Abstract
Lenke type 1 adolescent idiopathic scoliosis (AIS) is characterized by a structural main thoracic (MT) curve and a non-structural proximal thoracic (PT) curve. Accurate prediction of postoperative PT curve correction is crucial for achieving optimal surgical outcomes, including postoperative shoulder balance. This study aimed to determine which preoperative lateral bending and traction radiographs are most appropriate for assessing spontaneous postoperative PT curve correction. Fifty-five patients with Lenke type 1 AIS who underwent PSF between January 2006 and January 2020 were included. Preoperative curve flexibility was assessed using side-bending (SB), fulcrum-bending (FB), and traction (TR) radiographs. Radiographic measurements were conducted preoperatively, immediately postoperatively, and at the 2-year follow-up. The average preoperative Cobb angles for PT, main thoracic (MT), and thoracolumbar/lumbar (TL/L) curves were 24.7°, 53.5°, and 32.4°, respectively. SB radiographs demonstrated a significant correlation with 2-year postoperative PT Cobb angles (r = 0.526, p < 0.001), with no significant difference between preoperative SB measurements and actual 2-year postoperative outcomes (mean difference − 0.03°; 95%CI − 1.57 to 1.49; p = 0.88). FB radiographs accurately reflected MT correction but overestimated PT correction (mean difference 2.29°; 95%CI − 0.51 to 5.10; p = 0.11), while TR radiographs underestimated PT correction. These results indicate that SB radiographs can be used as a reliable reference for estimating postoperative spontaneous PT curve correction in Lenke type 1 AIS.
Similar content being viewed by others
Introduction
Lenke type 1 adolescent idiopathic scoliosis (AIS) has a structural main thoracic (MT) curve with a non-structural compensatory proximal thoracic (PT) curve and a thoracolumbar or lumbar (TL/L) curve1, which is the most frequently prevalent curve type in operative AIS2. In principle, spinal fusion for Lenke type 1 curves includes structural MT curves, but not non-structural PT curves1. In other words, surgeons cannot directly control the PT curve during surgery for Lenke type 1 curves.
Residual PT curves after spinal fusion for MT curves can affect surgical outcomes such as postoperative pulmonary function and shoulder balance. Newton et al. reported that the PT curve is associated with preoperative pulmonary dysfunction3. Regarding postoperative shoulder balance, overcorrection of MT curves relative to simultaneous correction of PT curves results in shoulder height imbalance4,5. Therefore, it is essential to predict spontaneous correction of PT curves after spinal fusion of MT curves in patients with Lenke type 1 AIS curves.
In the preoperative assessment of curve flexibility, active side-bending (SB) radiographs are usually used to determine the curve type of the Lenke classification and the fusion area1, and to predict postoperative correction4,5. In contrast, fulcrum-bending (FB), which is performed with patients bent over a fulcrum in the lateral position, has been reported to exhibit higher spinal flexibility than SB radiographs6,7. Additionally, FB radiographs can more accurately predict postoperative correction with modern spinal instruments such as pedicle screws8,9,10. FB correction approximates the postoperative curve correction for both PT and MT curves in patients with Lenke type 2 (double-thoracic curve type) AIS, in which both PT and MT curves are generally included in the instrumented fusion area11. In contrast, the prediction of postoperative spontaneous correction of non-structural unfused curves is challenging. Kirk et al. reported that supine traction (TR) radiographs demonstrated greater flexibility in the PT curve than SB radiographs in patients with double-thoracic curves12. In contrast, SB radiographs can predict postoperative spontaneous correction of PT curves8,13. However, because these studies included patients with heterogeneous curve types and upper instrumented vertebral (UIV) levels, these results cannot be simply applied to postoperative spontaneous correction of PT curves in patients with Lenke type 1 AIS. We, therefore, aimed to evaluate the ability of SB, FB, and TR radiographs to assist in the prediction of spontaneous correction of PT curves in patients with Lenke type 1 AIS undergoing posterior spinal fusion (PSF) of the MT region.
