.1%, 7438/73961) and students (12.5%, 1988/15957) had an increased likelihood of infection, with prevalence ratios of 2.8 (95% CI: 2.47–3.17, p < 0.001) and 3.47 (95% CI: 3.04–3.95, p < 0.001), respectively. Individuals from non-urbanized regions (10.1%, 9391/93390) had a higher positivity rate and were 1.19 times (95% CI: 1.06–1.33, p = 0.004) more likely to contract the infection compared to those from urban areas. Unmarried individuals (10.3%, 9207/89695) had higher infection rates, whereas married individuals were 0.65 times (95% CI: 0.59–0.71, p < 0.001) less likely to contract the infection. The proportion of blood donation candidates increased from 17% (16391/96654) in 2018 to 23.8% (22993/96654) in 2022. The prevalence of active HBV infection during this period ranged from 9.2 to 10.7%. Additionally, candidates selected between 2018 and 2021 had a higher likelihood, with prevalence ratios values between 1.07 and 1.17 (95% CI: 1.01–1.24, p < 0.05).
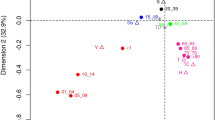
Multivariate analysis revealed that men [AOR: 1.38 (95% CI: 1.28–1.50), p < 0.001], employed [AOR: 3.25 (95% CI: 2.86–3.71), p < 0.001] and those living in non-urbanised regions [AOR: 1.16 (95% CI: 1.03–1.32), p = 0.019], were more likely to contract HBV infection. In contrast, individuals aged 30 years or older [AOR: 0.78 (95% CI: 0.75–0.82), p < 0.001], married [AOR: 0.66 (95% CI: 0.60–0.73), p < 0.001] and candidates screened between 2020 and 2022 [AOR: 0.93 (95% CI: 0.89–0.97), p = 0.002], had a lower likelihood to contract the infection (Fig. 1).
Trends in active hepatitis B virus infection and associated factors between 2018 and 2022
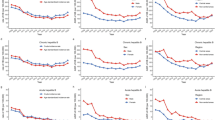
The result of the trend of active HBV infection cases in the adult population in Luanda is shown in Table 2. Overall, the cases of active HBV infection increased from 18.2% (1762/9668) to 21.9% (2113/9668). The average age of infected individuals has significantly decreased from 34.3 ± 7.82 years in 2018 to 30.7 ± 8.17 years in 2022 (p < 0.001). The active HBV Infections increased from 31.3% in 2018 to 52.5% in 2022, in individuals under 30 years old, while decreases were observed in the same periods for individuals between 30 and 40 years old (49.5–35.0%) or individuals over 40 years old (19.1–12.5%) (p < 0.001). Regarding gender, despite no statistical significance, we observed a slight reduction in the infection rate in females from 8.9% in 2018 to 8.2% in 2022, while an increase was observed in males (91.1–91.8%), in the same period (p = 0.149). Increases in active HBV infection rates were also observed in students (21.3–22.1%), while employed (76.7–76.3%) or unemployed (2.0–1.6%) individuals showed a decrease between 2018 and 2022 (p < 0.001). Increases in active HBV infection rates were also observed in individuals from urbanized regions (2.7–3.3%), while a decrease was observed in individuals from non-urbanized areas (97.3–96.7%) between 2018 and 2022, although no statistical significance was observed (p = 0.538). Regarding marital status, an increase in infection cases was observed in unmarried individuals (93.9–95.8%), while a decrease was observed in married individuals (6.1–4.2%) from 2018 to 2022 (p = 0.019).
Discussion
HBV infection is a very large burden in all sub-Saharan African regions3. The present study revealed a significantly high active HBV infection of 10% (95% CI: 9.4 − 10.6%) in the adult population of Luanda, the capital city of Angola. We show that in the last 5 years (2018–2022), the active HBV infection was high (> 8%), ranging from 9.2 to 10.7%. It is worth mentioning that regions with high HBV endemicity have been associated with high mortality rates from primary liver cancer, since chronic HBV infection is responsible for 40% of the global burden of hepatocellular carcinoma (HCC), with a high fatality rate11. Indeed, our research team recently identified that approximately 80% of HBsAg-positive individuals in Luanda, Angola, had chronic liver disease, while 20% had acute liver disease, based on the AST/ALT ratio, indicating that individuals up to 40 years old (OR: 1.97), women (OR: 1.61), living in non-urbanized areas (OR: 1.69), with low educational level (OR: 1.64), and unemployed (OR: 1.81) were more likely to develop chronic liver disease12. These findings showed that authorities should consider including nucleic acid testing (NAT) to ensure the identification of occult infections, as well as provide an assessment of liver function in HBV-infected individuals, whether in the acute or chronic phase.
