Abstract
This study aimed to explore the association between physical activity (PA) and the risk of Overactive Bladder (OAB) in American adults. This analysis comprises a cross-sectional study of comprehensive population data collected from the National Health and Nutrition Examination Surveys spanning the years 2007 to 2018. Adults were categorized into four PA patterns (inactive, insufficiently active, weekend warrior, and regularly active) based on self-reported PA levels. We employed a weighted logistic regression model, restricted cubic spline (RCS) analysis, and subgroup analyses to investigate the relationship between PA patterns and OAB. This research included 17,050 subjects. After thorough adjustments for covariates, multivariate logistic regression models revealed that weekend warrior, and regularly active adults had a reduced risk of OAB compared with inactive adults, with odds ratios (ORs) of 0.96 (95% CI 0.94, 0.98), and 0.97 (95% CI 0.95, 0.99), respectively. RCS analysis revealed a nonlinear relationship between total weekly PA duration (in minutes) and the incidence of OAB, with approximately 915.41 min of total PA duration (minutes per week) associated with the lowest risk of OAB. This study demonstrated that adults engaging in either the regularly active or weekend warrior patterns experienced a lower risk of OAB compared to inactive adults. PA could be considered as part of a broader strategy for OAB prevention.
Similar content being viewed by others
Introduction
Overactive bladder (OAB) is a urological issue marked by a sudden urge to urinate, often with increased nighttime urination and frequent urination, but without signs of a urinary tract infection or other clear health problems1,2. Over the last 40 years, studies in European countries have shown that OAB affects 13.4% of men and 14.6% of women3. OAB can greatly affect a person’s quality of life, especially with urgent urination impacting work productivity and social activities4. In the United States, OAB leads to billions of dollars in medical costs each year5. In clinical settings, the management of OAB emphasizes long-term, comprehensive treatment plans designed to alleviate symptoms. Currently, OAB is treated using various methods, such as drug therapy and behavioral therapy; however, further research is still needed to fully understand its effectiveness5,6.
Past research has found many possible risk factors for OAB, such as urinary tract infections, chronic illnesses, and mental health issues like sleep problems and depression7,8. The public widely acknowledges the health benefits of physical activity (PA). The World Health Organization (WHO) advises adults aged 18–64 to engage in at least 150 min per week of moderate-intensity aerobic activity, or at least 75 min per week of vigorous-intensity aerobic activity, or a combination of both that equates to the same level of exertion9. Several studies have reported that PA significantly reduced the risk of OAB10,11,12. However, we still lack a full understanding of the precise connection between PA and the risk of developing OAB. Similarly, no studies have focused on the impact of the duration and patterns of PA (both in terms of duration and frequency) on OAB. Consequently, the duration and patterns of physical activity that provide the greatest health benefits remain uncertain. A growing number of studies have explored the associations between physical activity (PA) patterns and disease risks13,14. These studies have shown that adults who engage in either a regularly active pattern or a weekend warrior pattern experience lower disease risks compared to inactive adults. Given our busy lifestyles, there is an urgent need to investigate the impact of PA duration and patterns on OAB and, potentially, to develop PA recommendations for adults who have limited time for exercise.
Therefore, the aim of the current study was to investigate the associations between the duration and patterns of PA and the risk of OAB among US adults, utilizing data from the National Health and Nutrition Examination Survey (NHANES).
Materials and methods
Data sources and participants
This research utilized data from the NHANES cycles spanning from 2007 to 2018, a recurring survey project designed to assess the health and nutritional status of U.S. residents. Annually, NHANES gathers comprehensive health and nutrition-related data from approximately 5000 Americans, covering demographics, socioeconomic status, dietary habits, and overall health conditions (https://www.cdc.gov/nchs/nhanes/index.htm). Only publicly accessible data were used in this analysis, thus eliminating the need for ethical approval.
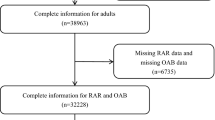
The participant selection process was meticulously defined to ensure the study sample’s representativeness. The initial cohort comprised 59,842 individuals. Inclusion criteria focused on adults aged 20 and older, in line with our study objectives. Exclusion criteria were systematically applied, resulting in the exclusion of individuals under 20 years old, those with missing data on OAB, those lacking data on physical activity, and those without significant covariate information. After applying these criteria, 17,050 participants were deemed eligible and included in the final analysis (Fig. 1). Notably, since questionnaires regarding OAB were restricted to adults aged 20 and older, only this age group was included in the final sample.