Methods
All methods were performed in accordance with the relevant guidelines and regulations. This retrospective single-center cohort study was approved by the Institutional Review Board of Niigata University (approval number: 2015-1385). All patients and their guardians provided written or opt-out informed consent prior to participation in the study. Seventy-one consecutive patients with Lenke type 1 AIS underwent PSF with pedicle screw constructs at our institution between January 2006 and January 2020. Of these, we included 55 patients with UIV levels between one proximal and distal vertebra relative to the upper end vertebra (UEV) of the MT curve. All patients included in this study were preoperatively assessed for flexibility of PT and MT curves using SB, FB, or TR radiographs. There were missing FB radiograph data of the PT curves in eight patients, missing FB radiographs of the MT curve in one patient, and missing TR radiographs in one patient. A minimum 2-year follow-up period was completed for all patients.
Radiographic examination
Standing whole-spine posteroanterior and lateral radiographs were obtained preoperatively, directly postoperative (1–2 months after surgery), and at the 2 years postoperatively (PO2Y). For the preoperative evaluation of curve flexibility, right and left SB and TR radiographs were obtained in the supine position. Additionally, FB radiographs for both the PT and MT curves were obtained under the direction of an attending surgeon, according to a previously published method in which the patient was asked to lie sideways over a radiolucent plastic cylinder placed under the rib corresponding to the apex of the curve (Fig. 1)11. To assess curve flexibility and correction rate, the following formulas were used:
A 17-year-old female patient with Lenke type 1 adolescent idiopathic scoliosis. (a) Standing posteroanterior radiographs before surgery. (b) Active side-bending radiographs. (c) Fulcrum-bending radiographs. (d) Traction-bending radiographs. (e) Standing posteroanterior radiographs at the 1-month follow-up. (f) Standing posteroanterior radiographs at the 2 years follow-up.
All radiographic measurements were performed by the first author, a board-certified spine surgeon.
Surgical procedure
The UIV level was determined between one proximal and distal vertebrae relative to the UEV of the MT curve. Conversely, the lower instrumented vertebral (LIV) level was selected according to the last-touching vertebra concept for selective thoracic fusion14 and characteristics of non-structural TL/L curve, including curve magnitude and its ratio compared to the MT curve15. Segmental pedicle screw constructs were used bilaterally. In 13 patients, hooks were used as UIV instruments because of narrow or no cancellous pedicle channels.
Routine posterior release, including resection of the spinous and inferior articular processes, was performed in the fused area. When the MT curve was rigid or > 30° on the FB radiograph, multilevel Ponte osteotomies (Schwab grade 2) were performed. Then, a 5.5-mm-diameter cobalt-chromium rod or titanium alloy rod contoured to the hyperkyphotic thoracic spine was placed on the concave side of the MT curve, applying translational force using multiple approximators or the rod rotation maneuver technique. If necessary, Scoliosis was additionally corrected using an in situ bending technique. A convex rod contoured to the hypokyphotic thoracic spine was then applied (differential rod contouring technique), followed by direct vertebral derotation in the MT curve. Finally, compression or distraction forces were applied between the pedicle screws to level the shoulder asymmetry and LIV. Bone transplantation was performed over the fusion area using local autogenous bone tips mixed with beta-tricalcium phosphate granules.
Statistical analysis
Statistical analyses were performed using GraphPad Prism (Version 6, San Francisco, La Jolla, CA). Data normality was evaluated using the Shapiro–Wilk test. Paired t-tests were used to compare the pre- and postoperative radiographic parameters when normality was confirmed. The Wilcoxon signed-rank test for paired samples was used for non-normally distributed data. For correlation analysis between preoperative and postoperative radiographic parameters, Pearson’s correlation coefficient (r) and Spearman’s rank correlation coefficient (ρ) were used for normally and non-normally distributed data, respectively. A correlation coefficient with an absolute value of at least 0.3 and p < 0.05 was considered statistically significant.
Results
Patient demographics
Patient characteristics are shown in Table 1. The average age at the time of surgery was 15.6 years (range, 12–24 years), including 3 male and 52 female patients. Lumbar modifiers A, B, and C were administered to 37, 6, and 12 patients, respectively. The Risser grades at the time of surgery were 1, 2, 3, 4, and 5 in patients 1, 3, 3, 38, and 10, respectively. UIV was selected as T3, T4, T5, T6, and T7 in 2, 33, 15, 4, and 1 patient(s), respectively. The LIV was selected as T11, T12, L1, L2, L3, and L4 in 1, 9, 14, 18, 12, and 1 patient(s), respectively. Ponte osteotomy of the MT curve was performed in 13 patients. One patient who underwent fusion to L4 had initially received a selective thoracic fusion with LIV at T12. However, due to distal adding-on observed during follow-up, a revision surgery was performed, extending the instrumentation to L4.