In the present study, active HBV infection is associated with certain sociodemographic and behavioural determinants such as age, gender, occupation, residence and marital status, that elucidate the multifaceted impact of sociodemographic and behavioural determinants on HBV infection risk, underscoring the necessity for targeted public health interventions in Angola. Indeed, the multivariate logistic regression model applied in the studied population revealed that men, employees and non-urbanized areas are more likely to test positive for HBsAg, while adult individuals aged 30 or over, and married were less likely compared to their counterparts.
The trend of active HBV infection over time in the capital of Angola increased from 16.8% in 2018 to 21.9%, equivalent to a rise of 5.1%. These results could jeopardize the WHO’s goal of eliminating viral hepatitis as a public health problem by 2030 1. The interactions between different sociodemographic and behavioural characteristics with susceptibility to HBV infections over the years remain poorly understood in Angola. According to our findings, the increase in active HBV infection in the Angolan population has been driven by the youngest individuals aged up to 30 years old, male, employed/student, resident in urbanised areas, and unmarried.
Younger individuals under 30 years old had a prevalence ratio of 1.52 times more likely to acquire HBV infection, with a prevalence of around 10.4 − 12.4%, which may be attributed to potential gaps in vaccination coverage or behavioural factors. As reported in other studies, in the age group up to 30 years, the most prominent presumptive source of HBV infection is sexual because it is a sexually active age13. However, future studies investigating the proportion of presumptive sources of HBV infection according to age should be carried out in Angola. Previous studies have indicated that prevalence rates in younger individuals in sub-Saharan African countries are up to 12% and are more pronounced among men3, which is consistent with our results, where a prevalence of 11.4% (95% CI: 10.4–12.4%) was observed in the young population aged 18–29 years, and the male gender is also predominant. From 1990 to 2005, there was an overall decrease in HBsAg prevalence in younger age groups globally, which might be closely related to widespread immunisation against HBV14. However, the increase in seroprevalence in the youngest Angolan population from 31.3% in 2018 to 52.5% in 2022 suggests a failure of immunisation measures against HBV in the younger population requesting urgent public health intervention in this risk group.
We revealed a remarkably increasing HBV positivity rate between 2018 and 2022 among males, although no statistical significance was observed (p = 0.149). Studies conducted with blood donors in Malaysia15, Brazil16, and China17 have also shown that male was associated with HBsAg seropositivity. Other studies conducted in Angola have also shown an increase in the prevalence and risk of sexually transmitted infections (STIs) such as HIV, HCV and Syphilis in the male population living in the capital of Angola7,18,19, pointing to men as the main source of the spread STIs. It is worth mentioning that unhygienic tattoos, piercings, high-risk sexual activities, and alcohol consumption are common practices among young men aged up to 30 years in Luanda. Therefore, conducting studies on the association between lifestyle or occupational risks and HBV could ensure control of the spread of HBV and related diseases in Angola.
The profile of infected individuals differed significantly according to place of residence, with non-urbanized areas being the most affected, with 10.1% prevalence and a prevalence ratio of 1.19 times (95% CI: 1.06–1.33, p = 0.004) more likely to be infected. Other studies have also reported that those living in non-urbanized areas had a higher risk of being HBsAg positive15. Differences in access to information about health services and prevention information, lifestyle, educational level, income, and other socioeconomic status of the population living in non-urbanized areas could help explain the increased prevalence as well as the high risk of HBV in these regions. Therefore, these findings emphasized that national strategies to prevent HBV infection should consider regional differences and demographic/socioeconomic status.