Diagnosis of overactive bladder
Based on previous study15, the Overactive Bladder Symptom Score (OABSS) was utilized to measure OAB16. A participant was classified as experiencing OAB if they had an OABSS of 3 or higher. In this study, OAB was defined by the concurrent presence of urinary frequency, urge urinary incontinence (UUI), and nocturia.
Trained research staff conducted face-to-face interviews to administer questionnaires, from which all information for diagnosing OAB was derived. To evaluate UUI, participants were asked: “During the past 12 months, have you leaked or lost control of even a small amount of urine with an urge or pressure to urinate and you couldn’t get to the toilet fast enough?”. The severity of UUI was assessed with the question: “How frequently does this occur?”. Regarding nocturia, participants were asked: “During the past 30 days, how many times per night did you most typically get up to urinate, from the time you went to bed at night until the time you got up in the morning?”. The responses were used to score the nocturia component of the OAB assessment.
Physical activity
In this study, participants self-reported their frequency and duration of leisure-time physical activity (PA) using the Global Physical Activity Questionnaire (GPAQ), unless otherwise noted. The GPAQ has been proven reliable for gathering information on daily moderate-intensity PA (MPA) and vigorous-intensity PA (VPA) engaged in for at least 10 continuous minutes during leisure time, work, or transportation, across a typical week. According to PA guidelines, one minute of vigorous-intensity activity is considered equivalent to 2 min of moderate-intensity activity17. In this study, PA patterns were calculated using a combination of frequency (number of sessions per week) and duration (length of each session). The total PA duration (minutes per week) was calculated as follows: 2 *vigorous PA + moderate PA. We then categorized total PA into four patterns: inactive (total PA duration = 0 min), insufficiently active (total PA duration < 150 min), weekend warrior (at least 150 min of total PA duration concentrated in 1 or 2 sessions), and regularly active (at least 150 min of total PA duration spread across more than 2 sessions)14.
Covariates
Based on previous studies15,18, the covariates in this study encompassed demographic data, lifestyle factors, and health status. These included age (< 25 years, 25–29.99 years, ≥ 30 years), gender (male, female), race (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian, Other Race), education level (Less than 9th grade, 9–11th grade/GED, High school graduate/GED, Some college or AA degree, College graduate or above), poverty income ratio (PIR)(< 1.3, 1.3–3.5, > 3.5),smoke (Yes, No), Alcohol user (Yes, No), Body mass index (BMI) (< 25.0 kg/m2, 25–29.99 kg/m2, ≥ 30 kg/m2), Hypertension (Yes, No), Diabetes (Yes, No, Borderline).
Statistical analysis
In accordance with the analytic guidelines issued by the National Center for Health Statistics, the appropriate survey weight was utilized to guarantee representativeness of the U.S. population. Given that six consecutive cycles were sourced from NHANES, the sample weights for a 2-year period were divided by six to ensure they were representative of the general population. Continuous variables are presented as the mean ± standard error, whereas categorical variables are presented as frequencies (percentages). Differences between groups for continuous variables were assessed using the weighted t-test, and differences for categorical variables were evaluated using the chi-square test (χ2), respectively.
To account for potential confounding variables, multivariate logistic regression analyses were conducted, both with and without adjustments for these variables, to further investigate the association between PA patterns and OAB. The crude model did not include any adjustments. Model 1 was adjusted for age, gender, race, education levels, and PIR. Model 2 incorporated all adjustments in Model 1, as well as BMI, smoke, alcohol user, hypertension, and diabetes. Additionally, Restricted Cubic Spline (RCS) regression models were employed to examine the dose–response relationship between total PA duration and OAB risk. Subgroup analyses were conducted to ensure the generalizability of the results across various subgroup populations.
All the statistical analyses were performed using R software (version 4.0.3). All p values were considered two-sided, and a p value < 0.05 indicated statistical significance.