Radiological assessments of curve flexibility and postoperative curve correction
The preoperative and postoperative radiographic data are shown in Table 2. The mean preoperative Cobb angles for the PT, MT, and TL/L curves were 24.7°, 53.5°, and 32.4°, respectively. On SB radiographs, the PT, MT, and TL/L curves were corrected to 16.4° (mean SB flexibility, 32.3%), 27.0° (49.2%), and 3.5° (97.1%), respectively. On the FB radiographs, the PT and MT were corrected to 14.3° (mean FB flexibility, 34.3%) and 18.7° (65.3%), respectively. On the TR radiographs, the PT, MT, and TL/L curves were corrected to 21.1° (mean TR flexibility, 4.5%), 32.6° (38.5%), and 18.0° (44.6%), respectively.
Directly postoperative radiographs demonstrated significant curve corrections in all curve regions; the mean Cobb angles decreased to 16.4° (correction rate, 28.5%) in the PT curve, 18.9° (64.4%) in the MT curve, and 11.3° (65.5%) in the TL/L curve (p < 0.001 for all). Curve corrections were maintained at the 2-year follow-up for the PT (16.3°, p = 0.92) and TL/L curves (12.2°, p = 0.28). In contrast, MT curve magnitude statistically significantly increased to 21.1° (p = 0.012), with a mean correction loss of 2.05° (95% confidence interval CI 0.49–3.61). The correction rates at the 2-year follow-up were 24.8%, 60.6%, and 64.4% in the PT, MT, and TL/L curves, respectively.
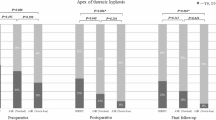
Comparisons between preoperative and 2-year postoperative thoracic curves
The results of the comparisons between the preoperative and postoperative curve corrections are shown in Table 3. The mean Cobb angle of the PT curve at 2 years after surgery was significantly larger than that in the FB radiograph (p = 0.03) and significantly smaller than that in the TR radiograph (p < 0.01); there was no significant difference in the mean Cobb angle of the PT curve between the 2-year postoperative and SB radiographs, with a mean difference of − 0.03° (p = 0.88; 95%CI − 1.57° to 1.49°). Regarding the MT curve, the mean Cobb angle 2 years after surgery did not differ from that on FB radiography, with a mean difference of 2.29° (p = 0.11; 95%CI − 0.51° to 5.10°), whereas it was significantly smaller than that on SB and TR radiographs (p < 0.001 for both). Correction rates 2 years postoperatively did not differ from SB (p = 0.52) and FB flexibilities (p = 0.20) in the PT curve but did not differ from FB flexibility (p = 0.086) in the MT curve.
Correlations between the preoperative and 2-year postoperative Cobb angles are shown in Table 4. The PT curve magnitude at the 2-year follow-up was significantly and positively correlated with those in the SB (r = 0.526, p < 0.001) and TR radiographs (r = 0.493, p < 0.001), but not significantly correlated with those in the FB radiographs. In contrast, the Cobb angles of the MT curve at the 2-year follow-up were not significantly correlated with those on any of the preoperative radiographs.
Evaluation of statistical power
A post hoc power analysis was used to evaluate the statistical power for detecting a clinically significant difference of 3° in the Cobb angle of the PT curve between preoperative SB radiographs and 2-year postoperative measurements using a paired t-test. The threshold of 3° was selected based on previous studies16,17,18, which commonly reported measurement errors of approximately 3° for Cobb angle assessment. The effect size (d) was calculated as 0.528 with 55 cases, a standard deviation of 5.7° for the differences, and a significance level of α = 0.05. Furthermore, the resulting power (1 − β) was approximately 0.86, indicating sufficient power to detect the predefined difference.