Interestingly, individuals with employment or some monthly income were 2.8 times more likely to contract HBV infection, suggesting that individuals with monthly income or financial power tend to have more than one sexual partner and engage in risky sexual practices which promote the dissemination of infectious agents. The number of sexual partners and its relationship with viral hepatitis was not assessed in the present study and deserves further investigation. Contrary results were observed in a study conducted with blood donors from Somalia, which found that unemployed blood donors (AOR = 3.78, 95% CI: 1.17–12.2), were more likely to become infected with HBV20. On the other hand, and as expected, married individuals were 0.62 times less likely to acquire HBV infections. These results may reflect the involvement of unmarried individuals with casual sexual partners and low use of protective measures during sexual encounters. Different results were observed in studies conducted in Pakistan, which showed that being married was significantly associated with HBV infection21, which can be explained by the shared use of common materials or equipment by the couple during family life, such as sharing personal hygiene items.
Some limitations should be considered in our study. The population of blood donor candidates may not represent the general population of Luanda, as well as the entire population of Angola. Our questionnaire included limited sociodemographic data to investigate risk factors for active HBV infection. We did not include important demographic determinants known to play a crucial role in the spread of viral hepatitis, such as sharing personal hygiene items, medical procedure history, practices associated with drug use, and sexual risk behaviours. Therefore, it is recommended that further studies be conducted to obtain more estimates of HBV infection considering questions that will examine a broader set of determinants related to STIs. Previous studies have also documented that HBV genotype might influence local epidemiology, due to variations in spatial distributions and genotype-specific determinants that affect its transmission potential. Therefore, further studies should investigate HBV genotypes as well as their impact on the increase in active HBV infection cases in Angola. It is also worth mentioning that the HBsAg used in the present study does not detect past infections and/or antibodies resulting from vaccination, suggesting that studies using other markers such as HBcAb (to identify exposure) and HBsAb (to detect immunity) should be performed including individuals HBsAg negative so that we can get a better picture of the HBV seroprevalence in Angola. Despite the weaknesses, our results highlight the growth of active HBV infections in the young Angolan population, which could serve to better understand the socioeconomic impact of STIs, evaluate the success of the HBV vaccination program and ensure targeted intervention in vulnerable populations to prevent new infections in Angola.
Conclusion
In conclusion, we revealed a high active HBV infection (10%) over the past 5 years in the adult population of Luanda, the capital city of Angola. Our findings highlight important epidemiological determinants associated with active HBV infection in the adult population. These findings might contribute to the updating and strengthening of ongoing intervention programs, emphasizing awareness raising for the adoption of safe sexual practices in high-risk populations. Further epidemiological and molecular studies are needed to provide national HBV infection prevalence data to estimate the disease burden and guide public health and vaccination policymakers in Angola.
Data availability
Data is provided within the manuscript. The data supporting this study’s findings are available on request from the corresponding author.
References
Hsu, Y. C., Huang, D. Q. & Nguyen, M. H. Global burden of hepatitis B virus: current status, missed opportunities and a call for action. Nat. Rev. Gastroenterol. Hepatol. 20, 524–537 (2023).
McNaughton, A. L. et al. Hepatitis B virus seroepidemiology data for Africa: modelling intervention strategies based on a systematic review and meta-analysis. PLoS Med. 17, e1003068 (2020).
Ott, J. J., Stevens, G. A., Groeger, J. & Wiersma, S. T. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine 30, 2212–2219 (2012).
Peliganga, L. B., Horta, M. A. P. & Lewis-Ximenez, L. L. Enduring challenges despite progress in preventing mother-to-child transmission of hepatitis B virus in Angola. Pathogens 11, 225 (2022).
Peliganga, L. B. et al. Transfusion transmissible infections in blood donors in the province of Bié, Angola, during a 15-year follow-up, imply the need for pathogen reduction technologies. Pathogens 10, 1633 (2021).
Vueba, A. N., Almendra, R., Santana, P., Faria, C. & Do Céu Sousa, M. Prevalence of HIV and hepatitis B virus among pregnant women in Luanda (Angola): Geospatial distribution and its association with socio-demographic and clinical-obstetric determinants. Virol. J. 18, 239 (2021).
Sebastião, C. S. et al. HIV, hepatitis B virus, hepatitis C virus, and syphilis among pregnant women attending antenatal care in Luanda, Angola: Seroprevalence and risk factors. J. Med. Virol. 92, 3265–3270 (2020).
Guimarães Nebenzahl, H., Lopes, Â., Castro, R. & Pereira, F. Prevalence of human immunodeficiency virus, hepatitis C virus, hepatitis B virus and syphilis among individuals attending anonymous testing for HIV in Luanda, Angola. South. Afr. Med. J. 103, 186 (2013).