Results
Participant characteristics
The present study included a total of 17,050 participants sourced from the NHANES. The characteristics of the study population, stratified by the presence of OAB, are detailed in Table 1. Statistically significant differences (p < 0.05) were observed across all indicators between the two groups. Specifically, participants diagnosed with OAB, in comparison to those without OAB, exhibited the following characteristics: a higher age, a preponderance of females, a greater proportion of non-Hispanic black ethnicity, a lower educational attainment, a lower poverty rate, a tendency towards smoking, an absence of alcohol consumption, a higher BMI, reduced levels of physical activity, and a heightened likelihood of suffering from hypertension and diabetes.
Association between PA and OAB
Table 2 demonstrates a negative correlation between PA and the risk of OAB. The crude model, as well as Models 1 to 2, exhibited consistent results. Additionally, the p-value for the trend analysis was less than 0.05 in all models. In Model 2, after comprehensive adjustments for covariates, the multivariate logistic regression models indicated that adults who were insufficiently active, weekend warriors (those who engage in substantial physical activity only on weekends), and regularly active had a decreased risk of OAB compared to inactive adults. It is noteworthy that the association between PA and OAB was significant in all groups with p < 0.05. Specifically, the odds ratios (ORs) were 0.98 (95% CI 0.95, 1.00) for insufficiently active adults, 0.96 (95% CI 0.94, 0.98) for weekend warriors, and 0.97 (95% CI 0.95, 0.99) for regularly active adults. Furthermore, as described in the Fig. 2, RCS analysis revealed a nonlinear relationship between low total PA duration (minutes per week) and OAB risk (P < 0.001). The curve initially showed a downward trend in OAB risk with increasing PA duration, reaching a nadir at approximately 915.41 min/week, followed by a slight upward trend at higher durations. However, the clinical relevance of this threshold is uncertain due to the small effect sizes observed in our study (ORs 0.96–0.98), and these findings should be interpreted as exploratory.
Subgroup and sensitivity analysis
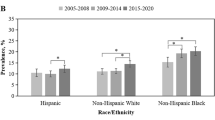
We performed subgroup analyses to explore the potential association between PA patterns and the risk of OAB in different populations based on age, gender, race, education level, PIR, smoke, alcohol user, BMI, hypertension, diabetes. The findings depicted in Table 3 show that this association was influenced by gender and PIR (P < 0.05). Notably, as shown in Fig. 3, both weekend warriors and regularly active groups showed a reduced incidence of OAB compared to inactive female in the gender subgroup.
To address potential reverse causation, we further stratified participants by OAB severity (mild: OABSS < 6; moderate-severe: OABSS ≥ 6). As shown in supplementary table 1, the inverse association between weekend warrior PA and OAB risk remained statistically significant in the mild subgroup (OR 0.96, 95% CI 0.94–0.99; p = 0.001), whereas no significant association was observed in moderate-severe cases (p > 0.9).
Discussion
This study innovatively examines the correlation between PA and OAB using a cross-sectional analysis. Our weighted multivariate logistic regression analysis shows that PA patterns are associated with OAB risk, even after accounting for all covariates. The RCS curve illustrates a nonlinear dose–effect relationship between total PA duration (minutes per week) and OAB. In summary, adults who engage in PA on weekends (weekend warriors) and those who maintain regular activity (regularly active) have a lower risk of OAB compared to inactive adults. While these effect sizes are small, they may hold public health relevance given the high prevalence of OAB (13.4% in European men and 14.6% in women) and the potential for PA to synergize with other lifestyle interventions. Notably, in the prediabetes subgroup, weekend warrior PA was associated with a 14% risk reduction (OR = 0.86) after full adjustment, highlighting potential amplified benefits in high-risk populations.
“Weekend warriors” refer to individuals who engage in physical activity predominantly on weekends, often in concentrated sessions to meet the weekly recommended PA duration. “Regularly active individuals” are those who spread their physical activity throughout the week, maintaining a consistent and regular exercise routine14.