Subgroup analysis with confounding factors
We performed a subgroup analysis to evaluate potential confounding factors (Table 5). Patients were categorized by age into the ≤ 18-year-old (n = 7) and ≥ 19-year-old (n = 48) groups. For Risser grade, patients were categorized into Risser 1–3 (n = 7) and 4–5 (n = 48) groups. Additionally, patients were classified based on the level of UIV into those with UEV or UEV + 1 (one distal vertebra) (n = 30) and UEV-1 (one proximal vertebra) (n = 25). Regarding the level of LIV, patients were categorized into L2 or above (n = 42) and L3 or below (n = 13) groups. When comparing the PT curve magnitude between preoperative SB and 2-year postoperative radiographs, no significant differences were found across all subgroups. The PT curve magnitude of TR radiograph was significantly larger than that of 2-year postoperative radiograph across all subgroups except for the LIV of the L3 or below group. However, the PT curve magnitude of FB radiographs was significantly smaller than that of 2-year postoperative radiographs in the ≤ 18-year-old, Risser 4–5, and LIV of the L2 or above groups, but no significant differences were found between them in the other groups.
Illustrative case
We demonstrated an illustrative case. The patient had a Lenke type 1AN curve. Preoperative imaging showed a PT curve of 21°, an MT curve of 52°, and an L curve of 23° (Fig. 1a). Side-bending radiographs revealed flexibility with PT, MT, and L curves corrected to 19°, 40°, and 9°, respectively (Fig. 1b). Fulcrum radiographs further reduced the curves to PT 9°, MT 24° (Fig. 1c). Under traction, the curves measured PT 23°, MT 33°, and L 24° (Fig. 1d).
The patient underwent PSF (T4-L1) at the age of 17 years. Postoperative 1-month imaging demonstrated correction with PT, MT, and L reduced to 18°, 20°, and 7°, respectively (Fig. 1e). At the 2-year follow-up, the curves remained stable with PT, MT, and L measured at 19°, 24°, and 12°, respectively (Fig. 1f). Sagittal imaging showed a T5–T12 angle of 14° preoperatively and 15° at the 2-year follow-up (Fig. 1g).
Discussion
This is the first study to evaluate the role of spinal flexibility radiography in predicting postoperative spontaneous PT curve correction only in patients with Lenke type 1 AIS who underwent PSF of the MT curve. Postoperatively, SB radiographs accurately predicted PT curve correction, with no significant difference in 2-year postoperative Cobb angles. FB radiographs were the only method that did not show a significant difference with 2-year postoperative outcomes for the MT curve. In addition, the PT curve magnitude at the 2-year follow-up showed a significant correlation with preoperative SB radiographic measurements.
Preoperative assessment of curve flexibility in patients with AIS is important for surgical planning and postoperative correction. Various radiographic methods have been used to assess curve flexibility, including SB, push-prone, FB, TR, TR under general anesthesia, and suspension radiography19,20. Although guidelines to select appropriate radiographic methods have not yet been established, the corrective ability of each radiographic method depends on the curve magnitude and location.
For MT curves, FB radiographs generally show the greatest spinal flexibility among SB, FB, and TR methods6,7,10,21. SB radiographs show higher flexibility for moderate MT curves (< 50°–60°), while TR is better for severe curves (> 60°)22,23. Our results align with these findings, that FB demonstrated the most flexibility because most of our patients (85.5%) had MT curves ≤ 60°. This was followed by SB and TR in terms of effectiveness.
With regard to the flexibility of PT curves, Watanabe et al. analyzed 163 PT curves and demonstrated that SB radiographs provide greater flexibility for moderate PT curves (< 30°), whereas TR radiographs are more effective for severe PT curves (> 30° to 40°)24. Similarly, in double-thoracic types, TR radiographs outperform SB radiographs in terms of flexibility12. In our study of Lenke type 1 patients with non-structural PT curves of mild-to-moderate severity (mean, 24.7°), SB radiographs provided superior flexibility compared to TR. Moreover, Watanabe et al. reported that in Lenke type 2 patients with structural PT curves, FB radiographs exhibit higher flexibility than TR radiographs11. Our findings concur, showing that FB radiographs render the greatest flexibility in Lenke type 1 patients with mild-to-moderate non-structural PT curves, followed by SB and TR radiographs.
Flexibility radiographs play a crucial role in predicting postoperative curve correction. A systematic review by Khodaei et al. identified FB as the most effective method to estimate the postoperative MT curve correction using contemporary spinal instrumentation20. Our findings align with those of that review, showing no significant differences in the magnitude of the MT curve between FB and 2-year postoperative radiographs.