Valente, F. et al. Epidemiology and molecular characterization of hepatitis B virus in Luanda, Angola. Mem. Inst. Oswaldo Cruz. 105, 970–977 (2010).
Schweitzer, A., Horn, J., Mikolajczyk, R. T., Krause, G. & Ott, J. J. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet 386, 1546–1555 (2015).
Mak, L. Y. Disease modifiers and novel markers in HBV-related HCC. J. Liver Cancer. https://doi.org/10.17998/jlc.2024.08.03 (2024).
Jandondo, D. et al. Sociodemographic and clinical features related to hepatitis B virus infection among rejected blood donors in Luanda, Angola. Health Sci. Rep. 7, (2024).
Pinto, C. S., Costa, G. B., Allaman, I. B. & Gadelha, S. R. Clinical, epidemiological aspects, and trends of hepatitis B in Brazil from 2007 to 2018. Sci. Rep. 11, 13986 (2021).
World Health Organisation. Consolidated Strategic Information Guidelines For Viral Hepatitis: Planning And Tracking Progress Towards Elimination.https://www.who.int/publications/i/item/9789241515191 (2019).
Muhamad, N. A. et al. Seroprevalence of hepatitis B virus and hepatitis C virus infection among Malaysian population. Sci. Rep. 10, 21009 (2020).
Pereira, L. M. M. B. et al. Population-based multicentric survey of hepatitis B infection and risk factor differences among three regions in Brazil. Am. J. Trop. Med. Hyg. 81, 240–247 (2009).
Wang, S. et al. Epidemiological study of hepatitis B and hepatitis C infections in Northeastern China and the beneficial effect of the vaccination strategy for hepatitis B: a cross-sectional study. BMC Public. Health. 18, 1088 (2018).
Sebastião, C. S., Morais, J. & Brito, M. Factors influencing HIV drug resistance among pregnant women in Luanda, Angola: findings from a cross-sectional study. Trop. Med. Infect. Dis. 6, 29 (2021).
Sebastião, C. S. et al. Genetic diversity and drug resistance of HIV-1 among infected pregnant women newly diagnosed in Luanda, Angola. PLoS One. 14, e0225251 (2019).
Mohamud, A. K., Inchon, P., Suwannaporn, S., Prasert, K. & Dirie, N. I. Assessment of prevalence and risk factors associated with hepatitis B virus infection among blood donors in Mogadishu Somalia. BMC Public. Health. 24, 690 (2024).
Qureshi, H., Bile, K. M., Jooma, R., Alam, S. E. & Afridi, H. U. R. Prevalence of hepatitis B and C viral infections in Pakistan: findings of a national survey appealing for effective prevention and control measures. East Mediterr. Health J. 16(Suppl), S15-23 (2010).
Acknowledgements
We would like to thank the clinical, scientific and technical management of the National Blood Institute for generously granting access to the data for scientific purposes.
Funding
This research was funded by the Fundação Calouste Gulbenkian (FCG), under the ENVOLVE Ciência PALOP program that funded the HITOLA project (Number 250466), Science and Technology Development Project (PDCT) within the scope of the MUTHIVAO project (Number 36 MESCTI/PDCT/2022), FCT MARVEL (PTDC/SAU-PUB/4018/2021), FCT GHTM-UID/04413/2020 and LA-REAL-LA/P/0117/2020.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.G.M., A.A., and C.S.S.; methodology, M.G.M., A.A., and C.S.S; software, C.S.S; validation, C.S.S; formal analysis, V.P. and C.S.S; investigation, M.G.M., J.V., F.C., A.A., M.L.S.S., J.M.K.S, and C.S.S.; resources, C.S.S; data curation, V.P. and C.S.S.; writing—original draft preparation, C.S.S.; writing—review and editing, V.P. and C.S.S.; visualization, C.S.S.; supervision, C.S.S.; project administration, E.M., D.M., and C.S.S; funding acquisition, C.S.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics declarations
The need for informed consent to participate was waived by an Institutional Review Board (IRB), with official letter number 428/GDG/INS/2024, approved on March 7th, 2024.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sebastião, C.S., Machado, M.G., Vigário, J. et al. Trends in active hepatitis B virus infection and associated risk factors among blood donor candidates from Luanda, Angola. Sci Rep 15, 16478 (2025). https://doi.org/10.1038/s41598-025-01089-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01089-w