PA and OAB are closely linked, with numerous studies exploring various facets of this relationship. Most of these studies have reported the protective role of PA. Chu et al.11 concentrated on the impact of OAB treatment on PA limitations in women, demonstrating potential improvements following therapy. Hakimi et al.19 investigated risk factors for OAB syndrome in menopausal women and their relationship to sexual function, also uncovering physical inactivity among those with OAB syndrome20. Chu et al.21 studied the short-term effect of fesoterodine on physical function related to fall risk in older women with OAB, emphasizing the significance of considering physical function in treatment plans. Senel et al.22 examined the impact of total knee arthroplasty on OAB symptoms in female patients and suggested that total knee arthroplasty may lead to symptomatic improvement post-surgery. Collectively, these studies contribute to our understanding of the relationship between PA and OAB, underscoring the importance of tailored treatment approaches for this condition. However, little is known about how the frequency of meeting the recommended weekly duration of PA and PA patterns influence OAB risk. To the best of our knowledge, our study is the first to investigate the association between weekly PA duration and PA patterns (e.g., weekend warriors and regularly active individuals) and OAB in American adults. Our results indicate that weekend warriors and regularly active adults have a reduced risk of OAB compared with inactive adults. This suggests that individuals with time constraints may still benefit from PA engagement, even if concentrated on weekends. Additionally, the RCS curve suggests a nonlinear relationship between total PA duration and OAB risk, with the lowest risk observed at ~ 915.41 min/week. While this pattern aligns with our hypothesis that excessive PA duration may not confer additional benefits, the modest effect sizes and observational design preclude definitive conclusions about the clinical utility of this threshold. Importantly, this exploratory analysis supports our rationale for investigating PA patterns (e.g., weekend warriors) rather than focusing solely on total duration. Further studies are needed to validate whether such a threshold exists and whether it reflects biological plausibility or confounding factors.
Several hypotheses have been proposed to highlight the beneficial effects of PA in alleviating OAB symptoms. Various studies have explored the relationship between obesity and OAB15,23,24. PA is considered a vital strategy for combating obesity. Leiria et al.25 examined the influence of insulin resistance on bladder function in the context of obesity-related OAB. They found that insulin relaxes the bladder through the activation of the PI3K/AKT/eNOS pathway in the mucosa, with impaired insulin action contributing to bladder dysfunction in obese individuals26. Research has demonstrated that PA has a significant impact on insulin levels and insulin sensitivity across diverse populations27,28. Studies indicate that oxidative stress can induce bladder hyperactivity and dysfunction, resulting in OAB symptoms29,30,31. PA may affect the occurrence and development of disease by affecting inflammation and oxidative stress32,33. Additionally, PA may improve OAB symptoms by affecting conditions associated with OAB, such as depression34,35.
Subgroup analysis and interaction analysis showed that the relationship between PA patterns and the risk of OAB remained consistent across most demographic characteristics, body mass index BMI levels, lifestyle habits, and health status. It is noteworthy that in the gender subgroup, we only found a negative correlation between physical activity patterns and OAB risk in women, but not in men. Given that OAB symptoms are most prevalent in women36, our findings are important in guiding people with OAB to improve their symptoms through exercise. Several factors may contribute to this gender difference, including physiological differences in urethral length and angle, hormonal influences, and gender-specific behaviors related to PA. These findings have important clinical implications, as they suggest that promoting PA among female patients may be associated with reduced OAB risk. However, it is important to note that our study was observational, and thus cannot establish causality. Further research, including randomized controlled trials, is needed to confirm these findings and explore the mechanisms underlying the gender-specific effects of PA on OAB risk. Our study found that PA significantly was associated with reduced OAB risk, with an interaction observed between this association and PIR. Despite the interaction, the inverse relationship between PA and OAB risk remained significant across all PIR subgroups. This interaction may reflect differences in access to physical activity resources or underlying OAB etiology across PIR levels. Future research should explore these potential mechanisms and develop interventions tailored to different economic strata to maximize the benefits of PA in reducing OAB risk.
Our research boasts numerous advantages. Firstly, we utilized a large sample from the NHANES database, enhancing the reliability and generalizability of our findings across diverse populations. Secondly, our study is the first to investigate the relationship between the duration and pattern of PA and the development of OAB. Thirdly, after adjusting for potential confounding factors, the results from various models and subgroup analyses demonstrated a strong correlation between PA and OAB. However, it is important to acknowledge some limitations of our study. As a cross-sectional analysis of retrospective NHANES data, it cannot establish causality. Reverse causation—where OAB symptoms (e.g., urinary incontinence) may reduce PA participation—is a critical concern. To address this, we stratified participants by OAB severity (mild: OABSS < 6; moderate-severe: OABSS ≥ 6) and found that the inverse association between weekend warrior PA and OAB risk persisted only in the mild subgroup, whereas no association was observed in moderate-severe cases. This divergence suggests that individuals with mild symptoms are less likely to limit PA, whereas those with severe symptoms may reduce PA due to symptom burden, thereby attenuating the observed relationship. Additionally, there may be unmeasured or residual confounding factors. Furthermore, all participants in the study were from the United States, which may limit the generalizability of our findings to other populations.