On the other hand, the systematic review by Khodaei et al. did not establish a definitive method to predict postoperative PT curve correction owing to the limited number and quality of prior studies, although various techniques have been explored. For structural PT curves that were included in instrumented fusion, there was no significant difference in the PT magnitude between preoperative FB and postoperative radiographs11,25. Conversely, non-structural PT curves are generally excluded from fixation procedures following the recommendations of Lenke et al.1, and pose challenges in direct surgical manipulation, complicating their postoperative correction predictions. Kuklo et al. evaluated the spontaneous PT curve correction in patients with major thoracic AIS who underwent PSF without PT curve instrumentations13. They reported positive correlations between postoperative PT correction and preoperative SB radiographs, and similar mean values of PT curve magnitude between preoperative SB (20°, 31% correction) and the latest postoperative radiographs (21°, 28% correction). However, that study had limitations due to the inclusion of both structural and non-structural PT curves across a broad range of magnitudes (20°–49°), which affected the selection of preoperative evaluation methods24. Our study focused on non-structural PT curves in patients with Lenke type 1 AIS undergoing PSF without PT curve instrumentation. We observed no significant differences in the magnitude of the PT curve between SB and PO2Y radiographs, whereas FB overestimated and TR underestimated correction. The clinical significance of SB and PO2Y was minimal, with a mean discrepancy of − 0.03° (95%CI − 1.57°–1.49°), which is comparable to or less than typical radiographic measurement errors26. Furthermore, we found a significant, moderate correlation between the PT curve magnitude of SB and postoperative radiographs. Our results regarding the PT and MT curves are consistent with those reported by Masuda et al., in which FB radiography predicted postoperative correction of the structural curve, whereas SB radiography predicted postoperative correction of the non-structural curve8.
In this study, fusion to L3 was performed in 14 cases. Nine and two out of fourteen cases with the LIV at L3 were classified as Lenke 1C and 1B, respectively. These cases underwent non-selective fusion based on the defined criteria: Cobb angle > 45°, significant rotation, or MT/L Cobb ratio < 1.227,28,29, or significant vertebral rotation. The remaining three cases were classified as Lenke 1AR, characterized by a rightward tilt of the L4 vertebra. Since their last touching vertebra was L3 or below, the LIV was extended to L3.
In these cases, L4 tilt was also a key consideration, as previous studies30,31 have shown that residual L4 tilt may increase the risk of future low back pain and disc degeneration. Thus, caudal extension of fusion was sometimes chosen to achieve better coronal alignment. However, whether to preserve a mobile but tilted L3 or to fuse a level L3 remains controversial and warrants further long-term investigation.
We also conducted subgroup analysis to evaluate the effect of various confounding factors, including age, bone maturity (Risser grade), and the level of UIV and LIV, in which the PT Cobb angle of preoperative SB radiographs did not significantly differ from that of 2-year postoperative radiographs in all subgroups. When compared to the analyses of the overall patients, the PT curve magnitude of FB or TR radiographs and 2-year postoperative radiographs did not significantly differ across all subgroups, possibly due to the small sample size (n = 7–13). However, consistent results were obtained across all subgroups regarding our primary conclusion on the relationship between SB and 2-year postoperative PT curves, suggesting that the influence of confounding factors was limited.
This study had some limitations. First, it was a retrospective study with a small sample size from a single institution. However, our study demonstrated sufficient statistical power (1 − β = 0.86) for detecting a clinically significant difference of 3° in the Cobb angle, which was the previously reported radiographic measurement error for Cobb angle16,17,18. Due to its retrospective nature, this study exhibited variability in implant densities, posterior release techniques, and corrective maneuvers using instrumentation. In addition, the accuracy of flexibility radiography generally depends on patient compliance and the examiner’s technique. Although the strength of our study was the homogeneity of the patients with a 100% follow-up rate, a multicenter study with prospective design is necessary. Furthermore, this study relied on measurements taken by a single observer, and intra-observer or inter-observer variability was not assessed. However, previous studies16,17,18 have reported that inter-observer variability for Cobb angle measurements is approximately 3°, with an intraclass correlation coefficient of approximately 0.95. Based on these findings, we consider the measurement error to be within a clinically acceptable range and unlikely to affect the study conclusions. Finally, this study did not analyze postoperative shoulder balance, which is affected by the postoperative PT curve correction. However, since multiple factors influence postoperative shoulder balance, this study focused on the relationship between preoperative PT curve flexibility and postoperative spontaneous PT curve correction as the first step of our project. This serves as a dataset for predicting postoperative shoulder imbalance in future studies.