Conclusion
Weekend warriors and adults who were regularly active had a lower risk of OAB compared with inactive adults who did not engage in such activities. These results suggest that adherence to PA recommendations may be associated with reduced OAB risk, and PA could be considered as part of a broader strategy for OAB prevention. Further research is needed to clarify causality and clinical relevance.
Data availability
In this study, publicly accessible datasets were analyzed. These datasets can be obtained from: www.cdc.gov/nchs/nhanes/.
References
White, N. & Iglesia, C. B. Overactive bladder. Obstet. Gynecol. Clin. North Am. 43, 59–68 (2016).
Przydacz, M., Golabek, T., Dudek, P., Lipinski, M. & Chlosta, P. Prevalence and bother of lower urinary tract symptoms and overactive bladder in Poland, an Eastern European Study. Sci. Rep. 10, 19819 (2020).
Irwin, D. E. et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur. Urol. 50, 1306–1314 (2006).
Sexton, C. C. et al. Impact of overactive bladder on work productivity in the United States: Results from EpiLUTS. Am. J. Manag. Care 15, S98–S107 (2009).
Hu, T.-W. et al. Estimated economic costs of overactive bladder in the United States. Urology 61, 1123–1128 (2003).
El-Zawahry, A. Combination pharmacotherapy for treatment of overactive bladder (OAB). Curr. Urol. Rep. 20, 33 (2019).
Coyne, K. S. et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: Results from the epidemiology of LUTS (EpiLUTS) study. BJU Int. 104, 352–360 (2009).
Zhang, Y. et al. Association between overactive bladder and depression in American adults: A cross-sectional study from NHANES 2005–2018.
Global Recommendations on Physical Activity for Health. (World Health Organization, Geneva, 2010).
de Oliveira, A. M. et al. Physical activity effects on bladder dysfunction in an obese and insulin-resistant murine model. Physiol. Rep. 9, e14792 (2021).
Chu, C. M., Harvie, H. S., Smith, A. L., Arya, L. A. & Andy, U. U. The impact of treatment of overactive bladder on physical activity limitations. J. Womens Health (Larchmt) 25, 801–805 (2016).
Coyne, K. S. et al. The impact of OAB on physical activity in the United States: Results from OAB-POLL. Urology 82, 799–806 (2013).
Mahe, J. et al. Association between weekend warrior physical activity pattern and all-cause mortality among adults living with type 2 diabetes: A prospective cohort study from NHANES 2007 to 2018. Diabetol. Metab. Syndr. 16, 226 (2024).
Chen, R. et al. Weekend warrior physical activity pattern is associated with lower depression risk: Findings from NHANES 2007–2018. Gen. Hosp. Psychiatry 84, 165–171 (2023).
Shang, Y., Chen, J. & Tai, Y. Association between weight-adjusted waist index and overactive bladder syndrome among adult women in the United States: A cross-sectional study. BMC Womens Health 24, 488 (2024).
Blaivas, J. G., Panagopoulos, G., Weiss, J. P. & Somaroo, C. Validation of the overactive bladder symptom score. J. Urol. 178, 543–547 (2007).
The Physical Activity Guidelines for Americans—PubMed. https://pubmed.ncbi.nlm.nih.gov/30418471/.
Zhang, Y. et al. Association between body roundness index and overactive bladder: Results from the NHANES 2005–2018. Lipids Health Dis. 23, 184 (2024).
Hakimi, S., Aminian, E., Alizadeh Charandabi, S. M., Bastani, P. & Mohammadi, M. Risk factors of overactive bladder syndrome and its relation to sexual function in menopausal women. Urologia 85, 10–14 (2018).
Risk factors of overactive bladder syndrome and its relation to sexual function in menopausal women—PubMed. https://pubmed.ncbi.nlm.nih.gov/29619902/.