Conclusion
Preoperative SB radiographs were useful for estimating postoperative PT curves, whereas FB and TR radiographs overestimated and underestimated operative correction, respectively. Our findings provide useful information for preoperative and intraoperative decision-making for MT curve correction in Lenke type 1 AIS.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are maintained by the first and corresponding author.
References
Lenke, L. G. et al. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Am. 83, 1169–1181 (2001).
Lenke, L. G. et al. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: does classification correlate with treatment?. Spine 27, 604–611. https://doi.org/10.1097/00007632-200203150-00008 (2002).
Newton, P. O. et al. Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis. A study of six hundred and thirty-one patients. J. Bone Jt. Surg. Am. 87, 1937–1946. https://doi.org/10.2106/JBJS.D.02209 (2005).
King, H. A., Moe, J. H., Bradford, D. S. & Winter, R. B. The selection of fusion levels in thoracic idiopathic scoliosis. J. Bone Jt. Surg. Am. 65, 1302–1313 (1983).
Lenke, L. G., Bridwell, K. H., Baldus, C., Blanke, K. & Schoenecker, P. L. Cotrel-Dubousset instrumentation for adolescent idiopathic scoliosis. J. Bone Jt. Surg. Am. 74, 1056–1067 (1992).
Hamzaoglu, A. et al. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine 30, 1637–1642. https://doi.org/10.1097/01.brs.0000170580.92177.d2 (2005).
Luk, K. D., Cheung, K. M., Lu, D. S. & Leong, J. C. Assessment of scoliosis correction in relation to flexibility using the fulcrum bending correction index. Spine 23, 2303–2307. https://doi.org/10.1097/00007632-199811010-00011 (1998).
Masuda, K. et al. The clinical role of preoperative fulcrum-bending and supine side-bending radiographs on the prediction of curve correction in adolescent idiopathic scoliosis. Eur. Spine J. 32, 1140–1145. https://doi.org/10.1007/s00586-023-07603-w (2023).
Cheung, K. M. et al. Predictability of the fulcrum bending radiograph in scoliosis correction with alternate-level pedicle screw fixation. J. Bone Jt. Surg. Am. 92, 169–176. https://doi.org/10.2106/JBJS.H.01831 (2010).
Klepps, S. J., Lenke, L. G., Bridwell, K. H., Bassett, G. S. & Whorton, J. Prospective comparison of flexibility radiographs in adolescent idiopathic scoliosis. Spine 26, E74-79. https://doi.org/10.1097/00007632-200103010-00002 (2001).
Watanabe, K. et al. Evaluating flexibility and predicting curve correction using fulcrum-bending radiographs in Lenke type 2 adolescent idiopathic scoliosis. J. Orthop. Sci. 28, 529–535. https://doi.org/10.1016/j.jos.2022.01.015 (2023).
Kirk, K. L., Kuklo, T. R. & Polly, D. W. Jr. Traction versus side-bending radiographs: Is the proximal thoracic curve the stiffer curve in double thoracic curves?. Am. J. Orthop. (Belle Mead NJ) 32, 284–288 (2003).
Kuklo, T. R. et al. Spontaneous proximal thoracic curve correction after isolated fusion of the main thoracic curve in adolescent idiopathic scoliosis. Spine 26, 1966–1975. https://doi.org/10.1097/00007632-200109150-00006 (2001).
Matsumoto, M. et al. Postoperative distal adding-on and related factors in Lenke type 1A curve. Spine 38, 737–744. https://doi.org/10.1097/BRS.0b013e318279b666 (2013).
Lindgren, A. M. et al. Preoperative factors associated with optimal outcomes of selective thoracic fusion at 5 years. Spine Deform 10, 1117–1122. https://doi.org/10.1007/s43390-022-00500-0 (2022).
Lechner, R. et al. Comparison of two- and three-dimensional measurement of the Cobb angle in scoliosis. Int. Orthop. 41, 957–962. https://doi.org/10.1007/s00264-016-3359-0 (2017).
Prestigiacomo, F. G., Hulsbosch, M., Bruls, V. E. J. & Nieuwenhuis, J. J. Intra- and inter-observer reliability of Cobb angle measurements in patients with adolescent idiopathic scoliosis. Spine Deform 10, 79–86. https://doi.org/10.1007/s43390-021-00398-0 (2022).