Chu, C. M., Harvie, H., Arya, L. A. & Andy, U. U. Short-term effect of fesoterodine on physical function relevant to fall risk in older women with overactive bladder. Female Pelvic Med. Reconstr. Surg. 27, 759–765 (2021).
Senel, C., Kizilay, Y. O., Turan, K., Ongun, S. & Tuzel, E. Does total knee arthroplasty affect overactive bladder symptoms in female patients?. Int. Urogynecol. J. 33, 939–945 (2022).
Association between weight-adjusted waist index and overactive bladder: a cross-sectional study based on 2009–2018 NHANES—PubMed. https://pubmed.ncbi.nlm.nih.gov/39296511/.
Lai, H. H. et al. Relationship between central obesity, general obesity, overactive bladder syndrome and urinary incontinence among male and female patients seeking care for their lower urinary tract symptoms. Urology 123, 34–43 (2019).
Leiria, L. O. et al. Insulin relaxes bladder via PI3K/AKT/eNOS pathway activation in mucosa: Unfolded protein response-dependent insulin resistance as a cause of obesity-associated overactive bladder. J. Physiol. 591, 2259–2273 (2013).
Insulin relaxes bladder via PI3K/AKT/eNOS pathway activation in mucosa: unfolded protein response-dependent insulin resistance as a cause of obesity-associated overactive bladder—PubMed. https://pubmed.ncbi.nlm.nih.gov/23478138/.
Borghouts, L. B. & Keizer, H. A. Exercise and insulin sensitivity: A review. Int. J. Sports Med. 21, 1–12 (2000).
MacGregor, K. A., Gallagher, I. J. & Moran, C. N. Relationship between insulin sensitivity and menstrual cycle is modified by BMI, fitness, and physical activity in NHANES. J. Clin. Endocrinol. Metab. 106, 2979–2990 (2021).
Wu, Y.-H. et al. Bladder hyperactivity induced by oxidative stress and bladder ischemia: A review of treatment strategies with antioxidants. Int. J. Mol. Sci. 22, 6014 (2021).
Fridovich, I. Superoxide anion radical (O2-.), superoxide dismutases, and related matters. J. Biol. Chem. 272, 18515–18517 (1997).
Akin, Y. et al. Impact of rho-kinase inhibitor hydroxyfasudil in protamine sulphate induced cystitis rat bladder. Low Urin. Tract. Symp. 7, 108–114 (2015).
Tian, D. & Meng, J. Exercise for prevention and relief of cardiovascular disease: Prognoses, mechanisms, and approaches. Oxid. Med. Cell Longev. 2019, 3756750 (2019).
El Assar, M., Álvarez-Bustos, A., Sosa, P., Angulo, J. & Rodríguez-Mañas, L. Effect of physical activity/exercise on oxidative stress and inflammation in muscle and vascular aging. Int. J. Mol. Sci. 23, 8713 (2022).
Ryan, M. P. The antidepressant effects of physical activity: Mediating self-esteem and self-efficacy mechanisms. Psychol. Health 23, 279–307 (2008).
Euteneuer, F. et al. Immunological effects of behavioral activation with exercise in major depression: An exploratory randomized controlled trial. Transl. Psychiatry 7, e1132 (2017).
Nambiar, A. K. et al. European association of urology guidelines on the diagnosis and management of female non-neurogenic lower urinary tract symptoms. Part 1: Diagnostics, overactive bladder, stress urinary incontinence, and mixed urinary incontinence. Eur. Urol. 82, 49–59 (2022).
Author information
Authors and Affiliations
Contributions
T. W. and B.X. designed the study, collected and preprocessed NHANES data, conducted statistical analyses, and drafted the manuscript. T. W. led the research team, coordinated tasks, revised the manuscript for clarity and journal guidelines, and handled communication with edit. All authors approved the final manuscript and declare no competing interests.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study used publicly available NHANES data with anonymized participant information. Ethical approval was not required as participants had previously provided informed consent for their data to be used in research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, T., Xu, B. The relationship between physical activity and overactive bladder among American adults: a cross-sectional study from NHANES 2007–2018. Sci Rep 15, 16280 (2025). https://doi.org/10.1038/s41598-025-01272-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01272-z