Wiliński, P., Piekutin, A., Dmowska, K., Zawieja, W. & Janusz, P. Which method of the radiologic measurements of the angle of curvature in idiopathic scoliosis is the most reliable for an inexperienced researcher?. Indian J. Orthop. https://doi.org/10.1007/s43465-024-01307-z (2024).
He, C. & Wong, M. S. Spinal flexibility assessment on the patients with adolescent idiopathic scoliosis: A literature review. Spine 43, E250–E258. https://doi.org/10.1097/BRS.0000000000002276 (2018).
Khodaei, M. et al. Radiographic methods to estimate surgical outcomes based on spinal flexibility assessment in patients who have adolescent idiopathic scoliosis: A systematic review. Spine J. 18, 2128–2139. https://doi.org/10.1016/j.spinee.2018.06.344 (2018).
Cheung, W. Y., Lenke, L. G. & Luk, K. D. Prediction of scoliosis correction with thoracic segmental pedicle screw constructs using fulcrum bending radiographs. Spine 35, 557–561. https://doi.org/10.1097/BRS.0b013e3181b9cfa9 (2010).
Polly, D. W. Jr. & Sturm, P. F. Traction versus supine side bending. Which technique best determines curve flexibility?. Spine 23, 804–808. https://doi.org/10.1097/00007632-199804010-00013 (1998).
Vaughan, J. J., Winter, R. B. & Lonstein, J. E. Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine 21, 2469–2473. https://doi.org/10.1097/00007632-199611010-00012 (1996).
Watanabe, K. et al. Traction versus supine side-bending radiographs in determining flexibility: What factors influence these techniques?. Spine 32, 2604–2609. https://doi.org/10.1097/BRS.0b013e318158cbcb (2007).
Li, J. et al. Coronal deformity correction in adolescent idiopathic scoliosis patients using the fulcrum-bending radiograph: A prospective comparative analysis of the proximal thoracic, main thoracic, and thoracolumbar/lumbar curves. Eur. Spine J. 20, 105–111. https://doi.org/10.1007/s00586-010-1495-6 (2011).
Goldberg, M. S. et al. Observer variation in assessing spinal curvature and skeletal development in adolescent idiopathic scoliosis. Spine 13, 1371–1377. https://doi.org/10.1097/00007632-198812000-00008 (1988).
Crawford, C. H. 3rd. et al. Selective thoracic fusion in Lenke 1C curves: prevalence and criteria. Spine 38, 1380–1385. https://doi.org/10.1097/BRS.0b013e3182987360 (2013).
Boniello, A. J. et al. Selective versus nonselective thoracic fusion in Lenke 1C curves: A meta-analysis of baseline characteristics and postoperative outcomes. J. Neurosurg. Spine 23, 721–730. https://doi.org/10.3171/2015.1.SPINE141020 (2015).
Kim, D. H., Hyun, S. J. & Kim, K. J. Selection of fusion level for adolescent idiopathic scoliosis surgery : Selective fusion versus postoperative decompensation. J. Korean Neurosurg. Soc. 64, 473–485. https://doi.org/10.3340/jkns.2020.0258 (2021).
Ohashi, M. et al. Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves: A mean 25-year follow-up. Spine 43, E1403–E1411. https://doi.org/10.1097/BRS.0000000000002716 (2018).
Nohara, A. et al. The effects of spinal fusion on lumbar disc degeneration in patients with adolescent idiopathic scoliosis: A minimum 10-year follow-up. Spine Deform 3, 462–468. https://doi.org/10.1016/j.jspd.2015.04.001 (2015).
Author information
Authors and Affiliations
Contributions
K.M. and M.O. wrote the main manuscript text and K.M.and M.O. prepared all figures and tables. K.M, M.O, K.W, K.H, T.H, M.S, T.M, and H.T were involved in data collection and analysis. K.H. and H.K. provided conceptual advice and supervision. All authors reviewed the manuscript and made substantial revisions.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Minato, K., Ohashi, M., Watanabe, K. et al. Association between preoperative proximal thoracic curve flexibility and postoperative spontaneous correction in Lenke type 1 adolescent idiopathic scoliosis: a retrospective study. Sci Rep 15, 16783 (2025). https://doi.org/10.1038/s41598-025-01604-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01604-z